Abstract
Low level laser therapy (LLLT) is widely used during the post-operative period to accelerate the healing process. It promotes beneficial biological action on neovascularization with anti-inflammatory and analgesic effects. Two systemically healthy patients with Miller's grade II recession on 33 and 41, respectively, were treated with free gingival graft. After surgery, second patient received LLLT using a 830 nm diode laser, with output power of 0.1 W on the first day half hour following surgery, on the third day, seventh day, and lastly on the ninth day. Both the patients were asked to assess the pain on second, fourth and tenth day using a Numerical Rating Scale and revascularization of the grafted area was assessed using a color Doppler ultrasound imaging on the fourth and the ninth day. Neovascularization was noted in both the patients but the second patient elicited marked increase in vascularity on the fourth as well as the tenth day and drastic reduction in pain on day four, with no change on the tenth day. The results showed that LLLT was an effective adjunctive treatment in promoting reevascularization and pain control during early healing of free gingival graft.
Keywords: Free gingival graft, low level laser, ultrasound doppler flowmetry
INTRODUCTION
Aesthetics is an integral part of periodontal practice. The clinician has to, not only address the biological and functional periodontal problems, but also deliver therapy with acceptable aesthetics. Of all mucogingival defects, gingival recession in the anterior, visible teeth is the commonest and most challenging clinical scenario to treat.
Mucogingival surgery includes all periodontal surgical procedures designed to correct defects in the morphology, position and/or amount of gingiva surrounding the teeth.[1] Among the mucogingival procedures, free gingival graft is a versatile modality of treatment for gingival recession and still remains a gold standard. Areas of gingival recession, in the absence of a mucogingival problem, in which there is an aesthetic or root sensitivity consideration, can also be treated with a free gingival graft.
For clinical success, survival of the graft is of utmost importance. Adequate blood supply from tissue adjacent to the graft bed is critical for the “take” of the graft. Although, case selection, thickness of graft and close adaptation of graft to the recipient bed play a vital role, the vascular supply can be increased with the use of low level laser therapy (LLLT). (LLLT) has been tried in many animal studies to examine the influence of laser radiation on the wound healing process, however only in the recent past, there has been a growing interest in the use of LLLT in gingival healing following various periodontal surgical procedures. LLLT uses low-powered laser light in the range of 1-1000 mW, at wavelengths from 632-1064 nm, to stimulate a biological response. These lasers emit no heat, sound, or vibration. Instead of generating a thermal effect, LLLT acts by inducing a photochemical reaction in the cell, a process referred to as biostimulation or photobiomodulation, so the thermal effects at this wavelength are insignificant.[2] LLLT has been shown not only to accelerate wound healing by acting on the inflammatory and other cells but also by improving microcirculation.[3] Lasers also have been reported to reduce pain, resulting in minimal post-operative discomfort.[4] Therapeutic effect is produced by absorption of these wavelengths in photoreceptors within the sub-cellular components, particularly the electron transport chain within the membranes of mitochondria. This causes the activation of respiratory chain, oxidation of NADH pool, causing increased supply of ATP, resulting in stimulation of normal functions of cell.[5]
Gingival blood flow can be measured by the invasive and non-invasive methods. The former include vital microscopy of gingival margin, implantation of microspheres into the internal carotid artery in animals, infused radio isotopes and radio labeled microspheres and high speed cinematography. Doppler sonography is a non-invasive, accurate and simple technique to measure continuous microcirculatory blood flow in many tissues. It works on “Doppler Shift” principle-, measuring the frequency change that light undergoes when reflected by moving objects, such as red blood cells (RBC). It has been extensively used in various medical clinical applications, also in the field of plastic surgery to monitor blood perfusion in skin transplants and flaps.
The purpose of this case report was to compare the gingival blood flow during healing of free gingival graft with and without adjunctive low level laser therapy using ultrasound doppler flowmetry and also to evaluate the pain perception following both the procedures.
CASE REPORT
Two systemically healthy patients (Case 1: 24 year old male; Case 2: 28 year old female) with Miller's grade II recession on 33 and 41, respectively, attending our outpatient clinic, were selected for the study [Figures 1 and 2]. The treatment plan was discussed, verbal and written consent was obtained from both the patients. They received scaling and root planing 1 week prior to the surgical procedure.
Figure 1.

Grade II recession on 33
Figure 2.

Grade III recession on 41
Surgical procedure
The direct technique of free gingival graft proposed by Miller[6] was performed. After administration of local anesthesia, root planing and flattening of the root surface was done. Root conditioning with tetracycline HCl for 1 min was performed. The recipient bed was prepared with two horizontal incisions on interdental papillae adjacent to the recession. These horizontal incisions at the distal end connected the vertical incisions on either side of the recession. A split thickness flap was elevated and dissected, being careful not to expose the bone at the apical end. A tin foil was used as a template, and gingival graft was harvested for the palate following adequate anesthesia. The graft was secured at the recipient site with 5-0 silk interrupted sutures and covered with a periodontal dressing [Figure 3].
Figure 3.

FGG secured with silk sutures
Low level laser therapy
Low level laser therapy was administered to case 2, on the first day half hour following surgery, then the third day, seventh day, and lastly on the ninth day. An 830 nm Diode laser [Figure 4] was used (Picasso, AMD LASERS™, LLC, A Dentsply International Company, Tulsa OK). The laser was fired in the non-contact mode, at a distance of 1 cm, using a setting of 0.1W as a continuous wave. The treated sites received 60 s of exposure, with an energy density (calculated as power/ areax time) of 3 J/cm[2] [Figure 5]. The laser treatment was carried out with adequate eye protection for the patient, operator and the assistant.
Figure 4.

830 nm Diode laser (Picasso, AMD LASERSTM, LLC)
Figure 5.

Laser fired in the non-contact mode
Subjective pain assessment
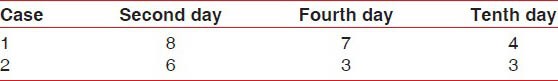
Both the patients were asked to assess the pain on second, fourth and tenth day using a Numerical Rating Scale. The NRS for pain ranged from 0 (no pain) to 10 (severe pain).
Ultrasound doppler flowmetry
This was done for both the patients on the fourth and the ninth day to assess the revascularization of the grafted area. The color Doppler ultrasound imaging was performed with an ACUSON X300™ (Seimens GE, Mountain View, CA, USA) ultrasound system, with 4D transducer technology. The probe used was a linear transducer probe (VF10-5) with 10 MHZ capacity [Figure 6]. The transducer was applied over the glove finger in a coronal plane with interspersed ultrasonic gel for proper contact [Figure 7]. The water filled glove finger served as a water media for sound waves to pass, thus providing better clarity and detail.
Figure 6.

Colour doppler linear transducer probe
Figure 7.
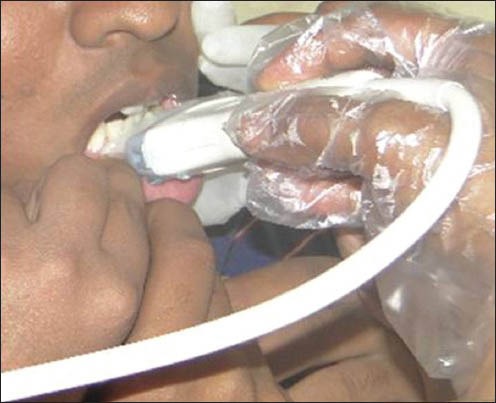
Transducer probe applied over the area of interest
RESULTS
Neovascularization was noted in both the patients on the fourth and the tenth day [Figures 8 and 9], however, in case 2, marked increase in vascularity when compared to case 1 was seen on the fourth as well as the tenth day [Figures 10 and 11]. On comparison of the pain assessment, case 2 had reduced pain on day two, four, and compared to case 1, but drastic reduction in the laser treated case was seen on day four, with no change on the tenth day [Table 1].
Figure 8.
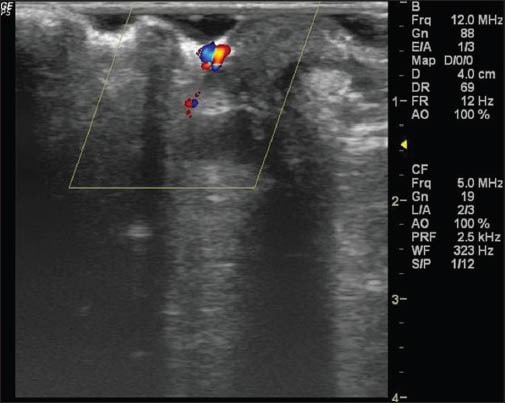
Case 1- Neovascularization on fourth day
Figure 9.
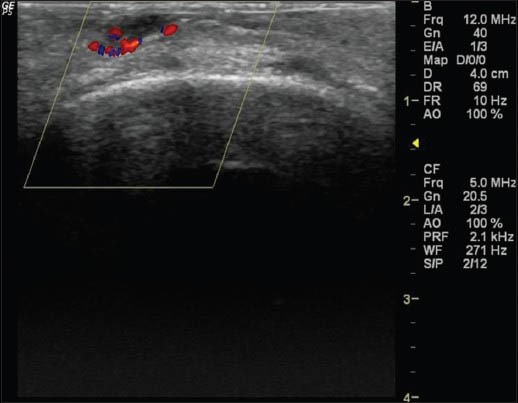
Case 2- Neovascularization on fourth day
Figure 10.
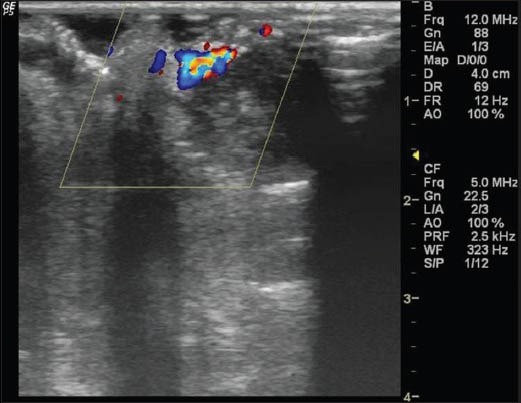
Case 1- Neovascularization on tenth day
Figure 11.
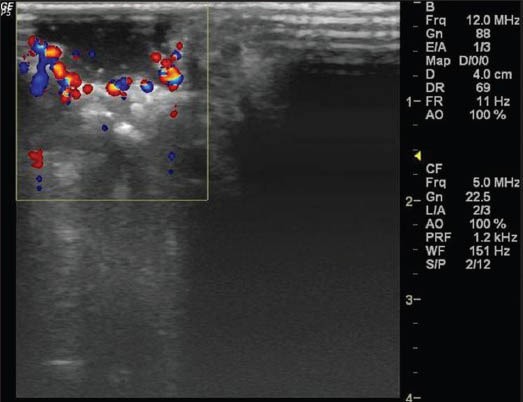
Case 2- Neovascularization on tenth day
Table 1.
Numerical rating scale for pain
DISCUSSION
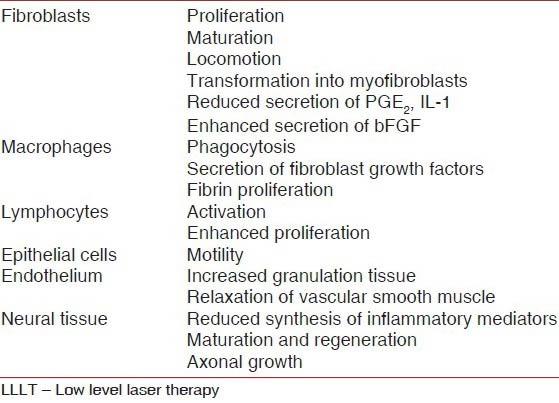
Low-level laser therapy in clinical practice has been investigated and employed for about 30 years and have shown to be beneficial. LLLT uses low-powered laser light at wavelengths from 632-1064 nm, to stimulate a biological response [Table 2]. Low level laser therapy has varied applications in dentistry, and in the field of periodontics, has been tried as an adjunct in the non-surgical treatment of chronic periodontitis.[7] It has also been studied in gingival healing after gingivectomy,[8] but to our knowledge, this is the first study to have explored the effects of LLLT on healing following FGG procedure, in terms of revascularization with the help of ultrasound Doppler flowmetry.
Table 2.
Possible mechanisms involved in the acceleration of wound healing by LLLT
In most of the studies the method used to study the blood flow is laser Doppler flowmetry. Pulpal blood flow measurements, perfusion following flap surgery, in gingival health and inflammation have been studied with laser Doppler flowmetry, but we used Doppler sonography because of the added advantage; comparison of blood flow changes between different sites in the same patient and different patients are possible. Moreover, Doppler sonography has not been tried, especially in periodontal plastic surgery, following the application of soft laser therapy.
It is a well known fact that the initial and revascularization phase are critical during the early healing of FGG (Nobuto et al. 1985).[9] In the initial phase, the graft receives nutrition from the connective tissue bed surrounding the recession, and in revascularization phase (after 4-5 days) anastomosis are established between blood vessels of the recipient bed and those in graft tissue, and is characterized by capillary proliferation. The results of the current study showed that revascularization is increased on day 4 and day 10 in patient treated with LLLT, compared to the other patient who did not receive LLLT. One of the prominent effects of LLLT during wound healing is stimulation of microcirculation. It causes vasodilatation, increasing local blood flow. It also causes relaxation of smooth muscle associated with endothelium.[10] This vasodilatation brings in oxygen and also allow for greater traffic of immune cells in to the tissue, contributing to accelerated healing. Many studies have shown that the intracellular metabolic changes resulting from biostimulation promoted by low power laser have resulted in accelerated cell division, especially of fibroblasts and epithelial and endothelial cells,[11,12] thus accounting for the improved circulation seen in our study.
The benefits of LLLT in wound healing are multi-fold. The anti-inflammatory and anti-edema effects exerted by laser occur through acceleration of microcirculation, resulting in changes in capillary hydrostatic pressure with edema reabsorption and disposal of the accumulation of intermediary metabolites.[13] Rocha Jr. et al.[14] observed a greater amount of fibroblasts in irradiated cells, showing a significant increase in fibroblast proliferation and decreased inflammatory infiltrate, concluding that LLLT accelerates the process of tissue repair. Studies by Saygun et al.[15] suggest that the biomodulation effects of LLLT may be associated with an increased production of growth factors such as bFGF and IGF-1. Literature also has shown that LLLT can be used to stimulate the growth of periodontal ligament fibroblasts.[16]
The pain quotient is also reduced in patient treated with LLLT. Though the Numerical rating scale scores are similar on day 10, pain was much less on the second and the fourth day in the LLLT treated patient. This may be attributed to the analgesic effect of LLLT. It stimulates the release of endorphins and thus inhibiting nociceptive signals and controlling pain mediators. In vivo studies of the analgesic effect of LLLT on nerves supplying the oral cavity have demonstrated that LLLT decreases the firing frequency of nociceptors, with a threshold effect seen in terms of the irradiance required to exert maximal suppression.[17]
The observed effect depends on a number of factors; power of the unit, wavelength used, distance from source to tissue, irradiation dose, exposure time, intensity, and method and number of irradiations. In this study, the selected parameters (power of 0.1W, dose of 3 J/cm2, exposure time of 60 sec fired in non-contact mode at a distance of 1 cm) on the day of surgery, third day, seventh day, and ninth day proved to be beneficial.
CONCLUSION
LLLT can be considered as a valuable adjunct to aid early healing and pain control. However, longitudinal studies with a larger sample size and different laser settings are required to validate the use of LLLT following surgery.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Friedman N. Mucogingival surgery. Tex Dent J. 1957;75:358. [Google Scholar]
- 2.Hashmi JT, Huang YY, Osmani BZ, Sharma SK, Naeser MA, Hamblin MR. Role of low level laser therapy in neurorehabilitation. PM R. 2010;(Suppl 2):S292–305. doi: 10.1016/j.pmrj.2010.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ihsan FR. Low-Level laser therapy accelerates collateral circulation and enhances microcirculation. Photomed Laser Surg. 2005;23:289–94. doi: 10.1089/pho.2005.23.289. [DOI] [PubMed] [Google Scholar]
- 4.Sato T, Kawatani M, Takeshige C, Takeshige C, Matsumoto I. Ga-Al-As laser irradiation inhibits neuronal activity associated with inflammation. Acupunct Electrother Res. 1994;19:141–51. doi: 10.3727/036012994816357312. [DOI] [PubMed] [Google Scholar]
- 5.Karu TI. Molecular mechanism of the therapeutic effect of low-intensity laser irradiation. Dokl Akad Nauk SSSR. 1986;291:1245–9. [PubMed] [Google Scholar]
- 6.Miller PD., Jr Root coverage using the free soft tissue autograft following citric acid application. III. A successful and predictable procedure in areas of deep-wide recession. Int J Periodontics Restorative Dent. 1985;5:14–37. [PubMed] [Google Scholar]
- 7.Qadri T, Miranda L, Tunér J, Gustafsson A. The short-term effects of low-level lasers as adjunct therapy in the treatment of periodontal inflammation. J Clin Periodontol. 2005;32:714–9. doi: 10.1111/j.1600-051X.2005.00749.x. [DOI] [PubMed] [Google Scholar]
- 8.Amorim JC, de Sousa GR, de Barros Silveira L, Prates RA, Pinotti M, Ribeiro MS. Clinical study of the gingiva healing after gingivectomy and low-level laser therapy. Photomed Laser Surg. 2006;24:588–94. doi: 10.1089/pho.2006.24.588. [DOI] [PubMed] [Google Scholar]
- 9.Nobuto T, Imai H, Yamaoka A. Microvascularization of the free gingival autograft. J Periodontol. 1988;59:639–46. doi: 10.1902/jop.1988.59.10.639. [DOI] [PubMed] [Google Scholar]
- 10.Walsh LJ. The current status of low level laser therapy in dentistry. Part 1. Soft tissue applications. Aust Dent J. 1997;42:247–54. doi: 10.1111/j.1834-7819.1997.tb00129.x. [DOI] [PubMed] [Google Scholar]
- 11.Rocha AM, Junior, Vieira BJ, Andrade LC, Monteiro A. Effects of low-level laser therapy on the progress of wound healing in humans: The contribution of in vitro and in vivo experimental studies. J Vasc Bras. 2007;6:258–66. [Google Scholar]
- 12.Conlan MJ, Rapley JW, Cobb CM. Biostimulation of wound healing by low-energy laser irradiation. J Clin Periodontol. 1996;23:492–6. doi: 10.1111/j.1600-051x.1996.tb00580.x. [DOI] [PubMed] [Google Scholar]
- 13.Camelo FP. Natal: Universidade Federal do Rio Grande do Norte; 2007. Avaliacao clinica do efeito da irradiacao pos-operatoria do laser de baixa intensidade na cicatrizacao de gengivoplastias em humanos [Dissertacao] [Google Scholar]
- 14.Rocha AM, Jr, Oliveira RG, Farias RE, Andrade LC, Aarestrup FM. Modulação da proliferação fibroblástica e da resposta inflamatória pela terapia a laser de baixa intensidade no processo de reparo tecidual. An Bras Dermatol. 2006;81:150–6. [Google Scholar]
- 15.Saygun I, Karacay S, Serdar M, Ural AU, Sencimen M, Kurtis B. Effects of laser irradiation on the release of basic fibroblast growth factor (bFGF), insulin like growth factor-1 (IGF-1), and receptor of IGF-1 (IGFBP3) from gingival fibroblasts. Lasers Med Sci. 2008;23:211–5. doi: 10.1007/s10103-007-0477-3. [DOI] [PubMed] [Google Scholar]
- 16.Kreisler M, Christoffers AB, Willershausen B, d’hoedt B. Effect of low-level GaAlAs laser irradiation on the proliferation rate of human periodontal ligament fibroblasts: An in vitro study. J Clin Periodontol. 2003;30:353–8. doi: 10.1034/j.1600-051x.2003.00001.x. [DOI] [PubMed] [Google Scholar]
- 17.Tsuchiya K, Kawata`ni M, Takeshige C, Matsumoto I. Laser irradiation abates neuronal responses to nociceptive stimulation of rat paw skin. Brain Res Bull. 1994;34:369–74. doi: 10.1016/0361-9230(94)90031-0. [DOI] [PubMed] [Google Scholar]


