Femoral vessels are the most used peripheral vessels for veno-arterial Extracorporeal Membrane Oxygenation (ECMO) support in adults and older children. They are easily harvested and are associated with a low incidence of neurological events.
In order to reduce bleeding and infection, the percutaneous technique is usually preferred to the open technique. Nevertheless this is associated to possible lower leg extremity ischemia [1] which is most commonly dealt with by using distal perfusion catheters [2]. However, despite the use of such catheters, ischemic complications are still described [3].
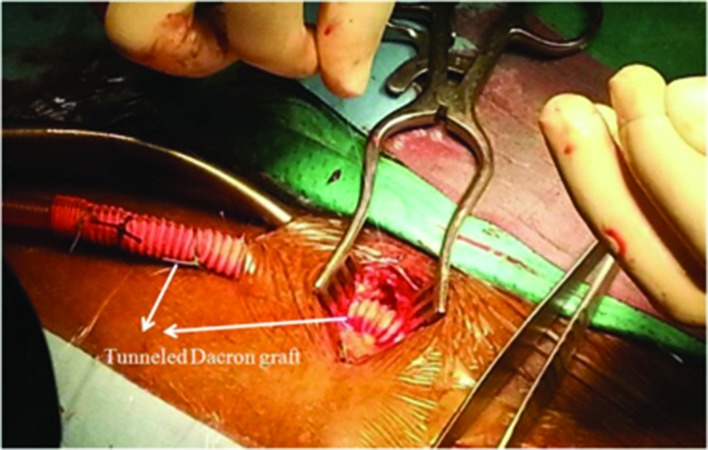
In the last 6 months we adopted a novel technique of femoral artery (FA) cannulation. The femoral vessels are harvested at the groin. The FA is clamped and incised longitudinally and a 8-mm Dacron graft (Vascutek, Scotland, UK) is anastomosed with a 6.0 prolene. At the end of the anastomotic procedure, an heparinized saline solution (25 mg of heparin in 500 cc. saline) is injected into the graft. The graft is subsequently clamped and the femoral artery is declamped in order to allow coagulation of the stitch holes. The graft is further tunneled inferiorly under the skin (Figure 1).
Figure 1.
Tunneled Dacron graft anastomosed on the femoral artery
An Elongated One-Piece arterial cannula 22 fr (EOPA, Medtronic, MN, USA) is introduced into the graft till its entrance into the leg, in order to avoid possible kinking of the dacron at skin incision.
This is of great importance when a centrifugal pump is used.
The femoral vein is cannulated with Seldinger technique using a 19-21 fr Bio-Medicus venous cannula (Medtronic, MN, USA) and tunneled as for the arterial cannula. The groin is then closed in layers (Figure 2).
Figure 2.
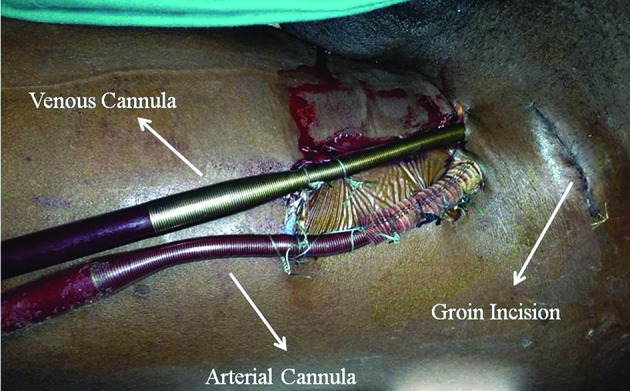
ECMO lines aspect. ECMO=Extracorporeal Membrane Oxygenation
In our Department the ECMO is achieved using a CentriMag (Levitronix, MA, USA) device and the oxygenator is a Quadrox (Maquet, NJ, USA) inserted in a Permanent Life Support circuit (Maquet).
Patient 1 was a 40 years old male, with a 1,75 m2 Body Surface Area, presenting with severe tricuspid regurgitation with a congenitally corrected transposition of great arteries and systemic ventricle dysfunction. Before starting the surgical procedure an intra aortic balloon pump was introduced in the right FA. He received a tricuspid valve replacement with a 33 mm biological valve. The patient was first successfully weaned from cardiopulmonary bypass. Six hours after the surgical procedure he experienced two episodes of ventricular fibrillation needing prompt cardioversion. We decided to use an ECMO support for six days using the left FA as described before.
Patient 2 was a 73 years old female, with 1,56 m2 Body Surface Area, presenting with heart failure due to aortic stenosis, aorto-right ventricular tunnel, sub-pulmonary ventricular septal defect and severe pulmonary regurgitation. She received tunnel and ventricular septal defect patch closure, aortic and pulmonary valve replacement with a 21 mm and 23 mm biological valve respectively.
The weaning from bypass was easily achieved but a septic shock occurred on the third day after surgery due to bacterial pneumonia. Since the hemodynamic parameters were deteriorating despite increasing levels of noradrenalin we decided to use ECMO support and femoral vessels were cannulated as described before.
None of the patients showed peripheral ischemia of the leg or even infection or bleeding from the site of cannulation. In both cases, the temperature gradient between the two feet was less than one degree, suggesting a symmetric perfusion.
Femoral vessels are commonly used as peripheral vessels for ECMO cannulation but the incidence of arterial vascular complications is still not negligible.
We recently adopted a new simple technique of cannulation of a side graft anastomosed to the FA similarly to what described previously for ECMO using the axillary artery [4].
This technique has the advantage of reducing the risk of lower leg ischemic injury, but it requires an open access that could induce bleeding and infection.
The distal venous drainage could possibly confer an additional advantage, but its role is still debated and we never use it in our experience. Furthermore a correct antegrade perfusion of the leg could minimize the advantage of the venous drainage.
To reduce bleeding, we anastomosed the graft without heparinization of the patient and with only a flushing of the graft with heparinized saline solution. This allows stitch holes closure and a significant reduction of bleeding. A cannula was inserted into the graft up to the level of the skin incision in order to prevent Dacron kinking or compression.
The insertion of both cannulae through a tunneled way allows the groin to be closed in layers and this possibly reduces risks for infection.
The two cases are not sufficient to assume that the technique would avoid leg ischemia but, as it allows to maintain antegrade perfusion, it should be effective. Furthermore it is reproducible and easy to perform and avoids the need to reconstruct the femoral arteries at the time of removal of the cannula.
Footnotes
Source of Support Nil.
Disclosures None declared.
Cite as: Quarti A, Iezzi F, Santoro G, Pozzi M. Femoral artery cannulation through a side graft in extracorporeal membrane oxygenation. Heart, Lung and Vessels. 2014; 6(2): 125-127.
References
- Bisdas T, Beutel G, Warnecke G, Hoeper MM, Kuehn C, Haverich A. et al. Vascular complications in patients undergoing femoral cannulation for extracorporeal membrane oxygenation support. Ann Thorac Surg. 2011;92:626–631. doi: 10.1016/j.athoracsur.2011.02.018. [DOI] [PubMed] [Google Scholar]
- Haley MJ, Fisher JC, Ruiz-Erizalde AR, Stolar CJ, Morrissehy NJ, Middlesworth W. Percutaneous distal perfusion of the lower extremity after femoral cannulation for veno-arterialextracorporeal membrane oxygenation in a small child. J Pediatr Surg. 2009;44:437–440. doi: 10.1016/j.jpedsurg.2008.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gander JW, Fisher JC, Reichstein AR, Gross ER, Aspelund G, Middlesworth W. et al. Limb ischemia after common femoral artery cannulation for venoarterial extracorporeal membrane oxygenation: an unresolved problem. J Pediatr Surg. 2010;45:2136–2140. doi: 10.1016/j.jpedsurg.2010.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navia JL, Atik FA, Beyer EA, Vega PR. Extracorporeal Membrane Oxygenation with right axillary artery perfusion. Ann Thorac Surg. 2005;79:2163–2165. doi: 10.1016/j.athoracsur.2004.01.031. [DOI] [PubMed] [Google Scholar]