Abstract
AIM: To assess the usefulness of the balloon assisted enteroscopy in preventing surgical intervention in patients with Peutz-Jeghers syndrome (PJS) having a small bowel large polyps.
METHODS: Seven consecutive asymptomatic pts (age 15-38 years) with PJS have been collected; six underwent polypectomy using single balloon enteroscopy (Olympus SIF Q180) with antegrade approach using push and pull technique. SBE system consists of the SIF-Q180 enteroscope, an overtube balloon control unit (OBCU Olympus Balloon Control Unit) and a disposable silicone splinting tube with balloon (ST-SB1). All procedures were performed under general anesthesia. Previously all pts received wireless capsule endoscopy (WCE). Prophylactic polypectomy was reserved mainly in pts who had polyps > 15 mm in diameter. The balloon is inflated and deflated by a balloon control unit with a safety pressure setting range from -6.0 kPa to +5.4 kPa. Informed consent has been obtained from pts or parents for each procedure.
RESULTS: Six pts underwent polypectomy of small bowel polyps; in 5 pts a large polyp > 15 mm (range 20-50 mm in diameter) was resected; in 1 patient with WCE negative, SBE was performed for previous surgical resection of gastrointestinal stromal tumors. In 2 pts endoscopic clips were placed due to a polypectomy. No surgical complication have been reported. SBE with resection of small bowel large polyps in PJS pts was useful to avoid gastrointestinal bleeding and emergency laparotomy due to intestinal intussusceptions. No gastrointestinal tumors were found in subsequent enteroscopic surveillance in all seven pts. In order surveillance, all pts received WCE, upper endoscopy, ileocolonoscopy every 2 years. No pts had extraintestinal malignant lesions. SBE was performed when WCE was positive for significant polyps (> 15 mm).
CONCLUSION: The effective of prophylactic polypectomy of small bowel large polyps (> 15 mm) could be the first line treatment for conservative approach in management of PJS patients.
Keywords: Peutz-Jeghers syndrome, Balloon assisted enteroscopy, Polypectomy
Core tip: Peutz-Jeghers syndrome (PJS) is an autosomal dominant disorder characterized by mucocutaneus pigmentation and multiple polyps in small bowel. Most of pts need surgical intervention for intussusceptions and gastrointestinal bleeding; the surgical risk is up to 50% in pts having a large polyps > 15 mm or rapidly growing. Enteroscopy balloon assisted with resection of small bowel large polyps is useful to avoid emergency laparotomy after performing wireless capsule endoscopy. The effective of prophylactic polypectomy of small bowel large polyps could be the first line treatment for conservative approach in management of PJS patients.
INTRODUCTION
Peutz-Jeghers syndrome (PJS) is a rare autosomal dominant hereditary disease due to mutation in serine/threonine kinase 11 tumour suppressor gene (STK 11 or LKB1), located on chromosome 19p13.3. The estimated incidence of PJS ranges between 1 in 50000 and 1 in 200000 live births[1]; it is characterized by mucocutaneous melanin pigmentation and hamartomatous polyps in the gastrointestinal tract[2]. These polyps are predominant in the small intestine (prevalence 64%), usually in the jejunum, followed by stomach and colon. The size of polyps requiring endoscopy resection for the high risk of intussusceptions, bleeding, obstruction and malignant transformation, has been considered > 15-20 mm in patients with polyposis[3]. However, the most frequent complication of PJS which occurred during the first decade of life, is intussusception that often needs multiple laparotomies with intestinal enterotomy that increase the risk for short-gut syndrome[4,5]. In the last few years, different diagnostic techniques have been developed for the assessment and therapeutic approach of small bowel polyps, such as small bowel follow-through, wireless capsule endoscopy (WCE), enteroclysis, magnetic resonance and balloon assisted enteroscopy (BAE). PJS is one of the most significant disease that benefit from WCE and BAE for management of this intestinal pathology. The diagnostic yield of WCE has been studied in PJS; usually it is safe, well tolerated and important for the detection of small bowel polyps smaller than 5 mm. When large polyps (> 15 mm) are detected, endoscopic intervention may be required to remove them. BAE is successfully used for surveillance and treatment in patients with PJS[6]. Since 2009, in our Istitution we are using single balloon enteroscopy (SBE) in pts with PJS for radical polypectomy that could provide a means of prophylactic polypectomy to prevent complications and avoid the need for laparotomy.
MATERIALS AND METHODS
Since 2009, we collected seven consecutive asymptomatic PJS pts (4 male, 3 female; age 15-38 years, mean age 22.2 years; weight 50-72 kg) underwent SBE (Olympus SIF Q180 enteroscope Olympus Optical Co., Tokyo, Japan) with anterograde approach and push and pull technique. Clinical and endoscopic characteristics of pts are summarized in Table 1.
Table 1.
Patient characteristics
| Patients | Sex | Age (yr) | Previous surgery | WCE | SBE | No. of polyps removed in small bowel | Size of polyps (mm) | Histology |
| 1 | M | 35 | Intussusceptions | Jejunal large polyps | Proximal jejunal polyps | 5 | 40 | Hamartomatous polyps |
| 2 | M | 34 | Intussusceptions | Jejunal polyps | Proximal jejunal polyps | 3 | 10 | Hamartomatous polyps |
| 3 | F | 16 | Intussusceptions | Jejunal large polyps | Distal jejunal polyps | 4 | 20 | Hamartomatous polyps |
| 4 | F | 21 | Intussusceptions Laparotomy for perforation following colonic polyp | Jejunal large polyps | Proximal jejunal polyps | 5 | 50 | Hamartomatous polyps |
| 5 | M | 31 | Intussusceptions Lapatotomy for GIST | Normal | Normal (Biopsies) | - | - | Normal |
| 6 | M | 17 | Intussusceptions | Jejunal large polyps | Proximal jejunal polyps | 4 | 40 | Hamartomatous polyps |
| 7 | F | 16 | Intussusceptions | Jejunal large polyps | Proximal jejunal polyps | 3 | 50 | Hamartomatous polyps |
GIST: Gastrointestinal stromal tumors; WCE: Wireless capsule endoscopy; SBE: Single balloon enteroscopy.
Before SBE procedure, all pts received upper endoscopy, ileo-colonoscopy and WCE (GIVEN Imaging Ltd., Yoqneam, Israel) to detect polyps’ location and size. WCE allows only an approximate estimation of the size of polyps based on previous experience, however, we estimated polyps size according to small bowel lumen size. The location of small-bowel polyps was estimated by analyzing the WCE transit time between pylorus passage and ileocecal valve. Prophylactic polypectomy was reserved mainly in patients who had polyps > 15 mm in diameter. SBE system consists of the SIF-Q180 enteroscope, an overtube balloon control unit (OBCU Olympus Balloon Control Unit) and a disposable silicone splinting tube with balloon (ST-SB1). The balloon is inflated and deflated by a balloon control unit with a safety pressure setting range from -6.0 kPa to +5.4 kPa. All procedures were performed under general anesthesia. Informed consent has been obtained from pts or parents for each procedure. Peroral insertion required the patient fast for 12 h. Perrectal insertion was not necessary because location of large polyps was predominantly in jejunum and proximal ileum. We performed polypectomy with a polypectomy snare and removed the excised polyp for histological evaluation. Polypectomy was carried out with ENDO CUT Q, a monopolar high frequency electrosurgical technique, based on cutting and coagulation cycles. All pts received intraoperative antibiotic prophylaxis. Fluoroscopic guidance was used when necessary to verify the correct looping and the withdrawal maneuvers of the endoscope. No hemoclips on the polyp pedicle prior to the polypectomy was placed to avoid post polypectomy bleeding. WCE and BAE were performed approximately every 2 years for surveillance and treatment of polyps. All pts underwent abdominal and testicular ultrasonography to exclude malignant extraintestinal complications. Ethical approval for this study was obtained from our ethics board.
RESULTS
Six pts underwent polypectomy of small bowel polyps; in these pts polyps were located in jejunum and proximal ileum according to WCE investigation previously performed (Figure 1). Five pts underwent to extensive polypectomy of small bowel large polyps > 15 mm in diameter (20 mm until 50 mm) (Figure 2); from three to five small bowel large polyps were removed in 5 pts. In one case WCE was normal; this patient underwent SBE for previous surgical resection for gastrointestinal stromal tumors (GIST); SBE was normal. Histological evaluation showed hamartoma tissue in all polyps retrieved. No bleeding or surgical complications have been reported; no complications due to SBE occurred after procedures. In 2 pts endoscopic clips have been placed on a large tearing of intestinal mucosa due to polypectomy procedure (Figure 3). Three of seven pts had multiple gastric micro polyps; no polypectomy was done. Four pts had multiple sessile colonic polyps, one of them with large multiple polyps underwent polypectomy. The mean procedure time was 72 min (range 60-120 min). Mean time of discharge of pts was 2 d. All pts had previous surgical resections of small bowel for polyps due to obstruction or intussusceptions. No gastrointestinal tumors were found in subsequent enteroscopic surveillance in all seven pts. All pts received WCE, upper endoscopy, ileocolonoscopy every 2 years. No pts had extraintestinal malignant lesions. SBE was performed when WCE was positive for significant polyps (> 15 mm).
Figure 1.
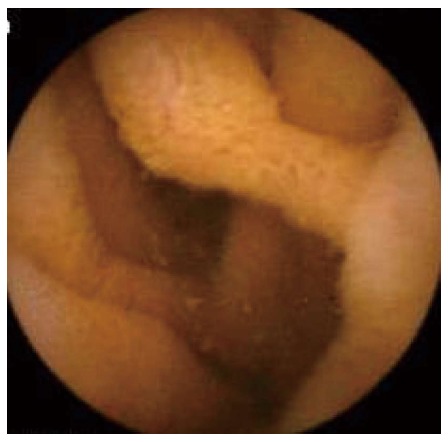
Wireless capsule endoscopy: Jejunal polyp.
Figure 2.
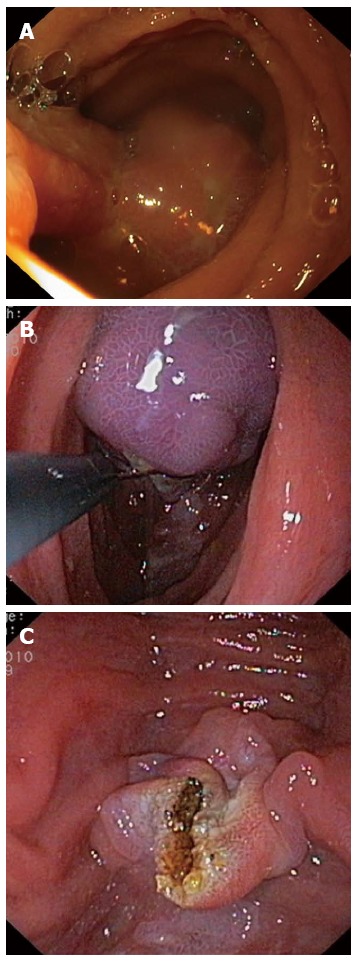
Extensive polypectomy of small bowel large polyps > 15 mm of diameter. A: Large jejunal polyp; B: Polypectomy: polyp captured with snare; C: Polyps pedicle post-polypectomy.
Figure 3.
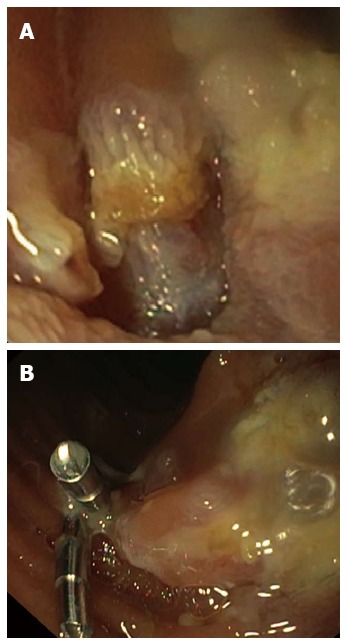
Endoscopic photograph. A: Tearing of intestinal mucosa post-polypectomy; B: Hemoclip placement.
DISCUSSION
PJS is characterized by hamartomatous polyps of small bowel predominantly located in the proximal jejunum. The majority of patients with PJS had a history of small bowel surgery. The risk of intussusception and intestinal obstruction before the age of 20 years is up to 50% in particular in patients having a large polyps > 15 mm or rapidly growing[6-8]. In the last few decades, several advanced endoscopic technique have been developed to allow a visualization of small bowel and therapeutic approach without surgery. Before the introduction of BAE, small bowel polyps were removed only by intraoperative endoscopy or surgical resection; now with BAE[9] it is possible to remove proximal end distal small bowel polyps endoscopically, preventing abdominal surgery. WCE and SBE play an important role in surveillance of patients affected by PJS. WCE is safe, well tolerated and permits to detect size, aspect and location of polyps on the entire length of the digestive tube[10,11]. In our series, all patients received upper endoscopy, ileocolonoscopy and WCE to detect polyps’ location and size before SBE procedure. WCE allows only an approximate estimation of the size of polyps; therefore, based on previous experience, we estimated polyps size according to small bowel lumen size. Katsinelos et al[12] estimated size polyps as small or large, using an open pylorus orifice (diameter 10 mm) as a reference for polyp size estimation. BAE offers diagnostic and therapeutic options for small bowel surveillance in PJS patients[9]; it is a safe procedure also in patients with previously abdominal surgery and in children[13,14]. When significant polyps are detected (> 15 mm), BAE should be the preferred method for prophylactic polypectomy[15]; Sakamoto et al[3] reported no intussusceptions developed in all pts underwent small bowel polypectomy. In our experience, endoscopic resection of small bowel large polyps was important to reduce the risk of acute intestinal intussusceptions or obstruction in all seven pts; no patients underwent small bowel resection during the surveillance. Small bowel surveillance is recommended every 2-3 years for pts with PJS from the age of 8-10 years by WCE[16] and endoscopy; removal of significant small bowel polyps reduces emergency surgery[15-17]. Our surveillance program provide a screening from 8 years or earlier if symptomatic (bleeding, abdominal pain) with upper endoscopy, colonoscopy, WCE and SBE according to WCE polyps detection. We suggest elective polypectomy with SBE when significant small bowel polyps are detected (> 15 mm) and laparotomy when polypectomy is not possible (size of polyps > 5 cm or high risk of complications). Follow up with WCE, upper endoscopy and SBE, if necessary, is recommended every 2 years in asymptomatic pts (Figure 4). Cancer predisposition in patient with PJS is known; the risk involves the small bowel, stomach, colon, pancreas and extraintestinal organs as Sertoli cells, breast and ovary. Intestinal polyps can transform in cancer; the risk is related to their dimension, even if malignant transformation is found occasionally in PJS polyps; however transformation sequence hamartoma-adenoma-carcinoma has been described[18-20]. It seems that there is no risk of tumor for the polyps smaller than one centimeter in patients with PJS[9]. No gastrointestinal tumor was found in our patients series during follow-up. In the past, one of our patients underwent surgical small bowel resection for gastrointestinal tumor, classified as a GIST at surgical specimen examination. Endoscopic polypectomy is a standardized technique and is not without risk. The hemoclip placement can be requested immediately after polyp resection[21,22]; in one of our cases hemoclip was used to avoid a post polypectomy complication due to a large tearing of small bowel mucosa. No bleeding and surgical complications have been reported after SBE procedure in our patients.
Figure 4.
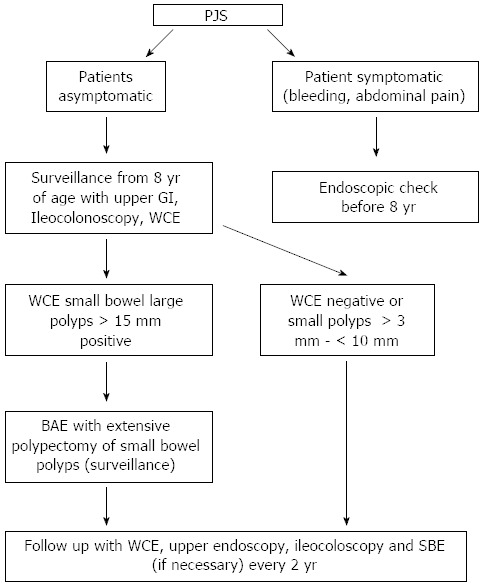
Surveillance algorithm. PJS: Peutz-Jeghers syndrome; WCE: Wireless capsule endoscopy; BAE: Balloon assisted enteroscopy; SBE: Single balloon enteroscopy. GI: Gastrointestinal.
In a conclusion, PJS is a pathological condition that require a regular follow-up and screening during the life[23,24]; WCE and SBE procedures with resection of small bowel significant polyps are useful in asymptomatic patients to avoid severe gastrointestinal bleeding and emergency laparotomy due to intussusceptions[25]. About this, we reported our surveillance program that could be useful to follow-up patients affected by PJS. The effective of prophylactic polypectomy of small bowel large polyps could be the first line treatment for conservative approach in management of PJS patients.
COMMENTS
Background
The major problems in the management of Peutz-Jeghers syndrome (PJS) are a large small-bowel polyps, which can cause intussusception and bleeding. The most of pediatric patients with PJS undergo a laparotomy for an episode of intestinal obstruction before they reached 18 years of age and a second laparotomy within 5 years. Balloon assisted enteroscopy (BAE) and wireless capsule endoscopy (WCE) play an important role for diagnostic, care and screening of a large small bowel polyps. Cancer predisposition in patient with PJS is known; transformation sequence hamartoma-adenoma-carcinoma has been described. Surveillance protocols in PJS have two main purposes: one is to detect sizeable gastroenterological polyps which could cause intussusception/obstruction or bleeding/anaemia, second is the detection of cancer at an early stage.
Research frontiers
The need for endoscopic access to improve diagnosis and treatment of small bowel disease has led to the development of novel technologies one of which is non-invasive, the video capsule, and a type of invasive technique, the device-assisted enteroscopy. Before the introduction of BAE, small bowel polyps were removed only by intraoperative endoscopy or surgical resection; now with BAE it is possible to remove proximal end distal small bowel polyps endoscopically, preventing abdominal surgery. Also WCE is a useful examination for the supervision of small intestinal polyposis and PJS; BAE and WCE are complementary investigations in the assessment of small bowel diseases that led to a radical change in their management.
Innovations and breakthroughs
The authors described a method to avoid the risk of surgery using a conservative approach proposing a surveillance algorithm in the management of patient with PJS. Surveillance program provides a screening from 8 years in asymptomatic pts or earlier (before 8 years) if symptomatic with upper endoscopy, colonoscopy, WCE and SBE according to WCE polyps detection. We suggest elective polypectomy with SBE when significant small bowel polyps are detected (> 15 mm) and laparotomy when polypectomy is not possible (size of polyps > 5 cm or high risk of complications).
Applications
The manuscript suggests that it is possible to manage PJS patients using a conservative approach with single balloon enteroscopy (SBE) and capsule endoscopy investigations. This technique should be used in dedicated pediatric endoscopy centers.
Terminology
BAE is a procedure which can allow advancement of long endoscope (200 cm) into the small bowel for diagnostic and therapeutic purposes. BAE uses one or two balloon systems. The system using two balloons is called double balloon enteroscopy and the system using a single balloon is called SBE.The procedure can be performed via the upper gastrointestinal (GI) tract (antegrade) or through the lower GI tract (retrograde).
Peer review
This study describes a safe and useful technique for treatment of small bowel large polyps in patients with polyposis syndrome. The application of the balloon assisted enteroscopy may avoid surgical intervention in patients with Peutz-Jeghers syndrome. It is well written.
Footnotes
Supported by “Generazione e Sviluppo” Onlus, ASTALDI s.p.a. and Fondazione Charlemagne Onlus
P- Reviewer: Casadesus D S- Editor: Wen LL L- Editor: A E- Editor: Zhang DN
References
- 1.Giardiello FM, Trimbath JD. Peutz-Jeghers syndrome and management recommendations. Clin Gastroenterol Hepatol. 2006;4:408–415. doi: 10.1016/j.cgh.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 2.Kopacova M, Tacheci I, Rejchrt S, Bures J. Peutz-Jeghers syndrome: diagnostic and therapeutic approach. World J Gastroenterol. 2009;15:5397–5408. doi: 10.3748/wjg.15.5397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sakamoto H, Yamamoto H, Hayashi Y, Yano T, Miyata T, Nishimura N, Shinhata H, Sato H, Sunada K, Sugano K. Nonsurgical management of small-bowel polyps in Peutz-Jeghers syndrome with extensive polypectomy by using double-balloon endoscopy. Gastrointest Endosc. 2011;74:328–333. doi: 10.1016/j.gie.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 4.Gao H, van Lier MG, Poley JW, Kuipers EJ, van Leerdam ME, Mensink PB. Endoscopic therapy of small-bowel polyps by double-balloon enteroscopy in patients with Peutz-Jeghers syndrome. Gastrointest Endosc. 2010;71:768–773. doi: 10.1016/j.gie.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 5.van Lier MG, Mathus-Vliegen EM, Wagner A, van Leerdam ME, Kuipers EJ. High cumulative risk of intussusception in patients with Peutz-Jeghers syndrome: time to update surveillance guidelines? Am J Gastroenterol. 2011;106:940–945. doi: 10.1038/ajg.2010.473. [DOI] [PubMed] [Google Scholar]
- 6.Korsse SE, Dewint P, Kuipers EJ, van Leerdam ME. Small bowel endoscopy and Peutz-Jeghers syndrome. Best Pract Res Clin Gastroenterol. 2012;26:263–278. doi: 10.1016/j.bpg.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 7.Shrivastava A, Gupta A, Gupta A, Shrivastava J. Unusual presentation of intussusception of the small bowel with peutz jeghers syndrome: report of a case. J Clin Diagn Res. 2013;7:2296–2297 ]. doi: 10.7860/JCDR/2013/5741.3503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ioannidis O, Papaemmanouil S, Paraskevas G, Kotronis A, Chatzopoulos S, Konstantara A, Papadimitriou N, Makrantonakis A, Kakoutis E. Recurrent small intestine intussusception in a patient with Peutz-Jeghers syndrome. Rev Esp Enferm Dig. 2012;104:37–39. doi: 10.4321/s1130-01082012000100009. [DOI] [PubMed] [Google Scholar]
- 9.Gorospe EC, Alexander JA, Bruining DH, Rajan E, Wong Kee Song LM. Performance of double-balloon enteroscopy for the management of small bowel polyps in hamartomatous polyposis syndromes. J Gastroenterol Hepatol. 2013;28:268–273 ]. doi: 10.1111/jgh.12058. [DOI] [PubMed] [Google Scholar]
- 10.Gastineau S, Viala J, Caldari D, Mas E, Darviot E, Le Gall C, Maurage C, Michaud L, Dabadie A. Contribution of capsule endoscopy to Peutz-Jeghers syndrome management in children. Dig Liver Dis. 2012;44:839–843. doi: 10.1016/j.dld.2012.05.018. [DOI] [PubMed] [Google Scholar]
- 11.Antunes H, Nascimento J, Peixoto P. Peutz-Jeghers syndrome: capsule endoscopy to stage disease. Lancet. 2013;381:e5. doi: 10.1016/S0140-6736(12)60830-7. [DOI] [PubMed] [Google Scholar]
- 12.Katsinelos P, Kountouras J, Chatzimavroudis G, Zavos C, Pilpilidis I, Fasoulas K, Paroutoglou G. Wireless capsule endoscopy in detecting small-intestinal polyps in familial adenomatous polyposis. World J Gastroenterol. 2009;15:6075–6079. doi: 10.3748/wjg.15.6075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aggarwal P, Kumaravel V, Upchurch BR. Single-balloon enteroscopy in managing Peutz Jeghers syndrome polyps. Therap Adv Gastroenterol. 2012;5:439–441. doi: 10.1177/1756283X12448455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Ridder L, Tabbers MM, Escher JC. Small bowel endoscopy in children. Best Pract Res Clin Gastroenterol. 2012;26:337–345. doi: 10.1016/j.bpg.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 15.Chen TH, Lin WP, Su MY, Hsu CM, Chiu CT, Chen PC, Kong MS, Lai MW, Yeh TS. Balloon-assisted enteroscopy with prophylactic polypectomy for Peutz-Jeghers syndrome: experience in Taiwan. Dig Dis Sci. 2011;56:1472–1475. doi: 10.1007/s10620-010-1464-2. [DOI] [PubMed] [Google Scholar]
- 16.Günther U, Bojarski C, Buhr HJ, Zeitz M, Heller F. Capsule endoscopy in small-bowel surveillance of patients with hereditary polyposis syndromes. Int J Colorectal Dis. 2010;25:1377–1382. doi: 10.1007/s00384-010-0982-x. [DOI] [PubMed] [Google Scholar]
- 17.Vidal I, Podevin G, Piloquet H, Le Rhun M, Frémond B, Aubert D, Leclair MD, Héloury Y. Follow-up and surgical management of Peutz-Jeghers syndrome in children. J Pediatr Gastroenterol Nutr. 2009;48:419–425. doi: 10.1097/mpg.0b013e318180af62. [DOI] [PubMed] [Google Scholar]
- 18.Gruber SB, Entius MM, Petersen GM, Laken SJ, Longo PA, Boyer R, Levin AM, Mujumdar UJ, Trent JM, Kinzler KW, et al. Pathogenesis of adenocarcinoma in Peutz-Jeghers syndrome. Cancer Res. 1998;58:5267–5270. [PubMed] [Google Scholar]
- 19.Hizawa K, Iida M, Matsumoto T, Kohrogi N, Yao T, Fujishima M. Neoplastic transformation arising in Peutz-Jeghers polyposis. Dis Colon Rectum. 1993;36:953–957. doi: 10.1007/BF02050632. [DOI] [PubMed] [Google Scholar]
- 20.Latchford AR, Phillips RK. Gastrointestinal polyps and cancer in Peutz-Jeghers syndrome: clinical aspects. Fam Cancer. 2011;10:455–461. doi: 10.1007/s10689-011-9442-1. [DOI] [PubMed] [Google Scholar]
- 21.Quintanilla E, Castro JL, Rábago LR, Chico I, Olivares A, Ortega A, Vicente C, Carbó J, Gea F. Is the use of prophylactic hemoclips in the endoscopic resection of large pedunculated polyps useful? A prospective and randomized study. J Interv Gastroenterol. 2012;2:183–188. doi: 10.4161/jig.23741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Feagins LA, Nguyen AD, Iqbal R, Spechler SJ. The prophylactic placement of hemoclips to prevent delayed post-polypectomy bleeding: an unnecessary practice? A case control study. Dig Dis Sci. 2014;59:823–828. doi: 10.1007/s10620-014-3055-0. [DOI] [PubMed] [Google Scholar]
- 23.Beggs AD, Latchford AR, Vasen HF, Moslein G, Alonso A, Aretz S, Bertario L, Blanco I, Bülow S, Burn J, et al. Peutz-Jeghers syndrome: a systematic review and recommendations for management. Gut. 2010;59:975–986. doi: 10.1136/gut.2009.198499. [DOI] [PubMed] [Google Scholar]
- 24.Bizzarri B, Borrelli O, de' Angelis N, Ghiselli A, Nervi G, Manfredi M, de' Angelis GL. Management of Duodenal-Jejunal Polyps in Children With Peutz-Jeghers Syndrome By Using Single Balloon Enteroscopy. J Pediatr Gastroenterol Nutr. 2014:Epub ahead of print. doi: 10.1097/MPG.0000000000000351. [DOI] [PubMed] [Google Scholar]
- 25.Hammad H, Esmadi M, Ahmad D, Reicks M, Rawlings A. Laparoscopic and hand-assisted deep enteroscopy with polypectomy in Peutz-Jeghers syndrome. Gastrointest Endosc. 2014;79:26. doi: 10.1016/j.gie.2013.07.044. [DOI] [PubMed] [Google Scholar]


