Abstract
Aim
Cardiopulmonary resuscitation (CPR) quality is associated with survival outcomes after out-of-hospital cardiac arrest. The objective of this study was to evaluate the effectiveness of simplified dispatcher CPR instructions to improve the chest compression (CC) quality during simulated pediatric cardiac arrest in public places.
Methods
Adult bystanders recruited in public places were randomized to receive one of two scripted dispatcher CPR instructions: (1) “Push as hard as you can” (PUSH HARD) or (2) “Push approximately 2 inches” (TWO INCHES). A pediatric manikin with realistic CC characteristics (similar to a 6-year-old child), and a CPR recording defibrillator was used for quantitative CC data collection during a 2-min simulated pediatric scenario. The primary outcome was average CC depth treated as a continuous variable. Secondary outcomes included compliance with American Heart Association (AHA) CPR targets. Analysis was by two-sided unpaired t-test and Chi-square test, as appropriate.
Results
128 out of 140 providers screened met inclusion/exclusion criteria and all 128 consented. The average CC depth (mean (SEM)) was greater in PUSH HARD compared to TWO INCHES (43 (1) vs. 36 (1) mm, p < 0.01) and met AHA targets more often (39% (25/64) vs. 20% (13/64), p = 0.02). CC rates trended higher in the PUSH HARD group (93 (4) vs. 82 (4) CC/min, p = 0.06). More providers did not achieve full chest recoil with PUSH HARD compared to TWO INCHES (53% (34/64) vs. 75% (48/64), p = 0.01).
Conclusions
Simplified dispatcher assisted pediatric CPR instructions: “Push as hard as you can” was associated with lay bystanders providing deeper and faster CCs on a simulated, 6-year-old pediatric manikin. However, percentage of providers leaning between CC increased. The potential effect of these simplified instructions in younger children remains unanswered.
Keywords: Cardiac arrest, Cardiopulmonary resuscitation, Chest compression, Dispatcher, Quality
1. Introduction
Pediatric in-hospital cardiac arrest survival outcomes have improved substantially over the past decade with nearly 40% of children having a good neurological outcome.1–3 However, survival after pediatric out-of-hospital arrest (OHCA) remains poor, with many children suffering neurological disability if they survive the initial event.4,5 Part of the reason for the substantial differences in survival rates lies in bystander cardiopulmonary resuscitation (CPR).6 Although the majority of pediatric OHCAs are witnessed, less than half will actually receive CPR, and when provided, it is of poor quality.4 As a result, the 2010 American Heart Association (AHA) Guidelines emphasized the importance of delivering high quality bystander Basic Life Support.7
Dispatcher assisted CPR is a promising approach to improve bystander CPR. Previous adult investigations revealed that instructions provided by emergency medical system (EMS) personnel via telephone improve the frequency of bystander CPR and more importantly, survival outcome.8–11 However, there is some evidence that existing dispatcher-assisted protocols could be further optimized to improve CPR quality provided by bystanders and likely as a result, patient outcomes.12–17
The ability of lay bystanders to follow dispatcher instructions given over the telephone and to provide high quality chest compressions (CCs) to a pediatric victim has not been well documented. In this investigation, we hypothesized that simplified simulated CPR instructions provided by dispatchers will result in bystanders delivering deeper chest compressions with improved compliance with 2010 AHA guidelines during simulated pediatric OHCA resuscitation.
2. Methods
2.1. Study design and population
This investigation is a prospective, randomized, simulation study. The primary objective was to evaluate the effect of simplified dispatcher-assisted CPR instructions on CPR quality provided by bystander rescuers during simulated pediatric resuscitation. The study protocol including consent procedures was approved by the institutional review board at the Children’s Hospital of Philadelphia (CHOP). All subjects provided verbal consent.
All lay volunteers older than 18 years of age were eligible for the study. We excluded subjects that were non-English speaking, had physical disabilities (including inability to kneel on the floor or inability to perform CPR for 2 min), and health care providers.
After obtaining permission by corresponding authorities, subjects were recruited in public areas of the city of Philadelphia (i.e., city parks, churches, lobbies of residential buildings) and at the lobby and common waiting areas of CHOP. Basic demographic information was obtained (age, gender, and history of prior CPR training). We did not exclude those with previous CPR training, as a population of trained and untrained CPR subjects would be a representative sample of those who might perform dispatcher assisted CPR after an OHCA.
2.2. Materials and measurements
Subjects were randomized to one of two scripted verbal CC instructions to: (1) “push as hard as you can” (PUSH HARD) or (2) “push down approximately 2 inches” (TWO INCHES). Randomization was stratified by gender and CPR experience. We used a standardized scenario and scripted instructions that were provided by a recorded voice. The voice and scripted instructions were kept identical for both groups (see Appendix 1), except for these two phrases. The only difference in the dispatcher instructions provided to the groups was regarding chest CC depth as described above. The headphones used to provide the instructions were tested with each subject before the experiment and calibrated to deliver the instructions at 75 dB. There was confirmation that all subjects were able to clearly hear the instructions before the CPR scenario was started.
A Pediatric CPR training manikin (Little Junior, Laerdal Corp., Wappinger Falls, NY, USA) was used for the CPR scenario. This manikin has an anterior–posterior chest depth of 140 mm (approximately the chest depth of a 6-year-old child), and as such, 47 mm was used as the CC depth target for AHA compliance (i.e., 1/3 anterior–posterior (AP) diameter). Each simulation evaluation session was for 2 min in duration and began with the delivery of the first chest compression. Quantitative CPR quality variables were measured by a CPR recording defibrillator (Philips Heartstart MRx defibrillator with Q-CPR technology) and included: depth (mm); rate (CC/min); count (actual number of CCs delivered per minute); and leaning (>2.5 kg).
2.3. Data analysis
A Microsoft Windows based software program, Q-CPR Review was used for the initial analysis of the quantitative chest compression data. Descriptive statistics were calculated as appropriate for the distribution of variables. Three distinct CPR epochs were prospectively designated for analysis: (1) first 5 CCs, (2) first 10 CCs, and (3) the entire 2 min simulated duration of CCs. The primary outcome of the study was chest compression depth (mm), treated as a continuous variable, and compared by Student’s t-test. Because each subject was evaluated during 3 distinct epochs, a standard Bonferroni correction was used to set the significance cutoff at 0.017 (0.05/3) for the primary outcome. Secondary outcomes included the continuous variables of CC rate, count, and percentage of CCs with leaning (>2.5 kg), and the dichotomous variables indicating compliance (Y/N) with AHA CPR targets (depth ≥1/3 anterior–posterior chest depth (47 mm); rate ≥100 CC/min; leaning < 10% of CCs). AHA compliance with 2010 AHA Guidelines was analyzed only at the 2 min epoch level by Chi square or Fisher exact tests as appropriate using p = 0.05 as the significance cut-off. Statistical analysis was completed by using Stata-IC (Version 12.0, Stata Corp., College Station, TX, USA).
3. Results
We approached a total of 140 adult bystanders. After careful screening for inclusion and exclusion criteria, 128 subjects were enrolled in the study. The 12 subjects were excluded for the following reasons: 5 subjects had physical disabilities; 3 subjects were non-English speaking; and 4 subjects opted to withdraw before starting the experiment. After stratifying for gender and CPR experience, an equal number of subjects were randomized to each group (64 PUSH HARD/64 TWO INCHES). There were no significant differences between the groups across demographic variables (Table 1). Gender and CPR experience had no significant effect on CPR quality.
Table 1.
Demographic variables.
| PUSH HARD | TWO INCHES | p | |
|---|---|---|---|
| Age: years (IQR) | 38 (25, 47) | 34 (24, 51) | 0.51 |
| Gender: male, n (%) | 29 (45) | 29 (45) | 0.99 |
| CPR experience: n (%) | 32 (50) | 33 (52) | 0.86 |
3.1. Continuous CPR quality variables
Depth
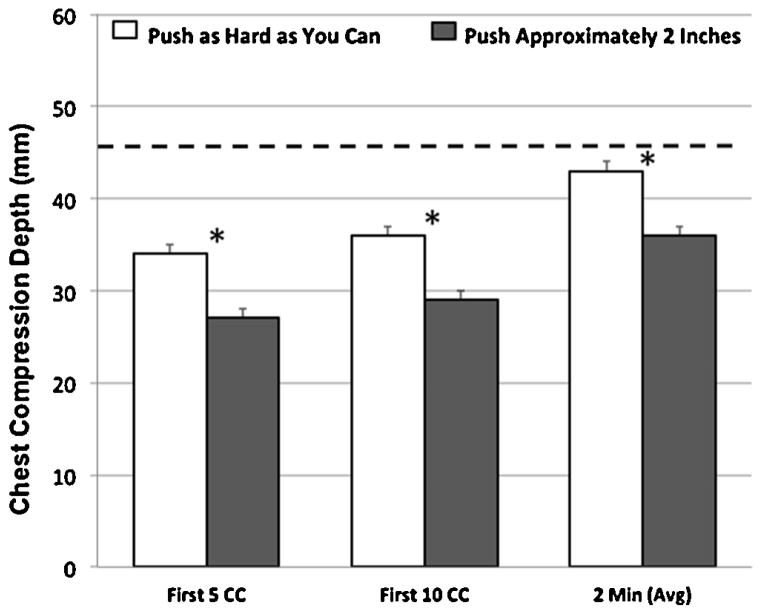
Subjects in the PUSH HARD group provided significantly deeper CCs (mean (SEM)) compared to subjects in the TWO INCHES group during the first 5 CCs (34 (1) vs. 26 (1) mm, p < 0.01), the first 10 CCs (36 (1) vs. 29 mm (1), p < 0.01), and during the entire 2 min episode (43 (1) vs. 36 (1) mm, p < 0.01) (Fig. 1).
Fig. 1.
Chest compression depth (mm) for the first 5 compressions, the first 10 compressions, and the entire 2 min evaluation session. Error bars denote standard error of the mean. CC indicates chest compression. Dotted line represents AHA target (1/3 anterior–posterior chest depth). *p < 0.01.
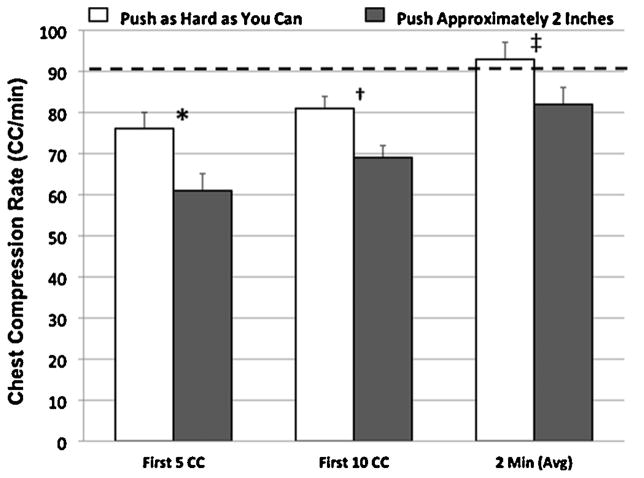
Rate
Subjects in the PUSH HARD group provided CCs of significantly higher rates (mean (SEM)) compared to subjects in the TWO INCHES group during the first 5 CCs (76 (4) vs. 61 (4) CC/min, p = 0.015) and the first 10 CCs (81 (3) vs. 69 (3) mm, p = 0.011). There was also a strong trend toward higher rates during the entire 2 min episode for PUSH HARD compared to TWO INCHES (93 (4) vs. 82 (4) CC/min, p = 0.06) (Fig. 2).
Fig. 2.
Chest compression rate (CC/min) for the first 5 compressions, the first 10 compressions, and the entire 2 min evaluation session. Error bars denote standard error of the mean. CC indicates chest compression. Dotted line represents threshold associated with adult survival (90 CC/min) [32]. *p = 0.015. †p = 0.011. ‡p = 0.06.
Count and leaning
There was no significant difference in CC count for subjects in PUSH HARD vs. TWO INCHES during the entire 2 min episode (76 (4) vs. 67 (5) CC delivered per minute, p = 0.15). There was also no difference in the percentage of CCs with leaning for subjects in PUSH HARD vs. TWO INCHES during the first 5 CCs (24 (4) vs. 21 (4)%, p = 0.67), the first 10 CCs (23 (4) vs. 20 (4)%, p < 0.26), and during the entire 2 min episode (15 (3) vs. 11 (3)%, p < 0.09) (Fig. 3).
Fig. 3.
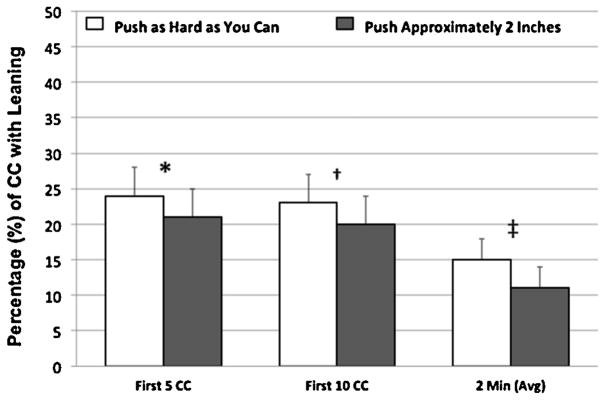
Chest compressions with significant leaning force (>2.5 kg), for the first 5 compressions, the first 10 compressions, and the entire 2 min evaluation session. Error bars denote standard error of the mean. CC indicates chest compression. *p = 0.67. †p = 0.26. ‡p = 0.09.
3.2. AHA compliance with 2010 pediatric CPR quality targets
Significantly more providers in the PUSH HARD group achieved a target CC depth of at least 1/3 anterior–posterior chest depth (47 mm) compared to the TWO INCHES group (39% (25/64) vs. 20% (13/64), p = 0.02). Compliance with AHA rate targets was not significantly different across the groups (36% (23/64) vs. 30% (19/64), p = 0.45). More providers did not achieve full chest recoil with PUSH HARD compared to TWO INCHES (53% (34/64) vs. 75% (48/64), p = 0.01). Even with scripted dispatcher instructions, only 14% of providers in the PUSH HARD group and 11% in the TWO INCHES group (p = 0.59) performed CCs that fully comply with all the current AHA recommendations (i.e., depth, rate, and leaning).
4. Discussion
This study provides further evidence that scripted and simplified dispatcher-assisted pediatric CPR instructions can significantly improve the depth and rate of chest compressions provided by lay rescuers. On average, this simplified approach improved chest compression depth by ~7 mm, an increase previously associated with improved outcomes.18–20 Importantly, this statistically significant difference was evident during the first 5 and 10 CC, suggesting that providers following simplified instructions achieve deeper and faster CCs more quickly.
The first evidence that bystander CPR quality can be improved by dispatcher-assisted CPR came from adult investigations. There are two simulation trials in adults that compared the effect of simplified scripted instructions on the quality of chest compressions provided by lay rescuers.12,13 Consistent with our results, they found that simplified instructions improved the depth of chest compressions without affecting the rate or chest recoil. The positive effect of simplified CPR instructions has also been well illustrated by the use of automatic external defibrillators (AED) by the lay public; where simplification of AED operation with voice and text prompts has reduced time to defibrillation and improved survival from out of hospital cardiac arrest in adults.21–23 While more established in the adult literature, there is little data on the influence of telephone scripts in the delivery of high quality bystander CPR in children. A retrospective study that reviewed tapes of EMS calls in Salt Lake City (UT), demonstrated that the script used by EMS dispatchers (“push down 1 inch”) to coach bystanders in pediatric CPR, resulted in a significant delay in commencing basic life support, including a 4 min delay to the provision of chest compressions.15 Likewise, an infant manikin study on telephone-based CPR performed by lay volunteers, demonstrated that none of the subjects were able to achieve the desired depth of chest compressions following the same instructions given by the EMS dispatcher (“push down 1 inch”).14 Clearly, methods to improve dispatcher-assisted CPR quality are warranted given the strong association between quality bystander CPR and improved outcomes.4,6,8–10,24
One crucial factor that potentially affects the quality of chest compressions during dispatcher assisted CPR is the ability of lay persons to actually understand the instructions.25 It is well known that even trained health care providers with appropriate coaching have difficulty estimating the force needed to achieve the target depth of 2 in.26,27 Additionally, the low incidence of cardiac arrest in the pediatric population and the added emotional distress are factors that can adversely affect the performance of chest compressions by both trained and untrained rescuers.4,28–30 For these reasons, it is important for dispatchers to provide clear and simple instructions that facilitate the rapid delivery of life saving maneuvers. Our instructions appear to have met these goals.
Of concern, our results report a significant increase in leaning between CC when subjects following simplified instructions approached target depth and rates. This finding is not surprising, since prior investigations have reported higher trends of incomplete chest recoil when subjects achieve faster31 and deeper32 chest compressions. The clinical significance of this “trade off” is unknown. The data associating CC leaning with survival comes from investigations conducted in animals,33,34 and has not been demonstrated in children. However, multiple human studies have demonstrated a strong association between CC depth and rate with survival, including observational studies in children.18–20 Thus, with our current data, the tradeoff of depth and rate at the expense of leaning seems reasonable.
This study has several limitations. First, this is a simulation-based study with a CPR manikin. As such, the testing environment is more controlled and less stressful for bystander rescuers compared to an actual pediatric resuscitation. Therefore, the effect of our simplified instructions to improve real CPR performance remains an unanswered question. Second, we used a recorded voice to standardize the dispatcher voice tone and audible volume for scripted instructions. While this was necessary to eliminate biases associated with auditory effects, we were not able to provide two-way communication between a bystander rescuer and a dispatcher. This eliminated the possibility of individualized coaching by the dispatcher. Next, the CPR manikin used in this study is known to have realistic chest compliance characteristics that mimic a real 6-year-old child during the down stroke (compression). However, the mechanical properties of chest recoil are less biofidelic, potentially affecting leaning evaluations.35
5. Conclusions
Simplified dispatcher CPR instructions to “push as hard as you can” compared to “push approximately two inches” resulted in the provision of deeper and faster chest compressions provided by lay rescuers. However, leaning increased with this simplified approach. Further study is warranted to evaluate the effect of simplified instructions to improve CPR quality during actual resuscitations and patient outcomes.
Acknowledgments
This study was supported by the Endowed Chair of Pediatric Critical Care Medicine at the Children’s Hospital of Philadelphia. We would like to thank all members of the Pediatric Intensive Care Unit and Emergency Department multidisciplinary team for supporting resuscitation research at our institution.
Abbreviations
- AHA
American Heart Association
- CPR
cardiopulmonary resuscitation
- CC
chest compression
Appendix 1
Scenario
“You are on your way to the restroom and you see a 6-year-old child who has collapsed in the hallway and is not moving nor breathing. You call his name, and there is no response trying to shake and stimulate him, there is no response. No one else is around. You shout loudly for help and rapidly dial your cell phone and call 911.”
Scripted instructions
1. PUSH 2 INCHES:
“We have geo-located you with our GPS. HELP IS ON THE WAY. STAY CALM. DON’T HANG UP… Listen carefully and I’ll tell you how to do chest compressions. Kneel down next to the child and put the heel of one of your hands on the center of the chest, right between the nipples.
PUSH DOWN approximately 2 in. Pump the chest hard and fast at least twice per second until help can take over. Let the chest come all the way up between pumps. Start now and keep doing it until help arrives and take over. I’ll stay on the line.”
“Remember: PUSH DOWN ABOUT 2 in. Pump the chest hard and fast at least twice per second until help can take over. Let the chest come all the way up between pumps.”
2. PUSH HARD:
“We have geo-located you with our GPS. HELP IS ON THE WAY. STAY CALM. DON’T HANG UP… Listen carefully and I’ll tell you how to do chest compressions. Kneel down next to the child and put the heel of one of your hands on the center of the chest, right between the nipples.
PUSH DOWN AS HARD AS YOU CAN. Pump the chest hard and fast at least twice per second until help can take over. Let the chest come all the way up between pumps. Start now and keep doing it until help arrives and take over. I’ll stay on the line.”
“Remember: PUSH AS HARD AS YOU CAN. Pump the chest hard and fast at least twice per second until help can take over. Let the chest come all the way up between pumps.”
Footnotes
A Spanish translated version of the summary of this article appears as Appendix in the final online version at http://dx.doi.org/10.1016/j.resuscitation.2013.09.003.
Conflict of interest statement
The authors acknowledge the following potential conflicts of interest. Vinay Nadkarni, Dana Niles, Akira Nishisaki, and Matt Maltese receive unrestricted research grant support from the Laerdal Foundation for Acute Care Medicine. Robert Sutton is supported through a career development award from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (K23HD062629).
References
- 1.Girotra S, Nallamothu BK, Spertus JA, et al. Trends in survival after in-hospital cardiac arrest. N Engl J Med. 2012;367:1912–20. doi: 10.1056/NEJMoa1109148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nadkarni VM, Larkin GL, Peberdy MA, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295:50–7. doi: 10.1001/jama.295.1.50. [DOI] [PubMed] [Google Scholar]
- 3.Girotra S, Spertus JA, Li Y, et al. Survival trends in pediatric in-hospital cardiac arrests: an analysis from get with the guidelines-resuscitation. Circ Cardiovasc Qual Outcomes. 2013;6:42–9. doi: 10.1161/CIRCOUTCOMES.112.967968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Atkins DL, Everson-Stewart S, Sears GK, et al. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: the resuscitation outcomes consortium epistry-cardiac arrest. Circulation. 2009;119:1484–91. doi: 10.1161/CIRCULATIONAHA.108.802678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Donoghue AJ, Nadkarni V, Berg RA, et al. Out-of-hospital pediatric cardiac arrest: an epidemiologic review and assessment of current knowledge [see comment] Ann Emerg Med. 2005;46:512–22. doi: 10.1016/j.annemergmed.2005.05.028. [DOI] [PubMed] [Google Scholar]
- 6.Lopez-Herce J, Garcia C, Dominguez P, et al. Outcome of out-of-hospital cardiorespiratory arrest in children. Pediatr Emerg Care. 2005;21:807–15. doi: 10.1097/01.pec.0000190230.43104.a8. [DOI] [PubMed] [Google Scholar]
- 7.Berg MD, Schexnayder SM, Chameides L, et al. Part 13: pediatric basic life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122:S862–75. doi: 10.1161/CIRCULATIONAHA.110.971085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akahane M, Ogawa T, Tanabe S, et al. Impact of telephone dispatcher assistance on the outcomes of pediatric out-of-hospital cardiac arrest. Crit Care Med. 2012;40:1410–6. doi: 10.1097/CCM.0b013e31823e99ae. [DOI] [PubMed] [Google Scholar]
- 9.Rea TD, Eisenberg MS, Culley LL, Becker L. Dispatcher-assisted cardiopulmonary resuscitation and survival in cardiac arrest. Circulation. 2001;104:2513–6. doi: 10.1161/hc4601.099468. [DOI] [PubMed] [Google Scholar]
- 10.Lerner EB, Rea TD, Bobrow BJ, et al. Emergency medical service dispatch cardiopulmonary resuscitation prearrival instructions to improve survival from out-of-hospital cardiac arrest: a scientific statement from the American Heart Association. Circulation. 2012;125:648–55. doi: 10.1161/CIR.0b013e31823ee5fc. [DOI] [PubMed] [Google Scholar]
- 11.Vaillancourt C, Verma A, Trickett J, et al. Evaluating the effectiveness of dispatch-assisted cardiopulmonary resuscitation instructions. Acad Emerg Med. 2007;14:877–83. doi: 10.1197/j.aem.2007.06.021. [DOI] [PubMed] [Google Scholar]
- 12.Dias JA, Brown TB, Saini D, et al. Simplified dispatch-assisted CPR instructions outperform standard protocol. Resuscitation. 2007;72:108–14. doi: 10.1016/j.resuscitation.2006.04.018. [DOI] [PubMed] [Google Scholar]
- 13.Mirza M, Brown TB, Saini D, et al. Instructions to push as hard as you can improve average chest compression depth in dispatcher-assisted cardiopulmonary resuscitation. Resuscitation. 2008;79:97–102. doi: 10.1016/j.resuscitation.2008.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dawkins S, Deakin CD, Baker K, Cheung S, Petley GW, Clewlow F. A prospective infant manikin-based observational study of telephone-cardiopulmonary resuscitation. Resuscitation. 2008;76:63–8. doi: 10.1016/j.resuscitation.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 15.Deakin CD, Evans S, King P. Evaluation of telephone-cardiopulmonary resuscitation advice for paediatric cardiac arrest. Resuscitation. 2010;81:853–6. doi: 10.1016/j.resuscitation.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 16.Deakin CD, Cheung S, Petley GW, Clewlow F. Assessment of the quality of cardiopulmonary resuscitation following modification of a standard telephone-directed protocol. Resuscitation. 2007;72:436–43. doi: 10.1016/j.resuscitation.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 17.Cheung S, Deakin CD, Hsu R, Petley GW, Clewlow F. A prospective manikin-based observational study of telephone-directed cardiopulmonary resuscitation. Resuscitation. 2007;72:425–35. doi: 10.1016/j.resuscitation.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 18.Kramer-Johansen J, Myklebust H, Wik L, et al. Quality of out-of-hospital cardiopulmonary resuscitation with real time automated feedback: a prospective interventional study. Resuscitation. 2006;71:283–92. doi: 10.1016/j.resuscitation.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 19.Edelson DP, Abella BS, Kramer-Johansen J, et al. Effects of compression depth and pre-shock pauses predict defibrillation failure during cardiac arrest. Resuscitation. 2006;71:137–45. doi: 10.1016/j.resuscitation.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 20.Stiell IG, Brown SP, Christenson J, et al. What is the role of chest compression depth during out-of-hospital cardiac arrest resuscitation? Crit Care Med. 2012;40:1142–98. doi: 10.1097/CCM.0b013e31823bc8bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marenco JP, Wang PJ, Link MS, Homoud MK, Estes NA., III Improving survival from sudden cardiac arrest: the role of the automated external defibrillator. JAMA. 2001;285:1193–200. doi: 10.1001/jama.285.9.1193. [DOI] [PubMed] [Google Scholar]
- 22.Beckers S, Fries M, Bickenbach J, Derwall M, Kuhlen R, Rossaint R. Minimal instructions improve the performance of laypersons in the use of semiautomatic and automatic external defibrillators. Crit Care. 2005;9:R110–6. doi: 10.1186/cc3033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sanna T, La Torre G, de Waure C, et al. Cardiopulmonary resuscitation alone vs. cardiopulmonary resuscitation plus automated external defibrillator use by non-healthcare professionals: a meta-analysis on 1583 cases of out-of-hospital cardiac arrest. Resuscitation. 2008;76:226–32. doi: 10.1016/j.resuscitation.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 24.Lopez-Herce J, Carrillo A. How can we improve the results of cardiopulmonary resuscitation in out-of-hospital cardiac arrest in children? Dispatcher-assisted cardiopulmonary resuscitation is a link in the chain of survival. Crit Care Med. 2012;40:1646–7. doi: 10.1097/CCM.0b013e31824317d1. [DOI] [PubMed] [Google Scholar]
- 25.Bradley SM, Fahrenbruch CE, Meischke H, Allen J, Bloomingdale M, Rea TD. Bystander CPR in out-of-hospital cardiac arrest: the role of limited english proficiency. Resuscitation. 2011;82:680–4. doi: 10.1016/j.resuscitation.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 26.Tomlinson AE, Nysaether J, Kramer-Johansen J, Steen PA, Dorph E. Compression force–depth relationship during out-of-hospital cardiopulmonary resuscitation. Resuscitation. 2007;72:364–70. doi: 10.1016/j.resuscitation.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 27.Odegaard S, Kramer-Johansen J, Bromley A, et al. Chest compressions by ambulance personnel on chests with variable stiffness: abilities and attitudes. Resuscitation. 2007;74:127–34. doi: 10.1016/j.resuscitation.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 28.Moler FW, Donaldson AE, Meert K, et al. Multicenter cohort study of out-of-hospital pediatric cardiac arrest. Crit Care Med. 2011;39:141–9. doi: 10.1097/CCM.0b013e3181fa3c17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vaillancourt C, Stiell IG, Wells GA. Understanding and improving low bystander CPR rates: a systematic review of the literature. CJEM. 2008;10:51–65. doi: 10.1017/s1481803500010010. [DOI] [PubMed] [Google Scholar]
- 30.Donoghue AJ, Nadkarni VM, Elliott M, Durbin D American Heart Assocation National Registry of Cardiopulmonary Resuscitation, Investigators. Effect of hospital characteristics on outcomes from pediatric cardiopulmonary resuscitation: a report from the national registry of cardiopulmonary resuscitation. Pediatrics. 2006;118:995–1001. doi: 10.1542/peds.2006-0453. [DOI] [PubMed] [Google Scholar]
- 31.Field RA, Soar J, Davies RP, Akhtar N, Perkins JD. The impact of chest compressions rate on quality of chest compressions–a manikin study. Resuscitation. 2012;83:360–4. doi: 10.1016/j.resuscitation.2011.07.012. [DOI] [PubMed] [Google Scholar]
- 32.Edelson DP, Edelson DP, Call SL, Yuen TC, Vanden Hoek TL. The impact of step stool on cardiopulmonary resuscitation: a cross-over mannequin study. Resuscitation. 2012;83:874–8. doi: 10.1016/j.resuscitation.2012.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yannopoulos D, McKnite S, Aufderheide TP, et al. Effects of incomplete chest wall decompression during cardiopulmonary resuscitation on coronary and cerebral perfusion pressures in a porcine model of cardiac arrest. Resuscitation. 2005;64:363–72. doi: 10.1016/j.resuscitation.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 34.Zuercher M, Hilwig RW, Ranger-Moore J, et al. Leaning during chest compressions impairs cardiac output and left ventricular myocardial blood flow in piglet cardiac arrest. Crit Care Med. 2010;38:1141–6. doi: 10.1097/CCM.0b013e3181ce1fe2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Arbogast KB, Nishisaki A, Balasubramanian S, et al. Expert clinical assessment of thorax stiffness of infants and children during chest compressions. Resuscitation. 2009;80:1187–91. doi: 10.1016/j.resuscitation.2009.07.005. [DOI] [PubMed] [Google Scholar]