Abstract
Objective
To determine the early risk factors for enlargement of the tracheoesophageal puncture (TEP) after total laryngectomy.
Design
Retrospective cohort study.
Setting
The University of Texas MD Anderson Cancer Center, Houston.
Patients
The study included 194 patients who underwent total laryngectomy (with or without pharyngectomy) and TEP (2003-2008).
Main Outcome Measures
Multiple logistic regression methods were used to evaluate early risk factors for an enlarged TEP.
Results
The incidence of an enlarged TEP was 18.6% (36 of 194 patients). After adjustment for follow-up time and radiotherapy history, patients with nodal metastases had a significantly higher risk of TEP enlargement (adjusted odds ratio, 6.6; 95% CI, 1.6-26.6) than those with node-negative disease. Total laryngopharyngectomy significantly increased the risk of an enlarged TEP (adjusted odds ratio, 4.5; 95% CI, 1.4-14.7) compared with simple total laryngectomy. Before multivariable adjustment, the preoperative body mass index was also significantly associated with enlargement (P for trend, .04)
Conclusions
These data suggest that 2 clinical factors—nodal staging and extent of resection—may help identify those at highest risk for TEP enlargement early after surgery. These simple indicators may ultimately aid in patient selection and prevention of an enlarged TEP after total laryngectomy.
Keywords: tracheoesophageal puncture, total laryngectomy, enlarged tracheoesophageal puncture, risk factors
INTRODUCTION
Tracheoesophageal puncture (TEP) is considered the criterion standard for alaryngeal voice rehabilitation after total laryngectomy because it is associated with superior voice quality and higher levels of patient satisfaction compared with other modes of voice restoration.1 The method relies on the placement of a valved silicone voice prosthesis within a surgically created fistula in the tracheoesophageal wall, which is commonly referred to as the TEP. One of the most challenging complications that may develop after TEP is enlargement of the TEP, which has been estimated to occur in 7% to 19% of patients.2-4 Enlargement of the TEP results in aspiration around the voice prosthesis and substantially increases the risk of pneumonia after total laryngectomy. Intractable aspiration resulting from an enlarged TEP has also been found to lead to chronic gastrostomy dependence in 14% of patients who develop the complication.5
The identification of patients who are at high risk for an enlarged TEP will enable clinicians to better select candidates for TEP, to individualize preoperative discussions of risk vs benefit, and, in some cases, to modify clinical practices in patients who have an increased risk of enlargement. A recent multivariable analysis found that 3 clinical factors were independently associated with the risk of TEP enlargement: advanced nodal classification, postlarygectomy stricture, and locoregional recurrence or distant metastasis after laryngectomy. Extended resections and postoperative radiotherapy are also predisposed to TEP enlargement.4 Many of the risk factors identified in this earlier analysis, including tumor recurrence and stricture, emerge well into the postoperative course. However, early identification of high-risk individuals is important to inform decisions about candidacy for the TEP procedure and prosthetic management. Therefore, the primary objective of this analysis was to identify early risk factors for an enlarged TEP.
METHODS
STUDY METHODS AND ELIGIBILITY
A retrospective cohort study was conducted to identify early risk factors for an enlarged TEP. All patients who underwent TEP for voice restoration after total laryngectomy at The University of Texas MD Anderson Cancer Center (MDACC), Houston, between May 2003 and December 2008, were eligible for inclusion in the study. Patients whose surgical resection and/or TEP was performed at an outside institution and those with less than 3 months of follow-up after TEP were excluded. A total of 194 of 237 potentially eligible subjects identified by a search of the MDACC TEP Tracking Database met inclusion criteria for the study. Institutional review board approval and a waiver of informed consent were obtained.
DATA COLLECTION
Data were extracted from the MDACC TEP Tracking Database, the MDACC Tumor Registry, and review of the electronic medical records. The primary dependent variable was a diagnosis of an enlarged TEP during the study period, defined by leakage around the voice prosthesis that was unresponsive to standard prosthetic management.4 Potential early risk factors included patient demographics, tobacco and alcohol history, medical comorbidities, disease characteristics, extent of surgery, and preoperative radiotherapy and chemotherapy. Patient demographics included sex, age at time of laryngectomy, self-reported race or ethnicity at time of registration, marital status at time of registration, and institutional pay code at time of registration as an indicator of socioeconomic status. Institutional pay codes were determined based on Federal Poverty Guidelines calculated by the pretax gross annual family income and the number of persons in the household. Self-reported tobacco and alcohol exposure were coded per institutional classifications in the patient history database.6,7 Smoking status at the time of laryngectomy was coded never (<100 lifetime cigarettes), former (quit at least 1 year before surgery), or current (smoking within 1 year of surgery). The pack-year history of smoking was calculated. Self-reported alcohol exposure was coded never (never or rarely drink), former (at least 1 drink per month but quit at least 1 year before surgery), or current (currently at least 1 drink per month). Preoperative medical comorbidities included a physician diagnosis of diabetes recorded at preoperative assessment, Adult Comorbidity Evaluation-27 comorbidity score,8 body mass index (BMI),9 thyroid-stimulating hormone level (reference range, 0.5-5.5 mIU/L), and serum albumin level (reference range, 3.5-4.7 g/dL [to convert to grams per liter, multiply by 10]). The MDACC Clinical Chemistry Normal Values Bulletin was used to define reference ranges.10
Disease variables collected included tumor stage (classified by TNM criteria), tumor site, and pathologic diagnosis. Tumor staging is evaluated before surgery with computed tomographic imaging and finalized on the basis of the surgical pathology report. The extent of surgery (ie, pharyngeal resection and/or reconstruction and/or neck dissection) is planned a priori and is known at the time of preoperative consultation in many cases. During surgery, the TEP is performed after the resection. Therefore, the extent of surgery and the method of closure are known before a primary TEP is performed. The extent of surgery was thus considered a potential covariate (ie, early risk factor) in this analysis. The extent of resection was classified based on the operative report as total laryngectomy, total laryngectomy plus partial pharyngectomy, or total laryngopharyngectomy (TLP). Neck dissection at the time of laryngectomy (yes/no) was also recorded.
STATISTICAL METHODS
Early risk factors for an enlarged TEP were analyzed using unconditional multiple logistic regression methods as described by Hosmer and Lemeshow.11 Unadjusted relative risk (RR) ratios and 95% confidence intervals were calculated, and univariable logistic regression models containing each covariate were fit before the multiple regression model was built. Covariates with P < .25 (likelihood ratio test χ2) in the univariable logistic models were selected as candidates for the multivariable model. Multiple logistic regression models were adjusted for length of follow-up and radiotherapy history. An a priori threshold (z score test, P < .10) was used to select variables for entry or removal during model building. Adjusted odds ratios (AORs) and 95% confidence intervals were calculated based on the final multivariable logistic regression model. Postestimation statistics were calculated. Nonparametric trend tests were conducted when trends were apparent between strata. Statistical significance was set at α = .05.
RESULTS
PATIENT CHARACTERISTICS
A total of 194 patients were included in this analysis. The mean (SD) age was 62 (11) years (range, 37-86 years), and 84.0% were male. Eighty-eight percent of the patients were smokers. More than half of the patients (n = 103 [53.1%]) underwent salvage laryngectomy after radiotherapy or chemoradiotherapy failure. Glottic (n = 87 [44.9%]) and supraglottic (n = 56 [28.9%]) primary tumors were most common. A detailed description of this cohort has been previously published.4 A summary of patient characteristics is provided in Table 1.
Table 1.
Univariable Associations between Patient Demographics, Preoperative Comorbidities, and Treatment Variables and Enlargement of the TEP (n=194)
|
Total Pts No. (%) |
Enlarged TEP No. (%) |
Unadjusted RR (95% CI) |
Trend
P |
|
|---|---|---|---|---|
| Sex | ||||
| Male | 162 (83.5) | 28 (17.3) | ||
| Female | 32 (16.5) | 8 (25.0) | 1.4 (0.7-2.9) | -- |
| Race/Ethnicity | ||||
| White | 151 (18.5) | 28 (18.5) | ||
| Hispanic | 21 (10.8) | 4 (19.1) | 1.0 (0.4-2.6) | |
| Black | 15 (7.7) | 3 (20.0) | 1.1 (0.4-3.1) | -- |
| Smoking | ||||
| Never | 24 (12.4) | 2 (8.3) | ||
| Former | 77 (40.0) | 15 (19.5) | 2.3 (0.6-9.5) | |
| Current | 93 (47.9) | 19 (20.4) | 2.5 (0.6-9.8) | 0.325 |
| Alcohol | ||||
| Never | 47 (24.2) | 8 (17.0) | ||
| Former | 54 (27.8) | 11 (20.4) | 1.2 (0.5-2.7) | |
| Current | 93 (47.9) | 17 (18.3) | 1.1 (0.5-2.3) | -- |
| Pre-TL BMI | ||||
| Healthy | 76 (39.2) | 16 (21.1) | ||
| Underweight | 12 (6.2) | 4 (33.3) | 1.6 (0.6-3.9) | |
| Overweight | 69 (35.6) | 11 (15.9) | 0.8 (0.4-1.5) | |
| Obese | 35 (18.0) | 3 (8.6) | 0.4 (0.1-1.3) | 0.040 |
| Pre-TL albumin | ||||
| Normal range | 136 (70.1) | 23 (16.9) | ||
| 2.1-2.7 g/dL | 11 (5.7) | 3 (27.3) | 1.6 (0.6-4.5) | |
| <2.1 g/dL | 8 (4.1) | 3 (37.5) | 2.2 (0.8-5.8) | 0.484 |
| TSH | ||||
| Normal range | 126 (65.0) | 26 (20.6) | ||
| Low | 11 (5.7) | 2 (18.2) | 0.7 (0.2-2.1) | |
| High | 21 (10.8) | 3 (14.3) | 0.9 (0.2-3.2) | -- |
| ACE-27 comorbidity | ||||
| None/mild | 129 (66.5) | 22 (17.1) | ||
| Moderate/severe | 65 (33.5) | 14 (21.5) | 1.3 (0.7-2.3) | |
| Tumor site | -- | |||
| Glottic/subglottic | 102 (52.6) | 14 (13.7) | ||
| Supraglottic | 56 (28.9) | 11 (19.6) | 1.4 (0.7-2.9) | |
| Hypopharynx | 21 (10.8) | 7 (33.3) | 2.4 (1.1-5.3) | |
| Other | 15 (7.7) | 4 (26.7) | 1.9 (0.7-5.1) | 0.037 |
| T classification | ||||
| T2 | 9 (4.6) | 2 (22.2) | ||
| T3 | 19 (9.8) | 3 (15.8) | 0.7 (0.1-3.5) | |
| T4 | 57 (29.4) | 13 (22.8) | 1.0 (0.3-3.8) | |
| Recurrent | 104 (53.6) | 18 (17.3) | 0.8 (0.2-2.8) | -- |
| N classification | ||||
| N0 | 41 (21.1) | 3 (7.3) | ||
| N1 | 12 (6.2) | 3 (25.0) | 3.4 (0.8-14.8) | |
| N2 or N3 | 34 (17.5) | 12 (37.5) | 4.8 (1.5-15.7) | |
| Recurrent | 104 (53.6) | 18 (17.3) | 2.4 (0.7-7.6) | 0.005 |
| Prior radiation | ||||
| No | 80 (41.2) | 17 (21.3) | ||
| Yes | 114 (58.8) | 19 (16.7) | 0.8 (0.4-1.4) | |
| Prior chemo | ||||
| No | 153 (78.9) | 32 (20.9) | ||
| Yes | 37 (19.1) | 4 (9.8) | 0.5 (0.2-1.2) | |
| Extent surgery | ||||
| TL | 147 (75.8) | 24 (16.3) | ||
| TL + PP | 26 (13.4) | 5 (19.2) | 1.2 (0.5-2.8) | |
| TLP | 21 (10.8) | 7 (33.3) | 2.0 (1.0-4.1) |
Non-significant associations with age, marital status, financial status, diabetes, type of radiotherapy, >1 course preoperative radiotherapy, and laryngeal dysfunction necessitating laryngectomy are not shown
TREATMENT CHARACTERISTICS
One hundred fourteen patients (59.0%) had received radiotherapy before total laryngectomy. Extended resections requiring free-flap reconstruction were performed in 47 of 134 patients (24.0%), including a partial pharyngectomy in 26 patients (13.4%) and TLP in 21 patients (10.8%). Neck dissections were performed at the time of laryngectomy in 121 patients (62.4%). The mean (SD) length of follow-up after laryngectomy was 24 (17) months (range, 3-72 months) after TEP.
EARLY RISK FACTORS FOR ENLARGED PUNCTURE
Univariable Associations
An enlarged TEP occurred in 36 patients (incidence, 18.6%) a median of 318 days after TEP (range, 1-1653 days). Unadjusted RR ratios are provided in Table 1. Nonsignificant elevated RR ratios were observed in current (RR, 2.5; 95% CI, 0.6-9.8) and former (RR, 2.3, 95% CI, 0.6-9.5) smokers compared with never smokers. However, mean pack-years of smoking were similar among those who did and did not develop an enlarged TEP (37.4 vs 45.0, respectively; P = .26). The risk of an enlarged TEP was also higher in individuals with preoperative nutritional deficiencies (eg, serum albumin depletion, underweight BMI). Before multivariable adjustment, preoperative BMI levels were significantly associated with rates of an enlarged TEP (P for trend, .04); an underweight BMI classification was associated with a higher risk of an enlarged TEP compared with a healthy BMI classification, whereas those with obese and overweight BMI classifications had a lower risk of an enlarged TEP. The risk of an enlarged TEP also increased progressively by preoperative levels of serum albumin depletion, but this trend was not statistically significant (P for trend, .48).
T classification was not significantly associated with the risk of an enlarged TEP, but patients with nodal metastases had a significantly higher risk of TEP enlargement. The risk of an enlarged TEP was lowest (14%) in patients with glottic or subglottic primary tumors, higher (20%) in patients with supraglottic cancers, and highest (33%) in patients with hypopharyngeal tumors (P for trend, .04). The risk of an enlarged TEP increased similarly with the extent of pharyngeal resection (P for trend, .12). Neck dissections were significantly more common in patients with nodal metastases (40 of 46 patients [87%]) than in those with node-negative cancers (28 of 41 patients [68%]; P = .04), but the rates of an enlarged TEP were similar in those who underwent neck dissection (24 of 121 patients [19.8%]) and those who did not undergo neck dissections (12 of 73 patients [16.4%]; RR, 1.2; 95% CI, 0.6-2.3).
Multiple Logistic Regression Model
After adjustment for length of follow-up and chemotherapy and radiotherapy history, 2 independent early risk factors were identified: nodal metastasis and TLP. Patients with nodal metastasis had a significantly higher risk of enlargement (AOR, 6.6; 95% CI, 1.6-26.6) than those with node-negative primary disease, and patients who underwent a TLP had a significantly increased risk of an enlarged TEP (AOR, 4.5; 95% CI, 1.4-14.7) compared with patients who underwent a total laryngectomy. The results of the multiple logistic regression analysis are summarized in Table 2.
Table 2.
Results of Multiple Logistic Regression Model on Preoperative Risk Factors for Enlarged TEP
| Adjusted* OR (95% CI) | |
|---|---|
| N classification | |
| NO | 1.0 (referent) |
| N+ | 6.6 (1.6-26.6) |
| Recurrent | 3.1 (0.7-14.3) |
| Surgery | |
| TL | 1.0 (referent) |
| TL + PP | 1.7 (0.5-5.4) |
| TLP | 4.5 (1.4-14.7) |
Abbreviations: PP, partial pharyngectomy, TLP, total laryngopharyngectomy
Adjusted for length follow-up, chemotherapy & radiation history
Risk of Enlarged TEP by Interactions of Nodal Classification and Extent of Surgery
Interactions among nodal staging and extent of surgery were further examined. A low-risk group and a high-risk group emerged. The low-risk subgroup of patients with node-negative primary disease who underwent a total laryngectomy without a pharyngectomy had a 7% incidence of TEP enlargement. In contrast, 4 of 5 patients (80%) in the high-risk subgroup who had node-positive primary cancer and who underwent TLP developed an enlarged TEP. The incidence of an enlarged TEP ranged from 15% to 27% in all other subgroups of patients. Interactions among nodal staging and extent of resection are provided in Table 3. Risk-stratified Kaplan-Meier curves are presented in the Figure.
Table 3.
Interactions between pre-operative risk factors: Incidence of enlarged TEP by extent of surgery and nodal staging
| Incidence of enlarged TEP No. (%) of patients |
|||
|---|---|---|---|
| TL | TL + PP | TLP | |
| N0 primary disease | 2/31(6.5%) | 1/6 (16.7%) | - |
| N+ primary disease | 10/36 (27.8%) | 1/5 (20.0%) | 4/5 (80.0% ) |
| Recurrent disease | 12/78 (15.4% ) | 3/14 (21.4%) | 3/12 (25.0%) |
Abbreviations: PP, partial pharyngectomy, TLP, total laryngopharyngectomy
Figure 1.
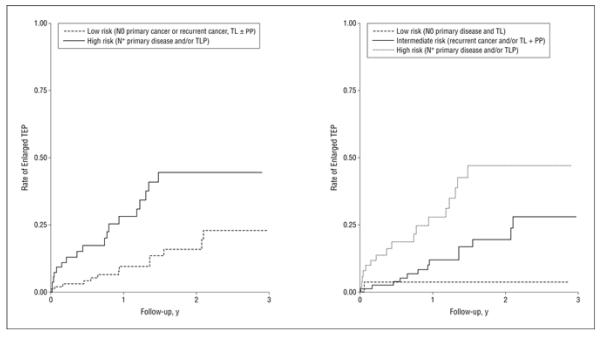
Risk-stratified Kaplan-Meier failure estimates for risk of an enlarged tracheoesophageal puncture (TEP) during 3 years of follow-up. PP indicates partial pharyngectomy; TL, total laryngectomy; and TLP, total laryngopharyngectomy.
COMMENT
Enlargement of the TEP remains a challenging complication of surgical prosthetic voice restoration. Published data suggest that the overall risk of developing TEP enlargement is between 7% and 19% among all patients who undergo TEP after laryngectomy, but the risk of complication is elevated in certain subgroups. Early identification of high-risk patients is necessary for clinicians to personalize the risk-benefit analysis regarding candidacy and timing (primary vs secondary) of the TEP procedure, to offer realistic expectations about potential complications, and to guide subsequent selection of appropriate voice prostheses. However, many of the risk factors identified in our previously published analysis occurred after surgery (eg, postoperative recurrence, postoperative stricture, postoperative radiotherapy). Herein, we restricted our risk factor analysis to clinical factors that were known early in the clinical course, before and immediately after surgery. The results of this analysis indicate that patients who undergo TLP (AOR, 4.5; 95% CI, 1.4-14.7) and those with N+ primary disease (AOR, 6.6; 95% CI, 1.6-26.6) have the highest risk of developing an enlarged TEP. It is possible that these factors are surrogates for previously identified postoperative factors that may more directly affect the risk of enlargement. However, nodal status and extent of surgery may alert clinicians to high-risk patients long before other risk factors (eg, stricture, recurrence) appear, in time to modify clinical decisions.
Total laryngopharyngectomy is associated with greater morbidity than laryngectomy alone. Previous authors have reported higher rates of TEP complications and stricture after TLP, and one-third of patients who had a TEP after TLP in the present study developed TEP enlargement.12,13 Total laryngopharyngectomy is most commonly required for patients with hypopharyngeal primary tumors who have the highest risk of cancer recurrence after surgery, and we have previously reported that postoperative recurrence is the strongest independent predictor of TEP enlargement.4 Also, circumferential neopharyngeal reconstruction (required after TLP) may be associated with vascular changes in the adjacent cervical esophageal tissues, where the TEP is located. These factors, in part, may have contributed to the 4.5-fold increased risk of TEP enlargement that was observed after TLP despite our practice of delaying TEP as a secondary procedure in 91% of TLP cases. However, many authors have established the feasibility of tracheoesophageal voice restoration after TLP.14,15 Tracheoesophageal voice offers the most satisfactory outcomes for properly selected patients after TLP and may enhance quality of life after an extreme surgical procedure. Therefore, TLP alone should not be considered a contraindication for tracheoesophageal voice restoration. Rather, a 33% risk of an enlarged TEP should be considered in the context of other psychosocial and clinical factors when evaluating candidacy for TEP in patients who are likely to require a TLP. At our institution, secondary TEP is typically preferred for individuals who require pharyngectomy and free-flap reconstruction. Delaying TEP in patients who require pharyngeal reconstruction allows clinicians to account for final pathologic staging, postsurgical healing, and the final extent of surgery in decisions and discussions about TEP candidacy.
Nodal metastasis significantly predicted the risk of TEP enlargement. Consistent with previously published results,4 patients with N+ primary disease were 6.6-fold more likely to develop an enlarged TEP than patients with N0 primary disease. However, neck dissections, which are more commonly performed in patients with node-positive disease, did not significantly increase the risk of an enlarged TEP. Other factors that might predispose to enlargement in those with N+ disease include a greater chance of postoperative disease recurrence and an increased likelihood of postoperative radiotherapy. Postoperative radiotherapy fields at our institution deliver higher radiotherapy doses locally to the TEP site than most definitive radiotherapy fields, and we have previously reported significantly elevated rates of an enlarged TEP in patients who require postoperative radiotherapy. While the mechanism of association is not entirely clear, these data suggest that nodal classification provides a simple early indicator of risk for TEP enlargement. Stratified 3 ways, the incidence of an enlarged TEP by nodal classification is lowest (7.3%) in patients with node-negative (N0) primary cancer, intermediate (17.3%) in patients who require salvage surgery for recurrent cancer, and highest (33%) in patients with node-positive (N+) primary cancer requiring laryngectomy.
Total laryngopharyngectomy and N+ primary disease were identified as independent early risk factors, and both were associated with a 33% risk of TEP enlargement. However, interactions between these 2 clinical factors best differentiated those with an extremely high or low risk of complication. Although composing a rare subgroup, accounting for only 5 of 194 patients in this cohort, most patients (80%) with N+ primary disease who required TLP developed an enlarged TEP. This select subgroup of patients, who primarily present with advanced N+ hypopharyngeal primary tumors, should be counseled to ensure realistic expectations given the high likelihood of TEP enlargement. A history of TLP for N+ primary disease does not preclude tracheoesophageal voice restoration in an otherwise excellent candidate, but the patient is likely to require additional procedures, more frequent clinic visits, and specialized prosthetic management to prevent pneumonia and leakage around the prosthesis. In contrast, only 7% of patients who presented with N0 primary disease and who required a total laryngectomy alone developed TEP enlargement. This “low-risk” group might be considered optimal candidates for TEP because they are less likely to require complex rehabilitation for the management of leakage complications. All other subgroups of patients for whom the rate of enlargement ranged from 15% to 28% may be considered an “intermediate-risk” group. The identification of extremely high- and low-risk groups may be used to individualize the risk-benefit evaluation for TEP and guide clinicians when selecting optimal voice prostheses for individual patients.
The findings of this study can be used to assist clinical decisions about TEP candidacy and prosthetic management early in the clinical trajectory. However, it is important to acknowledge that neither nodal staging nor extent of surgery is truly confirmed before surgery. Preoperative nodal staging based on imaging can change with final pathologic data. Previous authors have reported 87% to 91% concordance between nodal staging on computed tomographic and histologic findings.16,17 Therefore, nodal status is finalized based on surgical pathologic results well before critical decisions regarding candidacy for a secondary TEP are made and is established before surgery for many patients during the evaluation of candidacy for a primary TEP. Likewise, the planned extent of pharyngeal resection may change based on intraoperative findings. That is, it is sometimes the case that part of the pharynx might be spared when a TLP was planned before surgery, or, conversely, a pharyngectomy might be required when initially planned otherwise. Nonetheless, these simple clinical variables are confirmed early in the clinical course, as the extent of resection is known intraoperatively before a TEP is performed and nodal status is finalized by the surgical pathology report shortly after surgery. These early risk factors are particularly useful in helping clinicians personalize decisions about prosthetic management and candidacy for secondary TEP.
In conclusion, prevention of an enlarged TEP requires the identification of high-risk patients early in the clinical course. These data suggest that 2 simple clinical factors—nodal metastasis and planned extent of resection—may help identify patients who are at the highest risk of TEP enlargement. This information may ultimately aid in patient selection and risk reduction of this complication. However, these factors alone should not dictate decisions about candidacy for TEP but should be considered in the context of the overall clinical presentation. Attention to these risk factors (nodal metastasis and TLP) may alert clinicians to the patients who are at high risk for an enlarged TEP in time to modify clinical decisions regarding prosthetic management and timing of the TEP procedure.
Footnotes
Presented at the Combined Otolaryngological Spring Meetings, American Head & Neck Society, Chicago, IL, 4/28/2011
REFERENCES
- 1.Xi S. Effectiveness of voice rehabilitation on vocalisation in postlaryngectomy patients: a systematic review. Int J Evid Based Healthc. 2010;8(4):256–258. doi: 10.1111/j.1744-1609.2010.00177.x. [DOI] [PubMed] [Google Scholar]
- 2.Hutcheson KA, Lewin JS, Sturgis EM, Kapadia A, Risser J. Enlarged tracheoesophageal puncture after total laryngectomy: a systematic review and meta-analysis. Head Neck. 2011;33(1):20–30. doi: 10.1002/hed.21399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Op de Coul BM, Hilgers FJ, Balm AJ, Tan IB, van den Hoogen FJ, van Tinteren H. A decade of postlaryngectomy vocal rehabilitation in 318 patients: a single Institution’s experience with consistent application of provox indwelling voice prostheses. Arch Otolaryngol Head Neck Surg. 2000;126(11):1320–1328. doi: 10.1001/archotol.126.11.1320. [DOI] [PubMed] [Google Scholar]
- 4.Hutcheson KA, Lewin JS, Sturgis EM, Risser J. Multivariable analysis of risk factors for enlargement of the tracheoesophageal puncture after total laryngectomy. Head Neck. 2012;34(4):557–567. doi: 10.1002/hed.21777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hutcheson KA, Lewin JS, Sturgis EM, Risser J. Outcomes and adverse events of enlarged tracheoesophageal puncture after total laryngectomy. Laryngoscope. 2011;121(7):1455–1461. doi: 10.1002/lary.21807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dube SR, Asman K, Malarcher A, Carabollo R. Cigarette smoking among adults and trends in smoking cessation—United States, 2008. MMWR CDC Surveill Summ. 2009;58(44):1227–1232. [PubMed] [Google Scholar]
- 7.Dawson DA. [Accessed April 10, 2012];Methodological issues in measuring alcohol use. National Institute on Alcohol Abuse and Alcoholism (NIAAA) website. http://pubs.niaaa.nih.gov/publications/arh27-1/18-29.htm. [PMC free article] [PubMed]
- 8.Piccirillo JF. Importance of comorbidity in head and neck cancer. Laryngoscope. 2000;110(4):593–602. doi: 10.1097/00005537-200004000-00011. [DOI] [PubMed] [Google Scholar]
- 9. [Accessed March 15, 2010];Defining overweight and obesity. Centers for Disease Control and Prevention Web site. http://www.cdc.gov/obesity/adult/defining.html.
- 10.Pathology & Laboratory Medicine Bulletin of Information: Section of Clinical Chemistry: Clinical Chemistry Normal Values (Adult) The University of Texas MD Anderson Cancer Center; Houston: 2008. [Google Scholar]
- 11.Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed John Wiley & Sons Inc; Hoboken, NJ: 2000. [Google Scholar]
- 12.Bozec A, Poissonnet G, Chamorey E, et al. Results of vocal rehabilitation using tracheoesophageal voice prosthesis after total laryngectomy and their predictive factors. Eur Arch Otorhinolaryngol. 2010;267(5):751–758. doi: 10.1007/s00405-009-1138-x. [DOI] [PubMed] [Google Scholar]
- 13.Yu P, Hanasono MM, Skoracki RJ, et al. Pharyngoesophageal reconstruction with the anterolateral thigh flap after total laryngopharyngectomy. Cancer. 2010;116(7):1718–1724. doi: 10.1002/cncr.24947. [DOI] [PubMed] [Google Scholar]
- 14.Sinclair CF, Rosenthal EL, McColloch NL, et al. Primary versus delayed tracheoesophageal puncture for laryngopharyngectomy with free flap reconstruction. Laryngoscope. 2011;121(7):1436–1440. doi: 10.1002/lary.21836. [DOI] [PubMed] [Google Scholar]
- 15.Lewin JS, Barringer DA, May AH, et al. Functional outcomes after laryngopharyngectomy with anterolateral thigh flap reconstruction. Head Neck. 2006;28(2):142–149. doi: 10.1002/hed.20308. [DOI] [PubMed] [Google Scholar]
- 16.Shingaki S, Suzuki I, Nakajima T, Hayashi T, Nakayama H, Nakamura M. Computed tomographic evaluation of lymph node metastasis in head and neck carcinomas. J Craniomaxillofac Surg. 1995;23(4):233–237. doi: 10.1016/s1010-5182(05)80213-6. [DOI] [PubMed] [Google Scholar]
- 17.Haberal I, Celik H, Göçmen H, Akmansu H, Yörük M, Ozeri C. Which is important in the evaluation of metastatic lymph nodes in head and neck cancer: palpation, ultrasonography, or computed tomography? Otolaryngol Head Neck Surg. 2004;130(2):197–201. doi: 10.1016/j.otohns.2003.08.025. [DOI] [PubMed] [Google Scholar]


