Abstract
Objective
The aim of this study was to review the efficacy and safety of microvascular decompression (MVD) for idiopathic trigeminal neuralgia (ITN) in elderly patients older than 65 years.
Methods
From June 2006 to June 2011, a total of 59 elderly patients with ITN underwent MVD. We performed a retrospective study of the medical records and compared the outcome data with those from 164 patients younger than 64 years during the same period.
Results
The mean age of the elderly and younger patient groups was 72 and 55 years. The pain was completely relieved in 93.2% and partially relieved in another 5.1% of the elderly patient group after surgery. The mean follow-up period was 42 months (range, 16–75 mo). A total of 8.9% of the patients in the elderly patient group experienced recurrence. Headaches, nausea, and vomiting were more frequent complications. There were no mortalities and severe morbidities after surgery. Between the elderly and younger patient groups, no statistically significant differences existed in the outcomes.
Conclusions
Microvascular decompression is a safe and effective procedure for elderly patients with ITN. It is recommended that any patients with ITN should have the opportunity to choose MVD, unless their condition cannot tolerate general anesthesia.
Key Words: Microvascular decompression, trigeminal neuralgia, elderly, safety, long-term follow-up
Idiopathic trigeminal neuralgia (ITN) is a disorder characterized by recurrent, lancinating, paroxysmal, or electric shock–like pain within the trigeminal nerve distribution. With the intensified aging population, the proportion of elderly patients with ITN is gradually increased. It makes us pay more attention to the elderly patients. Microvascular decompression (MVD) has become the first choice for medically refractory ITN due to vascular compression. Owing to the risks of posterior fossa surgery, some percutaneous procedures and radiosurgery have been proposed for a majority of elderly patients .1
The purpose of this study was to confirm the efficacy and safety of MVD for ITN in elderly patients (>65 y) and to compare the outcome with a control group (<64 y).
METHODS
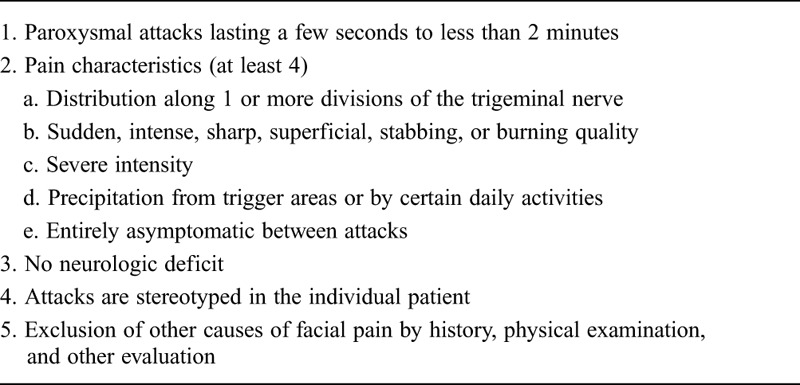
Patients with ITN operated on consecutively between June 2006 and June 2011 at the Department of Neurosurgery at Kowloon Hospital, Shanghai Jiaotong University School of Medicine, Suzhou, China, were studied. A total of 223 patients with ITN were divided into 2 groups: 59 patients older than 65 years and 164 patients younger than 64 years. The diagnosis for ITN was based on several criteria (Table 1).2,3 Magnetic resonance imaging was performed for all the patients to exclude patients with secondary TN and multiple sclerosis. Patients who had undergone previous MVD or who were in American Society of Anesthesiologists (ASA) grade III or higher were excluded at the same time.
TABLE 1.
Diagnostic Criteria for ITN
The medical records and operation videos of all patients were reviewed, and the important data were gained as follows: age, sex, preoperative general status, pain distribution and duration, compression vessel, and outcome of surgery. Follow-up was performed by outpatient clinic visits or telephone communication. The data of the elderly group were compared with those of the younger group. The project received full ethical approval from Kowloon Hospital, Shanghai Jiaotong University School of Medicine, Suzhou, China.
Operative Technique
Under general anesthesia, the patients were operated on in a lateral position. The retromastoid craniectomy was approximately 2 × 2 cm, exposing the edges of the sigmoid sinus, the transverse sinus, and their knee. The dura was opened, and cerebrospinal fluid (CSF) was slowly released to empty. The microscopic view was transferred to visualize the trigeminal nerve. The arachnoids surrounding the fifth nerve were opened sharply. With the microscopic view being transferred, the whole length of the fifth nerve from the root entry zone to the Meckel cavity was carefully explored. Conflicting vessels were dissected and moved away from the nerve, and pieces of Teflon were inserted to prevent compression again. The superior petrosal vein and its main branches were protected. If a small vein was found as the conflicting vessel, it would be coagulated and dissected. The dura was closed accurately, and the occipital bone was reconstructed.
Statistical Analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences 15.0 software (Statistical Package for the Social Sciences, Chicago, IL). Fisher exact test for statistical significance was used to analyze the outcomes including complications and pain control in the 2 groups of patients. P < 0.05 was considered statistically significant.
RESULTS
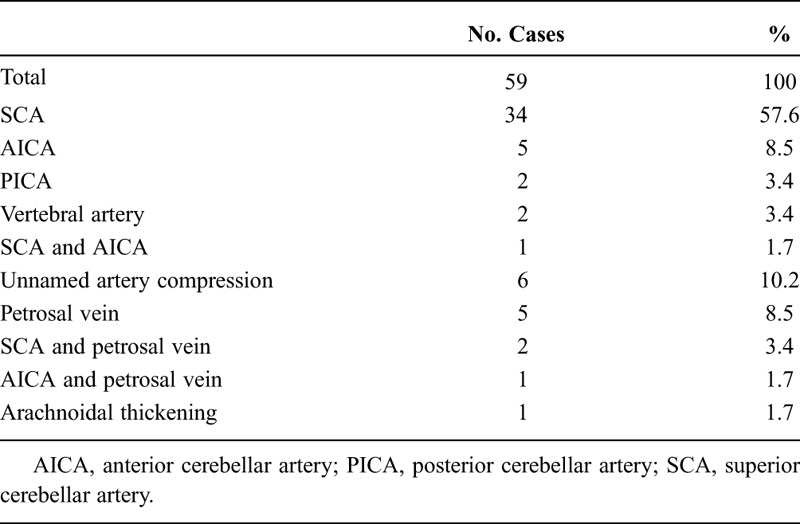
In the elderly patient group, the mean age was 72 years (range, 65–89 y). There were 31 men and 28 women. In the control group, the mean age was 55 years (36–64 y), with 75 men and 89 women. The second and third branches of the trigeminal nerve were affected most frequently in both groups. All patients were in ASA grade I or II. The superior cerebellar artery (alone or in association with other vessels) was the dominant conflicting vessel (Table 2).
TABLE 2.
Distribution of Neurovascular Compression
Outcome: Complications
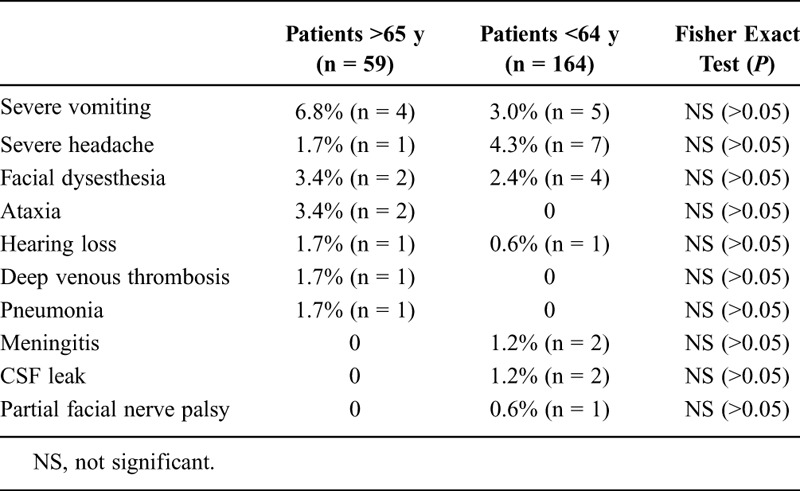
Headaches, nausea, and vomiting were more frequent complications after surgery in the 2 groups. The postoperative complications in the older group included severe vomiting in 4 patients; facial dysesthesia in 2 patients; ataxia in 2 patients; and hearing loss, deep venous thrombosis, severe headache, and pneumonia in 1 patient each.
In the younger group, the complications included severe headache in 7 patients, severe vomiting in 5 patients, facial dysesthesia in 4 patients, meningitis and CSF leak in 2 patients each, and hearing loss and partial facial nerve palsy in 1 patient each. There were no mortalities in either group.
The statistical analysis showed that no significant differences existed between the younger and older groups regarding the rate of complications (Table 3).
TABLE 3.
Complication of MVD in the 2 Patient Groups
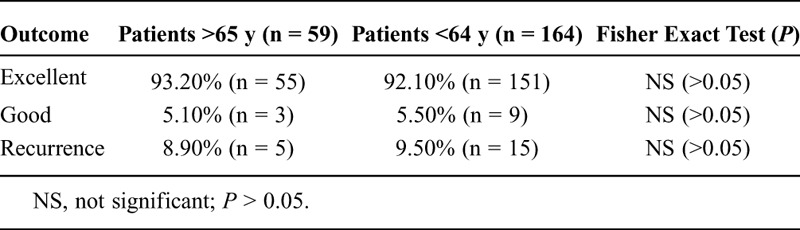
Outcome: Pain Control
The operative outcomes are considered to be excellent (complete relief) for ITN if the neuralgia became pain-free. The operative outcomes are considered to be good (partial relief) if the patients tolerated the pain well with medications or if mild pain not requiring medications still exists. The outcomes are poor in case of minimal or no relief from ITN.
In the elderly patient group, the pain was completely relieved in 93.2% and partially relieved in another 5.1% after surgery. Two patients were lost to follow-up: 1 died of cardiomyopathy and the other changed address and telephone number. A total of 8.9% of the patients experienced recurrence during a mean follow-up period of 42 months (range, 16–75 mo). The proportions of completely and partially relieved in the younger group were 92.1% and 5.5%. Three patients were lost to follow-up because of change of address and telephone number. A total of 9.5% experienced recurrence in a mean follow-up period of 45 months (range, 17–76 mo). The operative outcomes did not display any significant difference between the 2 groups (Table 4).
TABLE 4.
Pain Control in the 2 Groups
DISCUSSION
Idiopathic trigeminal neuralgia is one of the most unbearable pain disturbances. Currently, many kinds of percutaneous surgical modalities, such as thermocoagulation, balloon compression, and glycerol gangliolysis, as well as radiosurgical techniques are recommended to patients with ITN resistant to anticonvulsant medications. These treatments are performed widely, being more noninvasive and safer than posterior fossa exploration. However, there is considerable evidence to prove that neurovascular conflict plays a significant role in the pathogenesis of ITN and to recognize MVD as the sole medical and surgical management technique that directly addresses the presumed etiology of ITN. Microvascular decompression was first performed by Gardner.4 Then, Jannetta,5 using microsurgical techniques, popularized the procedure and named it. It can provide the longest-lasting pain relief and the lowest rates of facial dysesthesia and corneal reflex dysfunction. The patients always acquire immediate improvement or relief after the procedure of MVD, an occurrence as high as 95% to 97%.6,7 Meanwhile, it confers the best long-term outcome. In the largest outcome study to date, a series of 1204 patients by Barker et al8 with a mean follow-up period of 6.2 years, 70% were reported as an excellent, final result, requiring no medication to remain pain-free. The percentage of patients lost to follow-up was 13%. After the follow-up for a mean of 8.2 years, Sindou et al9 reported that the percentage to remain pain-free was 80% in a series of 330 patients.
The excellent result of MVD for ITN has been proven in large studies in the literature; however, a majority of neurosurgeons provided percutaneous or radiosurgical procedures for elderly patients on account of the risks of craniotomy. Literature2,10 evaluation of the alternative percutaneous procedures, including percutaneous radiofrequency thermocoagulation (PRT), percutaneous balloon compression, and percutaneous glycerol gangliolysis, revealed that PRT, related to the best short- and long-term outcome, was the more favorable choice than percutaneous balloon compression and percutaneous glycerol gangliolysis. However, studies comparing the efficacy of MVD with PRT showed that MVD is superior to PRT. In a comparison between MVD and PRT, Burchiel et al11 reported that 1-year pain-free rate was 90% and 65%, respectively. Tronnier et al12 compared the long-term outcome of MVD in 225 patients with that of PRT in 206 patients. The 2-year pain-free rate with MVD was 76.4%, compared with 50% with PRT. Although only 25% of patients undergoing PRT were pain-free at 4.5 years, the pain was still relieved in 63% of patients treated with MVD at 20 years. Compared with MVD and percutaneous technique, radiosurgery has become a noninvasive procedure for patients. However, it achieves the poorest immediate and long-term pain relief. After a median follow-up period of less than 18 months, Jawahar et al13 noted that only 42.3% of the patients treated with radiosurgery were pain-free.
Javadpour et al,14 in a series of 44 patients older than 70 years, demonstrated that MVD can be performed in elderly patients without causing higher morbidity and mortality when compared with younger patients. A number of studies15–18 proved that there was no significant difference between the elderly and younger patients in terms of short- and long-term pain relief. Meanwhile, the finding of posterior fossa exploration in the elderly does not differ from that in younger patients with ITN. The superior cerebellar artery alone, or in combination with a vein, was the most frequent operative finding. In our study, 98.3% and 97.6% of the patients in the elderly and younger groups, respectively, who underwent MVD acquired immediate pain relief. After a mean follow-up period of 42 months, the percentage of pain relief was 89.5% in the elderly group. A total of 88.2% of the younger patients achieved pain relief during the follow-up for a mean of 45 months. So far, no evidence demonstrates chronologic age as a predictor of adverse outcome and severe complications. There were no deaths or life-threatening morbidities in our series. Headaches, nausea, and vomiting were the most frequent complications. Other complications included hearing loss, trigeminal hyperesthesia, wound infection, cerebellar infarct/hematoma, CSF leak, and deep venous thrombosis. To decrease the occurrence of deep venous thrombosis and pneumonia, elderly patients should be encouraged to get out of bed early after operation.
Patients with ITN will experience a severe neuropathic pain condition affecting the facial area. Pain resulting from ITN is associated with a substantial patient burden, which would interfere with general activity, mood, work, and social relationships and reduce quality of life. During prolonged attacks, pain can be severe enough to induce inadequate nutrition and hydration or hypertension. More than one third of employed patients stated that ITN adversely affected their working status in terms of reduced hours, disability, or early retirement. Comorbid diseases including hypertension, diabetes, and cardiovascular disease were found in a considerable number of patients. Comorbid diseases must be paid careful attention to and treated appropriately. The general condition and risk of general anesthesia should be precisely evaluated before the operation. Anesthetist visits were very necessary to give some guidance to patients to promote anesthesia cooperation. Patients often worry about the efficacy and safety of MVD because of not being familiar with posterior fossa exploration. Sufficient and objective introduction of risks of MVD to patients is extremely necessary.
Physicians must focus on the anatomic features of elderly patients. Because of the atrophy of the cerebellum and broadening of cisterns, which give more space, exposure and exploration may be easier in elderly patients. The traction injury of cerebellar hemisphere and cranial nerves should be decreased. Incorrect and excessive retraction would damage the cerebellum and nerves, causing edema, contusion, or hematomas. These typically lead to cerebellar and nerve deficits but could have fatal results. In elderly patients, the arterial vessels are more fragile. The procedure should be particularly gentle to avoid any damage to the small perforators that supply the brain stem. Operators should suck out CSF slowly and disconnect the membrane perfectly so as to avoid the rupture of the superior petrosal veins and bridging veins even away from the surgical field. The importance of preserving the venous system has been underlined. Many of the severe morbidities and deaths in the procedure of MVD are caused by injury to the main branches of the superior petrosal veins.19,20 The whole length of the trigeminal nerve from the root entry zone to the Meckel cavity must be carefully, completely, and circumferentially inspected. The operator should take care not to overlook small vessels, whereas an unremarkable second compressive vessel may be ignored if special attention is paid to an obvious neurovascular conflict.
It is necessary to balance the efficacy and side effects of MVD in elderly patients. There were no mortalities and life-threatening cases in our series. In a series of 1590 patients treated with MVD, Kalkanis et al21 reports a mortality rate of 0.3%. It is more comparable with the 0.2% rate summarized by Sweet22 in a series of 8000 patients who underwent PRT. Meanwhile, the mortality and morbidity rates are lower after procedures performed at high-volume centers or by high-volume surgeons. With the development of anesthetic and microsurgical technique, neurosurgeons build up the confidence in MVD for patients with ITN. Meanwhile, high-resolution magnetic resonance imaging will precisely delineate the nature and location of neurovascular relationships so that neurosurgeons can prepare the procedure and evaluate patients thoroughly. Microvascular decompression is not an easy operation and requires sufficient experience and preparation. It is most important to pay attention to select candidates who are fit for general anesthesia. In our series, all patients who underwent MVD were in the ASA grade I or II. Patients with an ASA grade III or higher or not willing to take the risk of MVD were recommended to select percutaneous techniques or radiosurgery.
CONCLUSIONS
Microvascular decompression is an effective surgical option for elderly patients with ITN refractory to medication treatment and can be performed with low rate of complications. Microvascular decompression directly treats the presumed etiology and can achieve the best immediate and long-term pain relief. All elderly patients with ITN should be given the chance to select the procedure of MVD as long as they are fit for general anesthesia. The major criterion influencing the selection of treatment must be fitness and not age.
Footnotes
The authors report no conflicts of interest.
Author Contributions: Han-chun Chen and Dong-yi Jiang contributed equally to this work. De-bao Yang performed research, participated in data integrity and data analysis, and wrote the paper. Zhi-min Wang participated in study design and manuscript development. Dong-yi Jiang and Han-chun Chen participated in study design, study supervision, data analysis, and manuscript development.
REFERENCES
- 1.Laghmari M, EI Ouahabi A, Arkha Y, et al. Are the destructive neurosurgical techniques as effective as microvascular decompression in the management of trigeminal neuralgia? Surg Neurol 2007; 68: 505– 512 [DOI] [PubMed] [Google Scholar]
- 2.Cowan JA, Brahma B, Sagher O. Surgical treatment of trigeminal neuralgia: comparison of microvascular decompression, percutaneous ablation, and stereotactic radiosurgery. Techn Neurosurg 2003; 8: 157– 167 [Google Scholar]
- 3.International Headache Society. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Headache Classification Committee of the International Headache Society. Cephalalgia 1988; 8: 1– 96 [PubMed] [Google Scholar]
- 4.Gardner WJ. Concerning the mechanism of trigeminal neuralgia and hemifacial spasm. J Neurosurg 1962; 19: 947– 958 [DOI] [PubMed] [Google Scholar]
- 5.Jannetta PJ. Arterial compression of the trigeminal nerve at the pons in patients with trigeminal neuralgia. J Neurosurg 1967; 26: 159– 162 [DOI] [PubMed] [Google Scholar]
- 6.Kabatas S, Karasu A, Civelek E, et al. Microvascular decompression as a surgical management for trigeminal neuralgia: long-term follow-up and review of the literature. Neurosurg Rev 2009; 32: 87– 94 [DOI] [PubMed] [Google Scholar]
- 7.Klun B. Microvascular decompression and partial sensory rhizotomy in the treatment of trigeminal neuralgia: personal experience with 220 patients. Neurosurgery 1992; 30: 49– 52 [DOI] [PubMed] [Google Scholar]
- 8.Barker FG, Jannetta PJ, Bissonette DJ, et al. The long term outcome of microvascular decompression for trigeminal neuralgia. N Engl J Med 1996; 334: 1077– 1083 [DOI] [PubMed] [Google Scholar]
- 9.Sindou M, Leston JM, Decullier E, et al. Microvascular decompression for trigeminal neuralgia: the importance of a noncompressive technique—Kaplan-Meier analysis in a consecutive series of 330 patients. Neurosurgery 2008; 63: 341– 350 [DOI] [PubMed] [Google Scholar]
- 10.Taha JM, Tew JM., Jr Comparison of surgical treatments for trigeminal neuralgia: reevaluation of radiofrequency rhizotomy. Neurosurgery 1996; 38: 865– 871 [DOI] [PubMed] [Google Scholar]
- 11.Burchiel KJ, Steege TD, Howe JF, et al. Comparison of percutaneous radiofrequency gangliolysis and microvascular decompression for the surgical management of tic douloureux. Neurosurgery 1981; 9: 111– 119 [DOI] [PubMed] [Google Scholar]
- 12.Tronnier VM, Rasche D, Hamer J, et al. Treatment of idiopathic trigeminal neuralgia: comparison of long-term outcome after radiofrequency rhizotomy and microvascular decompression. Neurosurgery 2001; 48: 1261– 1267 [PubMed] [Google Scholar]
- 13.Jawahar A, Wadhwa R, Berk C, et al. Assessment of pain control, quality of life, and predictors of success after gamma knife surgery for the treatment of trigeminal neuralgia. Neurosurg Focus 2005; 18: E8. [DOI] [PubMed] [Google Scholar]
- 14.Javadpour M, Eldridge PR, Varma TR, et al. Microvascular decompression for trigeminal neuralgia in patients over 70 years of age. Neurology 2003; 60: 520. [DOI] [PubMed] [Google Scholar]
- 15.Ashkan K, Marsh H. Microvascular decompression for trigeminal neuralgia in the elderly: a review of the safety and efficacy. Neurosurgery 2004; 55: 840– 850 [DOI] [PubMed] [Google Scholar]
- 16.Günther T, Gerganov VM, Stieglitz L, et al. Microvascular decompression for trigeminal neuralgia in the elderly: long-term treatment outcome and comparison with younger patients. Neurosurgery 2009; 65: 477– 482 [DOI] [PubMed] [Google Scholar]
- 17.Qiang WS, Duan YP, Zhang JZ, et al. Microvascular decompression for trigeminal neuralgia in elderly patients. Chin J Neuromed 2009; 8: 399– 404 [Google Scholar]
- 18.Zhao WG, Xue YH, Shen JK, et al. Etiology of trigeminal neuralgia in elderly patients and its management with microvascular decompression. Chin J Geriatr 2005; 24: 441– 443 [Google Scholar]
- 19.Sinha D, Jagetia A, Sinha S. Brain stem infarction: a complication of microvascular decompression for trigeminal neuralgia. Neurol India 2006; 54: 325– 326 [DOI] [PubMed] [Google Scholar]
- 20.Masuoka J, Matasushima T, Hikita T, et al. Cerebellar swelling after sacrifice of the superior petrosal vein during microvascular decompression for trigeminal neuralgia. J Clin Neurosci 2009; 16: 1342– 1344 [DOI] [PubMed] [Google Scholar]
- 21.Kalkanis SN, Eskandar EN, Carter BS, et al. Microvascular decompression surgery in the United States,1996 to 2000: mortality rates, morbidity rates, and the effects of hospital and surgeon volumes. Neurosurgery 2003; 52: 1251– 1262 [DOI] [PubMed] [Google Scholar]
- 22.Sweet WH. The treatment of trigeminal neuralgia (tic douloureux). N Engl J Med 1986; 315: 174– 177 [DOI] [PubMed] [Google Scholar]


