Abstract
Gastrointestinal stromal tumors (GIST) are the most common mesenchymal tumors of the digestive tract. Approximately two thirds of clinically manifest tumors occur in the stomach, nearly one third in the small bowel, and the rest in the colorectal region with a few cases in the esophagus. GIST originate within the smooth muscle layer in the wall of the tubular gastrointestinal tract and grow mostly toward the serosa, far less often toward the mucosa. In the latter case, ulceration may develop and can cause gastrointestinal bleeding as the cardinal symptom. However, most GIST of the stomach are asymptomatic. They are increasingly detected incidentally as small intramural or submucosal tumors during endoscopy and particularly during endoscopic ultrasound. Epidemiological and molecular genetic findings suggest that early asymptomatic GIST of the stomach (< 1 cm) show self-limiting tumorigenesis. Thus, early (< 1 cm) asymptomatic gastric GIST (synonym: micro-GIST) are found in 20%-30% of the elderly. The mostly elderly people with early gastric GIST have an excellent GIST-specific prognosis. Patients with early GIST of the stomach can therefore be managed by endoscopic surveillance.
Keywords: Mirco-gastrointestinal stromal tumors, Gastrointestinal stromal tumor, Gastric, Neoplasia, Cancer, Endoscopy, Endoscopic ultrasound
Core tip: Small gastric gastrointestinal stromal tumors (GIST) are by far the commonest neoplasias of the stomach. Thus, early gastric GIST of less than 1 cm in size are found in 20%-30% of the elderly. The natural disease-specific prognosis of early gastric GIST (< 1 cm), also called micro-GIST, is excellent in the mostly elderly patients. Micro-GIST of the stomach appear to have a self-limiting tumorigenesis. Local endoscopic or surgical resection of early asymptomatic GIST (< 1 cm) of the stomach is in general not indicated in the elderly. Instead endoscopic surveillance is advised.
INTRODUCTION
Gastrointestinal stromal tumors (GIST) originate from mesenchymal cells, i.e., the socalled interstitial cells of Cajal that act as pacemakers, or from a common precursor cell along the intestine. Approximately 50%-70% of clinically manifest tumors arise in the stomach, 20%-30% in the small bowel, 5%-15% in the large bowel and less than 5% in the esophagus or other locations. The mean age at diagnosis is between 66 and 69 years for both women and men. About 3% of clinically manifest GIST are diagnosed before the age of 21 years. Their occurrence is predominantly sporadic[1]. There may be a connection with hereditary diseases in a small percentage of cases (neurofibromatosis type 1, Carney triad, familial GIST and mastocytosis).
Clinically manifest GIST are rare with an annual incidence rate of 10 to 20 cases per million population[2]. Much more common, on the other hand, are early (up to 1 cm large) asymptomatic gastric GIST, also called micro-GIST, which are found in 20%-30% of the elderly[3-5]. The striking discrepancy between the incidence of GIST in autopsy stomachs or gastrectomy specimens and the incidence of clinically manifest GIST suggests that early asymptomatic GIST of the stomach are precursor lesions from which clinically manifest GIST arise only in exceptional cases. Thus the characteristics of early asymptomatic GIST of the stomach will be discussed here with reference to clinical management.
SYMPTOMS AND DIAGNOSIS
The vast majority of early gastric GIST are asymptomatic. Patients with symptomatic gastric GIST, which are usually larger than 2-3 cm, most commonly present with gastrointestinal bleeding, anemia, epigastric pain and sometimes palpable resistance, vomiting, and weight loss.
GIST metastasize mainly to the liver and peritoneum. Lung and bone metastases are unusual, and lymph node metastases are rare. Laboratory examinations are of no diagnostic value. Metastases can be detected by ultrasound and CT scans; the latter may be optionally combined with positron emission tomography (FDGPET/CT)[6].
ENDOSCOPY
Gastroscopy is the standard procedure for diagnosing GIST of the stomach. Endoscopy detects the mostly intramural tumors and also enables endoscopic ultrasound (EUS)-guided acquisition of cytological and histological samples. The latter is imperative for a definitive diagnosis. In contrast to histology, cytology does not allow for determination of the mitotic rate. In emergency situations where urgent surgery is indicated, the clinically suspected diagnosis of GIST is verified postoperatively by histological evaluation of the resected tumor specimen.
Typical endoscopic findings in patients with early gastric GIST are shown in Figure 1. Early asymptomatic GISTs of the stomach are mostly detected incidentally during gastroscopy as submucosal protrusions < 1 cm in diameter. Due to their submucosal or intramural location, however, they usually cannot be verified histologically by routine biopsies of the superficial normal mucosa. Endoscopic submucosal resection (ESMR) might be a procedure for diagnosing the very few, early gastric GIST that are confined to the mucosa and submucosa[7]. No reports are available on ESMR or endoscopic mucosal resection (EMR) for early gastric GIST[8]. R0 resection of the more common gastric GIST that arise from the muscularis propria cannot be achieved using traditional endoscopic techniques. However, a lot of them can be completely en bloc resected by endoscopic submucosal dissection in expert hands[9]. (Laparoscopic) Surgical resection is the method of choice for larger GIST.
Figure 1.
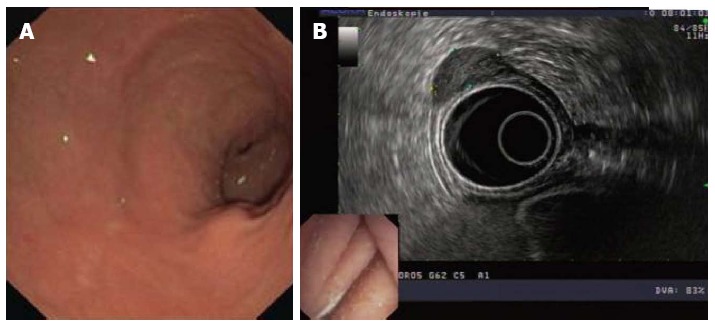
Typical endoscopic features of an early gastrointestinal stromal tumors of the stomach. A: Endoscopic image of an early GIST of the stomach; B: Endosonographic image of an early GIST of the stomach. Modified from reference [33]. GIST: Gastrointestinal stromal tumors.
EUS AND EUS-FNA
EUS plays a decisive role in the diagnosis, the measurement of size, the assessment of local infiltration, and clinical management of submucosal or intramural lesions of the stomach. It reliably distinguishes mucosal lesions from a submucosal mass or extramural compression. EUS is often able to correctly identify the type of lesion based on its echo features, its assignment to a specific wall layer or its location outside the stomach.
EUS examinations can be performed with a radial scanner (360°) or a linear echoendoscope. Filling the stomach with water optimizes acoustic coupling of the probe to the stomach wall. Gastric GIST typically arise from the fourth echo layer of the stomach wall (muscularis propria), rarely also from the submucosa (third echo layer). They are usually visualized as oval-to-elliptical hypoechoic lesions with a smooth border. Large GIST often show a large central anechoic blood vessel or hyperechoic air bubbles in the case of central ulceration. On EUS images, large GIST can appear inhomogeneous with hypo- and hyperechoic parts. GIST characteristically lack paragastric lymph node metastases; this too can be clearly demonstrated with EUS.
In the acquisition of cytological and histological samples, EUS-guided biopsy of the submucosal or intramural GIST plays a decisive role. The definitive cytological and/or histological verification of larger gastric GIST is currently achieved in 50%-70% of EUS-guided fine-needle aspiration (FNA) or EUS-guided Trucut punch biopsies[10-15]. The histological diagnosis of GIST requires immunohistochemical detection of CD117 and particularly in CD117-negative tumors of DOG1 with the corresponding histomorphological findings. Most early GIST of the stomach can be followed-up by endoscopic examinations (EUS) even without initial histological confirmation.
PATHOLOGY, METASTATIC RISK AND PROGNOSIS
The diagnosis of GIST first came into existence in 1998 when the CD117 antigen was identified as being almost invariably expressed by GIST in over 90% of the cases; in contrast, leiomyomas, leiomyosarcomas and other spindle-cell gastrointestinal tumors are typically CD117-negative. CD117 antigen is the type III transmembrane receptor tyrosine kinase KIT, a KIT proto-oncogene product[1]. Approximately 95% of GIST in adulthood overexpress KIT. Nearly 80% of GIST show KIT gene mutations that lead to constitutive activation of the KIT receptor. More than 60% of the KIT activating mutations occur in exon 11. About 10% of the cases have mutations in exon 9, much more rarely (< 2%) in exon 13 or 17. Instead of KIT mutations, about 15% of all GIST have analogous mutations in the plateletderived growth factor receptor alpha (PDGFRA) gene; here they cluster in exon 18, more rarely in exon 12 or 14. They are preferentially detected in the stomach but hardly ever in other gastrointestinal locations. The tumors often show an epithelioid histomorphological phenotype[16,17].
Much attention is nowadays payed to the diagnostic marker DOG1, a protein with 8 transmembrane domains that constitutes a calcium-regulated chloride ion channel. DOG1 probably has even higher sensitivity for GIST than CD117. Moreover, the marker shows high sensitivity for CD117-negative GIST[18,19]. In non-GIST, on the other hand, DOG1 positivity has only been observed in a few isolated cases. GIST express CD34 in 70%-80% of the cases, whereas a KIT expression is found in more than 90% of cases. Immunohistochemical stains for CD117, DOG1 and CD34 are now routinely used in the identification and diagnosis of GIST (Figure 2). Antibodies against smooth muscle actin, desmin and S100 enable to distinguish GIST from leiomyomas or schwannomas.
Figure 2.
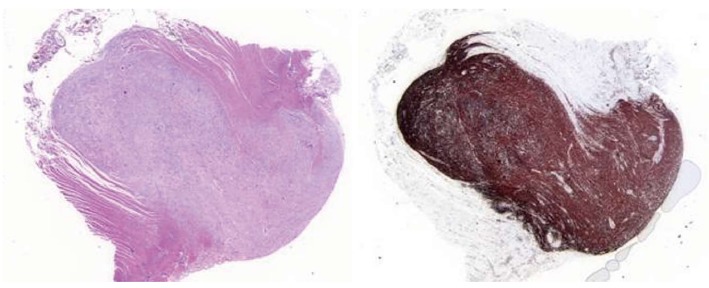
Histological images of an early gastrointestinal stromal tumors of the stomach. A: Gastric GIST of the muscularis propria displaying spindle cell type (HE stain); 2B: GIST of the muscularis propria displaying spindle cell type (CD 34 stain). Modified from reference [33]. GIST: Gastrointestinal stromal tumors.
According to Miettinen und Lasota, the postoperative prognosis of patients with gastric GIST can be predicted based on the following clinicopathological parameters: tumor location, tumor size and mitotic rate/5 mm2 (Table 1). The original population used 50 HPFs to evaluate this area but stated that with newer microscopes bearing larger field diameters an area of 5 mm² would be appropriate. Accordingly, the ESMO guidelines from 2012 recommend to evaluate 5 mm² instead of 50 HPFs[20-22]. Thus, tumors with a maximum diameter of 2 cm and low proliferative activity have a negligible risk of progression.
Table 1.
Risk of progression for gastric gastrointestinal stromal tumors according to Miettinen
| Tumor parameters |
Risk of tumor progression |
|
|
Mitosis rate |
Size |
|
| ≤ 5/5 mm2 | ≤ 2 cm | 0% |
| ≤ 5/5 mm2 | > 2-5 cm | 1.90% |
| ≤ 5/5 mm2 | > 5-10 cm | 3.60% |
| ≤ 5/5 mm2 | > 10 cm | 12% |
| > 5/5 mm2 | ≤ 2 cm | ND |
| > 5/5 mm2 | > 2-5 cm | 16% |
| > 5/5 mm2 | > 5-10 cm | 55% |
| > 5/5 mm2 | > 10 cm | 86% |
EARLY GIST (MICRO-GIST)
Early GIST of the stomach (< 1 cm) differ clinically and pathologically from clinically relevant tumors in that they have a markedly lower proliferation rate. They also occur more often as hypocellular lesions composed of spindle cells and frequently show marked sclerosis. Early gastric GIST (synonym: micro-GIST) exhibit distinctive molecular genetic characteristics: the incidence of KIT/PDGFRA mutations and particularly KIT exon 11 mutations is significantly lower in early than in clinically manifest GIST. There is a high frequency of unique mutations that have thus far not been found in clinically relevant GIST. A large Italian study identified five new mutations, three in KIT (p.Phe506Leu, p.Ser692Leu, p.Glu695Lys) and two in PDGFRA (p.Ser847X, p.Ser667Pro), as well as four double mutations[5]. These mutations apparently only cause low proliferative activity in GIST. There are also mutations consistent with clinically relevant GIST[23].
Prognosis of patients with early GIST of the stomach
Clinical progression of early gastric GIST (< 1 cm) has not yet been described in the world literature. Thus early gastric GIST generally show benign behavior irrespective of the mitotic rate and exhibit distinctive histopathological and molecular biological characteristics[5]. The GIST-specific prognosis of patients with early gastric GIST is excellent.
CLINICAL MANAGEMENT
Surgical resection of gastric GIST
Surgical R0 resection is the standard treatment for symptomatic gastric GIST and for those larger than 2 cm in diameter. An option in primary inoperable cases is neoadjuvant imatinib therapy with the aim of achieving secondary operability[20,24,25].
Drug therapy of gastric GIST
Drug therapy with a tyrosine kinase inhibitor is indicated in patients with distant metastases[20,25]. Patients with local disease undergo initial R0 resection followed by risk stratification based on tumor location, size, and mitotic activity[22]. A 3-year course of imatinib therapy is the current standard in patients with an intermediate or high risk of tumor relapse and the appropriate mutation analysis[26]. In a controlled phase-3 study, imatinib significantly prolonged survival in GIST with a high risk of progression[26]. Both the ESMO and NCCN guidelines recommend this type of therapy for GIST patients with a significant risk of relapse[20,25]. While evidencebased recommendations are available for the treatment of clinically manifest GIST, there are no uniform guidelines for clinical management of early gastric GIST. Rossi et al[5] recently reported that patients with early gastric GIST have an excellent prognosis irrespective of the mitotic rate. Epidemiological data also demonstrate the generally benign behavior of early GIST of the stomach. Rossi et al. coined the term “self-limiting tumorigenesis” to describe the tumor biology of early GIST of the stomach.
Surgical resection of early gastric GIST most likely is overtreatment in older people. The well-documented, generally benign behavior and the high prevalence of early gastric GIST in the elderly argue for a conservative management. Particularly in older patients, it is important to consider not only the hospital morbidity but also the low but not negligible perioperative mortality, which may amount to 1% or higher according to the published literature[27,28]. There are no clinical studies that have demonstrated any advantage (in quality-of-life or in survival) of surgery over endoscopic surveillance in patients with early (< 1 cm) gastric GIST[6].
ENDOSCOPIC SURVEILLANCE
Endoscopic surveillance should be performed in patients with early asymptomatic GIST of the stomach. Repeat endoscopic ultrasound at 12-mo intervals is generally recommended. If the size remains constant, the intervals can probably be extended in the elderly. Interestingly to note, rapid progression of a gastric GIST that had stayed stable at a size of 1.8 cm for 8 years has been reported[29].
If initial cytohistological assessment of early gastric GIST has not been performed or has not been conclusive and if there is strong clinical suspicion of early GIST, endoscopic ultrasound of the stomach should be repeated already after an interval of 2-3 mo. This short interval is not due to the (very low) probability of rapidly progressive GIST[30] but takes into account the (low) risk of a subepithelial lesion different from GIST. The correct evaluation of a subepithelial lesion by endoscopic ultrasound relies on an experienced team of endoscopists. Indeed the differential diagnosis of “subepithelial or submucosal lesions” of the stomach is complex and extensive[10,14]. The differential diagnosis has to include cysts, pseudocysts, varices, ectopic pancreatic tissue, leiomyomas, schwannomas, lipomas, lymphomas, gastric polyps, inflammatory fibroid polyps, submucosal metastases, protruding aneurysms, large lymph nodes, granular cell tumors and gastric carcinoids[31]. Even localized protrusion of the gallbladder, spleen or left liver lobe can appear as a submucosal lesion in conventional gastroscopy.
If the first repeat endoscopic ultrasound (2-3 mo after initial diagnosis) reveals no change in size of a small (< 1 cm) subepithelial or submucosal lesion, the surveillance interval can be extended to 12 mo. However, a lesion that becomes markedly larger after 2-3 mo requires a definitive (histological) diagnosis and therapy (such as surgical resection). In addition, a gastric GIST that increases in size during follow-up has to be considered for surgery[32] and be discussed on the tumor board.
Footnotes
P- Reviewer: Mubarak M S- Editor: Song XX L- Editor: A E- Editor: Zhang DN
References
- 1.Wardelmann E, Hohenberger P, Reichardt P, Merkelbach-Bruse S, Schildhaus HU, Büttner R. [Gastrointestinal stromal tumors of the stomach. Updates and differences compared to other locations] Pathologe. 2010;31:195–198. doi: 10.1007/s00292-009-1270-9. [DOI] [PubMed] [Google Scholar]
- 2.Nilsson B, Bümming P, Meis-Kindblom JM, Odén A, Dortok A, Gustavsson B, Sablinska K, Kindblom LG. Gastrointestinal stromal tumors: the incidence, prevalence, clinical course, and prognostication in the preimatinib mesylate era--a population-based study in western Sweden. Cancer. 2005;103:821–829. doi: 10.1002/cncr.20862. [DOI] [PubMed] [Google Scholar]
- 3.Agaimy A, Wünsch PH, Hofstaedter F, Blaszyk H, Rümmele P, Gaumann A, Dietmaier W, Hartmann A. Minute gastric sclerosing stromal tumors (GIST tumorlets) are common in adults and frequently show c-KIT mutations. Am J Surg Pathol. 2007;31:113–120. doi: 10.1097/01.pas.0000213307.05811.f0. [DOI] [PubMed] [Google Scholar]
- 4.Kawanowa K, Sakuma Y, Sakurai S, Hishima T, Iwasaki Y, Saito K, Hosoya Y, Nakajima T, Funata N. High incidence of microscopic gastrointestinal stromal tumors in the stomach. Hum Pathol. 2006;37:1527–1535. doi: 10.1016/j.humpath.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 5.Rossi S, Gasparotto D, Toffolatti L, Pastrello C, Gallina G, Marzotto A, Sartor C, Barbareschi M, Cantaloni C, Messerini L, et al. Molecular and clinicopathologic characterization of gastrointestinal stromal tumors (GISTs) of small size. Am J Surg Pathol. 2010;34:1480–1491. doi: 10.1097/PAS.0b013e3181ef7431. [DOI] [PubMed] [Google Scholar]
- 6.Bennett JJ, Rubino MS. Gastrointestinal stromal tumors of the stomach. Surg Oncol Clin N Am. 2012;21:21–33. doi: 10.1016/j.soc.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 7.Cantor MJ, Davila RE, Faigel DO. Yield of tissue sampling for subepithelial lesions evaluated by EUS: a comparison between forceps biopsies and endoscopic submucosal resection. Gastrointest Endosc. 2006;64:29–34. doi: 10.1016/j.gie.2006.02.027. [DOI] [PubMed] [Google Scholar]
- 8.Karaca C, Turner BG, Cizginer S, Forcione D, Brugge W. Accuracy of EUS in the evaluation of small gastric subepithelial lesions. Gastrointest Endosc. 2010;71:722–727. doi: 10.1016/j.gie.2009.10.019. [DOI] [PubMed] [Google Scholar]
- 9.He Z, Sun C, Wang J, Zheng Z, Yu Q, Wang T, Chen X, Liu W, Wang B. Efficacy and safety of endoscopic submucosal dissection in treating gastric subepithelial tumors originating in the muscularis propria layer: a single-center study of 144 cases. Scand J Gastroenterol. 2013;48:1466–1473. doi: 10.3109/00365521.2013.845796. [DOI] [PubMed] [Google Scholar]
- 10.Akahoshi K, Oya M. Gastrointestinal stromal tumor of the stomach: How to manage? World J Gastrointest Endosc. 2010;2:271–277. doi: 10.4253/wjge.v2.i8.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fernández-Esparrach G, Sendino O, Solé M, Pellisé M, Colomo L, Pardo A, Martínez-Pallí G, Argüello L, Bordas JM, Llach J, et al. Endoscopic ultrasound-guided fine-needle aspiration and trucut biopsy in the diagnosis of gastric stromal tumors: a randomized crossover study. Endoscopy. 2010;42:292–299. doi: 10.1055/s-0029-1244074. [DOI] [PubMed] [Google Scholar]
- 12.Hoda KM, Rodriguez SA, Faigel DO. EUS-guided sampling of suspected GI stromal tumors. Gastrointest Endosc. 2009;69:1218–1223. doi: 10.1016/j.gie.2008.09.045. [DOI] [PubMed] [Google Scholar]
- 13.Mekky MA, Yamao K, Sawaki A, Mizuno N, Hara K, Nafeh MA, Osman AM, Koshikawa T, Yatabe Y, Bhatia V. Diagnostic utility of EUS-guided FNA in patients with gastric submucosal tumors. Gastrointest Endosc. 2010;71:913–919. doi: 10.1016/j.gie.2009.11.044. [DOI] [PubMed] [Google Scholar]
- 14.Papanikolaou IS, Triantafyllou K, Kourikou A, Rösch T. Endoscopic ultrasonography for gastric submucosal lesions. World J Gastrointest Endosc. 2011;3:86–94. doi: 10.4253/wjge.v3.i5.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Suzuki T, Arai M, Matsumura T, Arai E, Hata S, Maruoka D, Tanaka T, Nakamoto S, Imazeki F, Yokosuka O. Factors Associated with Inadequate Tissue Yield in EUS-FNA for Gastric SMT. ISRN Gastroenterol. 2011;2011:619128. doi: 10.5402/2011/619128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pauls K, Merkelbach-Bruse S, Thal D, Büttner R, Wardelmann E. PDGFRalpha- and c-kit-mutated gastrointestinal stromal tumours (GISTs) are characterized by distinctive histological and immunohistochemical features. Histopathology. 2005;46:166–175. doi: 10.1111/j.1365-2559.2005.02061.x. [DOI] [PubMed] [Google Scholar]
- 17.Wardelmann E, Hrychyk A, Merkelbach-Bruse S, Pauls K, Goldstein J, Hohenberger P, Losen I, Manegold C, Büttner R, Pietsch T. Association of platelet-derived growth factor receptor alpha mutations with gastric primary site and epithelioid or mixed cell morphology in gastrointestinal stromal tumors. J Mol Diagn. 2004;6:197–204. doi: 10.1016/s1525-1578(10)60510-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Espinosa I, Lee CH, Kim MK, Rouse BT, Subramanian S, Montgomery K, Varma S, Corless CL, Heinrich MC, Smith KS, et al. A novel monoclonal antibody against DOG1 is a sensitive and specific marker for gastrointestinal stromal tumors. Am J Surg Pathol. 2008;32:210–218. doi: 10.1097/PAS.0b013e3181238cec. [DOI] [PubMed] [Google Scholar]
- 19.Liegl B, Hornick JL, Corless CL, Fletcher CD. Monoclonal antibody DOG1.1 shows higher sensitivity than KIT in the diagnosis of gastrointestinal stromal tumors, including unusual subtypes. Am J Surg Pathol. 2009;33:437–446. doi: 10.1097/PAS.0b013e318186b158. [DOI] [PubMed] [Google Scholar]
- 20.ESMO / European Sarcoma Network Working Group. Gastrointestinal stromal tumors: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23 Suppl 7:vii49–vii55. doi: 10.1093/annonc/mds252. [DOI] [PubMed] [Google Scholar]
- 21.Miettinen M, Lasota J. Histopathology of gastrointestinal stromal tumor. J Surg Oncol. 2011;104:865–873. doi: 10.1002/jso.21945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miettinen M, Sobin LH, Lasota J. Gastrointestinal stromal tumors of the stomach: a clinicopathologic, immunohistochemical, and molecular genetic study of 1765 cases with long-term follow-up. Am J Surg Pathol. 2005;29:52–68. doi: 10.1097/01.pas.0000146010.92933.de. [DOI] [PubMed] [Google Scholar]
- 23.Mikami T, Nemoto Y, Numata Y, Hana K, Nakada N, Ichinoe M, Murakumo Y, Okayasu I. Small gastrointestinal stromal tumor in the stomach: identification of precursor for clinical gastrointestinal stromal tumor using c-kit and α-smooth muscle actin expression. Hum Pathol. 2013;44:2628–2635. doi: 10.1016/j.humpath.2013.07.020. [DOI] [PubMed] [Google Scholar]
- 24.Hohenberger P, Eisenberg B. Role of surgery combined with kinase inhibition in the management of gastrointestinal stromal tumor (GIST) Ann Surg Oncol. 2010;17:2585–2600. doi: 10.1245/s10434-010-1053-9. [DOI] [PubMed] [Google Scholar]
- 25.von Mehren M, Benjamin RS, Bui MM, Casper ES, Conrad EU, DeLaney TF, Ganjoo KN, George S, Gonzalez R, Heslin MJ, et al. Soft tissue sarcoma, version 2.2012: featured updates to the NCCN guidelines. J Natl Compr Canc Netw. 2012;10:951–960. doi: 10.6004/jnccn.2012.0099. [DOI] [PubMed] [Google Scholar]
- 26.Joensuu H, Eriksson M, Hartmann H, Sundby Hall K, Schutte J, Reichardt A, Schlemmer M, Wardelmann E, Ramadori G, Al-Batran S, et al. Twelve versus 36 months of adjuvant imatinib (IM) as treatment of operable GIST with a high risk of recurrence: Final results of a randomized trial (SSGXVIII/AIO) J Clin Oncol. 2011:29 (suppl): Abstr LBA1. [Google Scholar]
- 27.Naguib SF, Zaghloul AS, El Marakby H. Gastrointestinal stromal tumors (GIST) of the stomach: retrospective experience with surgical resection at the National Cancer Institute. J Egypt Natl Canc Inst. 2008;20:80–89. [PubMed] [Google Scholar]
- 28.Sexton JA, Pierce RA, Halpin VJ, Eagon JC, Hawkins WG, Linehan DC, Brunt LM, Frisella MM, Matthews BD. Laparoscopic gastric resection for gastrointestinal stromal tumors. Surg Endosc. 2008;22:2583–2587. doi: 10.1007/s00464-008-9807-1. [DOI] [PubMed] [Google Scholar]
- 29.Nakajima T, Ushijima T, Kihara A, Murata K, Sugiyama T, Tsuneyama K, Imura J, Fukushima J, Horiuchi H. A gastrointestinal stromal tumor of the stomach demonstrating a stepwise progression from low- to high-grade malignancy. Case Rep Gastrointest Med. 2012;2012:606832. doi: 10.1155/2012/606832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tanaka J, Oshima T, Hori K, Tomita T, Kim Y, Watari J, Oh K, Hirota S, Matsumoto T, Miwa H. Small gastrointestinal stromal tumor of the stomach showing rapid growth and early metastasis to the liver. Dig Endosc. 2010;22:354–356. doi: 10.1111/j.1443-1661.2010.01032.x. [DOI] [PubMed] [Google Scholar]
- 31.Scherübl H, Cadiot G, Jensen RT, Rösch T, Stölzel U, Klöppel G. Neuroendocrine tumors of the stomach (gastric carcinoids) are on the rise: small tumors, small problems? Endoscopy. 2010;42:664–671. doi: 10.1055/s-0030-1255564. [DOI] [PubMed] [Google Scholar]
- 32.Miyazaki Y, Nakajima K, Kurokawa Y, Takahashi T, Takiguchi S, Miyata H, Yamasaki M, Hirota S, Nishida T, Mori M, et al. Clinical significance of surgery for gastric submucosal tumours with size enlargement during watchful waiting period. Eur J Cancer. 2013;49:2681–2688. doi: 10.1016/j.ejca.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 33.Scherübl H, Faiss S, Jahn HU, Knoefel WT, Liehr RM, Schwertner C, Steinberg J, Stölzel U, Weinke T, Zimmer T, et al. [Early asymptomatic GIST of the stomach] Dtsch Med Wochenschr. 2012;137:1650–1653. doi: 10.1055/s-0032-1305210. [DOI] [PubMed] [Google Scholar]


