Abstract
Cysts and cystic-appearing lesions around the knee are common and can be divided into true cysts (synovial cysts, bursae, ganglia, and meniscal cysts) and lesions that mimic cysts (hematomas, seromas, abscesses, vascular lesions, and neoplasms). The specific anatomic location of the cystic lesion often permits the correct diagnosis. In difficult cases, identifying a cystic mass in an atypical location and/or visualizing internal solid contrast enhancement on magnetic resonance imaging (MRI) should raise concern for a neoplasm and the need for further evaluation and intervention.
Keywords: Bursa, cyst, knee, synovial cyst
Introduction
Cysts and cystic-appearing soft-tissue lesions in and around the knee are common and can create a diagnostic dilemma if one is not aware of the potential diagnoses and pitfalls. Most of these lesions are benign and are related to the collection of fluid in bursae, herniation of synovium from the joint, or ganglia arising from tendons and ligaments.[1,2,3,4] However, other processes, both benign and malignant, can produce a cystic-appearing mass and lead to misdiagnosis.[5,6] Ultrasonography (USG) and magnetic resonance imaging (MRI) are the most useful imaging modalities in evaluating these cystic lesions. USG can distinguish cysts from solid lesions and assess the degree of vascularity within the lesion. MRI can help delineate the location of the lesion in relation to anatomic structures and also determine if the lesion is cystic or solid when contrast is administered. In most instances, the location of the lesion and the enhancement pattern are the most important factors in determining its etiology.
Given the many cystic lesions encountered around the knee, it is helpful to divide them into two categories: true cysts (those lined by cells; synovial, bursae, ganglia, and meniscal) and cyst mimickers (traumatic lesions, infectious processes, vascular lesions, and neoplasms) [Table 1]. In this article, we systematically review cystic soft-tissue knee lesions, explaining the important characteristics, typical appearances, and potential pitfalls. For the purpose of this review, we performed a systematic search of the electronic database PubMed to identify relevant studies published in the literature from 1991 to 2012 using the terms “cystic lesions of the knee,” “knee bursa,” “meniscal cysts,” and “synovial cysts of the knee.”
Table 1.
Classification of cysts and cystic-appearing lesions of the knee
Cysts
Synovial cysts
Synovial cysts connect to the joint space, since they represent herniation of synovial tissue into the surrounding soft tissues. At times, it may be difficult or even impossible to distinguish them from bursae or ganglia, which lack a true connection to the joint but at times can connect to the joint.[7] Moreover, the inconsistent use of the terms synovial cyst, bursa, and ganglion in clinical practice and in literature further complicates matters.[1,2,3,4]
Popliteal (Baker's) cyst
The popliteal (Baker's) cyst is by far the most common cyst in the knee, seen in up to 40% of MRI examinations.[4,8] It represents a communication between the posterior joint capsule and the normally occurring gastrocnemius-semimembranosus bursa/recess [Figure 1]. This connection can have a “ball-valve” like mechanism, which is typically opened during knee flexion and closed during extension.[8] Popliteal cysts are lined by synovium, may be simple or septated, and contain hemorrhage, debris, or even osseous loose bodies. Visualizing a communicating fluid collection arising between the tendons of the medial head of the gastrocnemius and semimembranosus is the key to making the diagnosis. Although many popliteal cysts are asymptomatic, large cysts may cause nerve entrapment, compress adjacent vascular structures, or limit knee flexion.[8] Popliteal cysts can be complicated by cyst rupture, which can be indistinguishable clinically from deep venous thrombosis and result in edema in the surrounding fascial planes and subcutaneous fat.
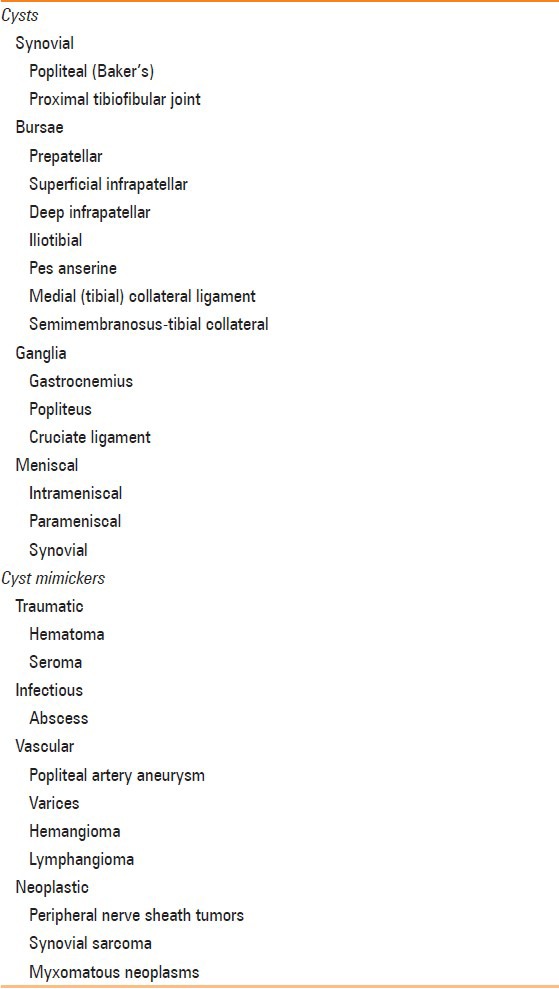
Figure 1(A-C).
Popliteal cyst. A 60-year-old female with knee pain. (A) Lateral knee radiograph demonstrates coarse calcifications (arrow) in the popliteal fossa. (B) Gray scale USG image at the level of popliteal fossa demonstrates a cystic lesion containing echogenic calcifications (arrow) with posterior acoustic shadowing. (C) Axial T2W image through right knee demonstrates the hyperintense popliteal cyst fluid arising between semimembranosus (arrowhead) tendon and medial head of gastrocnemius (asterisk), with hypointense loose bodies (arrow) layering dependently
Proximal tibiofibular joint cyst
The proximal tibiofibular joint (PTFJ) is a synovial joint that connects to the knee joint in 10% of patients[1] [Figure 2]. It is hypothesized that increased knee joint pressure in these patients can result in the formation of a synovial cyst in the PTFJ. These cysts are more common in patients with chronic knee pain and osteoarthritis, but have also been described in high-performance athletes.[1,7] Although relatively uncommon (<1% of MRI examinations) and often asymptomatic, large PTFJ cysts can compress the common peroneal nerve and result in foot drop and muscle weakness[7] [Figure 3].
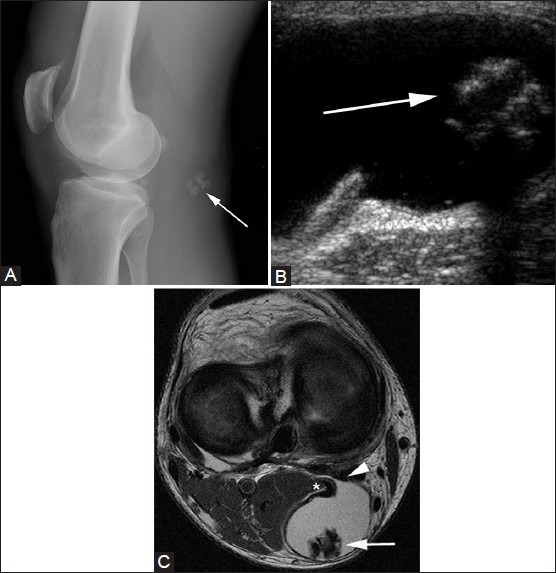
Figure 2(A-C).
PTFJ cyst. A 50-year-old male with palpable mass. Axial T1W MR image (A) demonstrates uniformly hypointense mass (arrow) with small tail (arrowhead), arising from proximal tibiofibular joint. Lesion (arrow) is hyperintense on coronal short tau inversion recovery (STIR) MR image (B) and does not enhance on post-contrast T1W fat-saturated image (C)
Figure 3(A, B).
PTFJ cyst. A 57-year-old man with foot drop. Axial proton density (PD) image (A) shows large cyst (arrows) compressing the common peroneal nerve (arrowhead). There is muscle edema (arrow) in anterior tibialis on the axial STIR image (B)
Bursae
Bursae are cystic lesions containing synovial fluid that reduces friction between moving structures such as tendons, ligaments, bone, and skin.[3,9,10] Bursae are often not visible on imaging unless irritated or inflamed due to trauma, infection, or arthritis. In general, bursae do not connect to the joint space, which distinguishes them from synovial cysts and normal joint recesses; however, at times, they can connect to the joint, such as the iliopsoas bursa.
There are numerous bursae in and around the knee. The prepatellar, superficial infrapatellar, and deep infrapatellar bursae are associated with the patella, whereas the pes anserine, iliotibial (IT), and medial (tibial) collateral ligament, fibular collateral, and semimembranosus-tibial collateral ligament bursae [Figure 4] are not.[3,4,9] Other classification systems categorize the suprapatellar, popliteal, and the gastrocnemius-semimembranosus joint spaces as bursae, though they connect to the knee joint and, thus, are technically joint recesses.[1,3,4,9]
Figure 4.
Semimembranosus/tibial collateral ligament bursa. A 45-year-old woman with posteromedial knee pain. Sagittal T2W fat-saturated image demonstrates a tubular bright cystic mass (arrow) just posterior to the semimembranosus tendon (arrowhead) (image courtesy of Dr. Justin Kung, Boston, MA)
Prepatellar and infrapatellar bursitis
The prepatellar bursa is located anterior to the patella, deep to the subcutaneous soft tissues. Inflammation of the bursa, popularly referred to as “housemaid's knee,” can result from direct trauma to the patella or repetitive injury, producing anterior knee pain which may be associated with a palpable mass [Figure 5]. Infrapatellar bursitis can occur in the superficial (between the tibial tubercle and the overlying skin) or deep (between the posterior aspect of the patellar tendon and the tibia) bursae.[4] Often called “vicar's” or “clergyman's” knee, it is caused by repetitive knee flexion from deep knee bends or jumping. On MRI, the bursa often appears as a triangular, uniformly T2 bright structure between the distal patellar tendon and anterior tibia [Figure 6].
Figure 5(A, B).
Prepatellar bursitis. A 16-year-old female with anterior knee pain. (A) T2W fat-saturated image demonstrates enlarged fluid-filled space in prepatellar region (arrows) with surrounding fat stranding. (B) T1W post-contrast image demonstrates only peripheral enhancement (arrows)
Figure 6.
Infrapatellar bursitis. A 28-year-old male with anterior knee pain. Sagittal fat-saturated T2W image shows triangular pocket of fluid (arrow) between distal patellar tendon and anterior tibia. There is also bone contusion in lateral femoral condyle and fluid in suprapatellar recess (arrowheads), resulting from transient lateral patellar dislocation
IT bursitis
IT bursitis occurs secondary to friction of the IT band against the lateral femoral epicondylar prominence. It is common in patients who participate in intense physical activity, such as distance runners, cyclists, and football players.[4] Repetitive varus stress to the knee can irritate the bursa, resulting in fluid accumulation within cyst-like structures that can appear as T2 bright masses near the distal insertion of the IT band onto Gerdy's tubercle [Figure 7].
Figure 7(A and B).
Iliotibial band cyst. A 46-year-old man with palpable abnormality. (A) Coronal T2W fat-saturated image demonstrates well-circumscribed hyperintense cyst (arrows) abutting the iliotibial band, which does not enhance internally following contrast administration on the post-contrast T1W fat-saturated image (B)
Pes anserine bursitis
The pes anserine bursa is situated on the medial aspect of the knee, between the pes anserine tendons (gracilis, sartorius, and semitendinosus) and the tibial insertion of the tibial collateral ligament. Pes anserine bursitis affects both genders equally, classically occurring in older overweight women with knee osteoarthritis or in athletes in sports that require running and side-to-side movement.[3,4] On MRI, there is a T2 bright cystic structure intimately associated with the pes anserine tendons on the posteromedial aspect of the knee, extending toward their insertion onto the anteromedial aspect of the tibia [Figure 8]. At times, pes anserine bursitis can be confused with a popliteal (Baker's) cyst. Baker's cysts are often larger, communicate with the joint, and can extend into the thigh, whereas pes anserine bursitis does not. Close scrutiny of the tendons associated with the cystic structure is most helpful in distinguishing between these two entities.
Figure 8(A, B).
Pes anserine bursitis. A 30-year-old male with medial knee pain. (A) Axial T2W and (B) sagittal T2W fat-saturated images demonstrate fluid signal (arrows) adjacent to the insertion of the pes anserine tendons
Medial (tibial) collateral ligament bursitis
The medial collateral ligament bursa, which lies between the superficial and deep layers of the medial collateral ligament [Figure 9], infrequently becomes inflamed and filled with fluid.[9] Physical activities that irritate the medial knee soft tissues, such as horseback and motorcycle riding, are potential causes.[9] Mass effect from osteophytes and rheumatoid arthritis are other precipitating factors. On imaging, an oblong fluid collection distends the deep and superficial fibers of the medial collateral ligament. Medial collateral ligament bursitis can at times be confused with a partial tear of the medial collateral ligament or a parameniscal cyst.[4]
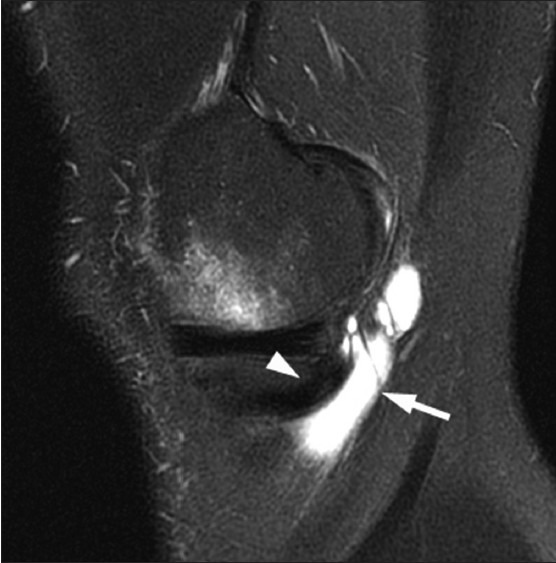
Figure 9.

Medial collateral ligament bursitis. A 56-year-old man with medial knee mass and pain. Coronal T2W fat-saturated image shows an oblong heterogeneous cystic mass (arrow) adjacent to the medial collateral ligament (arrowhead)
Ganglia
Ganglia are myxoid lesions of unknown cause which are characterized by dense connective tissue filled with gelatinous fluid rich in hyaluronic acid and other mucopolysaccharides. Unlike synovial cysts, ganglia do not communicate with the joint space and lack a cellular lining.[7] Based on imaging, however, it is difficult (or impossible) to distinguish ganglia from synovial cysts. Ganglia demonstrate low signal intensity on T1W images, high signal intensity on T2W images, and may show rim enhancement. They classically lack solid internal enhancement, though small multi-septated ganglia can simulate this appearance. Moreover, long-standing ganglia can cause pressure erosions in the adjacent bone, mimicking an aggressive process.
Ganglia around the knee can occur at any tendon insertion, but are most common at the tendon insertion of the medial and lateral gastrocnemius and the popliteus.[7,11] Gastrocnemius ganglia are more common at the medial head and often multiseptated [Figure 10]. Ganglia can be painful if large, although a major concern is mistaking one for a soft-tissue tumor. Popliteus tendon ganglia often arise near their insertion onto the lateral femoral condyle and are usually asymptomatic [Figure 11]. They may be mistaken for parameniscal cysts, and large ganglia can be painful.
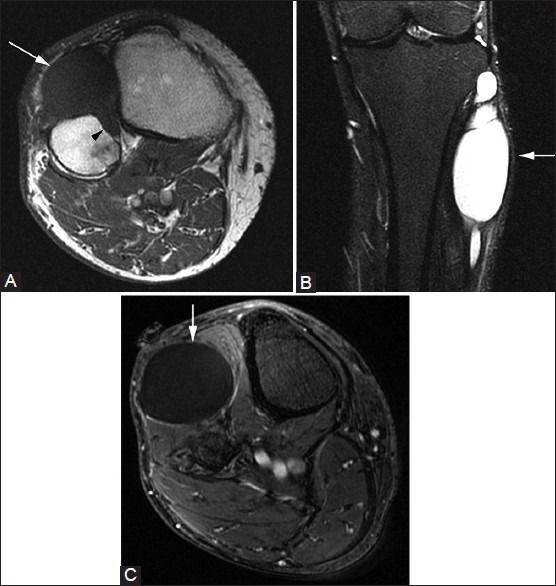
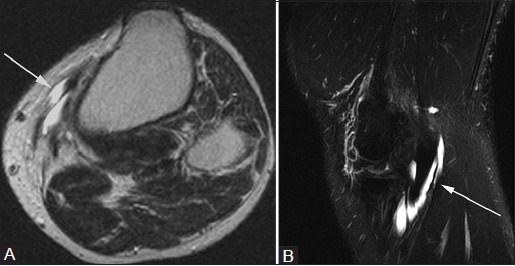
Figure 10(A-C).

Gastrocnemius ganglion. A 45-year-old male with knee pain. Sagittal PDW image (A) demonstrates lobulated lesion (arrows) at insertion of medial head of gastrocnemius that is hyperintense on sagittal (B) and coronal (C) T2W fat-saturated images
Figure 11(A, B).
Popliteus ganglion. A 34-year-old woman with knee pain. (A) Axial and (B) sagittal T2W fat-saturated images show a cystic lesion (arrow) in the popliteus tendon sheath
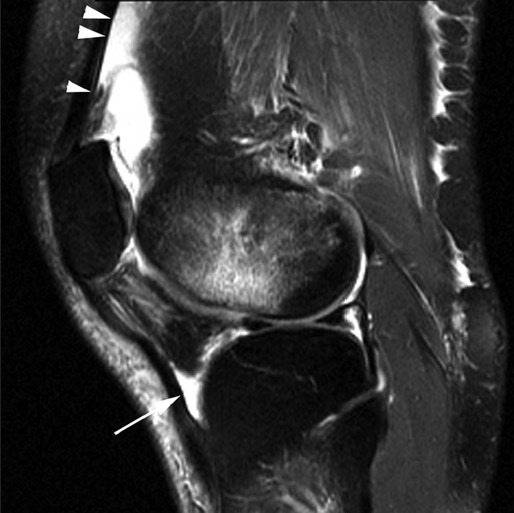
Intra-articular ganglia can be associated with cruciate ligaments. Anterior cruciate ligament (ACL) ganglia are more common than posterior cruciate ligament (PCL) ganglia and can have a “drumstick” appearance with enlargement and increased T2 signal in the proximal ACL fibers[12] [Figure 12]. This increased T2 signal can be seen as a discrete focus of fluid or a more diffuse abnormality of “mucoid degeneration.” It is important to distinguish ACL ganglia from a ligament tear because patients with ACL ganglia do not have instability and are usually asymptomatic. Although the ACL becomes enlarged due to the ganglion, one should still be able to see continuous intact ligament fibers, which distinguishes this process from an ACL tear. A PCL ganglion [Figure 13] is less common.
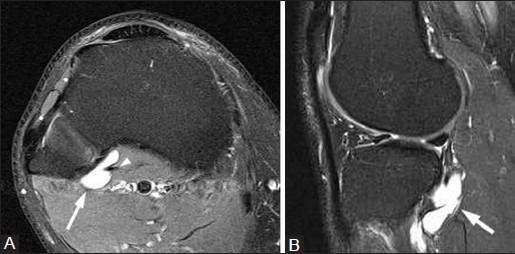
Figure 12(A, B).
ACL ganglion. A 31-year-old male with knee pain. (A) Sagittal PDW and (B) T2W fat-saturated images demonstrate cystic lesion in proximal fibers of anterior cruciate ligament (arrows), which expands ligament fibers and produces “drumstick” appearance. Note the presence of continuous intact ACL fibers
Figure 13.
PCL ganglion. A 28-year-old male with persistent pain after injury. Sagittal T2W fat-saturated image demonstrates multilobulated cystic lesion (arrow) involving distal posterior cruciate ligament
Meniscal cysts
The medial and lateral menisci are composed of type I collagen fibers oriented in a circumferential pattern in order to resist hoop stress.[13] They participate in load sharing and shock absorption. Meniscal cysts are believed to form as a result of tears in the meniscal fibrocartilage, with extrusion of synovial fluid through the meniscal tear.[13] Although lateral cysts are more common in the arthroscopic literature, medial parameniscal cysts are 2 times more common than lateral cysts in the radiologic literature.[12] Medial meniscal cysts are typically associated with posterior horn tears, whereas lateral meniscal cysts arise from anterior horn and body tears.[3,13] Lateral cysts are more symptomatic, with patients presenting with a painful palpable lump, which may account for its higher prevalence in the arthroscopic literature.
Meniscal cysts can be classified into three types: intrameniscal, parameniscal, and synovial.[3] Synovial meniscal cysts are rare, representing cystic outpouchings of the joint capsule that are not associated with trauma. Parameniscal cysts are the most common subtype and occur at the joint line as a focal mass emanating from a meniscal tear [Figure 14]. It is important to remember that medial parameniscal cysts may dissect through the soft tissues of the joint capsule or medial collateral ligament (MCL), thus appearing far from the tear origin. A thin connection to the original tear can usually be demonstrated. Intrameniscal cysts are rare and represent fluid collections within the meniscus that are in continuity with a meniscal tear.
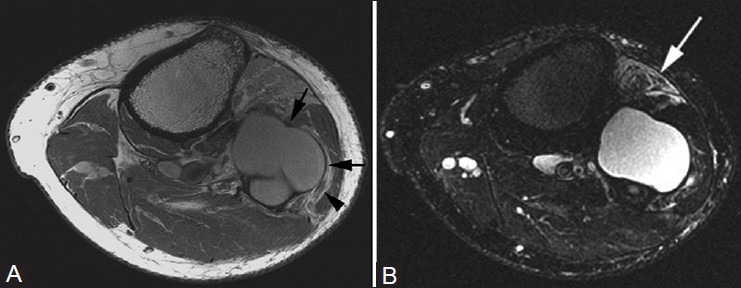
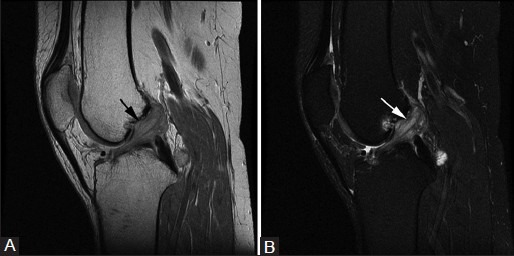
Figure 14(A, B).
Meniscal cyst. A 42-year-old female with knee pain and palpable lateral mass. (A) Coronal PDW image of the right knee demonstrates a multilobulated cyst (arrow) with internal septations, which arises from tear of body of lateral meniscus. (B) T2W fat-saturated image demonstrates cystic nature of this lesion (arrow), which did not enhance following contrast administration (not shown)
Meniscal cysts have low signal intensity on T1W images and increased signal intensity on fluid-sensitive sequences. Loculations or septations are common and show peripheral contrast enhancement, unlike the solid areas of enhancement seen with a neoplasm. On arthrography, a meniscal cyst may fill with contrast, but a lack of filling should not exclude the diagnosis.[13] Treatment of symptomatic cysts is by arthroscopic resection and repair of the causative meniscal tear.
Cyst mimickers
Traumatic lesions
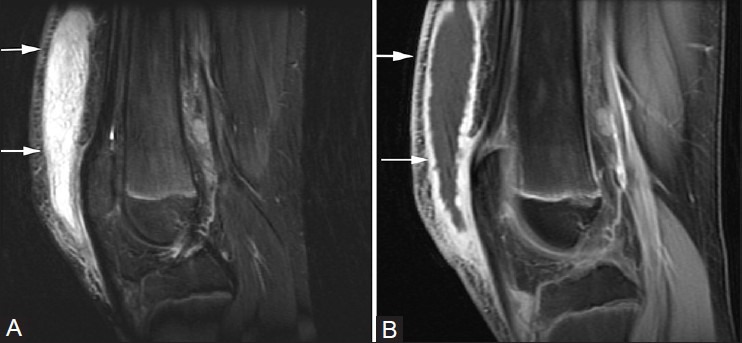
A hematoma represents a contained region of bleeding, which can be traumatic, iatrogenic, or spontaneous in origin [Figure 15]. As the chemical environment of hemoglobin changes over time, so does its MRI appearance.[2] Acute hematoma (hours to days) contains deoxyhemoglobin and is isointense to muscle on T1W images and hypointense on T2W images. In the subacute phase (1-4 weeks following initial injury), a hematoma can contain fluid with free methemoglobin, resulting in high signal intensity on both T1W and T2W images. A hypointense rim can result due to the presence of hemosiderin-laden macrophages.
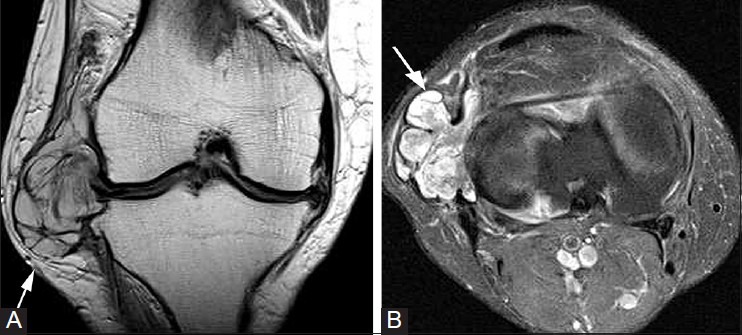
Figure 15(A-D).
Hematoma. A 46-year-old male with pain and swelling after fall. (A) Sagittal T1W image demonstrates a hyperintense lesion (arrows) with hypointense rim and surrounding fat stranding. Axial pre (B) and post (C) T1W fat-saturated, and subtracted post-contrast images (D) confirm lack of enhancement. Crescentic misregistration artifact is seen at the lateral aspect of the hematoma
Seromas are sterile collections of inflammatory exudate contained within a confined tissue space [Figure 16]. They most commonly form when a potential space is created during the surgery. MRI reveals a simple, thin-walled cystic mass that has high T2 intensity and is isointense or hypointense to muscle on T1W images. There can be rim enhancement, but the mass should not contain solid internal enhancement. If a hematoma is complicated by infection, there can be fat stranding in the surrounding soft tissues.
Figure 16(A-C).
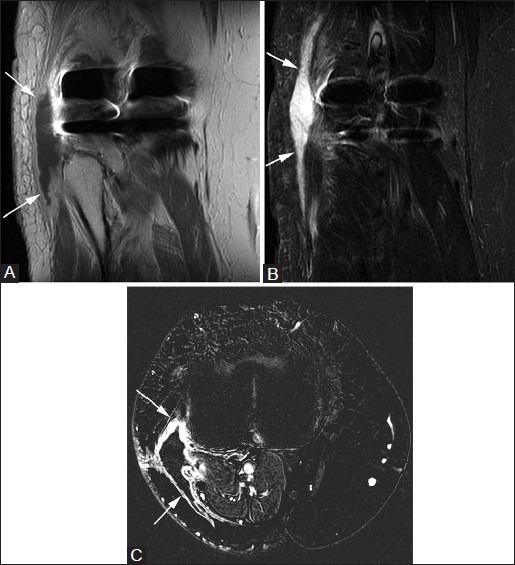
Seroma. A 71-year-old female with swelling following total knee arthroplasty. (A) Coronal T1W and (B) T2W fat-saturated images demonstrate linear fluid collection (arrows) along the lateral aspect of knee. (C) Post-contrast axial subtraction image shows rim enhancement only (arrows). Percutaneous needle drainage yielded non-infected serous fluid
Infection
An abscess can form in the soft tissues of the knee due to hematogenous spread, from direct extension of infection from adjacent tissues, like in osteomyelitis, or when the skin barrier has been breached by surgery or trauma.[5] MRI demonstrates a T2-hyperintense collection that is hypointense on T1W images. A characteristic finding is a thickened rim that enhances after contrast administration [Figure 17]. Moreover, the presence of perilesional edema and enhancement often can help distinguish this “cystic” lesion from a seroma or hematoma. A potential pitfall in distinguishing an abscess from a solid tumor is a phlegmon, which is a precursor to an abscess and can have solid enhancement mimicking a neoplasm. Clinical history and follow-up examinations are important for distinguishing between the two processes.
Figure 17(A-C).

Abscess. A 14-year-old female with fever and knee pain. (A) Sagittal T2W fat-saturated image demonstrates hyperintense mass (arrows) with surrounding soft-tissue edema in popliteal fossa. Axial (B) pre-and (C) post-contrast T1W images show peripheral enhancement (arrows) with lack of central enhancement
Vascular
Focal enlargement of veins, arteries, and lymphatic structures around the knee can produce a “cystic” mass.[2,14] These conditions include aneurysms, varices, hemangiomas, and lymphangiomas. In contrast to the entities described previously, these vascular lesions can have internal solid enhancement that mimics a tumor and may be confused with malignancy. Identifying a connection between the lesion and the vessel of origin can help make the proper diagnosis and avoid a potentially disastrous biopsy.
Aneurysms of the popliteal artery [Figure 18] account for up to 80% of peripheral arterial aneurysms and are bilateral in half of the cases.[1] On imaging, the distinguishing features of an aneurysm of the popliteal artery include location in the popliteal fossa and a lamellated appearance of alternating high and low signal intensity on MRI images consistent with mural thrombus.[1]
Figure 18(A-C).
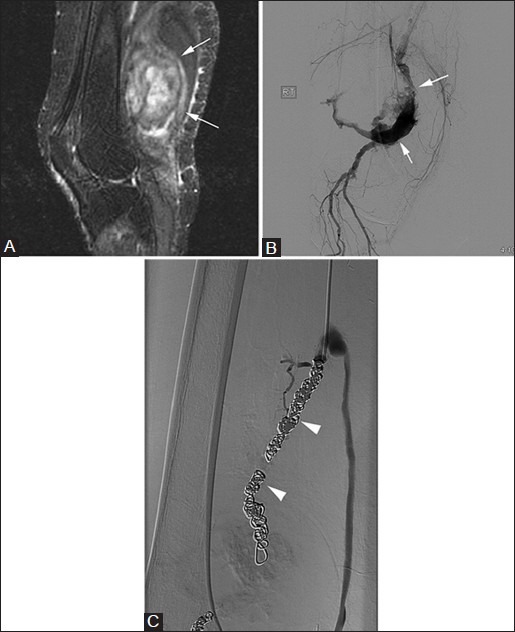
Popliteal artery aneurysm. A 62-year-old male with pulsatile mass in popliteal fossa. (A) Sagittal T2W fat-saturated image demonstrates heterogeneous mass in the region of popliteal fossa (arrows). (B) Digital subtraction angiography shows partial thrombosis of large popliteal fossa aneurysm (arrows), which was subsequently embolized with coils (arrowheads) (C)
Hemangiomas commonly occur in the extremities, including the knee. They are typically soft, compressible, non-pulsatile masses that give a bluish discoloration to the involved skin and subcutaneous tissues.[15] On imaging, hemangiomas appear as dilated venous channels which may contain thrombus and phleboliths [Figure 19]. These masses typically have low-to-intermediate signal intensity on T1W images, high signal intensity on fluid-sensitive sequences, and contain foci of low signal on all sequences from phleboliths.[15] Hemangiomas often respect tissue planes, though they may cause skeletal hypertrophy or remodeling. There may be secondary involvement of adjacent cortical bone from mass effect, or fatty atrophy of adjacent muscles due to alterations in regional blood flow.
Figure 19(A, B).
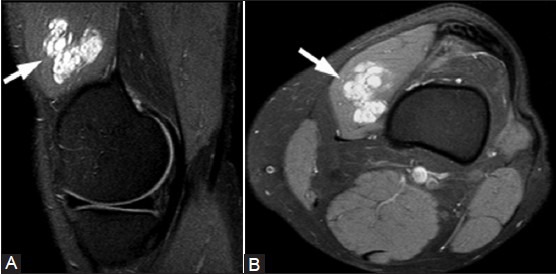
Intramuscular hemangioma. A 54-year-old female with knee mass and pain. (A) Sagittal T2W fat-saturated and (B) axial T1W fat-saturated post-contrast images show a lobulated enhancing cystic mass (arrows) in the vastus medialis
Lymphatic malformations are often present at birth, but may not become evident until later in life. MRI demonstrates a similar appearance to that of venous malformations; they may be macrocystic or microcystic, with the latter form predominating in the extremities [Figure 20]. They typically lack internal or solid areas of enhancement.[16] Venous varices may occur about the knee [Figure 21] and can be identified by showing connection to an adjacent vein.[14]
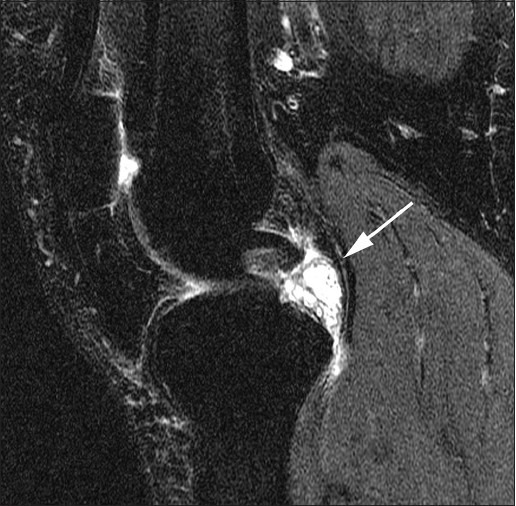
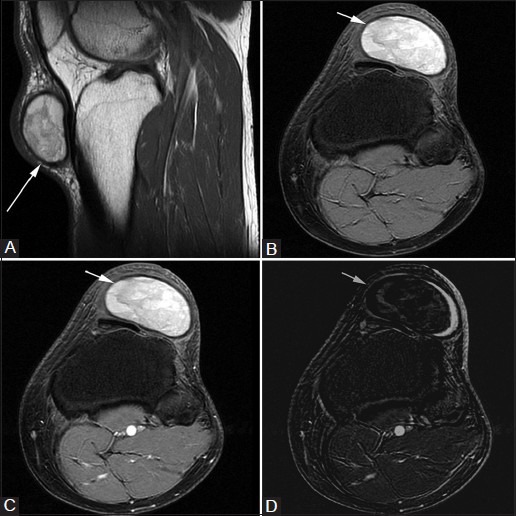
Figure 20(A, B).
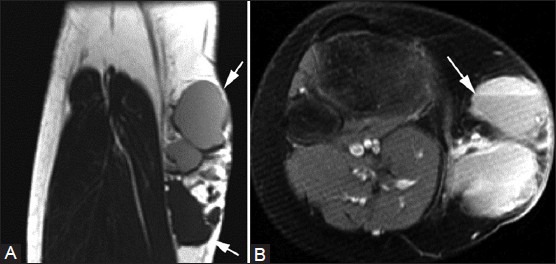
Lymphatic malformation. A 23-year-old female with palpable medial knee mass. (A) Coronal T1W image shows multilobulated cystic lesion (arrows) in the medial aspect of the knee that is isointense and hyperintense to muscle. (B) Axial fat-suppressed T2W image shows fluid-fluid levels (arrow) in this multicystic lesion
Figure 21.
Venous varix. A 57-year-old female with knee pain. Axial post-contrast T1W fat-saturated image demonstrates lobulated vascular structure (arrows) draining into the popliteal vein
Neoplasms
At times, a “cystic” mass about the knee can represent a benign or malignant neoplasm. The main diagnostic considerations are peripheral nerve sheath tumor (PNST), synovial sarcoma, and myxomatous tumor, all of which can appear uniformly isointense and hyperintense when compared to skeletal muscle on T1W and T2W MR images, respectively.[15] These neoplasms should have internal enhancement when contrast is administered, which distinguishes them from many of the cystic entities described previously. Exceptions are necrotic forms of these neoplasms [Figure 22].
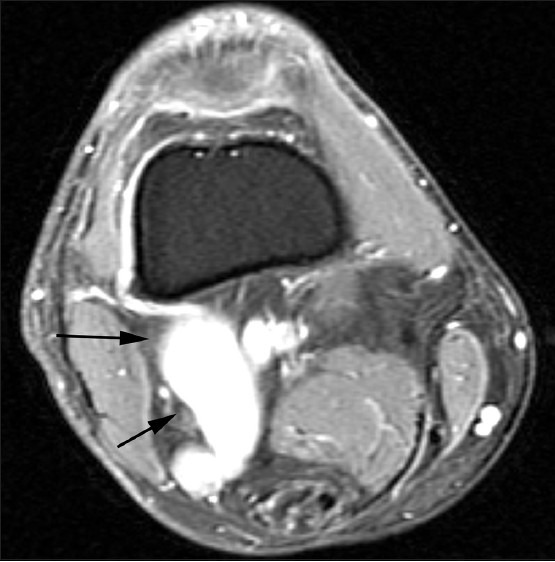
Figure 22(A-C).
Necrotic bladder cancer soft-tissue metastasis. A 65-year-old man with knee pain. (A) Coronal T2W fat-saturated and (B) axial T2W images show a cystic mass (arrows) in the vastus medialis with surrounding edema. (C) Axial T1W fat-saturated post-contrast image shows thick rim enhancement (arrow) and a lack of central enhancement due to tumor necrosis
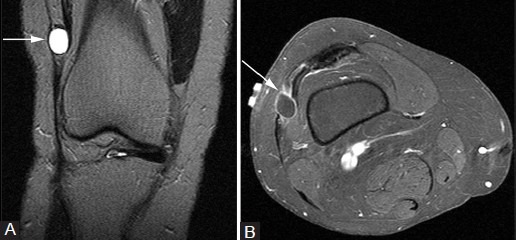
Benign PNSTs include schwannomas and neurofibromas. The more common schwannomas arise from schwann cells, which produce myelin and are located on the periphery of the nerve; neurofibromas arise from the nerve itself, making surgical resection more difficult.[15] On MRI imaging, a PNST appears as a fusiform mass arising from a nerve, occasionally producing a “tail” on both ends where the nerve enters and exits the mass [Figure 23]. Both schwannomas and neurofibromas can have a rim of peripheral fat, known as the “split fat” sign and/or a central focus of low signal within the hyperintense mass on T2W images, called a “target sign.”[15] Malignant peripheral nerve sheath tumors (MPNSTs) are rare, but should be considered if there is a rapid change in size of the lesion or the development of pain in a previously painless mass.[5,15]
Figure 23(A-D).
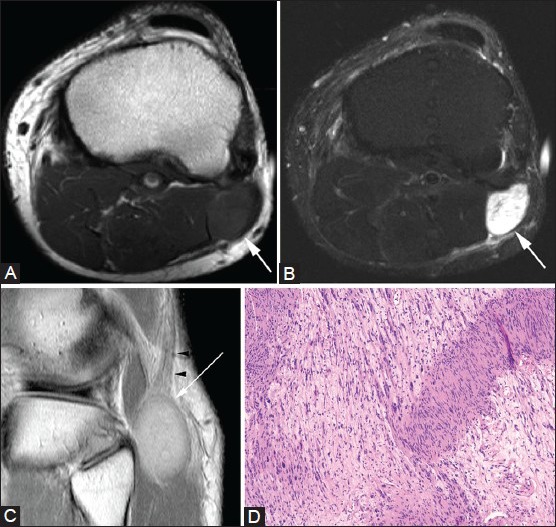
Schwannoma. A 38-year-old male with knee pain. Axial (A) T1W and (B) T2W fat-suppressed images show T2-hyperintense lesion (arrows) in the lateral soft tissue of the knee. (C) Coronal PDW image confirms that the mass (arrow) arises from common peroneal nerve (arrowheads). (D) Photomicrograph [hematoxylin and eosin (H and E), ×400] shows alternating hypocellular and hypercellular spindle cells with Verocay bodies and cytologically bland spindle cells with plump nuclei, consistent with a schwannoma
Synovial sarcoma is a lesion of unknown origin that accounts for 10% of all primary soft-tissue malignant tumors.[6] Despite its name, it does not arise from the synovium. Initial investigators mistook the tumor cells for synovial cells, leading to this misnomer. Synovial sarcomas occur most commonly in young adults, often around knee, ankle, and foot joints. They often appear as well-defined, non-infiltrative masses that are T1 hypointense and T2 hyperintense [Figure 24]. They may demonstrate a “triple signal” pattern on T2W MRI images, which is characterized by hypointense, isointense, and hyperintense regions within the mass relative to fat.[6] A helpful feature distinguishing synovial sarcoma from other soft-tissue tumors is the presence of punctate heterogeneous calcifications; if these are extensive, the lesion has a better prognosis.[6,15]
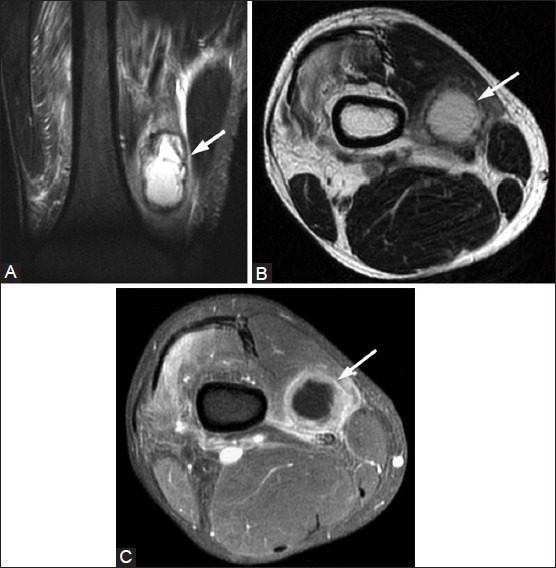
Figure 24(A-C).
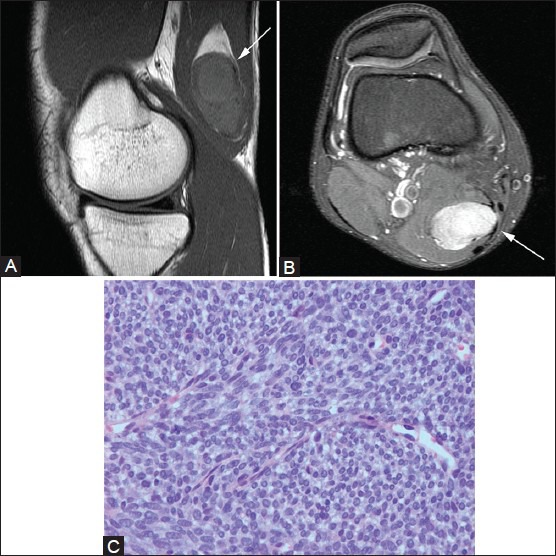
Synovial sarcoma. A 23-year-old male with palpable mass. (A) Sagittal T1W image demonstrates hypointense oblong mass in semimembranosus muscle (arrow), which has solid internal enhancement (arrow) on post-contrast T1W fat-saturated image (B). (C) Photomicrograph (H and E, ×200) shows a highly cellular spindle cell neoplasm composed of densely packed cells with scant cytoplasm. The tumor is characterized by its lack of nuclear pleomorphism and a mitotic rate that is lower than expected for such a cellular tumor, consistent with a synovial sarcoma
Myxomatous neoplasms, which may be benign or malignant, are associated with an overproduction of mucopolysaccharide substances.[15,17] These neoplasms include benign intramuscular and juxtaarticular myxomas, as well such malignant sarcomas with myxoid components such as myxoid liposarcomas and myxoid fibrosarcomas. Due to the abundant myxoid matrix, these tumors mimic cysts and appear hypointense on T1W images and extremely hyperintense on T2W images [Figure 25]. Internal and solid contrast enhancement helps distinguish these lesions from a cyst. On USG, myxomatous lesions appear as well-defined, hypovascular, and hypoechoic masses with minimal internal echoes, and they can demonstrate enhanced through transmission similar to cysts. On radiographs, a myxoma can be mistaken for a lipoma due to its low density. Malignant myxoid tumors are often difficult to distinguish from each other, but all are typically larger, with less-defined margins and heterogeneous signal on all sequences when compared to benign myxomatous lesions.[15,17]
Figure 25(A-C).
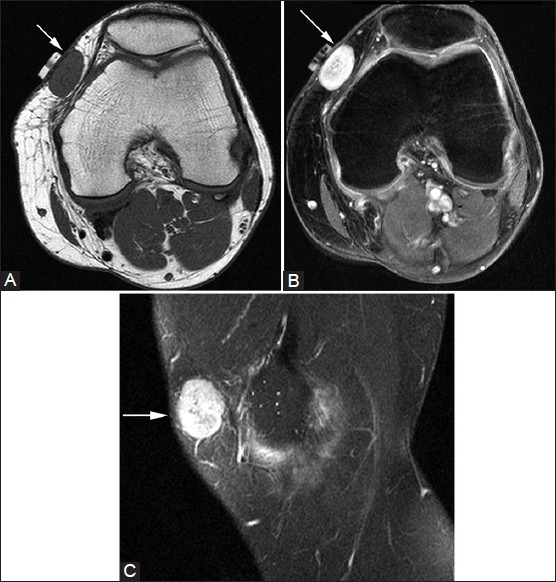
Juxta-articular myxoma. A 27-year-old female with palpable abnormality. (A) Axial T1W image shows well-circumscribed, ovoid cystic lesion in medial subcutaneous tissues that is hyperintense on the (B) axial T2W fat-saturated image. (C) Sagittal post-contrast T1W fat-saturated MR image shows solid internal enhancement (arrow)
Conclusion
Cysts and cystic-appearing lesions around the knee are common and can be divided into true cysts (synovial cysts, bursae, ganglia, and meniscal cysts) and lesions that mimic cysts (hematomas, seromas, abscesses, vascular lesions, and neoplasms). The specific anatomic location of the cystic lesion often permits the correct diagnosis. In difficult cases, identifying a cystic mass in an atypical location and/or visualizing internal solid contrast enhancement on MRI imaging should raise concern for a neoplasm and the need for further evaluation and intervention.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.McCarthy CL, McNally EG. The MRI appearance of cystic lesions around the knee. Skeletal Radiol. 2004;33:187–209. doi: 10.1007/s00256-003-0741-y. [DOI] [PubMed] [Google Scholar]
- 2.Beall DP, Ly JQ, Wolff JD, Sweet CF, Kirby AB, Murphy MP, et al. Cystic masses of the knee: Magnetic resonance imaging findings. Curr Probl Diagn Radiol. 2005;34:143–59. doi: 10.1067/j.cpradiol.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 3.Beaman FD, Peterson JJ. MR imaging of cysts, ganglia, and bursae about the knee. Radiol Clin North Am. 2007;45:969–82. doi: 10.1016/j.rcl.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 4.Marra MD, Crema MD, Chung M, Roemer FW, Hunter DJ, Zaim S, et al. MRI features of cystic lesions around the knee. Knee. 2008;15:423–38. doi: 10.1016/j.knee.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 5.Butler MG, Fuchigami KD, Chako A. MRI of posterior knee masses. Skeletal Radiol. 1996;25:309–17. doi: 10.1007/s002560050087. [DOI] [PubMed] [Google Scholar]
- 6.Bakri A, Shinagare AB, Krajewski KM, Howard SA, Jagannathan JP, Hornick JL, et al. Synovial sarcoma: imaging features of common and uncommon primary sites, metastatic patterns, and treatment response. Am J Roentgenol. 2012;199:W208–15. doi: 10.2214/AJR.11.8039. [DOI] [PubMed] [Google Scholar]
- 7.Kim JY, Jung SA, Sung MS, Park YH, Kang YK. Extra-articular soft tissue ganglion cyst around the knee: Focus on the associated findings. Eur Radiol. 2004;14:106–11. doi: 10.1007/s00330-003-1969-6. [DOI] [PubMed] [Google Scholar]
- 8.Handy JR. Popliteal cysts in adults: a review. Semin Arthritis Rheum. 2001;31:108–18. doi: 10.1053/sarh.2001.27659. [DOI] [PubMed] [Google Scholar]
- 9.De Maeseneer M, Shahabpour M, Van Roy F, Goossens A, De Ridder F, Clarijs J, et al. MR imaging of the medial collateral ligament bursa: Findings in patients and anatomic data derived from cadavers. Am J Roentgenol. 2001;177:911–7. doi: 10.2214/ajr.177.4.1770911. [DOI] [PubMed] [Google Scholar]
- 10.Chatra PS. Bursae around the knee joints. Indian J Radiol Imaging. 2012;22:27–30. doi: 10.4103/0971-3026.95400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.James SL, Connell DA, Bell J, Saifuddin A. Ganglion cysts at the gastrocnemius origin: A series of ten cases. Skeletal Radiol. 2007;36:139–43. doi: 10.1007/s00256-006-0225-y. [DOI] [PubMed] [Google Scholar]
- 12.Fernandes JL, Viana SL, Mendonca JL, Freitas FM, Bezerra AS, Lima GA, et al. Mucoid degeneration of the anterior cruciate ligament: Magnetic resonance imaging findings of an underdiagnosed entity. Acta Radiol. 2008;49:75–9. doi: 10.1080/02841850701660497. [DOI] [PubMed] [Google Scholar]
- 13.Campbell SE, Sanders TG, Morrison WB. MR imaging of meniscal cysts: Incidence, location, and clinical significance. Am J Roentgenol. 2001;177:409–13. doi: 10.2214/ajr.177.2.1770409. [DOI] [PubMed] [Google Scholar]
- 14.Jans L, Ditchfield M, Jaremko JL, Stephens N, Verstraete K. MRI demonstrates the extension of juxta-articular venous malformation of the knee and correlates with joint changes. Eur Radiol. 2010;20:1792–8. doi: 10.1007/s00330-010-1733-7. [DOI] [PubMed] [Google Scholar]
- 15.Wu JS, Hochman MG. Soft-tissue tumors and tumorlike lesions: A systematic imaging approach. Radiology. 2009;253:297–316. doi: 10.1148/radiol.2532081199. [DOI] [PubMed] [Google Scholar]
- 16.Wunderbaldinger P, Paya K, Partik B, Turetschek K, Hormann M, Horcher E, et al. CT and MR imaging of generalized cystic lymphangiomatosis in pediatric patients. Am J Roentgenol. 2000;174:827–32. doi: 10.2214/ajr.174.3.1740827. [DOI] [PubMed] [Google Scholar]
- 17.Daluiski A, Seeger LL, Doberneck SA, Finerman GA, Eckardt JJ. A case of juxta-articular myxoma of the knee. Skeletal Radiol. 1995;24:389–91. doi: 10.1007/BF00197076. [DOI] [PubMed] [Google Scholar]


