Abstract
Pyometra is the accumulation of pus in the uterine cavity, and spontaneous perforation of pyometra resulting in generalized diffuse peritonitis is extremely uncommon. We report a rare case of diffuse peritonitis caused by spontaneous perforation of pyometra. A 66-year-old postmenopausal woman with diffuse abdominal pain and vomiting was admitted to our institution. She had a history of mixed connective-tissue disease and had been taking steroids for 20 years. Under a diagnosis of generalized peritonitis secondary to perforation of the gastrointestinal tract or uterus, supravaginal hysterectomy and bilateral salpingo-oophorectomy were performed. Unfortunately, wound dehiscence and infection occurred during the postoperative course, which were exacerbated by her immunocompromised state. Despite intensive care and a course of antibiotics, the patient died of multiple organ failure resulting from sepsis on the 36th postoperative day. Although correct diagnosis, early intervention, and proper treatment can reduce morbidity and mortality of spontaneous perforation of pyometra, if severe infection occurs, this disease can be life threatening for immunocompromised hosts.
1. Introduction
Pyometra is the accumulation of pus in the uterine cavity resulting from interference with its natural drainage [1], which may or may not be associated with malignancy. As an uncommon condition, it has been reported to occur in 0.1-0.2% of all gynecologic patients and 13.6% of elderly gynecologic outpatients [2]. Pyometra develops gradually and, as it progresses, may enlarge the uterus, causing degenerative changes that may rarely lead to sloughing of the uterine wall with subsequent spillage of contents into the abdominal cavity [3]. Spontaneous perforation of pyometra resulting in generalized diffuse peritonitis is very rare. To date, about 50 case reports of spontaneous perforation of pyometra have been documented in the English literature. This paper reports an additional case of spontaneous uterine perforation of pyometra.
2. Case Presentation
A 66-year-old multiparous postmenopausal woman was admitted because of diffuse abdominal pain and vomiting during the previous 24 hours. She had history of mixed connective-tissue disease and had been taking steroids for 20 years. In addition, she had received hemodialysis for chronic renal failure dating from 2 months previously. Her gynecologic history was unremarkable, and there was no history of postmenopausal bleeding or vaginal discharge. On physical examination, she appeared ill, with vital signs as follows: body temperature 37.3°C, blood pressure 96/61 mmHg, pulse rate 82 beats/min, and oxygen saturation 96% (oxygen mask 4 L/min). Her abdomen was distended, with tenderness in the lower portion. Vaginal examination showed no cervical and vaginal anomalies, vaginal discharge, or detectable pelvic mass. Results of laboratory investigations on admission were as follows: white blood cell (WBC) count 3.0 × 103/μL, hemoglobin 11.3 g/dL, and C-reactive protein (CRP) 7.32 mg/dL. Progression to sepsis was suspected because the WBC count documented at the previous institution was 13.0 × 103/μL, a drastic decline. A contrast-enhanced computed tomography (CT) scan showed the presence of fluid within the abdominal cavity and a significantly distended fluid-filled uterus. In addition, free air was detected in the abdominal and uterine cavities (Figure 1).
Figure 1.
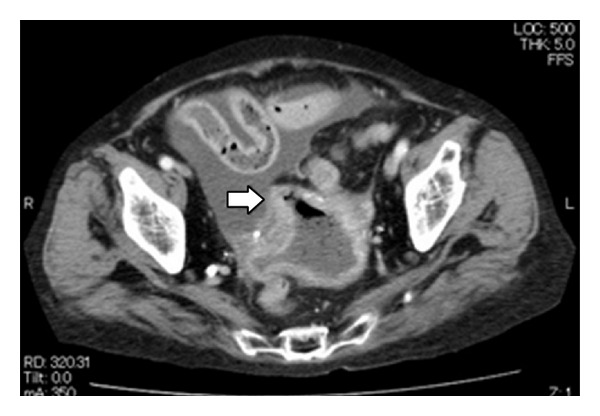
Transverse view of contrast-enhanced computed tomography scan showing the presence of fluid within the abdominal cavity and a significantly distended fluid-filled uterus. In addition, free air was detected in the abdominal and uterine cavities. White arrow indicates the perforation site.
A preoperative diagnosis of generalized peritonitis secondary to perforation of the gastrointestinal tract or uterus was established. Consequently, emergent laparotomy was performed. At laparotomy about 300 mL of seropurulent, fluid was encountered in the peritoneal cavity. No abnormal findings were found in the gastrointestinal tract; however, a perforation with a diameter of 1 cm was found in the uterine fundus. The fallopian tubes and ovaries were normal. A supravaginal hysterectomy and bilateral salpingo-oophorectomy were performed (Figure 2).
Figure 2.
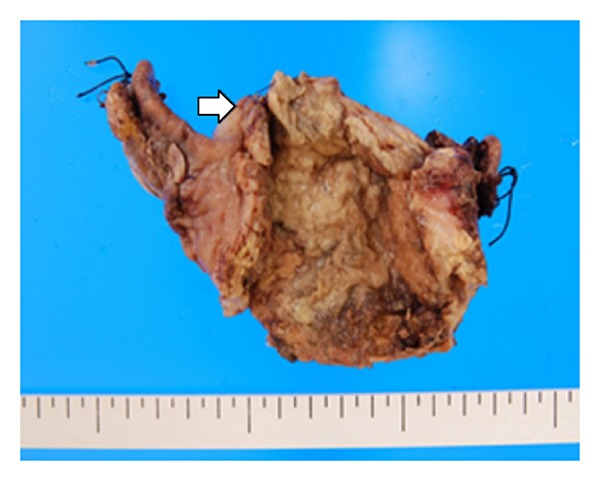
The resected corpus of the uterus. White arrow indicates the perforation site.
Culture of the pus grew Klebsiella pneumoniae, Escherichia coli, and Bacteroides fragilis. Histologic examination revealed pyometra with no evidence of malignancy. Cervical cytology performed after surgery was negative for intraepithelial lesion or malignancy.
Figure 3 shows the postoperative course. The patient was admitted to the intensive care unit with strict management of respiration and circulation. Under antibiotic therapy with doripenem (750 mg/day, daily administration), her condition improved over time and she was transferred to the gynecology unit on postoperative day (POD) 8. However, she broke into high fever on POD 9. Antibiotics were changed from doripenem to micafungin (75 mg/day, daily administration) because the culture of her sputum grew Candida albicans and β-d-glucan was increased in the blood. Subsequently, wound dehiscence occurred, and secondary wound closure was performed on POD 11. She was transferred to the intensive care unit again after surgery, and vancomycin (500 mg/day, alternate-day administration) was added to antibiotic therapy because methicillin-resistant Staphylococcus aureus was detected from wound culture. From POD 11, high fever continued and platelet count declined once again. Although hepatic and renal dysfunctions were not revealed, sepsis and multiple organ failure were suspected. Despite the readministration of doripenem, thromboses of the inferior vena cava caused by infection and cerebral infarction were found on POD 26. Although antibiotics were changed from doripenem to linezolid (600 mg/day, daily administration) or vancomycin, sepsis grew progressively worse. Despite exhaustive clinical efforts, the patient died on POD 36.
Figure 3.
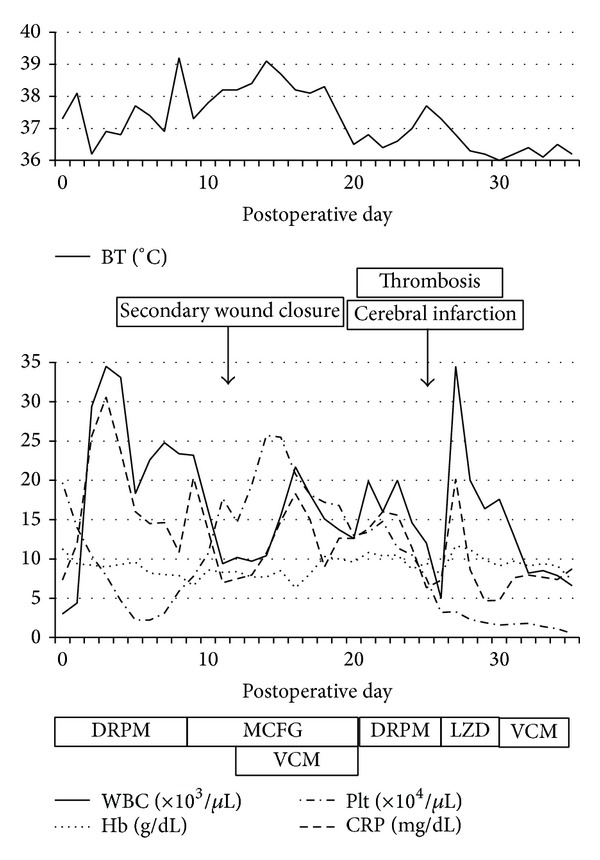
Postoperative course. BT: body temperature; WBC: white blood cell count; Hb: hemoglobin; Plt: platelet; CRP: C-reactive protein; DRPM: doripenem; MCFG: micafungin; VCM: vancomycin; LZD: linezolid.
3. Discussion
Pyometra is rare in the general population but more common in elderly women. It is caused as a result of occlusion of the cervical canal by malignant or benign tumors, surgery, radiotherapy, or senile cervicitis [11]. Pyometra is a difficult diagnosis. The classic triad of symptoms is postmenopausal bleeding, vaginal discharge, and lower abdominal pain, but none of these is specific for pyometra and some patients have no symptoms at all [29]. Spontaneous perforation of pyometra is no less rare. To date, only 50 case reports have been documented in the English literature.
A PubMed literature search using key words such as “pyometra,” “perforation,” and “rupture” was performed, and only English-language articles were collected. Table 1 summarizes the 42 cases of spontaneous perforation of pyometra during the past decade, from 2004 to 2013, including our case. The median age was 75 years (range, 40–93). The common clinical symptoms were abdominal pain (41 cases, 97.6%), fever (23 cases, 54.8%), and vomiting (13 cases, 31.0%). No case had genital bleeding and five cases (11.9%) were in shock at the time of admission. Data regarding the associated malignancy were available in all 42 cases. Of the 11 cases (26.2%) with malignant tumor, eight (72.7%) had cervical cancer and three (27.3%) had sigmoid colon cancer. Although preoperative diagnosis was confirmed in all 42 cases, an accurate preoperative diagnosis was made in only 13 cases (30.9%). The other preoperative diagnoses included perforation of the gastrointestinal tract in 20 cases (47.6%), generalized peritonitis in five cases (11.9%), appendicitis in one case (2.4%), pneumoperitoneum in one case (2.4%), mesenteric artery ischemia in one case (2.4%), and incarcerated hernia in one case (2.4%). The low preoperative diagnostic rate suggested that preoperative diagnosis of spontaneous perforation of pyometra was difficult. Laparotomy was performed in all 42 cases as an initial treatment. Total, subtotal, or supravaginal hysterectomies were performed in 37 cases (88.1%), drainage in four cases (9.5%), and surgical closure of perforated uterine wall in one case (2.4%). Data regarding the perforation site were available in 35 cases. The sites of uterine perforation were the fundus in 27 cases (77.1%), anterior in five cases (14.3%), and posterior in three cases (8.6%). Bacteriological studies of peritoneal pus were performed in 25 cases. The common etiological organisms were Escherichia coli (10 cases, 40.0%) and Bacteroides species (five cases, 20.0%). The other bacteria were Klebsiella, Streptococcus, Staphylococcus, Acinetobacter, Porphyromonas, Enterococcus, and Actinomyces species. No bacteria were detected from the culture in four cases (16.0%). Data regarding complicated diseases were available in 29 cases. Nine cases (31.0%) involved an immunocompromised state, such as renal failure, diabetes mellitus, and steroid administration. The prognoses were documented in 33 cases. The total number of patients who died was five (15.2%). Of those in an immunocompromised state, four patients died, or the mortality rate was 44.4%. This may suggest that immunocompromised hosts represent a group at high risk for spontaneous perforation of pyometra. It is hoped that further cases are accumulated and that statistical analysis is performed.
Table 1.
Cases of spontaneous perforation of pyometra from the literature review and our own case.
| Patients | First author | Age | Symptoms | Preoperative diagnosis | Associated malignancy | Perforation site | Bacterial culture | Treatment | Immunocompromised state | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Nuamah [4] | 79 | AP, F, and V | PGIT | None | Fundus | ND | TAH + BSO | ND | Died (MOF) |
| 2 | Shahid [5] | 80 | AP | PGIT | CC | Fundus | ND | TAH + BSO | ND | Survived |
| 3 | Chan [6] | 73 | AP, shock | PP | None | Fundus | Klebsiella pneumoniae, Streptococcus viridans | TAH + BSO | DM | Survived |
| 4 | Tsai [7] | 40 | AP, F | GP | None | Fundus | ND | STH | ND | Survived |
| 5 | Yildizhan [8] | 92 | AP, V | PGIT | None | Fundus | Escherichia coli, Bacteroides fragilis | TAH + BSO | ND | Survived |
| 6 | Geranpayeh [9] | 63 | AP, F, and V | PGIT | None | ND | Negative | TAH + BSO | ND | Survived |
| 7 | Lee [10] | 60 | AP, F | PGIT | CC | Fundus | B. fragilis | TAH + BSO | DM, RF | ND |
| 8 | Saha [3] | 60 | AP | PGIT | None | Fundus | Staphylococcus aureus | SVH + BSO | ND | Survived |
| 9 | Li [11] | 69 | AP, F, and V | PGIT, GP | None | Anterior | B. fragilis | SVH + BSO | None | Survived |
| 10 | Vyas [12] | 60 | AP, V | PP | CC | Fundus | Acinetobacter species | Drainage | ND | Survived |
| 11 | Izumi [13] | 83 | AP | PP | None | Fundus | Bacteroides distasonis, Porphyromonas asaccharolytica, and Streptococcus oralis | TAH | None | Survived |
| 12 | Ou [14] | 78 | AP, F | PGIT | SCC | ND | ND | TAH + BSO | ND | ND |
| 13 | 54 | AP, F | Pneumoperitoneum | None | ND | ND | TAH + BSO | ND | ND | |
| 14 | 78 | AP | PP | CC | ND | ND | TAH + BSO | ND | ND | |
| 15 | 80 | AP | PGIT | CC | ND | ND | Drainage | ND | ND | |
| 16 | 73 | AP, F | PP | CC | ND | ND | TAH + BSO | ND | ND | |
| 17 | 81 | AP, F | GP | None | ND | ND | TAH | ND | ND | |
| 18 | Kim [15] | 80 | AP | PP | None | Fundus | ND | TAH + BSO | None | Survived |
| 19 | Chen [16] | 68 | AP, F | PGIT | SCC | Fundus | ND | TAH + BSO + OME | ND | Survived |
| 20 | Agarwal [17] | 60 | AP, F | PGIT | CC | Fundus | ND | Drainage | ND | Survived |
| 21 | Stunell [18] | 64 | AP | PP | None | Fundus | ND | TAH + BSO | None | ND |
| 22 | Lim [19] | 89 | AP, F | GPIT | None | Fundus | E. coli | TAH + BSO | None | Survived |
| 23 | 87 | AP | GPIT | None | Fundus | Enterococcus faecalis | Surgical closure | None | ND | |
| 24 | Chaopotong [20] | 88 | AP, F, and V | GP | None | Fundus | Negative | TAH + BSO | DM | Died (sepsis) |
| 25 | Sahoo [21] | 50 | AP, F, and shock | GPIT | None | Fundus | ND | TAH + BSO | ND | Survived |
| 26 | Shapey [22] | 84 | AP, V | GPIT | None | Anterior | Negative | TAH | Steroid administration | Survived |
| 27 | Ikeda [23] | 80 | AP | PP | CC | Anterior | E. coli | TAH + BSO | None | Survived |
| 28 | 81 | AP, F | PGIT | None | Fundus | E. coli | TAH + BSO | None | Survived | |
| 29 | 93 | AP, F | PGIT | None | Posterior | K. pneumoniae, Enterococcus faecalis, and Streptococcus species | TAH | None | Survived | |
| 30 | 84 | AP | PGIT | SCC | Anterior | E. coli | TAH + BSO | None | Survived | |
| 31 | 74 | AP, F | PP | None | Fundus | E. coli, Staphylococcus epidermidis | STH + BSO | None | Survived | |
| 32 | 79 | AP, F | Appendicitis | None | Fundus | E. coli | TAH | None | Survived | |
| 33 | 66 | Shock | PP | None | Anterior | K. pneumoniae | Drainage | DM | Died (strangulation ileus) | |
| 34 | Kutuk [24] | 71 | AP, F, and V | GP | None | Fundus | E. coli | TAH + BSO | ND | Survived |
| 35 | 75 | AP, V | Mesenteric artery ischemia | None | Fundus | Negative | TAH + BSO | None | Survived | |
| 36 | 68 | AP | GPIT | None | Posterior | E. coli | TAH + BSO | RF | Died (sepsis) | |
| 37 | Hagiya [25] | 86 | AP, shock | PP | None | Fundus | Actinomyces species | TAH + BSO | DM | Survived |
| 38 | Mallah [26] | 78 | AP, F, and V | Incarcerated hernia | None | Fundus | ND | TAH + BSO | None | Survived |
| 39 | 61 | AP, F, V, and shock | GP | None | Posterior | ND | TAH + BSO | None | Survived | |
| 40 | Abu-Zaid [27] | 63 | AP, F, and V | PP | None | Fundus | Streptococcus constellatus | TAH + BSO | None | Survived |
| 41 | Patil [28] | 74 | AP, F | PGIT | None | Fundus | ND | TAH + BSO | DM | Survived |
| 42 | Kitai [present case] | 66 | AP, V | PP | None | Fundus | E. coli, B. fragilis | SVH + BSO | RF, steroid administration | Died (sepsis) |
AP: abdominal pain; F: fever; V: vomiting; PGIT: perforation of the gastrointestinal tract; PP: perforation of pyometra; GP: generalized peritonitis; CC: cervical cancer; SCC: sigmoid colon cancer; TAH: total abdominal hysterectomy; STH: subtotal hysterectomy; SVH: supravaginal hysterectomy; BSO: bilateral salpingo-oophorectomy; DM: diabetes mellitus; RF: renal failure; MOF: multiple organ failure.
4. Conclusion
Although correct diagnosis, early intervention, and proper treatment can reduce morbidity and mortality of spontaneous perforation of pyometra, if severe infection occurs, this disease can be life threatening for immunocompromised hosts.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- 1.Muram D, Drouin P, Thompson FE, Oxorn H. Pyometra. Canadian Medical Association Journal. 1981;125(6):589–592. [PMC free article] [PubMed] [Google Scholar]
- 2.Sawabe M, Takubo K, Esaki Y, Hatano N, Noro T, Nokubi M. Spontaneous uterine perforation as a serious complication of pyometra in elderly females. Australian and New Zealand Journal of Obstetrics and Gynaecology. 1995;35(1):87–91. doi: 10.1111/j.1479-828x.1995.tb01840.x. [DOI] [PubMed] [Google Scholar]
- 3.Saha PK, Gupta P, Mehra R, Gael P, Huria A. Spontaneous perforation of pyometra presented as an acute abdomen: a case report. MedGenMed Medscape General Medicine. 2008;10(1, article 15) [PMC free article] [PubMed] [Google Scholar]
- 4.Nuamah NM, Hamaloglu E, Konan A. Spontaneous uterine perforation due to pyometra presenting as acute abdomen. International Journal of Gynecology and Obstetrics. 2006;92(2):145–146. doi: 10.1016/j.ijgo.2005.09.027. [DOI] [PubMed] [Google Scholar]
- 5.Shahid N, Khan H, Onon TS. Perforation of pyometra leading to diffuse peritonitis is not necessarily iatrogenic. Journal of Obstetrics and Gynaecology. 2006;26(1):76–77. doi: 10.1080/01443610500419485. [DOI] [PubMed] [Google Scholar]
- 6.Chan KS, Tan CK, Mak CW, Chia CC, Kuo CY, Yu WL. Computed tomography features of spontaneously perforated pyometra: a case report. Acta Radiologica. 2006;47(2):226–227. doi: 10.1080/02841850500480634. [DOI] [PubMed] [Google Scholar]
- 7.Tsai MS, Wu MH. Images in clinical medicine. Pneumoperitoneum due to spontaneously perforated pyometra. The New England Journal of Medicine. 2006;354(21, article e23) doi: 10.1056/NEJMicm050686. [DOI] [PubMed] [Google Scholar]
- 8.Yildizhan B, Uyar E, Sişmanoğlu A, Güllüoğlu G, Kavak ZN. Spontaneous perforation of pyometra. Infectious Diseases in Obstetrics and Gynecology. 2006;2006 doi: 10.1155/IDOG/2006/26786.26786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Geranpayeh L, Fadaei-Araghi M, Shakiba B. Spontaneous uterine perforation due to pyometra presenting as acute abdomen. Infectious Diseases in Obstetrics and Gynecology. 2006;2006:2 pages. doi: 10.1155/IDOG/2006/60276.60276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee S, Huang L, Seow K, Hwang J. Spontaneous perforation of a pyometra in a postmenopausal woman with untreated cervical cancer and “forgotten” intrauterine device. Taiwanese Journal of Obstetrics and Gynecology. 2007;46(4):439–441. doi: 10.1016/s1028-4559(08)90021-8. [DOI] [PubMed] [Google Scholar]
- 11.Li C, Chang W. Spontaneous perforated Pyometra with an intrauterine device in menopause: a case report. Japanese Journal of Infectious Diseases. 2008;61(6):477–478. [PubMed] [Google Scholar]
- 12.Vyas S, Kumar A, Prakash M, Kapoor R, Kumar P, Khandelwal N. Spontaneous perforation of pyometra in a cervical cancer patient: a case report and literature review. Cancer Imaging. 2009;9(1):12–14. doi: 10.1102/1470-7330.2009.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Izumi J, Hirano H, Yoshioka H, Takisawa J. Computed tomography findings of spontaneous perforation of pyometra. Japanese Journal of Radiology. 2010;28(3):247–249. doi: 10.1007/s11604-009-0413-5. [DOI] [PubMed] [Google Scholar]
- 14.Ou YC, Lan KC, Lin H, Tsai CC, Changchien CC. Clinical characteristics of perforated pyometra and impending perforation: specific issues in gynecological emergency. Journal of Obstetrics and Gynaecology Research. 2010;36(3):661–666. doi: 10.1111/j.1447-0756.2010.01184.x. [DOI] [PubMed] [Google Scholar]
- 15.Kim J, Cho D, Kim Y, Lee J, Jeong Y. Sealed-off spontaneous perforation of a pyometra diagnosed preoperatively by magnetic resonance imaging: a case report. Journal of Magnetic Resonance Imaging. 2010;32(3):697–699. doi: 10.1002/jmri.22277. [DOI] [PubMed] [Google Scholar]
- 16.Chen P-H, Hsien-Liu, Lee S-L, Chang C-Y, Chang C-C. Pneumoperitoneum caused by perforation of pyometra associated with a lost intrauterine device and perforated malignancy of the sigmoid colon. Taiwanese Journal of Obstetrics and Gynecology. 2011;50(1):124–125. doi: 10.1016/j.tjog.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 17.Agarwal R, Suneja A, Sharma A, Vaid NB. An unusual etiology of spontaneous pyometra perforation; a case report. Journal of Reproduction and Infertility. 2011;12(3):235–238. [PMC free article] [PubMed] [Google Scholar]
- 18.Stunell H, Hou D, Finlayson S, Harris AC. Spontaneous perforation of pyometra due to acute necrotising endometritis. Journal of Obstetrics and Gynaecology. 2011;31(7):673–674. doi: 10.3109/01443615.2011.598969. [DOI] [PubMed] [Google Scholar]
- 19.Lim SF, Lee SL, Chiow AKH, Foo CS, Wong ASY, Tan SM. Rare cause of acute surgical abdomen with free intraperitoneal air: spontaneous perforated pyometra. A report of 2 cases. American Journal of Case Reports. 2012;13:55–57. doi: 10.12659/AJCR.882629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chaopotong P, Benjapibal M, Thamkhantho M. Spontaneous perforation of pyometra in an elderly woman: a case report. Journal of the Medical Association of Thailand. 2012;95(5):723–726. [PubMed] [Google Scholar]
- 21.Sahoo SP, Dora AK, Harika M, Kumar R. Spontaneous uterine perforation due to pyometra presenting as acute abdomen. Indian Journal of Surgery. 2011;73(5):370–371. doi: 10.1007/s12262-011-0265-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shapey IM, Nasser T, Dickens P, Haldar M, Solkar MH. Spontaneously perforated pyometra: an unusual cause of acute abdomen and pneumoperitoneum. Annals of the Royal College of Surgeons of England. 2012;94(8):e246–e248. doi: 10.1308/003588412X13373405387410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ikeda M, Takahashi T, Kurachi H. Spontaneous perforation of pyometra: a report of seven cases and review of the literature. Gynecologic and Obstetric Investigation. 2013;75(4):243–249. doi: 10.1159/000349981. [DOI] [PubMed] [Google Scholar]
- 24.Kutuk MS, Ozgun MT, Tas M, Uludag S. Spontaneous uterine perforation due to pyometra. Journal of Obstetrics and Gynaecology. 2013;33(3):322–323. doi: 10.3109/01443615.2012.754415. [DOI] [PubMed] [Google Scholar]
- 25.Hagiya H. Pyometra perforation caused by actinomyces without intrauterine device involvement. Case Reports in Obstetrics and Gynecology. 2013;2013:2 pages. doi: 10.1155/2013/658902.658902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mallah F, Eftekhar T, Naghavi-Behzad M. Spontaneous rupture of pyometra. Case Reports in Obstetrics and Gynecology. 2013;2013:2 pages. doi: 10.1155/2013/298383.298383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abu-Zaid A, Alomar O, Nazer A, Azzam A, Abudan Z, Al-Badawi I. Generalized peritonitis secondary to spontaneous perforation of pyometra in a 63-year-old patient. Case Reports in Obstetrics and Gynecology. 2013;2013:4 pages. doi: 10.1155/2013/929407.929407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patil V, Patil LS, Shiragur S, Ichalakaranji R. Spontaneous rupture of pyometra—a rare cause of peritonitis in elderly female. Journal of Clinical and Diagnostic Research. 2013;7(8):1735–1736. doi: 10.7860/JCDR/2013/5393.3272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hansen PT, Lindholt J. Spontaneously perforated pyometra. A differential diagnosis in acute abdomen. Annales Chirurgiae et Gynaecologiae. 1985;74(6):294–295. [PubMed] [Google Scholar]


