Abstract
Gastrointestinal stromal tumors (GISTs) are the most frequent gastrointestinal tumors of mesodermal origin. Gastric GISTs represent approximately 70% of all gastrointestinal GISTs. The only curative option is surgical resection. Many surgical groups have shown good results with the laparoscopic approach. There have not been any randomized controlled trials comparing the open vs laparoscopic approach, and all recommendations have been based on observational studies. The experience obtained from gastric laparoscopic surgery during recent decades and the development of specific devices have allowed the treatment of most gastric GISTs through the laparoscopic approach.
Keywords: Gastrointestinal stromal tumors, Laparoscopy, Surgery, Stomach, Gastrectomy
Core tip: Gastrointestinal stromal tumors (GISTs) are the most frequent gastrointestinal tumors of mesodermal origin. Gastric GISTs represent approximately 70% of all gastrointestinal GISTs. The only curative option is surgical resection. Many surgical groups have shown good results with the laparoscopic approach. There have not been any randomized controlled trials comparing the open vs laparoscopic approach, and all recommendations have been based on observational studies. The experience obtained from gastric laparoscopic surgery during recent decades and the development of specific devices have allowed the treatment of most gastric GISTs through the laparoscopic approach.
INTRODUCTION
Gastrointestinal stromal tumors (GISTs) are the most frequent gastrointestinal tumors of mesodermal origin[1], and gastric GISTs represent approximately 70% of all gastrointestinal GISTs[2]. These tumors are derived from the interstitial cells of Cajal[3], and have been shown to harbor gain of function mutations in the cell-surface KIT receptor in approximately 90% or in the platelet-derived growth factor receptor α (PDGFRA) in 8%[4].
Most tumors are limited to the primary organ, and less than 2% of tumors present lymph node metastasis. GISTs can also metastasize to the peritoneum and infrequently present hematogenous metastasis to other intra-abdominal viscera, lung, pleura, bone and brain[5].
Most patients are asymptomatic; the tumors are usually found as an incidental finding in 4%-39% of cases[6-11]. In most surgical series, the most frequent symptoms are gastrointestinal bleeding (14%-68%), abdominal pain (16.1%-45%), abdominal mass (3.3%-21%), early satiety (36%), anemia (19.4%-77%), weight loss (11%), bowel obstruction (3.6%), liver metastasis (3.6%), dyspeptic symptoms (9.7%) and dysphagia (9%)[6-10]. There is a clear relationship between tumor size and symptoms, smaller tumores are generally asymptomatic[4].
The diagnosis is usually made by endoscopy or abdominal imaging. During endoscopy, it is possible to see gastric lumen narrowing associated with normal protruded mucosa, although in larger tumors, the mucosa can show ulcers due to local ischemia[12,13]. The ideal method for diagnosis is endoscopic ultrasonography (EUS), which can define the size, vascular pattern and form of the tumor and differentiate between an extra-luminal compression and a submucous growth. GISTs are hypoechoic tumors located at the fourth layer, although some reports have shown tumors located at the third layer. However, the imaging of these tumors is not sensitive (43%), which necessitates histologic evaluation. EUS also helps guide fine needle aspiration biopsies, showing better performance than biopsies under normal endoscopy[12]. The sensitivity of FNAB guided by EUS increases by 10% if a pathologist makes an immediate examination of the adequacy of the sample[13]. In some series, preoperative diagnosis was only possible 52.3%[7].
Computed tomography (CT) is necessary for preoperative stratification. CT can usually show intra- or extraluminal tumors with different morphologic patterns according to size. Larger tumors can show irregular margins and heterogeneous internal density, and if the diameter is larger than 6 cm, the tumors are usually accompanied by central necrosis. Magnetic resonance imaging (MRI) is recommended in cases of simultaneous liver metastasis because of the possibility of conducting a combined resection. PET-CT can be useful in patients with undetermined findings on CT or MRI[14]. However, there is not a good correlation between imaging findings and malignancy[15].
A differential diagnosis with other submucous tumors such as leiomyoma, leiomyosarcoma, schwannoma, granular cell tumors, heterotopic pancreatic tissue, lipoma, neurofibroma, Kaposi tumors and non-functional adrenal tumors should be performed[16,17]. Immunohistochemistry for GIST detection is very useful and shows positivity for CD117 (95% of GISTs)[16]. Only 2% are usually related to PDGFRA mutations[16,18]. Other helpful tests are CD34 that is positive in 70% of the cases and vimentin[16].
SURGICAL TREATMENT
The only curative option is surgical resection, which can be offered to patients with good functional status and non-metastatic resectable tumors, although in some cases, a metastasis resection surgery can be performed in association with resection of the primary tumor[19]. Surgical principles for resection include total extracapsular resection, avoiding tumor fracture or bleeding, which are associated with recurrence and peritoneal sarcomatosis[20]. There are no recommended margins, because microscopic margins status doesn´t correlate with survival as does the mitotic count and tumor size. Wedge resection is a good option for tumors located in the anterior wall or greater curve. For tumors located at the antrum wedge resection can produce a stenosis, so formal gastric resections are favored. Wider margins have not shown any oncologic advantage[21], and lymph node dissection has not been indicated[22]. The National Comprehensive Cancer Network (NCCN) guidelines suggest that tumors smaller than 1 cm that do not fulfill high risk endosonographic criteria (irregular borders, cystic spaces, ulcer of echogenic heterogeneous focus) can be observed during endoscopic follow-up at each 6-12-mo interval[23]. Most larger tumors need adjuvant treatment with imatinib mesylate to avoid recurrence[2].
LAPAROSCOPIC TREATMENT
Open surgical resection was the standard of treatment until two decades ago. Many surgical groups have shown good results with the laparoscopic approach. Although NCCN guidelines suggest that laparoscopic resection is indicated in tumors less than 2 cm, many surgeons have reported a safe excision of tumors > 5 cm and other up to 10 cm[24-26]. Lukaszczry and Pretez in 1992 were the first to report a successful laparoscopic resection of a gastric GIST[27].
The laparoscopic techniques can be divided into different subtypes: transgastric resections, endoscopy-assisted laparoscopic resections, wedge resections, partial gastrectomy and hand-assisted laparoscopic resections[24]. The surgical approach depends on tumor size and location (Figure 1). Privette et al[25] proposed a classification system based on tumor location as a guideline to choose the best surgical approach. Trocars and operating tables are organized in a similar manner to any other hiatus procedures, with the surgeon located between the legs. A 12-15 mmHg pneumoperitoneum is established, and a 30° camera and a liver retractor are useful. Before resection, it is mandatory to review the abdominal cavity to rule out peritoneum or liver metastasis. If the surgeons suspect solid organ metastasis, the use of intraoperative ultrasound with biopsy can help in the operative decision. Assistance by endoscopy during the surgical procedure is useful for locating the tumor and guiding resection, and staining with ink could help delineate the resection margins.
Figure 1.
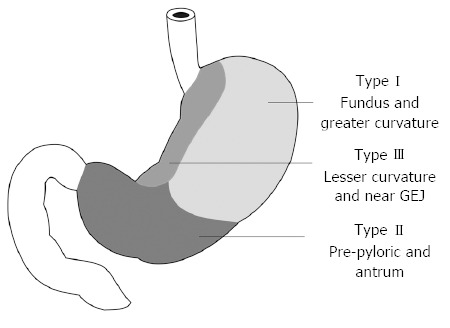
Surgical approach according to gastrointestinal stromal tumor localization.
Tumors located at the fundus and at the anterior and posterior walls can be resected by partial gastrectomy or wedge resection. In cases of small tumors, the greater curve is mobilized, ligating the gastroepiploic vessels with an ultrasonic scalpel or a thermal device. The gastric wall is elevated with sutures placed in the seromuscular layer around the tumor to obtain a complete resection with a linear mechanical stapler, guaranteeing macroscopic margins. In cases of larger tumors, the gastric wall is directly opened and the tumor is resected, maintaining a free margin with a late direct closure using a continuous suture. In cases where tumors are located in the posterior wall, an anterior gastrotomy is made exactly above the tumor, usually assisted by endoscopy. The tumor is resected by the techniques described, with a late closure of the anterior wall with a continuous suture[11,26].
For tumors located at the antrum or at the prepyloric area, partial gastrectomy is recommended due to the high risk of stenosis and delayed stomach emptying when wedge resections are used. In these cases, the greater and lesser curves are dissected to obtain retrogastric access. The duodenum is sectioned just distal to the pylorus with a linear mechanical stapler, and the proximal section is also made with a mechanical stapler; this is usually assisted by endoscopy. Finally, a Roux-en-Y anastomosis is made[25].
Tumors located at the esophagogastric junction are infrequent and represent less than 5% of all tumors. Some authors have recommended enucleation of these tumors based on the high morbidity (6%-24%) and mortality (0%-1.5%) with classical resections and due to the lack of advantage in prognosis and survival[28]. However, the best surgical approach is still debated[29]. The enucleation is made through an anterior gastrotomy, and in these cases, a submucous infiltration with epinephrine is recommended to avoid bleeding and perforation. The use of devices such as an ultrasonic scalpel or an electrocautery has been recommended[10,28].
Some authors have varied the surgical technique using transgastric trocars and endoscopy-assisted insufflation. In these cases, smaller tumors can even be extracted by the mouth using endoscopy[25]. For larger tumors, other authors have suggested a hand-assisted technique because it allows for better exploration and easier handling and dissection of the tumor[12,13]. Others have also shown good results with the single-port approach or dissections without insufflation[8]. In all cases, the use of a bag is recommended for the extraction of the tumor to avoid recurrence and metastasis at the port insertion sites[30,31].
Until now, there have not been any randomized controlled trials comparing the open vs laparoscopic approach, and all recommendations have been based on observational studies. Actual recommendations are based on outcomes related to surgical technique (intact specimen, free margins) and prognosis (operative complications, recurrence, cancer free survival)[32] reported from these observational studies. Tables 1 and 2 show the results of comparative and non-comparative published series.
Table 1.
Non-comparative series of laparoscopic resection of gastric gastrointestinal stromal tumor
| Ref. | n | Age (yr) | Tumor size | Tumor localization | Type of surgery | OR time (min) | Notes | Complications/ conversions | Follow-up (mo) |
| Privette et al[25] | 12 | 60.5 | 5.2 cm PG 4.6 cm TransG 5.5 cm DG | 5 Fundus or greater curvature 3 Prepyloric or antral 5 Lesser curvature | 5 PG × Lap 3 DG × Lap 5 TransG × Lap | PG 180 (122-262) DG: 322 (256-340) TransG: 236 (202-265) | 9/12 GIST 1 Schwannoma 2 Leiomiomas LOS: GP: 3.4 GD: 8.3 GT: 3.3 | 16.6% complication 1 Enterotomy 1 GI Bleeding No conversions | Only specified for 5 pts |
| Sexton et al[32] | 61 | 59.1 ± 19 | 3.8 ± 1.8 AR: 229.7 NAR 140.9 | Fundus 19 Antrum 18 Body 17 GE junction 7 Pylorus 2 | PG 52 DG 4 TotGas 3 TransG 3 | 151.9 ± 67.3 | LOS: 3.9 ±2 LOS AR: 3.9, NAR: 4.1 | 16.4% complication No conversions 1 POP death | 15 (0-103) 3 recurrences |
| Berindoague et al[9] | 22 | 66.7 | 5.6 (2.5-12.5) | Upper third 6 Middle third 7 Lower third 10 | GP 13 1 LAP-HA TotGas 1 LAP TotGast 1 LAP-HA GD 1 TransG | NR | 18/22 GIST 1 Adenomyoma 1 Hamartoma 1 Plasmocytoma 1 Parasitic Tumor (anisakis) LOS 6 (4-32) | 18.2% complication 3 Delayed gastric emptying 1 Intestinal Obstruction 2 Conversions (9.1%) | 32 m (1-72) 1 recurrence |
| De Vogelaere et al[24] | 31 | 63.8 | 4.4 (0.4-11) | Anterior gastric wall 23 Others not specified | 31 PG | 99 | LOS 8.5 | 3.2% Complication 1 POP Bleeding | 56.3 No recurrences |
| Hwang et al[10] | 63 | 52.8 | 3.5 GE Junction 3.4 Prepyloric Size of other tumor not specified | 7 GE junction Upper third 22 Middle third 11 Lower third 19 4 Prepyloric | 3 DG 37 PG 23 TransG (5 Enucleations) | 86.1 ± 43.7 | LOS 5.3 ± 1 1.8 41 GIST 8 Leiomyoma 4 Carcinoids 1 Liposarcoma 6 Heterotopic Pancreas 2 Hyperplastic Polyps 1 Parasitic Infection | 4.7% Complication 1 Staple line bleeding 1 SSI 1 Staple line dehiscence | 14.9 (2-42) No recurrences |
| Novitsky et al[26] | 50 | 60 ± 13 | 4.4 ± 2.0 cm | GE Junction 8 Cardias 9 Anterior Wall 10 Posterior Wall 4 Greater Curvature 6 Lesser Curvature 3 Antrum 4 Prepyloric 6 | TotGas 1 DG 2 PG 40 LAP/END 4 LAP-HA 3 | 135 ± 56 | LOS 3.8 ± 1.6 | 8% 4 Minor complications | 36 (4-84) 4 recurrences |
| Lai et al[2] | 28 | 56.9 ± 12.4 | 3.4 ± 1.6 | Upper third 13 Middle third 8 Lower third 7 | 28 PG | 189.6 ± 79.5 Stapled 194.3 ± 50.5 Hand-Sewn | LOS 6.7 ± 1.8 | 3.5% conversion | 43.3 ± 23.5 No recurrences |
| Choi et al[36] | 23 | 59.7 ± 8.3 | 4.2 ±2.1 | Upper third 13 Middle third 5 Lower third 5 | 23 PG | 104.3 | LOS 5.2 ± 2.3 | 4.3% complication 1 Delayed gastric emptying No conversions | 61 (7-98) |
| Nguyen et al[22] | 28 | 65 | 4.6 (0.4-11.5) | LAP PG 22 Subtotal Gastrectomy 3 OS (Converted) : TotGas 1 Intraluminal excision 1 1 Not specified | 23 GP × LAP 3 GD × LAP 1 GT × LAP 1 TotGas × CA (converted) | 143 (46-336) This includes Small Bowel GIST resections. No data only on gastric resections | LOS 4 (1-50 d) | 9% complications 11% 3 conversions Mortality 1 POP death This includes Small Bowel GIST resections. No data only on gastric resections | NS |
| Huguet et al[37] | 33 | 68 | 3.9 (0.5-10.5), | GE Junction 5 Body 24 Antrum 4 | PG 29 LAP-HA PG 4 | 124 (30-253) | LOS 3 (1-40) | 9% complications 2 POP Bleeding 1 SSI 6% conversions | 13 (3-64) No recurrences |
| Ronellenfitsch et al[38] | 17 | 56 (43-79) | 2.9 (0.8-6) | 11 Not specified 6 Antrum | 17 PG | 130 (80-201) | LOS 7 (5-95) | 11.8% Complications: Staple leaks 5% conversion (peritoneal adhesions) | 18 (1-53) No recurrences |
| Tagaya et al[39] | 15 | 65.3 (52-75 years) | TransG 2.9 (1.7-6.5) GP 3.9 (1.2-8) | TransG: Upper third 4 Middle third 1 Lower third 1 PG: Greater curvature 2 Lesser curvature 1 Anterior wall 2 Middle third Ant wall 1 Middle Third Post wall 1 | TransG 8 PG 7 | TransG:168 (132-211) PG: 121 (60-190) | LOS TransG: 8.8 ( 7-12) LOS PG: 9.6 (7-14) | No complications | After final Pathology only 9 tumors were GIST TransG 18-73 PG: 6-122 No recurrences |
GLA: Gasless laparoscopy-assisted; PG: Wedge Resection or Partial Gastrectomy; DG: Distal Gastrectomy; TransG: Transgastric Gastrectomies; TotGas: Total Gastrectomy; OS: Open surgery; AR: Anatomic resections; NAR: Non-anatomic resections; LOS: Length of stay; NS: Not specified; LAP/END: Laparoendoscopic resection; LAP-HA: Laparoscopic hand-assisted; RG: Remnant Gastrectomy; Prox Gas: Proximal Gastrectomy; SSI: Surgical site infection.
Table 2.
Comparative series of laparoscopic resection of gastric gastrointestinal stromal tumor
| Ref. | n | Age | Tumor size | Tumor localization | Type of surgery | OR time (min) | Notes | Complications/ conversions | Follow-up (mo) |
| Wu et al[8] | 28 | 61.6 GLA 60.7 CA | 2.6 ± 1 1.8 GLA 2.5 ± 1.0 CA | Anterior fundus: 5 GLA 5 CA Posterior fundus: 6 GLA 2 CA Anterior body: 3 GLA 3 CA Posterior Body: 1 GLA 3 CA | 15 GLA 13 OS All were Wedge Resections | GLA 129 ± 36.1 CA 110.8 ± 38.1 | GLA Less POP Pain during the first 3 d Earlier oral intake Less LOS 5.8 vs 7.2 días | 7.1% complication 1 OS Ileus 1 Enterotomy during GLA corrected during LAP | NR |
| Catena et al[7] | 21 | 50.1 | 4.5 ± 2.0 | Body 16 Antrum 4 Fundus 1 | 21 PG | 151 ± 56 | LOS 4.8 ± 1.6 | No intraoperative complications | 35 (5-58) |
| 25 | 54.6 | 6.2 ± 1.9 | Body 17 Antrum 6 Fundus 2 | 25 OS (PG) | 134 ± 33 | LOS 7.1 ± 1.2 | No differences in complications | 91 (80-136) 1 recurrence | |
| Melstrom et al[31] | 46 | 62 Lap | OS 6.39 82.1-10) | Lap: Upper third 6 Middle third 10 NS 1 OS: Upper third 6 Lower third 22 NS 1 | 17 PG 24 PG × OS 4 DG × OS 1 TotGas × OS | Lap 135 OS 157 | LOS: OS 6.25 LAP 2.68 I | Complications OS: 13.8% LAP: 11.8% 6% conversion | OS 59 4 recurrences LAP 32 No Recurrences |
| 17 LAP | 60 OS | LAP 4.27 (1.5-9.1) | |||||||
| 29 OS | |||||||||
| De Vogelaere et al[11] | 53 | Total 5.9 | LAP : 2.7% 1 Pulmonary | Lap 83 | |||||
| 37 LAP | LAP 63.7 ± 15.4 | LAP 5.6 | Not specified | Not specified | LAP 48.5 ± 16 | LOS Lap 7 | Embolism | No Recurrences LAP | |
| 16 OS | OS 63.7 ± 10.7 | OS 7.5 | Not specified | Not specified | OS 155 ± 48.1 | LOS OS 14 | OS 18.7% complications: Pneumonia 1 Anastomotic Ulcer 1 Fistula 1 | OS 71 6 recurrences CA | |
| Karakousis et al[40] | 80 | 68 | OS 4.3 (2-9) | OS : Fundus 7 | OS 39 PG 1 DG | OS 89 LAP 96 | LOS: LAP 4 OS 7 | Complications OS 25% LAP 14% 32.5% Conversions | LAP 28 (0.3-70 m) Recurrences 1 LAP OS 43 (0.1-139) Recurrences 1 OS |
| OS 40 | LAP 3.6 (0-7-7.8) | Body/antrum 32 Pylorus 1 Lesser curvature 12 | LAP 40 PG | ||||||
| LAP 40 | LAP: Fundus 3 Body/antrum 37 Pylorus 0 Lesser curvature 10 | ||||||||
| Kim et al[41] | 104 LAP 80 OS 24 | 59.8 ± 10.5 | 5.1 ± 3.3 | Upper third 61 Middle third 24 Lower third 19 | Technique according to procedures was NS 99 PG 5 TotGas | LAP 91.1 ± 57 CA 165.8 ± 75.6 | LOS LAP 4.6 ± 2.3 CA 9.8 ± 4.1 | 1% Complications 1 Delayed Gastric Emptying | 49.3 (8.4-164.4) Recurrences 5 No Difference in recurrences between OS and LAP |
| Silberhummer et al[21] | 63 OS 41 LAP 22 | 62.3 ± 14.4 | CA 5.8 ± 4.0 LAP 3.5 ±1.4 | Body 29 Antrum 18 Fundus 10 GE Junction 6 | OS: PG 32 DG 5 RG 4 LAP 19 Tumorectomy 3 PG | 135 ± 56 | LOS LAP 7.8 (± 3.1) LOS CA 12.8 ± 5.0 | 4.7% complications: 1 Gastrocutaneous Fistula 1 Catheter Sepsis 1 POP Ileus LAP: 18.2% conversions | 37 ± 27.9 Recurrences in 4 (7%) |
| Nishimura et al[42] | LAP 39 | 62 | LAP 3.8 (0.8-7.3) | LAP: Upper third 19 Middle third 16 Lower third 4 | LAP GP: 12 LAP-HA 17 TransG 10 | LAP: 136 min OS: 115 min | NR | No Complications Conversion Rate 2.6% | LAP: 18.9 (2.6-96.4) Recurrences 4 LAP |
| OS 28 | OS: 4.2 (2.0-7.0) | OS Upper third 11 Middle third 11 Lower third 6 | OS PG: 19 Prox Gas: 5 TotGas: 3 DG:1 | OS: 31.2 (4.4-121.9) 1 Recurrence OS | |||||
| Otani et al[43] | 60 OS 22 LAP 38 | 59 (32-86) | 4,25 (1.8-15.0) | Upper third 36 Middle third 20 Lower third 4 | LAP: PG: 35 LAP-HA: LAP-HA PG 2 LAP-HA DG 1 OS: PG 11 ProxGas 9 DG 2 | LAP 141 LAP-HA 188 CA 197 | LOS LAP 7.2 vs 13.7 CA | 3.3% complications: 1 Gastric Stenosis 1 Anastomotic Leak | 53 mo 2 Recurrences |
GLA: Gasless laparoscopy-assisted; PG: Wedge resection or partial gastrectomy; DG: Distal gastrectomy; TransG: Transgastric gastrectomies; TotGas: Total gastrectomy; OS: Open surgery; AR: Anatomic resections; NAR: Non-anatomic resections; LOS: Length of stay; NS: Not specified; LAP/END: Laparoendoscopic resection; LAP-HA: Laparoscopic hand-assisted; RG: Remnant gastrectomy; Prox Gas: Proximal gastrectomy; SSI: Surgical site infection.
Recently, Koh et al[33] published a systematic review of eleven observational studies comparing laparoscopic vs open resection with evaluation of short and long term outcomes. In their study, which included 381 patients in the laparoscopic group and 384 patients in the open group, the laparoscopic approach showed a lower frequency of minor complications (OR = 0.517; 95%CI: 0.277-0.965), lower length of stay [mean difference -3.421 d (-4.737 to -2.104)], shorter time to the initiation of oral diet [mean difference -1.887 d (-2.785 to -0.989)] and lower intraoperative bleeding [mean difference -86.508 mL (-141.184 to -31.831 mL)]. They could not find any statistically significant differences in reoperation rate, operative time, positive margins, local recurrence, cancer free survival and overall survival. However, comparisons showed that most high risk tumors were treated with open gastrectomy, introducing a selection bias.
The rate of conversion to open surgery is 0%-31%[11], and this cannot be considered a complication but rather an intraoperative decision to obtain better tumor control when the surgeon is faced with adverse intraoperative conditions.
Follow up
Follow-up is mandatory in all patients, even in the absence of malignancy. Patients should be reviewed every 3-6 mo during the first 5 years. An annual endoscopy and CT are recommended to rule out local recurrence[20]. The survival rate of patients with early tumors is greater than 90%[34]. A size larger than 10 cm, a high mitotic rate and intraoperative rupture are risk factors for recurrence[35].
CONCLUSION
The experience obtained from gastric laparoscopic surgery during recent decades and the development of specific devices have allowed the treatment of most gastric GISTs through the laparoscopic approach. As with all surgical techniques, the laparoscopic approach must be applied in select patients with particular characteristics based on functional status, tumor size, location and surgeons’ experience. The case series presented in this review support laparoscopic resection as a safe and effective alternative, with similar rates of complications, but with lower pain and an early recovery. It is important to realize that tumor size by itself is not an adequate factor to contraindicate the laparoscopic approach and that other factors should be considered in the decision.
Footnotes
P- Reviewers: Mello ELR, Nezhat FR, Rodrigo L S- Editor: Song XX L- Editor: A E- Editor: Zhang DN
References
- 1.Raut CP, Morgan JA, Ashley SW. Current issues in gastrointestinal stromal tumors: incidence, molecular biology, and contemporary treatment of localized and advanced disease. Curr Opin Gastroenterol. 2007;23:149–158. doi: 10.1097/MOG.0b013e32802086d0. [DOI] [PubMed] [Google Scholar]
- 2.Lai IR, Lee WJ, Yu SC. Minimally invasive surgery for gastric stromal cell tumors: intermediate follow-up results. J Gastrointest Surg. 2006;10:563–566. doi: 10.1016/j.gassur.2005.08.028. [DOI] [PubMed] [Google Scholar]
- 3.Hirota S, Isozaki K, Moriyama Y, Hashimoto K, Nishida T, Ishiguro S, Kawano K, Hanada M, Kurata A, Takeda M, et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998;279:577–580. doi: 10.1126/science.279.5350.577. [DOI] [PubMed] [Google Scholar]
- 4.Liegl-Atzwanger B, Fletcher JA, Fletcher CD. Gastrointestinal stromal tumors. Virchows Arch. 2010;456:111–127. doi: 10.1007/s00428-010-0891-y. [DOI] [PubMed] [Google Scholar]
- 5.Vassos N, Agaimy A, Hohenberger W, Croner RS. Extraabdominal lymph node metastasis in gastrointestinal stromal tumors (GIST) J Gastrointest Surg. 2011;15:1232–1236. doi: 10.1007/s11605-011-1464-3. [DOI] [PubMed] [Google Scholar]
- 6.Wu Y, Zhu X, Ding Y. Diagnosis and treatment of gastrointestinal stromal tumors of the stomach: report of 28 cases. Ann Clin Lab Sci. 2007;37:15–21. [PubMed] [Google Scholar]
- 7.Catena F, Di Battista M, Fusaroli P, Ansaloni L, Di Scioscio V, Santini D, Pantaleo M, Biasco G, Caletti G, Pinna A. Laparoscopic treatment of gastric GIST: report of 21 cases and literature’s review. J Gastrointest Surg. 2008;12:561–568. doi: 10.1007/s11605-007-0416-4. [DOI] [PubMed] [Google Scholar]
- 8.Wu JM, Yang CY, Wang MY, Wu MH, Lin MT. Gasless laparoscopy-assisted versus open resection for gastrointestinal stromal tumors of the upper stomach: preliminary results. J Laparoendosc Adv Surg Tech A. 2010;20:725–729. doi: 10.1089/lap.2010.0231. [DOI] [PubMed] [Google Scholar]
- 9.Berindoague R, Targarona EM, Feliu X, Artigas V, Balagué C, Aldeano A, Lahoud A, Navines J, Fernandez-Sallent E, Trias M. Laparoscopic resection of clinically suspected gastric stromal tumors. Surg Innov. 2006;13:231–237. doi: 10.1177/1553350606295960. [DOI] [PubMed] [Google Scholar]
- 10.Hwang SH, Park do J, Kim YH, Lee KH, Lee HS, Kim HH, Lee HJ, Yang HK, Lee KU. Laparoscopic surgery for submucosal tumors located at the esophagogastric junction and the prepylorus. Surg Endosc. 2009;23:1980–1987. doi: 10.1007/s00464-008-9955-3. [DOI] [PubMed] [Google Scholar]
- 11.De Vogelaere K, Hoorens A, Haentjens P, Delvaux G. Laparoscopic versus open resection of gastrointestinal stromal tumors of the stomach. Surg Endosc. 2013;27:1546–1554. doi: 10.1007/s00464-012-2622-8. [DOI] [PubMed] [Google Scholar]
- 12.Ponsaing LG, Kiss K, Loft A, Jensen LI, Hansen MB. Diagnostic procedures for submucosal tumors in the gastrointestinal tract. World J Gastroenterol. 2007;13:3301–3310. doi: 10.3748/wjg.v13.i24.3301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sakamoto H, Kitano M, Kudo M. Diagnosis of subepithelial tumors in the upper gastrointestinal tract by endoscopic ultrasonography. World J Radiol. 2010;2:289–297. doi: 10.4329/wjr.v2.i8.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kalkmann J, Zeile M, Antoch G, Berger F, Diederich S, Dinter D, Fink C, Janka R, Stattaus J. Consensus report on the radiological management of patients with gastrointestinal stromal tumours (GIST): recommendations of the German GIST Imaging Working Group. Cancer Imaging. 2012;12:126–135. doi: 10.1102/1470-7330.2012.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chourmouzi D, Sinakos E, Papalavrentios L, Akriviadis E, Drevelegas A. Gastrointestinal stromal tumors: a pictorial review. J Gastrointestin Liver Dis. 2009;18:379–383. [PubMed] [Google Scholar]
- 16.Ponsaing LG, Kiss K, Hansen MB. Classification of submucosal tumors in the gastrointestinal tract. World J Gastroenterol. 2007;13:3311–3315. doi: 10.3748/wjg.v13.i24.3311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chung SD, Chueh JS, Yu HJ. Laparoscopic resection of gastric gastrointestinal stromal tumors presenting as left adrenal tumors. World J Gastroenterol. 2012;18:96–98. doi: 10.3748/wjg.v18.i1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miettinen M, Sobin LH, Lasota J. Gastrointestinal stromal tumors of the stomach: a clinicopathologic, immunohistochemical, and molecular genetic study of 1765 cases with long-term follow-up. Am J Surg Pathol. 2005;29:52–68. doi: 10.1097/01.pas.0000146010.92933.de. [DOI] [PubMed] [Google Scholar]
- 19.DeMatteo RP, Lewis JJ, Leung D, Mudan SS, Woodruff JM, Brennan MF. Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg. 2000;231:51–58. doi: 10.1097/00000658-200001000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roggin KK, Posner MC. Modern treatment of gastric gastrointestinal stromal tumors. World J Gastroenterol. 2012;18:6720–6728. doi: 10.3748/wjg.v18.i46.6720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Silberhumer GR, Hufschmid M, Wrba F, Gyoeri G, Schoppmann S, Tribl B, Wenzl E, Prager G, Laengle F, Zacherl J. Surgery for gastrointestinal stromal tumors of the stomach. J Gastrointest Surg. 2009;13:1213–1219. doi: 10.1007/s11605-009-0872-0. [DOI] [PubMed] [Google Scholar]
- 22.Nguyen SQ, Divino CM, Wang JL, Dikman SH. Laparoscopic management of gastrointestinal stromal tumors. Surg Endosc. 2006;20:713–716. doi: 10.1007/s00464-005-0435-8. [DOI] [PubMed] [Google Scholar]
- 23.Demetri GD, Benjamin RS, Blanke CD, Blay JY, Casali P, Choi H, Corless CL, Debiec-Rychter M, DeMatteo RP, Ettinger DS, et al. NCCN Task Force report: management of patients with gastrointestinal stromal tumor (GIST)--update of the NCCN clinical practice guidelines. J Natl Compr Canc Netw. 2007;5 Suppl 2:S1–29; quiz S30. [PubMed] [Google Scholar]
- 24.De Vogelaere K, Van Loo I, Peters O, Hoorens A, Haentjens P, Delvaux G. Laparoscopic resection of gastric gastrointestinal stromal tumors (GIST) is safe and effective, irrespective of tumor size. Surg Endosc. 2012;26:2339–2345. doi: 10.1007/s00464-012-2186-7. [DOI] [PubMed] [Google Scholar]
- 25.Privette A, McCahill L, Borrazzo E, Single RM, Zubarik R. Laparoscopic approaches to resection of suspected gastric gastrointestinal stromal tumors based on tumor location. Surg Endosc. 2008;22:487–494. doi: 10.1007/s00464-007-9493-4. [DOI] [PubMed] [Google Scholar]
- 26.Novitsky YW, Kercher KW, Sing RF, Heniford BT. Long-term outcomes of laparoscopic resection of gastric gastrointestinal stromal tumors. Ann Surg. 2006;243:738–45; discussion 745-7. doi: 10.1097/01.sla.0000219739.11758.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lukaszczyk JJ, Preletz RJ. Laparoscopic resection of benign stromal tumor of the stomach. J Laparoendosc Surg. 1992;2:331–334. doi: 10.1089/lps.1992.2.331. [DOI] [PubMed] [Google Scholar]
- 28.Coccolini F, Catena F, Ansaloni L, Lazzareschi D, Pinna AD. Esophagogastric junction gastrointestinal stromal tumor: resection vs enucleation. World J Gastroenterol. 2010;16:4374–4376. doi: 10.3748/wjg.v16.i35.4374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Coccolini F, Catena F, Ansaloni L, Pinna AD. Gastrointestinal stromal tumor and mitosis, pay attention. World J Gastroenterol. 2012;18:587–588. doi: 10.3748/wjg.v18.i6.587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim MD, Kang DH, Park JH, Lee JH, Choi CW, Kim do H, Kim HW, Kim GH. Abdominal wound metastasis after laparoscopic surgery of gastrointestinal stromal tumor. Gut Liver. 2010;4:283–286. doi: 10.5009/gnl.2010.4.2.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Melstrom LG, Phillips JD, Bentrem DJ, Wayne JD. Laparoscopic versus open resection of gastric gastrointestinal stromal tumors. Am J Clin Oncol. 2012;35:451–454. doi: 10.1097/COC.0b013e31821954a7. [DOI] [PubMed] [Google Scholar]
- 32.Sexton JA, Pierce RA, Halpin VJ, Eagon JC, Hawkins WG, Linehan DC, Brunt LM, Frisella MM, Matthews BD. Laparoscopic gastric resection for gastrointestinal stromal tumors. Surg Endosc. 2008;22:2583–2587. doi: 10.1007/s00464-008-9807-1. [DOI] [PubMed] [Google Scholar]
- 33.Koh YX, Chok AY, Zheng HL, Tan CS, Chow PK, Wong WK, Goh BK. A systematic review and meta-analysis comparing laparoscopic versus open gastric resections for gastrointestinal stromal tumors of the stomach. Ann Surg Oncol. 2013;20:3549–3560. doi: 10.1245/s10434-013-3051-1. [DOI] [PubMed] [Google Scholar]
- 34.Fujimoto Y, Nakanishi Y, Yoshimura K, Shimoda T. Clinicopathologic study of primary malignant gastrointestinal stromal tumor of the stomach, with special reference to prognostic factors: analysis of results in 140 surgically resected patients. Gastric Cancer. 2003;6:39–48. doi: 10.1007/s101200300005. [DOI] [PubMed] [Google Scholar]
- 35.Joensuu H, Vehtari A, Riihimäki J, Nishida T, Steigen SE, Brabec P, Plank L, Nilsson B, Cirilli C, Braconi C, et al. Risk of recurrence of gastrointestinal stromal tumour after surgery: an analysis of pooled population-based cohorts. Lancet Oncol. 2012;13:265–274. doi: 10.1016/S1470-2045(11)70299-6. [DOI] [PubMed] [Google Scholar]
- 36.Choi SM, Kim MC, Jung GJ, Kim HH, Kwon HC, Choi SR, Jang JS, Jeong JS. Laparoscopic wedge resection for gastric GIST: long-term follow-up results. Eur J Surg Oncol. 2007;33:444–447. doi: 10.1016/j.ejso.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 37.Huguet KL, Rush RM, Tessier DJ, Schlinkert RT, Hinder RA, Grinberg GG, Kendrick ML, Harold KL. Laparoscopic gastric gastrointestinal stromal tumor resection: the mayo clinic experience. Arch Surg. 2008;143:587–90; discussion 591. doi: 10.1001/archsurg.143.6.587. [DOI] [PubMed] [Google Scholar]
- 38.Ronellenfitsch U, Staiger W, Kähler G, Ströbel P, Schwarzbach M, Hohenberger P. Perioperative and oncological outcome of laparoscopic resection of gastrointestinal stromal tumour (GIST) of the stomach. Diagn Ther Endosc. 2009;2009:286138. doi: 10.1155/2009/286138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tagaya N, Mikami H, Kubota K. Laparoscopic resection of gastrointestinal mesenchymal tumors located in the upper stomach. Surg Endosc. 2004;18:1469–1474. doi: 10.1007/s00464-004-8800-6. [DOI] [PubMed] [Google Scholar]
- 40.Karakousis GC, Singer S, Zheng J, Gonen M, Coit D, DeMatteo RP, Strong VE. Laparoscopic versus open gastric resections for primary gastrointestinal stromal tumors (GISTs): a size-matched comparison. Ann Surg Oncol. 2011;18:1599–1605. doi: 10.1245/s10434-010-1517-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kim KH, Kim MC, Jung GJ, Kim SJ, Jang JS, Kwon HC. Long term survival results for gastric GIST: is laparoscopic surgery for large gastric GIST feasible? World J Surg Oncol. 2012;10:230. doi: 10.1186/1477-7819-10-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nishimura J, Nakajima K, Omori T, Takahashi T, Nishitani A, Ito T, Nishida T. Surgical strategy for gastric gastrointestinal stromal tumors: laparoscopic vs. open resection. Surg Endosc. 2007;21:875–878. doi: 10.1007/s00464-006-9065-z. [DOI] [PubMed] [Google Scholar]
- 43.Otani Y, Furukawa T, Yoshida M, Saikawa Y, Wada N, Ueda M, Kubota T, Mukai M, Kameyama K, Sugino Y, et al. Operative indications for relatively small (2-5 cm) gastrointestinal stromal tumor of the stomach based on analysis of 60 operated cases. Surgery. 2006;139:484–492. doi: 10.1016/j.surg.2005.08.011. [DOI] [PubMed] [Google Scholar]


