Abstract
We present the imaging findings in two cases of IgG4-related disease involving the sinonasal region in the pediatric age group. Imaging findings in IgG4-related disease affecting the nasal cavity and paranasal sinuses have been rarely reported in literature. The diagnosis is made by a combination of clinical, imaging, and histopathologic findings. Radiologists should be aware of the imaging findings of this condition to ensure early diagnosis and treatment.
Keywords: IgG4-related disease, pediatric, sinonasal, young
Introduction
IgG4-related disease (IgG4-RD) is an autoimmune condition characterized by increased serum IgG4 levels and infiltration of IgG4 plasma cells into the tissues. IgG4 is a subtype of IgG and comprises approximately 3-6% of total IgG. Increase in serum IgG4 levels has been associated with various conditions like autoimmune pancreatitis, sclerosing cholangitis, Mikulicz disease, and retroperitoneal fibrosis, which have now been encompassed together as IgG4-RD. The organs predominantly involved in this condition are pancreas, salivary glands, and biliary tract. In the head and neck region, the salivary, lacrimal, and pituitary glands are the commonly affected structures.[1,2] IgG4-RD affecting the nasal cavity and paranasal sinuses is very rare. Here, we report a case series of two patients of pediatric age group (adolescents 12-16 years) diagnosed with IgG4-RD involving the sinonasal region.[3] Imaging findings related to sinonasal involvement are limited to case reports.[4] A literature search on PubMed showed only seven reports of IgG4-RD with sinonasal involvement.[4,5,6,7,8,9,10] In addition, sinonasal IgG4 involvement in pediatric age group has not been reported previously in the literature to the best of our knowledge.
Case Reports
Case 1
A 15-year-old girl presented with recurrent epistaxis and bilateral progressive nasal obstruction of 9 months duration. Epistaxis was severe and required anterior nasal packing on one occasion. On rhinoscopy, the nasal cavity was crowded with thickening of the nasal septum and inferior turbinates on both sides. Magnetic resonance imaging (MRI) showed T1-isointense, T2-hypointense [Figure 1A and B] soft tissue thickening involving the nasal septum, anterior part of the right inferior turbinate, right lateral nasal wall, and uncinate process. Erosion of the uncinate process, inferior turbinate, and septum was seen with extension of soft tissue thickening along the medial wall of the right maxillary sinus [Figure 1B]. In addition, the mass was seen to extend along the right naso-lacrimal duct. On post-contrast study, moderate heterogeneous enhancement of the soft tissue was seen with central hypoenhancing areas [Figure 1C]. Parotid, pituitary, lacrimal, and submandibular glands were normal. Serum IgG4 levels were raised (206 mg/dl; 95th percentile range = 6-112 mg/dl). Endoscopic examination was done under general anesthesia which confirmed the imaging findings. Histopathology showed dense fibrosis with lymphoplasmocytic infiltrate and immunohistochemistry revealed IgG4 plasma cells constituting 50% of IgG plasma cells, confirming the diagnosis of IgG4-RD. Patient was started on prednisolone and is currently on follow-up.
Figure 1(A-C).
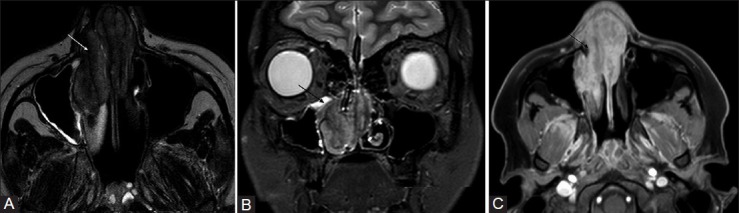
A 15-year-old female with recurrent epistaxis and nasal obstruction. MRI T2W axial and coronal (A, B) images revealed T2-hypointense soft tissue thickening (arrows in A, B) involving the nasal septum and right lateral nasal wall, with extension into the right maxillary sinus (arrow in B). Post-contrast T1W axial image (C) revealed heterogeneous enhancement of lesion (arrow) with central hypoenhancing regions. Biopsy with immunohistochemistry of lesion and raised serum IgG4 levels confirmed the diagnosis of IgG4-related disease
Case 2
A 15-year-old girl presented with recurrent right-sided blood stained nasal discharge of 7 years duration and right-sided facial swelling with difficulty in opening her mouth for 3 months. She also complained of intermittent abdominal pain. On clinical examination, she had a saddle nose deformity with a thickened septum. Mild right eye proptosis was also noted, but her visual acuity was normal. MRI revealed a T1-isointense, T2-hypointense [Figure 2A–D] sheet-like soft tissue thickening extending along the right lateral nasal wall, nasal roof, nasal septum, right maxillary, ethmoid and sphenoid sinus. Erosion of the lamina papyracea, floor of orbit, and posterolateral wall of the maxilla was seen with extension of the lesion into the pterygopalatine fossa, medial orbit, orbital apex, and right cavernous sinus [Figure 2D]. The medial rectus muscle was involved and there was enhancement of the optic nerve sheath. Lesion showed intense homogenous enhancement on post-contrast scans [Figure 2C]. Serum IgG4 levels were elevated (579 mg/dl; 95th percentile range = 6-112 mg/dl). She underwent biopsy of the sinonasal mass which revealed prominent sclerosis and dense lymphoplasma cell infiltrate. Immunohistochemistry revealed IgG4 plasma cells constituting 50% of IgG plasma cells and IgG4-positive cells >30/hpf, which was consistent with IgG4-related sclerosing disease. Ultrasound (USG) abdomen detected mild right hydrouretronephrosis. Computed tomography (CT) abdomen showed ill-defined sheet-like retroperitoneal soft tissue along the right iliac vessels encasing the right ureter, which was consistent with a diagnosis of retroperitoneal fibrosis. Patient was started on prednisolone (1 mg/kg/day). On follow-up after 4 months, there was significant reduction in her serum IgG4 levels (138 mg/dl). Repeat MRI, however, revealed persistent sino-orbital disease with additional increase in soft tissue thickening in the right cavernous sinus with resultant narrowing of the right internal carotid artery (ICA) [Figure 2E]. There was mild persistent hydroureteronephrosis. Patient was started on rituximab (two intravenous infusions of 600 mg- 15 days apart) due to inadequate response to prednisolone and is currently on follow-up.
Figure 2(A-E).
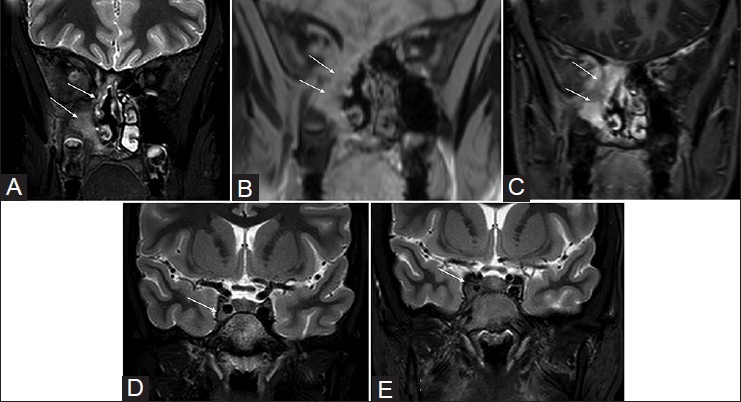
A 15-year-old female with recurrent right-sided epistaxis and mild proptosis. MRI T2W and T1 high-resolution isotropic volume examination (THRIVE) coronal images (A, B) showed T2-hypointense (arrow in A), T1-isointense (arrow in B) sheet-like soft tissue thickening extending along the right lateral nasal wall, nasal septum, and right maxillary sinus. Post-contrast T1W coronal image (C) showed homogenous contrast enhancement (arrow). T2W coronal image (D) showed soft tissue extension into the right cavernous sinus (arrow). On follow-up MRI imaging after 4 months, T2W coronal image (E) showed increase in soft tissue thickening in right cavernous sinus with narrowing of right ICA (arrow)
Discussion
IgG4 disease is a systemic disorder characterized by infiltration of IgG4 plasma cells into the tissues resulting in fibrosis and resultant organ dysfunction. It is an emerging disease entity which is increasingly been reported worldwide. Initially reported with autoimmune pancreatitis, it was subsequently associated with sclerosing cholangitis, retroperitoneal fibrosis, interstitial pneumonia, and mediastinal fibrosis.[1] This entity has various synonyms like IgG4-related sclerosing disease, IgG4-related autoimmune disease, systemic IgG4 plasmacytic syndrome, hyper IgG4 disease, and IgG4-related multiorgan lymphoproliferative syndrome, but IgG4-RD is the preferred terminology now.[11] IgG4-RD is associated with increased serum levels of IgG4. The normal range of IgG4 is 4.8-105 mg/dl. This condition is described more commonly in elderly males.[1] It was interesting to note that both patients in our series were young patients in the pediatric age group and this further expands our understanding of the spectrum of this unique condition.
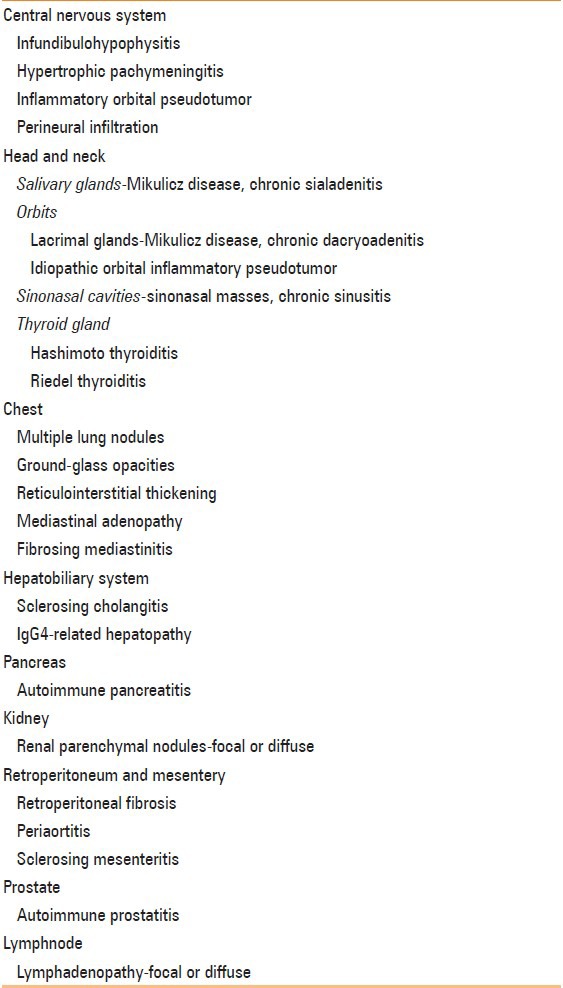
IgG4-RD involves multiple organs synchronously or metachronously, and sometimes may show isolated organ involvement [Table 1].[1,2,11] Clinical symptoms vary depending on the organs involved, and organ dysfunction is a result of cellular infiltration and fibrosis. Commonly involved regions in this condition are pancreas, biliary tract, kidney, retroperitoneum, lungs, head and neck, and blood vessels. In the head and neck region, involvement of salivary glands, lacrimal gland, thyroid gland and nasal cavities is seen.[1,2,4,5] Common imaging manifestations of IgG4-RD in the head and neck include enlargement of the salivary and lacrimal glands, thyroid lesions, and inflammatory pseudotumors in the orbit. Involvement of sinonasal cavity is considered rare, with very few reports describing the imaging findings of this entity.
Table 1.
Systemic manifestations of IgG4-related disease
Presenting symptoms in cases of sinonasal involvement are chronic rhinitis, blood-stained nasal discharge, and nasal obstruction, as was noted in our series.[12] On CT, IgG4 involvement is seen as homogenous soft tissue lesions with or without bone destruction. On MRI, involvement is seen as T2-hypointense soft tissue in the nasal and paranasal sinuses, which shows homogenous enhancement on post-contrast scans.[1,4,5,8,10] In our patients, IgG4 involvement was seen as T2-hypointense sheet-like soft tissue thickening involving the nasal and paranasal sinuses, extending along the walls of contiguous structures, using existing structures as scaffolds with surrounding bone destruction. In one case, MRI showed heterogeneous soft tissue enhancement with central hypoenhancing areas. Histopathology in this case revealed dense fibrosis. Although homogenous contrast enhancement is described commonly in this condition, lesions may show slightly heterogeneous enhancement due to dense fibrosis.
Sasaki et al. have described a case of IgG4-related sclerosing disease in the sinonasal region which showed perineural and bone marrow infiltration.[6] Similarly in our study, infiltration of the pterygopalatine fossa and superior orbital fissure with cavernous sinus extension was seen in one case. Cavernous sinus involvement resulted in narrowing of the ipsilateral ICA, which was probably due to fibrotic nature of the lesion. Toyoda et al. reported that when T2-hypointense lesions are noted in the head and neck region, investigation of IgG4 levels and imaging of chest and abdomen should be done to look for systemic manifestations of IgG4 disease.[5] Systemic manifestation noted in one of our cases was retroperitoneal fibrosis.
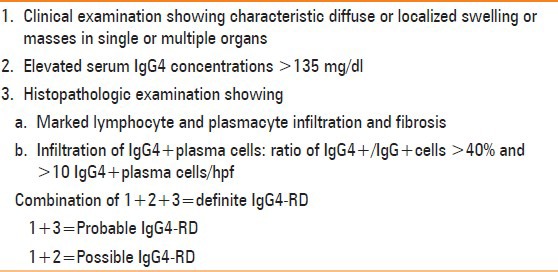
Differentials which need to be considered for T2-hypointense sinonasal lesions include lymphoma, invasive aspergillosis, Wegner's granulomatosis, and solitary fibrous tumor. These can be differentiated based on clinical presentation and by estimation of serum IgG4 levels. Umehara et al. have proposed comprehensive clinical diagnostic criteria (CCD) for the diagnosis of IgG4-RD [Table 2].[11] Moteki et al. studied patients with IgG4-related chronic rhinosinusitis and compared them with a control group of non-IgG4–related chronic rhinosinusitis.[12] They noted that nasal mucosa positive staining of IgG4 is not specific for IgG4 disease and there should be elevated serum IgG4 levels for diagnosis of IgG4 disease. In our study, all cases showed elevated serum IgG4 levels. This condition shows very good response to corticosteroid therapy. However, in some cases of IgG4-RD, treatment might be ineffective or there may be relapse during steroid tapering. Azathioprine or rituximab is useful in such cases.[2] In one of our cases, there was progression of the disease on corticosteroid therapy, with increase in soft tissue in the cavernous sinus despite reduction in serum IgG4 levels. Thus, there may be mismatch in the imaging findings and serum IgG4 levels.
Table 2.
Comprehensive clinical diagnostic criteria for IgG4-RD
Conclusion
IgG4 is an autoimmune condition associated with infiltration of IgG4 plasma cells into the tissues, resulting in fibrosis. Sinonasal involvement is seen as T2-hypointense sheet-like soft tissue thickening extending along the walls of contiguous structures with variable enhancement and surrounding bone destruction. A possibility of IgG4-related sinonasal disease should be considered in a patient with history of nasal obstruction and blood-stained nasal discharge having a locally invasive moderately enhancing T2-hypointense lesion on imaging with elevated serum IgG4 levels. Radiologists should be aware of the imaging findings of this entity to ensure early diagnosis and treatment.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Fujita A, Sakai O, Chapman MN, Sugimoto H. IgG4-related disease of the head and neck: CT and MR imaging manifestations. Radiographics. 2012;32:1945–58. doi: 10.1148/rg.327125032. [DOI] [PubMed] [Google Scholar]
- 2.Horger M, Lamprecht HG, Bares R, Spira D, Schmalzing M, Claussen CD, et al. Systemic IgG4-related sclerosing disease: Spectrum of imaging findings and differential diagnosis. AJR Am J Roentgenol. 2012;199:276–82. doi: 10.2214/AJR.11.8321. [DOI] [PubMed] [Google Scholar]
- 3.Williams K, Thomson D, Seto I, Contopoulos-Ioannidis DG, Ioannidis JP, Curtis S, et al. Standard 6: Age groups for pediatric trials. Pediatrics. 2012;129(Suppl 3):153–60. doi: 10.1542/peds.2012-0055I. [DOI] [PubMed] [Google Scholar]
- 4.Lindau RH, Su YB, Kobayashi R, Smith RB. Immunoglobulin G4-related sclerosing disease of the paranasal sinus. Head Neck. 2013;35:E321–4. doi: 10.1002/hed.23175. [DOI] [PubMed] [Google Scholar]
- 5.Toyoda K, Oba H, Kutomi K, Furui S, Oohara A, Mori H, et al. MR Imaging of IgG4-Related Disease in the Head and Neck and Brain. AJNR Am J Neuroradiol. 2012;33:2136–9. doi: 10.3174/ajnr.A3147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sasaki T, Takahashi K, Mineta M, Fujita T, Aburano T. Immunoglobulin G4 − Related Sclerosing Disease Mimicking Invasive Tumor in the Nasal Cavity and Paranasal Sinuses. AJNR Am J Neuroradiol. 2012;33:19–20. doi: 10.3174/ajnr.A2495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ishida M, Hotta M, Kushima R, Shibayama M, Shimizu T, Okabe H. Multiple IgG4-related sclerosing lesions in the maxillary sinus, parotid gland and nasal septum. Pathol Int. 2009;59:670–5. doi: 10.1111/j.1440-1827.2009.02425.x. [DOI] [PubMed] [Google Scholar]
- 8.Ikeda R, Awataguchi T, Shoji F, Oshima T. A case of paranasal sinus lesions in IgG4-related sclerosing disease. Otolaryngol Head Neck Surg. 2010;142:458–9. doi: 10.1016/j.otohns.2009.09.019. [DOI] [PubMed] [Google Scholar]
- 9.Pace C, Ward S. A rare case of IgG4-related sclerosing disease of the maxillary sinus associated with bone destruction. J Oral Maxillofac Surg. 2010;68:2591–3. doi: 10.1016/j.joms.2009.07.073. [DOI] [PubMed] [Google Scholar]
- 10.Alt JA, Whitaker GT, Allan RW, Vaysberg M. Locally destructive skull base lesion: IgG4-related sclerosing disease. Allergy Rhinol (Providence) 2012;3:e41–5. doi: 10.2500/ar.2012.3.0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Umehara H, Okazaki K, Masaki Y, Kawano M, Yamamoto M, Saeki T, et al. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod Rheumatol. 2012;22:21–30. doi: 10.1007/s10165-011-0571-z. [DOI] [PubMed] [Google Scholar]
- 12.Moteki H, Yasuo M, Hamano H, Uehara T, Usami S. IgG4-related chronic rhinosinusitis: a new clinical entity of nasal disease. Acta Otolaryngol. 2011;131:518–26. doi: 10.3109/00016489.2010.533699. [DOI] [PMC free article] [PubMed] [Google Scholar]


