Abstract
To evaluate the current literature about how successfully periprosthetic hip joint infections can be managed by debridement and prosthesis retention. A literature search was performed through PubMed until September 2013. Search terms were “DAIR (debridement, antibiotics, irrigation, and retention)” alone and in combination with “hip” as well as “hip infection + prosthesis retention”. A total of 11 studies reporting on 292 cases could be identified. Five different treatment modalities have been described with varying success rates (debridement-21% infection eradication rate; debridement + lavage-75% infection eradication rate; debridement, lavage, with change of modular prosthesis components-70.4% infection eradication rate; debridement, lavage, change of modular prosthesis components + vacuum-assisted closure-92.8% infection eradication rate; acetabular cup removal + spacer head onto retained stem-89.6% infection eradication rate). With regard to the postoperative antibiotic therapy, no general consensus could be drawn from the available data. Debridement, antibiotic therapy, irrigation, and prosthesis retention is an acceptable solution in the management of early and acute hematogenous periprosthetic hip joint infections. The current literature does not allow for generalization of conclusions with regard to the best treatment modality. A large, multi-center study is required for identification of the optimal treatment of these infections.
Keywords: Hip joint infection, Prosthesis retention, Debridement, Hip revision, Antibiotic therapy, Irrigation
Core tip: Infections after total hip arthroplasty are a hazardous complication. Prosthesis retention is though to be possible in case of early infections, whereas several treatment modalities might be applied. The ideal treatment procedure is still unknown. The present work reviews the current literature about how successfully periprosthetic hip joint can be managed by debridement and prosthesis retentiond and treid to shed some light onto this difficult topic.
INTRODUCTION
Despite numerous prophylactic measures infections still occur in 1%-2% after total hip arthroplasty (THA), whereas this rate may increase after revision surgery[1]. In the future, the overall infection rate is likely to increase as the life expectancy of the implants is increased and patients are followed up longer. Depending on the time of infection manifestation, duration of symptoms, virulence and antibiotic resistance profile of the pathogen organism, and the general medical condition of the patient, several treatment options are available including both one- and two-stage procedures[1].
Hip joint infections are actually categorized into early, delayed, and late infections[1]. Although these terms are widely accepted, a discrepancy regarding the precise differentiation of the time periods still exists. Some authors define early infections as those occurring within the first four[2,3] or six[1] postoperative weeks, whereas others propose the first three months to be the limit[4]. Similar to that, the definition of late infections vary from the period beyond the first four postoperative weeks[2,3] to beyond the first 24 postoperative months[4].
The correct definition of the joint infection with regard to the time of infection manifestation is important for making the correct decision about the ideal treatment procedure. Generally, it is accepted that early infections are likely to be successfully managed by debridement, lavage, and prosthesis retention, whereas late infections require prosthesis removal and one- or two-stage-reimplantation in order to achieve infection eradication[5]. However, the literature data about this topic cannot be always evaluated and compared to each other to a sufficient and reliable way due to inhomogenities in the treatment procedure, patients’ collective, antibiotic therapy or length of follow-up.
Hence, the aim of the present study was to evaluate the current literature about how successfully periprosthetic hip joint infections can be managed by debridement and prosthesis retention.
LITERATURE SEARCH
A literature search was performed through PubMed from the begin of PubMed until September 2013 (Figure 1). Search terms were “DAIR (debridement, antibiotics, irrigation, and retention)” alone and in combination with “hip” as well as “hip infection + prosthesis retention”. Only English studies were included. Reviews, case reports and case series with a number of patients < 10 were excluded from the study. Studies reporting about both hip and knee cases but not allowing for differentiation between the particular outcome were also excluded. From the identified studies, a search was carried through the bibliography of each article in order to identify further studies. All studies were analysed with regard to publication date, number of patients treated, type of infection, surgical treatment modalities, surgical complications, type and length of antibiotic therapy, follow-up, and level of evidence. Studies reporting only partly on these parameters were also excluded.
Figure 1.
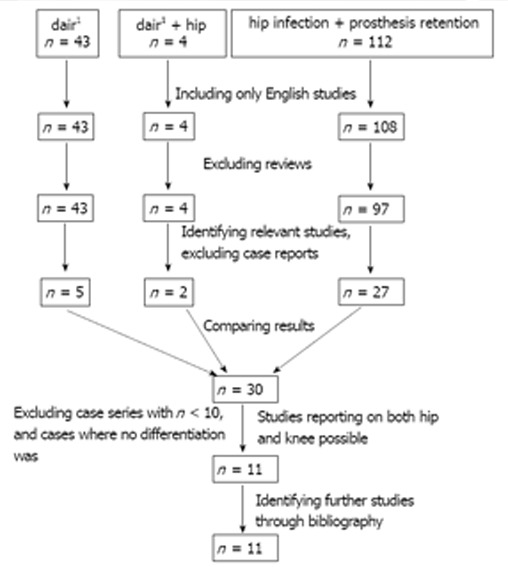
Flow chart diagram showing the single steps of literature search for identification of relevant studies. 1dair: Debridement, antibiotics, irrigation, and retention.
RESEARCH
A total of 11 studies reporting on 292 cases could be identified (Figure 1)[2-3,6-14]. Two studies were published before and nine after 2000. Two studies had a level of evidence III and nine level of evidence IV (Table 1).
Table 1.
Overview of 11 studies reporting about prosthesis retention at the site of periprosthetic hip joint infections with regard to publication year, number of patients treated, type of infection, and level of evidence
| Ref. | Publication year | Number of patients | Type of infection | Level of evidence |
| Aboltins et al[6] | 2007 | 13 | 7 early1 | IV |
| 6 late | ||||
| Aboltins et al[7] | 2013 | 19 | All early1 | III |
| Anagnostakos et al[8] | 2010 | 12 | All late2 | IV |
| Choi et al[9] | 2012 | 28 | All early3 | III |
| Crockarell et al[10] | 1998 | 42 | 19 early3 | IV |
| 19 late | ||||
| 4 acute hematogenous | ||||
| Kelm et al[11] | 2009 | 28 | All early2 | IV |
| Klouche et al[12] | 2011 | 12 | All early3 | IV |
| Lee et al[13] | 2013 | 19 | 10 late3 | IV |
| 9 acute hematogenous | ||||
| Tsukayama et al[2] | 1996 | 41 | 35 early3 | IV |
| 6 acute hematogenous | ||||
| Waagsbø et al[3] | 2009 | 40 | 30 early4 | IV |
| 10 late | ||||
| Westberg et al[14] | 2013 | 38 | Early3 | IV |
Early < 3 mo after surgery; late > 3 mo after surgery;
Early < 6 wk after surgery; late > 6 wk after surgery;
Early < 4 wk after surgery; late > 4 wk after surgery; Acute hematogenous > 4 wk after surgery due to bacteremia;
Early < 4 wk after surgery; late > 4 wk after surgery.
Of the 292 cases, there were 216 early and 57 late infections (with a variable definition of early vs. late infection). The remaining 19 cases were acute hematogenous according to the criteria by Tsukayama et al[2] (Table 1).
Regarding the treatment procedures, five different modalities have been described (Figure 2). One study[10] reported on debridement and another on debridement and irrigation[12]. Six studies performed debridement, lavage and change of modular prosthesis components (polyethylene (PE) liner, femoral stem head)[2,3,6,7,9,14], whereas in one of these studies the PE liner was not changed in all patients[9]. One study combined this procedure along with the use of the vacuum-assisted closure therapy[11]. Two studies reported on partial prosthesis retention[8,13]. In both studies, the infected acetabular cup was removed and an antibiotic-loaded spacer head was placed onto the retained femoral stem. Although it is difficult to evaluate the cumulative infection eradication rate for each procedure separately, literature data indicate a higher success rate for the two latter procedures (Figure 2).
Figure 2.
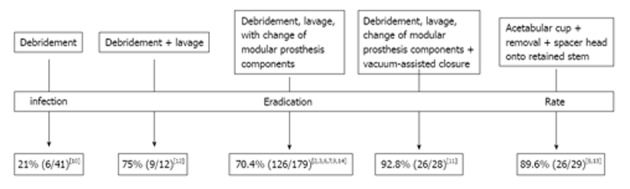
Overview of treatment procedures for management of periprosthetic hip joint infections.
Complications beside persistence of infection or emergence of new infection included mostly prosthesis dislocations and aseptic prosthesis loosening (Table 2).
Table 2.
Overview of 11 studies reporting about prosthesis retention at the site of periprosthetic hip joint infections with regard to surgical treatment modalities, -complications, infection eradication rate and length of follow-up
| Ref. | Surgical treatment procedure | Surgical complications | Infection eradication rate |
| Aboltins et al[6] | Debridement, lavage, | 1/13 aseptic prosthesis loosening | 92.30% |
| Change of PE-liner | |||
| [Median = 1 (1-4)] | |||
| Aboltins et al[7] | Debridement, lavage, | N.c.d. | 89.50% |
| Change of PE-liner | |||
| [Median = 3 (3-6)] | |||
| Anagnostakos et al[8] | Acetabular cup removal + | 2/12 draining sinus | 91.60% |
| Spacer head onto retained stem | After spacer head implantation; | ||
| Mean implantation period 88 (35-270) d | 1/12 spacer dislocation; | ||
| 3/12 prosthesis dislocation | |||
| Choi et al[9] | 19/28 debridement, irrigation, | 5/28 staged revision, | 50% |
| Change of PE-liner | 6/28 repeated debridement, | ||
| 9/28 debridement, irrigation, | 4/28 resection arthroplasty | ||
| No change of PE-liner | |||
| Crockarell et al[10] | Debridement | 1/42 prosthesis dislocation, | 21%1 |
| 1/42 periprosthetic femoral fracture, | |||
| 1/42 exitus due to sepsis | |||
| Kelm et al[11] | Debridement, pulsatile lavage, | None | 92.80% |
| Change of PE-liner, | |||
| Vacuum-assisted closure | |||
| Klouche et al[12] | Debridement, irrigation | n.r. | 75% |
| Change of PE-liner and femoral head | |||
| Lee et al[13] | Acetabular cup removal + | n.r. | 89.50% |
| Spacer head onto retained stem | |||
| Tsukayama et al[2] | Debridement, change of PE-liner | 1/35 acetabular component loosening | 71% (early) |
| 2/6 acetabular component loosening | 50% (acute hematogenous) | ||
| Waagsbø et al[3] | Debridement + prosthesis retention | n.r. | 67.50% |
| Westberg et al[14] | Debridement, pulsatile lavage, | 8/38 prosthesis dislocation | 71% |
| Change of modular prosthesis components |
PE: Polyethylene; N.c.d.: Not clearly described; n.r.: Not reported;
4/19 early successful, 2/4 acute hematogenous, 0/19 late.
With regard to the postoperative antibiotic therapy, no general consensus could be drawn from the available data (Table 3). Some studies gave only intravenous antibiotics, whereas others combined intravenous and oral antibiotics. Similar discrepancies could be observed regarding the length of antibiotic therapy, which varied from four weeks to one year (Table 3).
Table 3.
Overview of 11 studies reporting about prosthesis retention at the site of periprosthetic hip joint infections with regard to the systemic antibiotic therapy
| Study | Systemic antibiotic therapy |
| Aboltins et al[6] | All intravenous glycopeptide or beta-lactam for median 10 (3-29) d |
| All oral rifampicin+fusidic acid for median 17 (6-33) mo | |
| Aboltins et al[7] | All intravenous glycopeptide + beta-lactam for median 15 (12-34) d |
| All oral rifampicin + fucidic acid or ciprofloxacin for median 356 (230-395) d | |
| Anagnostakos et al[8] | All intravenous for 4 wk + oral for 2 wk |
| Choi et al[9] | All intravenous for 6 wk |
| Crockarell et al[10] | 41/42 intravenous for 29 (2-72) d |
| 26/42 oral after iv For 70 (5-376) d; 3/42 chronic suppression | |
| Kelm et al[11] | Intravenous for 2 wk followed by oral for 2 wk |
| Klouche et al[12] | Intravenous for 6 wk followed by oral for 6 wk |
| Lee et al[13] | Intravenous for 4-6 wk |
| Tsukayama et al[2] | Early: intravenous for 4 wk; acute hematogenous: intravenous for 6 wk |
| Waagsbø et al[3] | Overall duration of antibiotic therapy 0.1 (8.2-14.2) wk, of which intravenous 4.4 (4.2-6.1) wk |
| Westberg et al[14] | Overall duration of antibiotic therapy 7 (3-39) wk |
All studies provided a mean follow-up of at least 24 mo (Table 2). Depending on the salvage procedure used in each study, the infection eradication rate ranged from 21% to beyond 90% (Table 2).
DISCUSSION
The aim of the present study was to evaluate the current literature about how successfully periprosthetic hip joint infections can be managed by debridement and prosthesis retention. There was a low level of evidence among the 11 identified studies. Most infections were early infections, whereas a variable definition of the type of infection was evident through the studies. Five different modalities have been described with an infection eradication rate ranging from 21% to beyond 90%. With regard to the postoperative antibiotic therapy, no general consensus could be drawn from the available data about the ideal type or length of the therapy.
Periprosthetic joint infections (PJI) still remain a hazardous complication after primary and revision THA. A regimen of debridement, irrigation, prosthesis retention, and antibiotic therapy is generally accepted for acute infections without complicating factors such as significant comorbidity, not intact soft tissues surrounding the prosthesis or loosening of the prosthesis[15]. The aim of the present review was to investigate whether it is possible to treat these infections by prosthesis retention.
To the best of our knowledge, our literature search revealed 11 relevant studies. One possible cause for that might be the literature review only through PubMed and not also through other libraries. Moreover, our strict inclusion criteria led to the exclusion of numerous studies which might have provided more information and allowed for a more reliable interpretation of the data. On the other hand, more heterogenous data may not allow for meaningful conclusions. However, the purpose of the present study was to evaluate only studies reporting on hip joint infections. Several well-designed studies with a higher level of evidence report about DAIR including both THA and total knee arthroplasty (TKA) cases, whereas a differentiation of the results between both primary surgeries is not possible[15-28]. Similar to that, other studies present data only about small case series[29-31]. We represent the opinion that the proper identification of relevant studies is crucial when a systematic literature review is performed.
The findings of the present review indicate that the infection eradication rates with regard to prosthesis retention are lower compared to those reported after one- or two-stage revision surgery[5]. Although single studies demonstrated high success rate exceeding 90%, the relative small number of patients treated as well as the low level of evidence does not allow for generalization of conclusions. Two possible causes might be responsible for this lower infection eradication rate: the low power of the included patients of the identified studies, and the patients’ collectives themselves, which are different compared with those treated by one- or two-stage revision arthroplasty.
The present review identified five different treatment modalities for management of THA-PJIs with varying success rates. Especially older studies showed lower success rates compared to younger ones. This discrepancy might be possibly explained by advances in surgical and debridement techniques, introduction of the vacuum-assisted therapy, use of pulsatile lavage or even antiseptic solutions as well as application of new and more potent antimicrobial drugs. Moreover, some studies present some partly surprising results. Choi et al[9] retrospectively compared 28 cases having prosthesis retention with 65 cases having been treated by staged revision and identified risk factors for infection persistence, whereas different surgical indications were present for acute vs late infections. Infection of revision THA, acute phase treatment (less than four weeks), and polybacterial infection were identified as independent predictors for failure of infection control after initial surgery. The only risk factor associated with failure of infection control at the latest follow-up was the S. aureus microorganism. Additional subgroup analysis to identify other possible contributing factors identified no difference between methicillin-sensitive and methicillin-resistant staphylococcus or head/liner exchange and no exchange[9]. These findings are contradictory to the general acceptance that prosthesis retention is feasible at the site of early infection with a short duration of symptoms. Similar accounts for the non-significant difference between head/liner exchange and no exchange. Theoretically, the change of modular prosthesis components should reduce the bacterial load in the wound, and hence lead to better infection eradication rates. However, Choi et al[9] concluded that retention treatment can be considered an initial treatment option in selected cases of primary THA with a single organism, non-S. aureus infection with 50% chance of infection control and no disadvantages in terms of additional procedure, hospital stay, and treatment duration.
The decision with regard to the ideal treatment procedure for management of PJIs of the hip joint is made based on several factors such as time of infection manifestation, duration of symptoms, local soft-tissue situation, number of prior surgeries, identification of pathogen organism, its virulence and antibiotic resistance profile as well as patient’s comorbidities. Various risk factors have been described that are associated with occurrence of PJI, such as rheumatoid arthritis, diabetes mellitus, malignancy, obesity, and use of immunosuppressive drugs[15,20,32-34]. Revision surgery also increases the risk of PJI[17,33,34]. Factors that have been associated with a worse outcome of PJI treatment including both THA and TKA involve infections caused by Staphylococcus species[15], and more specifically by Staphylococcus aureus and methicillin-resistant Staphylococcus aureus (MRSA)[17,35-37], polymicrobial PJI[20], intra-articular purulence[15], retention of exchangeable components[20], and longer time between initial arthroplasty and PJI diagnosis[16,20,36,38].
Despite the aforementioned known risk factors the ideal treatment procedure is difficult to choose due to the definition of the infection itself. Although several classification systems have been proposed[1-4], the exact definition of an early vs. late periprosthetic infection still remains controversial. This distinguishment is essential since it is widely accepted that only early infections can be successfully treated by prosthesis retention. With regard to early as well as late infections the discrepancy between the several classification systems means that symptoms that are present for several weeks to months might not be ideally treated. The only point that all these systems agree for is the cause for the emergence of each infection[1]. Early infections are attributed to an intraoperative contamination[1]. Delayed or low-grade infections are also attributed to an intraoperative contamination, however an infection manifestation has not evolved due to a small bacteria number, low virulence of the causative organism or adverse local conditions for bacteria growth[1]. Late infections are hematogenously acquired, whereas in 20%-40% of the cases the primary infection source remains unidentified[1]. Acute hematogenous infections take a special place among periprosthetic infections. These infections occur like late infections months after the surgery, are characterized by a sudden onset of symptoms and caused by bacteremia. Practically, all these definitions are an attempt to separate surgically from nonsurgically acquired infections, and the problem is where to draw the line. Clearly, not every early infection is surgically acquired and not all late infections are from other sources[1].
Moreover, an unanswered question regards the insertion of antibiotic-loaded device (cement beads or collagen sponges) when DAIR is performed. To the best of our knowledge, the effect of antibiotic-impregnated beads at the site of DAIR has not been studied. A possible disadvantage of the insertion of beads regards the removal of the beads in an additional surgery. The use of gentamicin-loaded collagen sponges has been described in a few studies in the treatment of PJI[39-41].
The optimal antibiotic treatment (the choice and duration) of PJIs is still unknown. Some authors recommend a duration of antibiotic treatment for 6 mo for TKA-PJIs and 3 mo for THA-PJIs when treated with DAIR[4]. In some recent studies, it has been reported that a shorter course of antibiotics might be also an alternative in DAIR treatment[21,23,28,37]. This confusion regarding the optimal duration of antibiotic therapy is also evident in the present literature review. Antibiotics were administered over different periods varying from four weeks to one year. Due to the relative small power of the included cases and inhomogenities in the treatment procedures and collectives themselves it cannot be stated which antibiotic treatment is the optimal.
In conclusion, the present literature review shows that debridement, irrigation, antibiotic therapy, change of modular prosthesis components and prosthesis retention is an acceptable solution in the management of early and acute hematogenous periprosthetic hip joint infections. Factors that have been associated with a worse outcome of PJI treatment involve infections caused by Staphylococcus species, and more specifically by Staphylococcus aureus and MRSA, polymicrobial PJI, intra-articular purulence, retention of exchangeable components, and longer time between initial arthroplasty and PJI diagnosis. The current literature does not allow for generalization of conclusion with regard to the best treatment modality. A large, multi-center study is required for identification of the optimal treatment of these infections.
Footnotes
P- Reviewers: Azzoni R, Kumar P, Maheshwari AV, Tomislav S S- Editor: Wen LL L- Editor: A E- Editor: Lu YJ
References
- 1.Anagnostakos K, Schmid NV, Kelm J, Grün U, Jung J. Classification of hip joint infections. Int J Med Sci. 2009;6:227–233. doi: 10.7150/ijms.6.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tsukayama DT, Estrada R, Gustilo RB. Infection after total hip arthroplasty. A study of the treatment of one hundred and six infections. J Bone Joint Surg Am. 1996;78:512–523. doi: 10.2106/00004623-199604000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Waagsbø B, Sundøy A, Martinsen TM, Nymo LS. Treatment results with debridement and retention of infected hip prostheses. Scand J Infect Dis. 2009;41:563–568. doi: 10.1080/00365540902984719. [DOI] [PubMed] [Google Scholar]
- 4.Trampuz A, Zimmerli W. Prosthetic joint infections: update in diagnosis and treatment. Swiss Med Wkly. 2005;135:243–251. doi: 10.4414/smw.2005.10934. [DOI] [PubMed] [Google Scholar]
- 5.Fink B. Revision of late periprosthetic infections of total hip endoprostheses: pros and cons of different concepts. Int J Med Sci. 2009;6:287–295. doi: 10.7150/ijms.6.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aboltins CA, Page MA, Buising KL, Jenney AW, Daffy JR, Choong PF, Stanley PA. Treatment of staphylococcal prosthetic joint infections with debridement, prosthesis retention and oral rifampicin and fusidic acid. Clin Microbiol Infect. 2007;13:586–591. doi: 10.1111/j.1469-0691.2007.01691.x. [DOI] [PubMed] [Google Scholar]
- 7.Aboltins C, Dowsey MM, Peel T, Lim WK, Parikh S, Stanley P, Choong PF. Early prosthetic hip joint infection treated with debridement, prosthesis retention and biofilm-active antibiotics: functional outcomes, quality of life and complications. Intern Med J. 2013;43:810–815. doi: 10.1111/imj.12174. [DOI] [PubMed] [Google Scholar]
- 8.Anagnostakos K, Jung J, Kelm J, Schmitt E. Two-stage treatment protocol for isolated septic acetabular cup loosening. Hip Int. 2010;20:320–326. doi: 10.1177/112070001002000305. [DOI] [PubMed] [Google Scholar]
- 9.Choi HR, von Knoch F, Kandil AO, Zurakowski D, Moore S, Malchau H. Retention treatment after periprosthetic total hip arthroplasty infection. Int Orthop. 2012;36:723–729. doi: 10.1007/s00264-011-1324-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crockarell JR, Hanssen AD, Osmon DR, Morrey BF. Treatment of infection with débridement and retention of the components following hip arthroplasty. J Bone Joint Surg Am. 1998;80:1306–1313. doi: 10.2106/00004623-199809000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Kelm J, Schmitt E, Anagnostakos K. Vacuum-assisted closure in the treatment of early hip joint infections. Int J Med Sci. 2009;6:241–246. doi: 10.7150/ijms.6.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klouche S, Lhotellier L, Mamoudy P. Infected total hip arthroplasty treated by an irrigation-debridement/component retention protocol. A prospective study in a 12-case series with minimum 2 years’ follow-up. Orthop Traumatol Surg Res. 2011;97:134–138. doi: 10.1016/j.otsr.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 13.Lee YK, Lee KH, Nho JH, Ha YC, Koo KH. Retaining well-fixed cementless stem in the treatment of infected hip arthroplasty. Acta Orthop. 2013;84:260–264. doi: 10.3109/17453674.2013.795830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Westberg M, Grøgaard B, Snorrason F. Early prosthetic joint infections treated with debridement and implant retention: 38 primary hip arthroplasties prospectively recorded and followed for median 4 years. Acta Orthop. 2012;83:227–232. doi: 10.3109/17453674.2012.678801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kuiper JW, Vos SJ, Saouti R, Vergroesen DA, Graat HC, Debets-Ossenkopp YJ, Peters EJ, Nolte PA. Prosthetic joint-associated infections treated with DAIR (debridement, antibiotics, irrigation, and retention): analysis of risk factors and local antibiotic carriers in 91 patients. Acta Orthop. 2013;84:380–386. doi: 10.3109/17453674.2013.823589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Azzam KA, Seeley M, Ghanem E, Austin MS, Purtill JJ, Parvizi J. Irrigation and debridement in the management of prosthetic joint infection: traditional indications revisited. J Arthroplasty. 2010;25:1022–1027. doi: 10.1016/j.arth.2010.01.104. [DOI] [PubMed] [Google Scholar]
- 17.Brandt CM, Sistrunk WW, Duffy MC, Hanssen AD, Steckelberg JM, Ilstrup DM, Osmon DR. Staphylococcus aureus prosthetic joint infection treated with debridement and prosthesis retention. Clin Infect Dis. 1997;24:914–919. doi: 10.1093/clinids/24.5.914. [DOI] [PubMed] [Google Scholar]
- 18.Byren I, Bejon P, Atkins BL, Angus B, Masters S, McLardy-Smith P, Gundle R, Berendt A. One hundred and twelve infected arthroplasties treated with ‘DAIR’ (debridement, antibiotics and implant retention): antibiotic duration and outcome. J Antimicrob Chemother. 2009;63:1264–1271. doi: 10.1093/jac/dkp107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lehner B, Fleischmann W, Becker R, Jukema GN. First experiences with negative pressure wound therapy and instillation in the treatment of infected orthopaedic implants: a clinical observational study. Int Orthop. 2011;35:1415–1420. doi: 10.1007/s00264-011-1274-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lora-Tamayo J, Murillo O, Iribarren JA, Soriano A, Sánchez-Somolinos M, Baraia-Etxaburu JM, Rico A, Palomino J, Rodríguez-Pardo D, Horcajada JP, et al. A large multicenter study of methicillin-susceptible and methicillin-resistant Staphylococcus aureus prosthetic joint infections managed with implant retention. Clin Infect Dis. 2013;56:182–194. doi: 10.1093/cid/cis746. [DOI] [PubMed] [Google Scholar]
- 21.Martínez-Pastor JC, Muñoz-Mahamud E, Vilchez F, García-Ramiro S, Bori G, Sierra J, Martínez JA, Font L, Mensa J, Soriano A. Outcome of acute prosthetic joint infections due to gram-negative bacilli treated with open debridement and retention of the prosthesis. Antimicrob Agents Chemother. 2009;53:4772–4777. doi: 10.1128/AAC.00188-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moran E, Masters S, Berendt AR, McLardy-Smith P, Byren I, Atkins BL. Guiding empirical antibiotic therapy in orthopaedics: The microbiology of prosthetic joint infection managed by debridement, irrigation and prosthesis retention. J Infect. 2007;55:1–7. doi: 10.1016/j.jinf.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 23.Puhto AP, Puhto T, Syrjala H. Short-course antibiotics for prosthetic joint infections treated with prosthesis retention. Clin Microbiol Infect. 2012;18:1143–1148. doi: 10.1111/j.1469-0691.2011.03693.x. [DOI] [PubMed] [Google Scholar]
- 24.Tattevin P, Crémieux AC, Pottier P, Huten D, Carbon C. Prosthetic joint infection: when can prosthesis salvage be considered? Clin Infect Dis. 1999;29:292–295. doi: 10.1086/520202. [DOI] [PubMed] [Google Scholar]
- 25.Theis JC, Gambhir S, White J. Factors affecting implant retention in infected joint replacements. ANZ J Surg. 2007;77:877–879. doi: 10.1111/j.1445-2197.2007.04263.x. [DOI] [PubMed] [Google Scholar]
- 26.Trebse R, Pisot V, Trampuz A. Treatment of infected retained implants. J Bone Joint Surg Br. 2005;87:249–256. doi: 10.1302/0301-620x.87b2.15618. [DOI] [PubMed] [Google Scholar]
- 27.Van Kleunen JP, Knox D, Garino JP, Lee GC. Irrigation and débridement and prosthesis retention for treating acute periprosthetic infections. Clin Orthop Relat Res. 2010;468:2024–2028. doi: 10.1007/s11999-010-1291-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vilchez F, Martínez-Pastor JC, García-Ramiro S, Bori G, Maculé F, Sierra J, Font L, Mensa J, Soriano A. Outcome and predictors of treatment failure in early post-surgical prosthetic joint infections due to Staphylococcus aureus treated with debridement. Clin Microbiol Infect. 2011;17:439–444. doi: 10.1111/j.1469-0691.2010.03244.x. [DOI] [PubMed] [Google Scholar]
- 29.Estes CS, Beauchamp CP, Clarke HD, Spangehl MJ. A two-stage retention débridement protocol for acute periprosthetic joint infections. Clin Orthop Relat Res. 2010;468:2029–2038. doi: 10.1007/s11999-010-1293-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Everts RJ, Chambers ST, Murdoch DR, Rothwell AG, McKie J. Successful antimicrobial therapy and implant retention for streptococcal infection of prosthetic joints. ANZ J Surg. 2004;74:210–214. doi: 10.1111/j.1445-2197.2004.02942.x. [DOI] [PubMed] [Google Scholar]
- 31.Krasin E, Goldwirth M, Hemo Y, Gold A, Herling G, Otremski I. Could irrigation, debridement and antibiotic therapy cure an infection of a total hip arthroplasty? J Hosp Infect. 2001;47:235–238. doi: 10.1053/jhin.2000.0809. [DOI] [PubMed] [Google Scholar]
- 32.Choong PF, Dowsey MM, Carr D, Daffy J, Stanley P. Risk factors associated with acute hip prosthetic joint infections and outcome of treatment with a rifampinbased regimen. Acta Orthop. 2007;78:755–765. doi: 10.1080/17453670710014527. [DOI] [PubMed] [Google Scholar]
- 33.Bongartz T, Halligan CS, Osmon DR, Reinalda MS, Bamlet WR, Crowson CS, Hanssen AD, Matteson EL. Incidence and risk factors of prosthetic joint infection after total hip or knee replacement in patients with rheumatoid arthritis. Arthritis Rheum. 2008;59:1713–1720. doi: 10.1002/art.24060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jämsen E, Huhtala H, Puolakka T, Moilanen T. Risk factors for infection after knee arthroplasty. A register-based analysis of 43,149 cases. J Bone Joint Surg Am. 2009;91:38–47. doi: 10.2106/JBJS.G.01686. [DOI] [PubMed] [Google Scholar]
- 35.Cobo J, Miguel LG, Euba G, Rodríguez D, García-Lechuz JM, Riera M, Falgueras L, Palomino J, Benito N, del Toro MD, et al. Early prosthetic joint infection: outcomes with debridement and implant retention followed by antibiotic therapy. Clin Microbiol Infect. 2011;17:1632–1637. doi: 10.1111/j.1469-0691.2010.03333.x. [DOI] [PubMed] [Google Scholar]
- 36.Marculescu CE, Berbari EF, Hanssen AD, Steckelberg JM, Harmsen SW, Mandrekar JN, Osmon DR. Outcome of prosthetic joint infections treated with debridement and retention of components. Clin Infect Dis. 2006;42:471–478. doi: 10.1086/499234. [DOI] [PubMed] [Google Scholar]
- 37.Soriano A, García S, Bori G, Almela M, Gallart X, Macule F, Sierra J, Martínez JA, Suso S, Mensa J. Treatment of acute post-surgical infection of joint arthroplasty. Clin Microbiol Infect. 2006;12:930–933. doi: 10.1111/j.1469-0691.2006.01463.x. [DOI] [PubMed] [Google Scholar]
- 38.Barberán J, Aguilar L, Carroquino G, Giménez MJ, Sánchez B, Martínez D, Prieto J. Conservative treatment of staphylococcal prosthetic joint infections in elderly patients. Am J Med. 2006;119:993.e7–993.10. doi: 10.1016/j.amjmed.2006.03.036. [DOI] [PubMed] [Google Scholar]
- 39.Diefenbeck M, Mückley T, Hoffmann GO. Prophylaxis and treatment of implant-related infections by local apllication of antibiotics. Injury. 2006;37:S95–104. doi: 10.1016/j.injury.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 40.Swieringa AJ, Tulp NJ. Toxic serum gentamicin levels after the use of gentamicin-loaded sponges in infected total hip arthroplasty. Acta Orthop. 2005;76:75–77. doi: 10.1080/00016470510030355. [DOI] [PubMed] [Google Scholar]
- 41.Swieringa AJ, Goosen JH, Jansman FG, Tulp NJ. In vivo pharmacokinetics of a gentamicin-loaded collagen sponge in acute periprosthetic infection: serum values in 19 patients. Acta Orthop. 2008;79:637–642. doi: 10.1080/17453670810016650. [DOI] [PubMed] [Google Scholar]


