Abstract
AIM: To determine if a new brush design could improve the diagnostic yield of biliary stricture brushings.
METHODS: Retrospective chart review was performed of all endoscopic retrograde cholangiopancreatography procedures with malignant biliary stricture brushing between January 2008 and October 2012. A standard wire-guided cytology brush was used prior to protocol implementation in July 2011, after which, a new 9 French wire-guided cytology brush (Infinity sampling device, US Endoscopy, Mentor, OH) was used for all cases. All specimens were reviewed by blinded pathologists who determined whether the sample was positive or negative for malignancy. Cellular yield was quantified by describing the number of cell clusters seen.
RESULTS: Thirty-two new brush cases were compared to 46 historical controls. Twenty-five of 32 (78%) cases in the new brush group showed abnormal cellular findings consistent with malignancy as compared to 17 of 46 (37%) in the historical control group (P = 0.0003). There was also a significant increase in the average number of cell clusters of all sizes (21.1 vs 9.9 clusters, P = 0.0007) in the new brush group compared to historical controls.
CONCLUSION: The use of a new brush design for brush cytology of biliary strictures shows increased diagnostic accuracy, likely due to improved cellular yield, as evidenced by an increase in number of cellular clusters obtained.
Keywords: Malignant biliary stricture, Endoscopic retrograde cholangiopancreatography, Brush cytology, Diagnostic yield, Cytopathology
Core tip: The sensitivity of brush cytology for biliary strictures has historically been low (around 30%-60%). Many studies have described efforts to improve cellular yield and diagnostic accuracy with varying success. We describe the development of an improved biliary brush cytology protocol with the use of a new biliary brush design which more than doubled the diagnostic yield of our brush cytology as compared to the historical cases. Cytopathological analysis also showed increased cellular yield, and thus better diagnostic accuracy, with the improved protocol implementation.
INTRODUCTION
Brush cytology during endoscopic retrograde cholangiopancreatography (ERCP) remains one of the most common approaches to sample biliary strictures. Cytologic brushing has an excellent safety profile, widespread availability, and is relatively quick and simple to perform[1,2]. However, the reported sensitivity for brush cytology is low, ranging from 30%-60%[3]. Many studies have described efforts to improve cellular yield and diagnostic accuracy. These include disruption of the biliary epithelium by dilating the stricture prior to brushing, two or more brush passes, use of an extra-long cytology brush, immunohistochemistry, cell block method, and mutational analysis, all with varying success[4-15].
Obtaining adequate cellular yield appears to be a key factor in maximizing diagnostic sensitivity and accuracy. In 2011, a new wire-guided cytology brush (Infinity sampling device, US Endoscopy, Mentor, OH) was released for use. This brush has a 9 French sheath, and a combination of stiff and soft bristles designed with the objective of maximizing tissue acquisition. The aim of our study was to see if the use of this new brush would be able to improve the diagnostic sensitivity of ERCP-guided biliary brushing of malignant biliary strictures.
MATERIALS AND METHODS
Retrospective chart review of consecutive ERCPs, performed between January 2008 and October 2012 at our academic center, was conducted. ERCP procedures which involved cytologic brushing of a biliary stricture for suspected malignant biliary obstruction were included in the study. All patients were eventually diagnosed with a malignant biliary obstruction either by endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) or by surgical resection. Our study was approved by the Geisinger Health System Institutional Review Board.
Procedures performed between January 2008 and June 2011 served as historical controls. In this cohort, ERCP cytology brushing was performed with a standard 8 French wire-guided brush (Cytomax, Cook Medical, Bloomington IN; or RX, Boston Scientific, Marlborough MA). Two passes, each with multiple to-and-fro movements across the biliary stricture, were performed. Smears on slides were prepared, and the brush head was then cut off and sent in the cytology transport medium (RPMI).
A standardized protocol was instituted on July 1st, 2011 for ERCP brushing of biliary strictures. All cases were performed with the new 9 French wire-guided cytology brush (Infinity sampling device, US Endoscopy, Mentor, OH) (Figure 1). This brush can be used with a short wire as well as a long wire system. After placement of a biliary guidewire across the stricture, two separate passes, each with multiple to and fro movements, were performed with the brush across the biliary stricture. With the cytologic material collected from the first pass, two touch-prep smears were prepared, one of which was sprayed with fixative (Protocol Cytologic Fixative, Fisher Scientific, Pittsburgh, PA), and the other smear was air-dried. The brush was then agitated in the RPMI cytology fluid to dislodge accumulated cellular material. The brush was subsequently rinsed with water and a second pass was performed with the same brush over the biliary guidewire. The brush was then removed; the brush head was cut off and placed into the same tube of RPMI cytology fluid (Figure 2).
Figure 1.
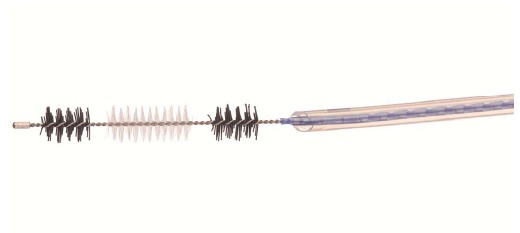
Detail of the 9 French cytology brush (Infinity sampling device, US Endoscopy, Mentor, OH).
Figure 2.
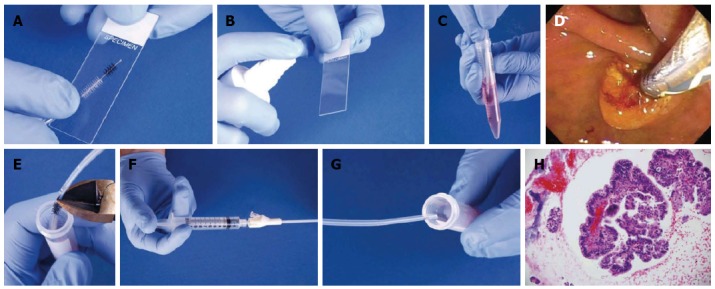
Brushing technique. Two passes performed in the stricture. A, B: The first pass was used to make two smears (A), with one smear sprayed with fixative (B); C: The brush was then agitated in the RPMI cytology fluid to dislodge material into the fluid; D: The brush was rinsed with water. A second pass was performed with the same brush; E: The brush was cut off into the same tube of RPMI; F, G: Contents of catheter were flushed via salvage cytology technique; H: The sample was processed as a cell block.
Salvage cytology was performed by injecting 5 mL of RPMI cytology fluid through the brush catheter after brushing was completed. The two smear slides and the tube of RPMI containing the brush head and salvage cytology were all submitted to cytology. The smears were stained, and a cell block was made from the tube contents. Smears and cell blocks were reviewed by 2 experienced cytopathologists blinded to the final diagnosis. Cellular yield was meticulously quantified by counting the number and size of cell clusters seen (large clusters > 50 cells, medium clusters 6-49 cells, small clusters 2-5 cells, and single cells). In accordance to current standards in the literature, cytopathological diagnosis of “malignant” or “suspicious” were considered positive, while “atypical” cases were considered negative[9].
RESULTS
Thirty-two new protocol cases and 46 historical controls were analyzed. There were no significant differences in gender (63% vs 56% male, respectively, P = 0.55), or age (mean 70 vs 68 years old, respectively, P = 0.45) between the groups. The majority of cases were either pancreatic adenocarcinoma or cholangiocarcinoma as eventually confirmed by EUS-FNA or surgical resection. The degree of the biliary strictures was similar in both the groups. The 32 cases in the new protocol cohort consisted of 23 cases of pancreatic adenocarcinoma, 7 cases of cholangiocarcinoma, and 2 gallbladder cancers. Twenty-five of these 32 (78%) cases were diagnosed with malignancy based on biliary brush cytology using the new brush and cytology protocol. The 46 cases in the historical control group consisted of 22 cases of cholangiocarcinoma, 20 cases of pancreatic adenocarcinoma, and 4 others (2 gallbladder cancers, 1 colon cancer, 1 of unknown primary). Seventeen of these 46 (37%) cases were diagnosed with malignancy based on biliary brush cytology using the standard brushes and cytology yield. There was an increased diagnostic yield of brush cytology of these malignant biliary strictures in the new protocol group as compared to the historical controls (P = 0.0003) (Table 1).
Table 1.
Diagnostic yield for the new brush protocol vs historical control
| New brush protocol | Historical control | P value | |
| Mean age (yr) | 70 | 68 | 0.45 |
| Gender (males) | 63% | 56% | 0.55 |
| All cases | 25/32 (78%) | 17/46 (37%) | 0.0003 |
| Pancreatic adenocarcinoma | 17/23 (74%) | 6/20 (30%) | 0.005 |
| Cholangiocarcinoma | 7/7 (100%) | 8/22 (36%) | 0.004 |
| Other | 1/2 (50%) | 3/4 (75%) | 0.6 |
| 2 gallbladder cancers | 2 gallbladder, 1 colon, 1 unknown |
There was also a significant increase in the average number of cell clusters of all sizes obtained with the new brush compared to the standard brushes (21.1 vs 9.9 clusters, P = 0.0007). This relationship held true when cluster size was broken down into four different categories (large clusters > 50 cells, medium clusters 6-49 cells, small clusters 2-5 cells, and single cells) for all cases. For each of the subsets of cluster size, there was a significant increase in the number of clusters in the new brush group compared to the historical control group (P = 0.005, 0.0004, 0.01, 0.009 respectively) (Figure 3).
Figure 3.
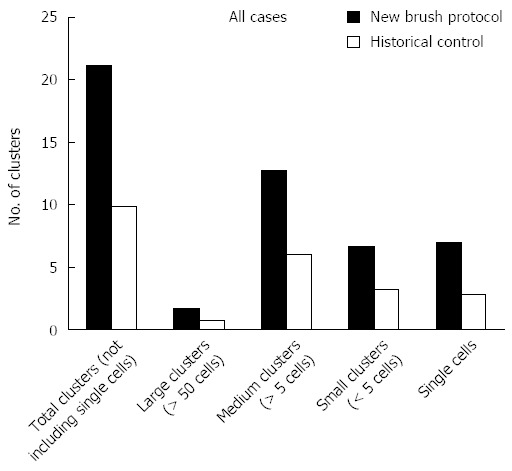
Number of clusters obtained by cytologic brushing for all cases.
In the subgroup of patients with pancreatic adenocarcinoma, there was an increase in average total cell clusters of all sizes (20.9 vs 6.1, P = 0.001) as well as large, medium, small clusters and single cells (P = 0.0001, 0.0001, 0.0004, and 0.0012, respectively). Diagnostic yield was 74% (17/23) in the new brush group compared to 30% (6/20) in the historical controls, P = 0.005.
Similar results were seen in the subgroup of patients with cholangiocarcinoma, with an increase in average total cell clusters of all sizes (24.6 vs 10.8), as well as large, medium, small clusters and single cells (P = 0.04, 0.01, 0.03, and 0.01, respectively). Diagnostic yield was 100% (7/7) for the new brush group compared to 36% (8/22) in the historical controls, P = 0.004.
DISCUSSION
Tissue diagnosis of biliary strictures is of critical importance in treatment planning. This is usually done via brush cytology during ERCP, however the diagnostic yield with standard brushings have been low and variable. Changes in technique (predilation, making a second pass, or scraping the stricture with the tip of the cytology brush catheter) can increase yield. Forceps biopsy at the time of ERCP can also be done, with slightly higher diagnostic yield (43%-60%)[3], but can be technically challenging to obtain in some certain cases, especially by less experienced endoscopists. In addition, the diagnostic yield can be low in extrinsic biliary obstruction such as from pancreatic head cancer as compared to cholangiocarcinoma, which typically has an intraductal lesion.
Per-oral cholangioscopy can have sensitivities as high as 78%-89% for the diagnosis of malignancy in indeterminate biliary strictures. However, the utility of this method is limited due several reasons such as scope fragility, requirement of special equipment with high acquisition costs, and requirement of a high level of endoscopic expertise. In addition, “real world” results have not matched those initially obtained by a group of highly skilled biliary endoscopists. Furthermore, tissue sampling is still required for a diagnosis of malignancy which is usually performed through either brush or biopsy methods[6,16,17].
Endoscopic ultrasound allows detailed examination of the common bile duct and pancreatic head, and tissue sampling can be performed via EUS-FNA with diagnostic yield as high as 89%[12,18-21]. However, many patients who undergo EUS-FNA for the diagnosis of ductal malignancy will have already undergone ERCP with brushing, and there are costs associated with the second procedure. If EUS-FNA is done in cases of cholangiocarcinoma, there is the potential for tumor seeding. In fact, the Mayo Clinic protocol for liver transplantation in cholangiocarcinoma considers FNA to be a contraindication to liver transplantation[12,22,23]. Probe-based confocal laser endomicroscopy is a newer technology which can offer real-time histologic evaluation of indeterminate biliary strictures during ERCP with overall diagnostic accuracy of over 80%, but it is not widely available, and further studies need to be performed prior to more generalized use[24-28].
A potentially unrecognized source of variability in sampling is how specimens are handled after they are obtained. Some endoscopists always make a smear, and some never do. Some cytology departments always make a cell block and some do this only on request. There is evidence that creation of a cell block can increase the cellular yield and ability to interpret architecture, thereby increasing the sensitivity of cytodiagnosis compared to conventional smears[15]. Multiple studies have consistently shown that cell block along with smear cytology can markedly improve both the sensitivity and specificity of cytologic specimens in the diagnosis of malignancies, especially when the diagnosis from smear alone is non-diagnostic, and that it is cost-effective[29-34]. The increased quantitative cytology yield is also useful if more specialized tests are required on the tissue. For example, detection of aneuploidy via digital image analysis (DIA) or fluorescence in situ hybridization (FISH) may be useful in increasing the diagnostic yield in certain difficult indeterminate biliary strictures[35].
Several aspects of the new brush design are likely to have contributed to improved results. The new brush incorporates an increased brush diameter and length, as well as a new bristle design. Stiffer bristles are present on the proximal and distal ends of the brush, which may dislodge more underlying tissue due to a more abrasive effect. Softer bristles in the middle of the brush are then able to capture the abraded material. Some authors recommend removing the brush and catheter as a unit, to prevent loss of cellular material[5]. The new brush also has a slightly larger catheter (9 French compared to 8 French) which decreases the “squeegee effect” of causing tissue loss from the bristles when the brush is retracted. This slightly bigger catheter size did not cause any technical difficulties in advancing the brush over the biliary wire to the desired location as compared to the 8 French brushes. The ability to collect cells for so-called “salvage cytology” from the brush sheath may also contribute to the increase in the amount of tissue collected[36,37]. It is logical that more tissue disruption prior by brushing can improve cellular yield; which is supported by studies demonstrating that two consecutive brushings improved cancer detection rate from 33% to 44%[7], and three consecutive brushings increased the rate from 40% to 60%[38]. In the new brush protocol, we uniformly performed two passes, which may also have contributed to the better diagnostic yield. One limitation of our study is that it is a retrospective review, and the new brush was used in conjunction with a standardized brushing and specimen processing protocol, which may potentially affect the outcomes of the results. However, other than the brush design itself, the tissue acquisition and processing technique was similar in both groups.
With the use of a newly designed ERCP cytology brush, we were able to more than double the diagnostic yield of our brush cytology. Proper specimen processing with the production of smears as well as cell-blocks further increases the cytologist’s ability to make a firm diagnosis on the obtained tissue. When it comes to the pathologist’s point of view, “tissue is the issue” and increased tissue yields improves the pathologist’s ability to make a diagnosis in cases of potentially malignant biliary stricture.
ACKNOWLEDGMENTS
Data from this study was presented in May 2013 as a poster presentation at Digestive Disease Week 2013 in Orlando, FL, United States.
COMMENTS
Background
The sensitivity of brush cytology for biliary strictures during endoscopic retrograde cholangiopancreatography has historically been low (around 30%-60%) despite various technical variations.
Research frontiers
There is a great need to improve the diagnostic yield of biliary brushings, which is most common and widely used modality for evaluation of biliary strictures.
Innovations and breakthroughs
Many studies have described efforts to improve cellular yield and diagnostic accuracy. These include disruption of the biliary epithelium by dilating the stricture prior to brushing, two or more brush passes, use of an extra-long cytology brush, forceps biopsy method, per-oral cholangioscopy, endoscopic ultrasound-guided fine needle aspiration, probe-based confocal laser endomicroscopy, immunohistochemistry, cell block method, fluorescence in situ hybridization and mutational analysis, all with varying success.
Applications
The goal was to determine if by simply using a new brush design and implementing a standardized cytology processing protocol would improve the diagnostic yield of biliary stricture brushings as compared to historical controls.
Peer review
This is a well-written manuscript dealing with an interesting topic. The methodology is straight-forward and the conclusions drawn are in concern with the logics and results of the study.
Footnotes
P- Reviewers: Murata A, Wehrmann T S- Editor: Song XX L- Editor: A E- Editor: Zhang DN
References
- 1.Vandervoort J, Soetikno RM, Montes H, Lichtenstein DR, Van Dam J, Ruymann FW, Cibas ES, Carr-Locke DL. Accuracy and complication rate of brush cytology from bile duct versus pancreatic duct. Gastrointest Endosc. 1999;49:322–327. doi: 10.1016/s0016-5107(99)70008-8. [DOI] [PubMed] [Google Scholar]
- 2.Papachristou GI, Smyrk TC, Baron TH. Endoscopic retrograde cholangiopancreatography tissue sampling: when and how? Clin Gastroenterol Hepatol. 2007;5:783–790. doi: 10.1016/j.cgh.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 3.Weber A, von Weyhern C, Fend F, Schneider J, Neu B, Meining A, Weidenbach H, Schmid RM, Prinz C. Endoscopic transpapillary brush cytology and forceps biopsy in patients with hilar cholangiocarcinoma. World J Gastroenterol. 2008;14:1097–1101. doi: 10.3748/wjg.14.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bardales RH, Stanley MW, Simpson DD, Baker SJ, Steele CT, Schaefer RF, Powers CN. Diagnostic value of brush cytology in the diagnosis of duodenal, biliary, and ampullary neoplasms. Am J Clin Pathol. 1998;109:540–548. doi: 10.1093/ajcp/109.5.540. [DOI] [PubMed] [Google Scholar]
- 5.Baron TH, Lee JG, Wax TD, Schmitt CM, Cotton PB, Leung JW. An in vitro, randomized, prospective study to maximize cellular yield during bile duct brush cytology. Gastrointest Endosc. 1994;40:146–149. doi: 10.1016/s0016-5107(94)70156-3. [DOI] [PubMed] [Google Scholar]
- 6.Chen YK, Pleskow DK. SpyGlass single-operator peroral cholangiopancreatoscopy system for the diagnosis and therapy of bile-duct disorders: a clinical feasibility study (with video) Gastrointest Endosc. 2007;65:832–841. doi: 10.1016/j.gie.2007.01.025. [DOI] [PubMed] [Google Scholar]
- 7.de Bellis M, Fogel EL, Sherman S, Watkins JL, Chappo J, Younger C, Cramer H, Lehman GA. Influence of stricture dilation and repeat brushing on the cancer detection rate of brush cytology in the evaluation of malignant biliary obstruction. Gastrointest Endosc. 2003;58:176–182. doi: 10.1067/mge.2003.345. [DOI] [PubMed] [Google Scholar]
- 8.de Bellis M, Sherman S, Fogel EL, Cramer H, Chappo J, McHenry L, Watkins JL, Lehman GA. Tissue sampling at ERCP in suspected malignant biliary strictures (Part 2) Gastrointest Endosc. 2002;56:720–730. doi: 10.1067/mge.2002.129219. [DOI] [PubMed] [Google Scholar]
- 9.De Bellis M, Sherman S, Fogel EL, Cramer H, Chappo J, McHenry L, Watkins JL, Lehman GA. Tissue sampling at ERCP in suspected malignant biliary strictures (Part 1) Gastrointest Endosc. 2002;56:552–561. doi: 10.1067/mge.2002.128132. [DOI] [PubMed] [Google Scholar]
- 10.Farrell RJ, Jain AK, Brandwein SL, Wang H, Chuttani R, Pleskow DK. The combination of stricture dilation, endoscopic needle aspiration, and biliary brushings significantly improves diagnostic yield from malignant bile duct strictures. Gastrointest Endosc. 2001;54:587–594. doi: 10.1067/mge.2001.118715. [DOI] [PubMed] [Google Scholar]
- 11.Fogel EL, deBellis M, McHenry L, Watkins JL, Chappo J, Cramer H, Schmidt S, Lazzell-Pannell L, Sherman S, Lehman GA. Effectiveness of a new long cytology brush in the evaluation of malignant biliary obstruction: a prospective study. Gastrointest Endosc. 2006;63:71–77. doi: 10.1016/j.gie.2005.08.039. [DOI] [PubMed] [Google Scholar]
- 12.Khashab MA, Fockens P, Al-Haddad MA. Utility of EUS in patients with indeterminate biliary strictures and suspected extrahepatic cholangiocarcinoma (with videos) Gastrointest Endosc. 2012;76:1024–1033. doi: 10.1016/j.gie.2012.04.451. [DOI] [PubMed] [Google Scholar]
- 13.Venu RP, Geenen JE, Kini M, Hogan WJ, Payne M, Johnson GK, Schmalz MJ. Endoscopic retrograde brush cytology. A new technique. Gastroenterology. 1990;99:1475–1479. doi: 10.1016/0016-5085(90)91178-9. [DOI] [PubMed] [Google Scholar]
- 14.Fritcher EG, Kipp BR, Halling KC, Oberg TN, Bryant SC, Tarrell RF, Gores GJ, Levy MJ, Clayton AC, Sebo TJ, et al. A multivariable model using advanced cytologic methods for the evaluation of indeterminate pancreatobiliary strictures. Gastroenterology. 2009;136:2180–2186. doi: 10.1053/j.gastro.2009.02.040. [DOI] [PubMed] [Google Scholar]
- 15.Shivakumarswamy U, Arakeri SU, Karigowdar MH, Yelikar B. Diagnostic utility of the cell block method versus the conventional smear study in pleural fluid cytology. J Cytol. 2012;29:11–15. doi: 10.4103/0970-9371.93210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kawakubo K, Isayama H, Sasahira N, Kogure H, Takahara N, Miyabayashi K, Mizuno S, Yamamoto K, Mohri D, Sasaki T, et al. Clinical utility of single-operator cholangiopancreatoscopy using a SpyGlass probe through an endoscopic retrograde cholangiopancreatography catheter. J Gastroenterol Hepatol. 2012;27:1371–1376. doi: 10.1111/j.1440-1746.2012.07133.x. [DOI] [PubMed] [Google Scholar]
- 17.Shah RJ, Langer DA, Antillon MR, Chen YK. Cholangioscopy and cholangioscopic forceps biopsy in patients with indeterminate pancreaticobiliary pathology. Clin Gastroenterol Hepatol. 2006;4:219–225. doi: 10.1016/s1542-3565(05)00979-1. [DOI] [PubMed] [Google Scholar]
- 18.Rösch T, Hofrichter K, Frimberger E, Meining A, Born P, Weigert N, Allescher HD, Classen M, Barbur M, Schenck U, et al. ERCP or EUS for tissue diagnosis of biliary strictures? A prospective comparative study. Gastrointest Endosc. 2004;60:390–396. doi: 10.1016/s0016-5107(04)01732-8. [DOI] [PubMed] [Google Scholar]
- 19.Mohamadnejad M, DeWitt JM, Sherman S, LeBlanc JK, Pitt HA, House MG, Jones KJ, Fogel EL, McHenry L, Watkins JL, et al. Role of EUS for preoperative evaluation of cholangiocarcinoma: a large single-center experience. Gastrointest Endosc. 2011;73:71–78. doi: 10.1016/j.gie.2010.08.050. [DOI] [PubMed] [Google Scholar]
- 20.Fritscher-Ravens A, Broering DC, Knoefel WT, Rogiers X, Swain P, Thonke F, Bobrowski C, Topalidis T, Soehendra N. EUS-guided fine-needle aspiration of suspected hilar cholangiocarcinoma in potentially operable patients with negative brush cytology. Am J Gastroenterol. 2004;99:45–51. doi: 10.1046/j.1572-0241.2003.04006.x. [DOI] [PubMed] [Google Scholar]
- 21.Fritscher-Ravens A, Broering DC, Sriram PV, Topalidis T, Jaeckle S, Thonke F, Soehendra N. EUS-guided fine-needle aspiration cytodiagnosis of hilar cholangiocarcinoma: a case series. Gastrointest Endosc. 2000;52:534–540. doi: 10.1067/mge.2000.109589. [DOI] [PubMed] [Google Scholar]
- 22.Gleeson FC, Rajan E, Levy MJ, Clain JE, Topazian MD, Harewood GC, Papachristou GI, Takahashi N, Rosen CB, Gores GJ. EUS-guided FNA of regional lymph nodes in patients with unresectable hilar cholangiocarcinoma. Gastrointest Endosc. 2008;67:438–443. doi: 10.1016/j.gie.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 23.Rosen CB, Heimbach JK, Gores GJ. Liver transplantation for cholangiocarcinoma. Transpl Int. 2010;23:692–697. doi: 10.1111/j.1432-2277.2010.01108.x. [DOI] [PubMed] [Google Scholar]
- 24.Meining A, Shah RJ, Slivka A, Pleskow D, Chuttani R, Stevens PD, Becker V, Chen YK. Classification of probe-based confocal laser endomicroscopy findings in pancreaticobiliary strictures. Endoscopy. 2012;44:251–257. doi: 10.1055/s-0031-1291545. [DOI] [PubMed] [Google Scholar]
- 25.Wallace M, Lauwers GY, Chen Y, Dekker E, Fockens P, Sharma P, Meining A. Miami classification for probe-based confocal laser endomicroscopy. Endoscopy. 2011;43:882–891. doi: 10.1055/s-0030-1256632. [DOI] [PubMed] [Google Scholar]
- 26.Meining A, Chen YK, Pleskow D, Stevens P, Shah RJ, Chuttani R, Michalek J, Slivka A. Direct visualization of indeterminate pancreaticobiliary strictures with probe-based confocal laser endomicroscopy: a multicenter experience. Gastrointest Endosc. 2011;74:961–968. doi: 10.1016/j.gie.2011.05.009. [DOI] [PubMed] [Google Scholar]
- 27.Meining A, Frimberger E, Becker V, Von Delius S, Von Weyhern CH, Schmid RM, Prinz C. Detection of cholangiocarcinoma in vivo using miniprobe-based confocal fluorescence microscopy. Clin Gastroenterol Hepatol. 2008;6:1057–1060. doi: 10.1016/j.cgh.2008.04.014. [DOI] [PubMed] [Google Scholar]
- 28.Shieh FK, Drumm H, Nathanson MH, Jamidar PA. High-definition confocal endomicroscopy of the common bile duct. J Clin Gastroenterol. 2012;46:401–406. doi: 10.1097/MCG.0b013e31822f3fcd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Erkiliç S, Ozsaraç C, Küllü S. Sputum cytology for the diagnosis of lung cancer. Comparison of smear and modified cell block methods. Acta Cytol. 2003;47:1023–1027. doi: 10.1159/000326639. [DOI] [PubMed] [Google Scholar]
- 30.Liu K, Dodge R, Glasgow BJ, Layfield LJ. Fine-needle aspiration: comparison of smear, cytospin, and cell block preparations in diagnostic and cost effectiveness. Diagn Cytopathol. 1998;19:70–74. doi: 10.1002/(sici)1097-0339(199807)19:1<70::aid-dc15>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 31.Dekker A, Bupp PA. Cytology of serous effusions. An investigation into the usefulness of cell blocks versus smears. Am J Clin Pathol. 1978;70:855–860. doi: 10.1093/ajcp/70.6.855. [DOI] [PubMed] [Google Scholar]
- 32.Nathan NA, Narayan E, Smith MM, Horn MJ. Cell block cytology. Improved preparation and its efficacy in diagnostic cytology. Am J Clin Pathol. 2000;114:599–606. doi: 10.1309/G035-P2MM-D1TM-T5QE. [DOI] [PubMed] [Google Scholar]
- 33.Thapar M, Mishra RK, Sharma A, Goyal V, Goyal V. Critical analysis of cell block versus smear examination in effusions. J Cytol. 2009;26:60–64. doi: 10.4103/0970-9371.55223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Axe SR, Erozan YS, Ermatinger SV. Fine-needle aspiration of the liver. A comparison of smear and rinse preparations in the detection of cancer. Am J Clin Pathol. 1986;86:281–285. doi: 10.1093/ajcp/86.3.281. [DOI] [PubMed] [Google Scholar]
- 35.Moreno Luna LE, Kipp B, Halling KC, Sebo TJ, Kremers WK, Roberts LR, Barr Fritcher EG, Levy MJ, Gores GJ. Advanced cytologic techniques for the detection of malignant pancreatobiliary strictures. Gastroenterology. 2006;131:1064–1072. doi: 10.1053/j.gastro.2006.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Green LK, Zachariah S, Graham DY. The use of gastric salvage cytology in the diagnosis of malignancy: a review of 731 cases. Diagn Cytopathol. 1990;6:1–4. doi: 10.1002/dc.2840060102. [DOI] [PubMed] [Google Scholar]
- 37.Caos A, Olson N, Willman C, Gogel HK. Endoscopic “salvage” cytology in neoplasms metastatic to the upper gastrointestional tract. Acta Cytol. 1986;30:32–34. [PubMed] [Google Scholar]
- 38.Rabinovitz M, Zajko AB, Hassanein T, Shetty B, Bron KM, Schade RR, Gavaler JS, Block G, Van Thiel DH, Dekker A. Diagnostic value of brush cytology in the diagnosis of bile duct carcinoma: a study in 65 patients with bile duct strictures. Hepatology. 1990;12:747–752. doi: 10.1002/hep.1840120421. [DOI] [PubMed] [Google Scholar]


