Sir,
Deep anterior lamellar keratoplasty (DALK) involves removal of the diseased anterior layers of the corneal stroma and preserves the healthy Descemet membrane (DM) and endothelium of the host. As the DM is kept intact in DALK surgery, it is arguable that the healing is faster and the wound more durable compared to penetrating keratoplasty (PK). The main drawback of DALK is the occurrence of a high amount of postoperative astigmatism. Although sutures after PK are removed over a period of 1–2 years, early suture removal after DALK can be carried out to combat high postoperative astigmatism. We describe a case of complete dehiscence of a DALK graft after early suture removal.
Case report
A 40-year-old man with advanced keratoconus underwent DALK in his left eye (OS) using the big bubble technique.1, 2 After a successful centration of the host cornea, an 8.00-mm Hessburg–Barron suction trephine was used to trephine through the anterior corneal stroma. No perforation of the DM was noted during surgery. The stromal dissection was completed up to the DM. An 8.25-mm donor button, without the DM and endothelium, was sutured on to the host bed using single running suture technique. Postoperatively, dexamethasone and chloramphenicol eye drops were given every 2 h. Visual acuity 24 h after surgery was counting fingers in the operated eye. Slit lamp exam (SLE) revealed corneal edema. No leaks were observed. The graft–host junction was well apposed. The follow-up during subsequent weeks revealed an improvement of the graft edema and astigmatism. The videokeratography revealed 4.5 diopters of astigmatism after 4 months. Continuous suturing was removed, but during the procedure an opening of the surgical wound located at 1–2 o'clock hour corresponding to the suture knot was noted (Figure 1a). A contact lens was placed. Close follow-up and antibiotics were recommended. Five days later patient presented with loss of vision, foreign body sensation and redness. The patient denied any trauma or additional mechanical damage. He also referred: ‘Doctor, I had to remove my contact lens because of discomfort'. Inside the contact lens case the graft was found (Figure 1c). SLE revealed the absence of the whole donor graft with DM exposed (Figure 1b). Anterior chamber was stable; no signs of infection or perforation were visible. The digital tonometry (gently) was used to estimate intraocular pressure. The ocular tone was apparently normal, but it is well known that this method is notoriously unreliable. The patient was hospitalized and emergency DALK surgery was performed with the placement of a new 8.25-mm graft. The second surgery was uneventful. Immediate follow-up was also free of complications (Figure 1d). One year after surgery, the best-corrected visual acuity was 20/25 in his OS.
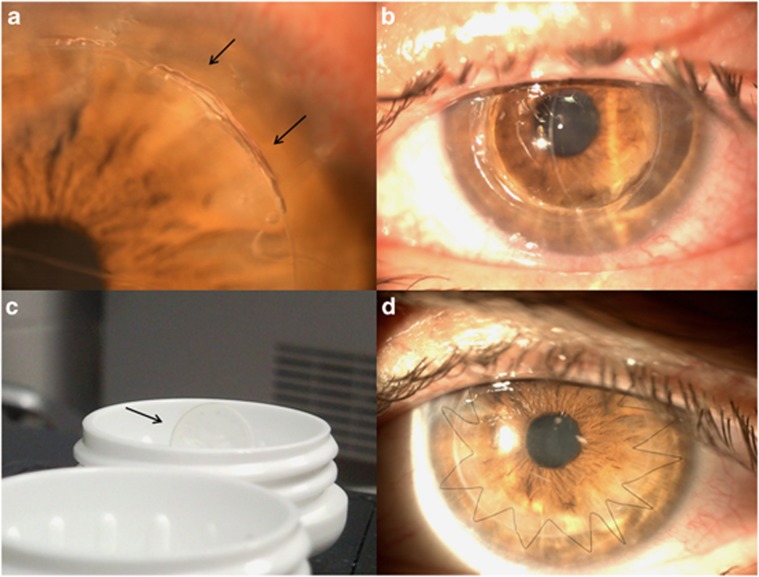
Figure 1.
(a) Slit lamp photograph shows a surgical wound dehiscence located at 1–2 o'clock hours after suture removal. (b) The clinical appearance seen through slit lamp photograph reveals the absence of the whole donor graft and the DM exposed. Note the anterior chamber is deep and formed. (c) The contact lens case shows the graft inside. Slit lamp photograph 1 month after the second DALK is shown in (d).
Discussion
Mannan et al1 reported a case of spontaneous wound dehiscence after DALK. The sutures were removed by the end of 5 months and the patient developed spontaneous 270° wound dehiscence.
In DALK, suture removal time should be ∼6 months after surgery.2, 3, 4, 5, 6 The wound healing in the present case has not been probably completed earlier, therefore extensive wound dehiscence may be observed even after minimal mechanical force. Another interesting fact derived from this case is the resistance of DM. The globe remained stable only with 10–12 μm of corneal thickness.
Postoperative medical and nonmedical cares must be strictly followed to reduce complications and improve the result of surgery.
The authors declare no conflict of interest.
References
- Mannan R, Jhanji V, Sharma N, Pruthi A, Vajpayee RB. Spontaneous wound dehiscence after early suture removal after deep anterior lamellar keratoplasty. Eye Contact Lens. 2011;37 (2:109–111. doi: 10.1097/ICL.0b013e31820c7014. [DOI] [PubMed] [Google Scholar]
- Anwar M, Teichmann KD. Big-bubble technique to bare Descemet's membrane in anterior lamellar keratoplasty. J Cataract Refract Surg. 2002;28 (3:398–403. doi: 10.1016/s0886-3350(01)01181-6. [DOI] [PubMed] [Google Scholar]
- Fontana L, Parente G, Tassinari G. Clinical outcomes after deep anterior lamellar keratoplasty using the big-bubble technique in patients with keratoconus. Am J Ophthalmol. 2007;143 (1:117–124. doi: 10.1016/j.ajo.2006.09.025. [DOI] [PubMed] [Google Scholar]
- Javadi MA, Naderi M, Zare M, Jenaban A, Rabei HM, Anissian A. Comparison of the effect of three suturing techniques on postkeratoplasty astigmatism in keratoconus. Cornea. 2006;25 (9:1029–1033. doi: 10.1097/01.ico.0000230498.99648.69. [DOI] [PubMed] [Google Scholar]
- Anwar M, Teichmann KD. Deep lamellar keratoplasty: surgical technique for anterior lamellar keratoplasty with and without baring of Descemet's membrane. Cornea. 2002;21 (4:374–383. doi: 10.1097/00003226-200205000-00009. [DOI] [PubMed] [Google Scholar]
- Acar BT, Vural ET, Acar S. Does the type of suturing technique used affect astigmatism after deep anterior lamellar keratoplasty inkeratoconus patients. Clin Ophthalmol. 2011;5:425–428. doi: 10.2147/OPTH.S18889. [DOI] [PMC free article] [PubMed] [Google Scholar]