Abstract
There has been increased interest in and experimentation with demand-side mechanisms such as the use of vouchers that place purchasing power in the hands of targeted consumers to improve the uptake of healthcare services in low-income settings. A key measure of the success of such interventions is the extent to which the programmes have succeeded in reaching the target populations. This article estimates the coverage of facility deliveries by a maternal health voucher programme in South-western Uganda and examines whether such coverage is correlated with district-level characteristics such as poverty density and the number of contracted facilities. Analysis entails estimating the voucher coverage of health facility deliveries among the general population and poor population (PP) using programme data for 2010, which was the most complete calendar year of implementation of the Uganda safe motherhood (SM) voucher programme. The results show that: (1) the programme paid for 38% of estimated deliveries among the PP in the targeted districts, (2) there was a significant negative correlation between the poverty density in a district and proportions of births to poor women that were covered by the programme and (3) improving coverage of health facility deliveries for poor women is dependent upon increasing the sales and redemption rates. The findings suggest that to the extent that the programme stimulated demand for SM services by new users, it has the potential of increasing facility-based births among poor women in the region. In addition, the significant negative correlation between the poverty density and the proportions of facility-based births to poor women that are covered by the voucher programme suggests that there is need to increase both voucher sales and the rate of redemption to improve coverage in districts with high levels of poverty.
Keywords: Maternal health vouchers, programme coverage, health facility delivery, Uganda
KEY MESSAGES.
To the extent that the safe motherhood voucher programme in South-western Uganda stimulates demand for maternal healthcare services by new users, it has the potential of increasing facility-based births among poor women.
There was a significant negative correlation between the poverty density in a district and proportions of births to poor women that were covered by the programme suggesting that there is need to increase both voucher sales and the rate of redemption to improve coverage in districts with high levels of poverty.
Increasing the rate of redemption can be enhanced through community sensitization on the importance of seeking care.
Background
Although motherhood is often a positive and fulfilling experience, for many women in low-income settings it is associated with suffering, ill-health and even death [World Health Organization (WHO) 2012]. Key indicators in meeting Millennium Development Goal (MDG) 5 include reducing the maternal mortality ratio by three quarters between 1990 and 2015 and increasing the proportion of births attended by skilled health personnel [United Nations (UN) 2000]. However, with less than 2 years left to 2015, progress towards meeting the target has been slow and uneven across countries, with most African countries not likely to meet goals (Bhutta et al. 2010; Hogan et al. 2010; UN 2010). The slow progress especially in sub-Saharan Africa underscores the need for mechanisms that can accelerate scale-up and uptake of effective skilled delivery services.
A key factor influencing the uptake of appropriate health services is access. This is defined along three dimensions: availability, acceptability and affordability of services (Thiede et al. 2007). Availability refers to whether the appropriate health services exist where and when they are needed, while acceptability pertains to the nature of service provision and how this is perceived by individuals and communities (Thiede et al. 2007). The affordability dimension of access, on the other hand, refers to the balance between the cost of utilizing health services and the individual’s ability to pay as well as the perceived protection from the economic consequences of health costs (Thiede et al. 2007). These dimensions of access affect the poor more than the rich (Campbell and Graham 2006; Ronsmans and Graham 2006; Hill et al. 2007; Peters et al. 2007; Mahmood 2010). For example, the lifetime risk of dying during or following pregnancy in sub-Saharan Africa is 1 in 39 compared with 1 in 3800 in the developed world (WHO 2012). Even within countries, there are major variations in the risk of maternal death between wealth quintiles; the majority of maternal deaths in sub-Saharan Africa region occur in the absence of skilled routine and emergency care (Kinney et al. 2010).
Government intervention in the health sector has typically been through supply-side subsidies that cover some or all of the costs of health services inputs (infrastructure, staff, drugs, equipment, non-medical consumables), but provide little incentive to attract clients or increase productivity (World Bank 2004). The weaknesses of such interventions in increasing uptake of health facility services have led to increased interest in and experimentation with demand-side mechanisms that place purchasing power in the hands of targeted consumers to spend on specific services at accredited facilities, thereby increasing access and encouraging quality improvement. Examples of demand-side financing mechanisms that are being explored include output-based aid (OBA) vouchers and social health insurance programmes (Gorter et al. 2003; Janssen et al. 2004; Borghi et al. 2006; Bhatia and Gorter 2007; Lagomarsino et al. 2012; Moreno-Serra and Smith 2012).
Vouchers, for example, link demand-side consumer subsidies with payments to providers for supplying a set of contracted services to the intended beneficiaries. A voucher management agency (VMA) co-ordinates the programme functions, from selection of accreditation bodies, production and distribution of vouchers to the management of cash flows. Using a targeting methodology, low-income clients can buy the vouchers at a steep discount or receive them free if living in extreme poverty. Clients exchange the voucher for a set of pre-determined health services at accredited health facilities. Facilities are accredited to ensure that they meet a given minimum standard of quality for participation in the voucher programme. Following service provision, facilities can claim for reimbursement at a pre-agreed rate. Vouchers offer clients their choice of skilled health care from accredited health facilities while contracted facilities benefit from the additional client volume and reimbursements.
Findings from existing voucher programmes show increased utilization of reproductive health services among target population groups as a result of such interventions (Ir et al. 2010; Agha 2011; Bellows et al. 2011; Bellows et al. 2013; Obare et al. 2013). However, a key measure of an intervention’s success that is missing from much of the voucher evaluation literature is the extent to which the programmes have succeeded in reaching the target populations. The question can be examined in the context of programme coverage, which is a critical measure for the assessment of the performance of health systems in achieving objectives such as improving population health and reducing health inequalities. This article estimates the demographic coverage of the maternal health voucher programme in South-western Uganda and examines whether such coverage is correlated with district-level characteristics such as poverty density and the number of contracted facilities. The article focuses on crude coverage of the programme without analysing the effectiveness of such coverage. Coverage in this context is defined as the proportion of estimated deliveries financed by the voucher programme among all estimated deliveries in each district. We further estimate the expected voucher sales and redemption rates that would be required to realize coverage of ∼50% of all deliveries to poor women in the target districts based on the 2010 figures.
Context
Uganda has a high maternal mortality ratio estimated at 438 deaths per 100 000 live births with complications of pregnancy and childbirth being among the leading causes of morbidity and mortality among Ugandan women of reproductive age [Uganda Bureau of Statistics (UBOS) and ICF International Inc. 2012]. Although 95% of mothers in the country received antenatal care from a skilled provider for their most recent birth, only 57% of the births occurred in a health facility (UBOS and ICF International Inc. 2012). There are also wide socio-economic disparities in the use of health services with the most vulnerable households facing major barriers in accessing, and much lower use of facility-based maternal health services. For instance, women in the poorest wealth quintile are 2.8 times less likely to deliver in a health facility compared with those in the richest quintile (UBOS and ICF International Inc. 2012).
Both institutional- and individual-level factors contribute to the low proportion of facility-based deliveries. At the institutional level, adequate quantities of affordable, good quality essential medicines and health supplies are not always available. Approximately 72% of government health units have monthly stockouts of any indicator medicine and supplies and are often poorly staffed [Ministry of Health (MoH) 2010a]. Inadequate financial and human resources, lack of capital investment and poor management have affected the ability of the public sector to fulfill its mandate of providing quality healthcare services to all those in need resulting in greater reliance on the private sector (MoH 2010a). Perceived low quality of care in facilities, distance to health facilities, transportation challenges, costs of services including informal charges or expenses, opportunity costs from time lost while seeking care, provider attitudes, power dynamics including ineffective decision making at the household level and socio-cultural norms are among client-level factors that affect the uptake of services in the country and similar settings (Thaddeus and Maine 1994; Ammoti-Kaguna and Nuwaha 2000; Afsana and Rashid 2001; Musoke 2002; Kyomuhendo 2003; Amone et al. 2005; UBOS and Macro International Inc. 2007; Essendi et al. 2010; Ir et al. 2010; Gabrysch et al. 2011; Njuki et al. 2012).
In terms of healthcare expenditure in Uganda, households in aggregate contributed 49% of the national health expenditure out-of-pocket; the central government contributed 15%, while development partners and international non-governmental organizations combined contributed 36% in the 2009/10 financial year (MoH 2013). Government spending on reproductive health as a percentage of the total government expenditure on health in the year 2009/10 was 4.6%, which amounted to 4% of the total expenditure on reproductive health services with the remaining 96% being from other sources (MoH 2013). In particular, households contributed 72% of the total amount spent on reproductive health services; other private entities contributed 3.4%, while donors and other development partners contributed 20.6% during the same accounting period (MoH 2013). Thus, households in Uganda continue to bear the greatest cost of maternal and reproductive health services despite the fact that lower level public health units and general wings of publicly owned hospitals do not normally charge user fees.
Unlike the public sector, the private sector charges user fees with the costs of medicines being 3–5 times more expensive than in the public sector and therefore not affordable for many people (MoH 2010a). It was, for instance, estimated that as of 2000, the direct costs to clients (including travel and waiting time, transport fees, drugs and supplies and any official or unofficial user fees) of accessing normal delivery services in Uganda were United States Dollar (USD) 2.26 in public and USD 22.75 in private facilities (Levin et al. 2000). Similarly, the direct costs of accessing surgical deliveries were USD 13.22 in public and USD 59.24 in private facilities (Levin et al. 2000). Not less than 9% of household expenditure is on health, while 4.8% of households in Uganda have health expenditures that are deemed ‘catastrophic’ with 2.3% being pushed into impoverishment because of medical bills (Xu et al. 2007).
It is in such context that the reproductive health vouchers programme was implemented in the country. The programme began in 2006 as a pilot in four districts in Western Uganda with funding from the German Development Bank (KfW) and subsidizing treatment for sexually transmitted infections. It was expanded in late 2008 to cover safe motherhood (SM) services in 20 districts with additional funding from KfW and the Global Partnership on Output-based Aid (GPOBA-World Bank). Distribution, behaviour change communication and marketing activities were conducted to create demand for services and promote full utilization of the voucher benefit packages. Approximately 151 community-based voucher distributors (70% of whom were village health team members) were trained to promote and distribute the SM voucher, known as ‘HealthyBaby’, to poor rural women using a district customized poverty grading tool.
The poverty grading tool scored women against socio-demographic characteristics such as geographical location, marital status, parity, place of last delivery for those who had delivered before, access to services such as health care, water, land and livestock ownership, housing structure, sources of income, average number of meals a day and ownership of household assets. The scores ranged from 0 to 21 points with an individual being ranked as poor if she scored between 0 and 9 points, middle income if she scored between 10 and 15 points and rich if she scored between 16 and 21 points. Women scoring between 0 and 12 points were eligible to purchase the voucher. The poverty grading tool was administered by distributors recruited from communities where the programme intended to target services. Community-based targeting was the preferred method to minimize inclusion biases (Ridde et al. 2010). All qualifying mothers bought the voucher at a cost of Uganda Shillings 3000 (equivalent USD 1.50) or qualified for a free voucher if determined to be destitute.
The voucher subsidized four antenatal care visits, delivery and post-natal care services up to 6 weeks post-delivery for economically disadvantaged women. Ninety-four private-for-profit and not-for-profit facilities offering basic or comprehensive emergency obstetric care were accredited and contracted to provide services to SM voucher clients. Providers from each accredited facility were trained on the operations of the programme at the time of inception. Standard operating procedures (SOPs) including treatment guidelines and protocols for safe delivery were distributed to each accredited facility. SOPs followed Ministry of Health defined national standards and protocols for safe deliveries. Clients redeemed the vouchers for a pre-defined package of services at an accredited facility with no further payments expected. Following service provision, health facilities lodged claims for payment with the VMA. After reviewing claims for minimum standards of care, services were reimbursed on a pre-agreed rate.
Methods
To estimate coverage, the VMA claims data for 2010 were analysed to obtain the number of voucher deliveries in each of the programme districts. The year 2010 was selected because it was the first complete calendar year of implementation of the SM voucher programme in the country. Coverage was estimated among the general population (GP) and poor population (PP) in each district using Equations (1) and (2):
| (1) |
| (2) |
where VDvp is the proportion of SM voucher facility deliveries (SMvp) in GP. VDPvp is the proportion of SM voucher facility deliveries (SMvp) in PP.
GP size was estimated based on 2010 projections by the UBOS under the assumption that the population growth rates remained constant over the period.
Poverty density indices obtained from the UBOS were used to estimate the number of PP in the voucher districts for 2010. Poverty estimates focused on the cost of meeting caloric needs with some allowance for non-food items (UBOS 2010). Specifically, the percentage of individuals estimated to be living in households with real private consumption per adult equivalent below the poverty line for the region (divided into rural and urban) was used.
The national crude birth rate from the 2011 Uganda Demographic and Health Survey was used to estimate the expected number of deliveries in 2010. The crude birth rate was assumed to have remained constant throughout the projection period and that it was the same for both poor and non-PPs.
Voucher coverage in both the GP and PP was calculated for the year 2010. The expected levels of voucher redemption rate necessary to achieve ∼50% coverage among the PP were then estimated.
Results
SM voucher sales and utilization
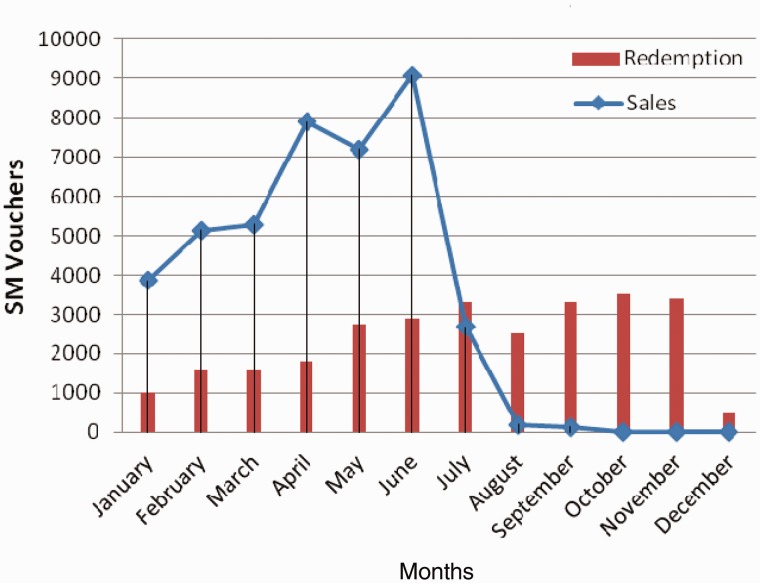
A total of 41 487 SM vouchers were sold in the 20 districts in 2010. Bushenyi district which had the highest number of accredited facilities (12), recorded the highest voucher sales of 7416 with Lyantonde recording the lowest sales of 246 vouchers. Out of the total SM vouchers that were sold in 2010, 68% (28 182) were redeemed for normal and caesarean delivery services during that year. Monthly trends in voucher redemption mirrored voucher sales from January through June. Voucher redemption dropped slightly in August but peaked in September and October before dipping at the end of the year. Voucher sales, on the other hand, dipped in July and the downward trend continued into September when the sales target was achieved for the year. No sales were made in the months of October, November and December (Figure 1).
Figure 1.
Monthly trends in voucher sales and redemption for health facility deliveries 2010.
More than half the vouchers sold in two-thirds of the districts were redeemed for delivery services in 2010 (Table 1). The number of vouchers redeemed in six of the districts exceeded the total number of vouchers sold over the same period implying that some voucher clients chose to deliver in districts other than those where they bought the vouchers. Only one district, Hoima, had a redemption rate of <20%.
Table 1.
Voucher uptake and coverage in GP and PP in year 2010
| Districts | Number of accredited facilities | GP (2010) | Expected deliveries GP (CBR = 0.042) | Poverty rate (% households in poverty) | PP (2010) | Expected deliveries PP (CBR = 0.042) | Voucher sales | Number of voucher deliveries | Redemption rate (%) | Voucher coverage GP (Equation 1) (%) | Voucher coverage PP (Equation 2) (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bundibugyo | 1 | 312 500 | 13 125 | 25.3 | 79 063 | 6370 | 1958 | 551 | 28 | 4 | 17 |
| Bushenyi | 12 | 858 600 | 36 061 | 18.4 | 157 982 | 11 900 | 7416 | 4880 | 66 | 14 | 74 |
| Hoima | 3 | 499 100 | 20 962 | 25.3 | 126 272 | 7142 | 1530 | 243 | 16 | 1 | 5 |
| Ibanda | 4 | 242 800 | 10 198 | 18.4 | 44 675 | 3387 | 906 | 892 | 98 | 9 | 48 |
| Isingiro | 5 | 396 700 | 16 661 | 18.4 | 72 993 | 4284 | 929 | 1112 | 120a | 7 | 36 |
| Kabale | 5 | 490 000 | 20 580 | 18.4 | 90 160 | 6747 | 1004 | 541 | 54 | 3 | 14 |
| Kabarole | 5 | 403 200 | 16 934 | 25.3 | 102 010 | 4627 | 689 | 1088 | 158a | 6 | 25 |
| Kamwenge | 3 | 317 000 | 13 314 | 25.3 | 80 201 | 5478 | 298 | 292 | 98 | 2 | 9 |
| Kanungu | 5 | 241 800 | 10 156 | 18.4 | 44 491 | 3765 | 3067 | 2027 | 66 | 20 | 108a |
| Kasese | 7 | 695 500 | 29 211 | 25.3 | 175 962 | 13 990 | 5897 | 5791 | 98 | 20 | 78 |
| Kibaale | 3 | 613 300 | 25 759 | 25.3 | 155 165 | 9494 | 964 | 1677 | 174a | 7 | 26 |
| Kiruhura | 7 | 280 200 | 11 768 | 18.4 | 51 557 | 3026 | 3791 | 1265 | 33 | 11 | 58 |
| Kyenjojo | 3 | 504 700 | 21 197 | 25.3 | 127 689 | 8153 | 355 | 419 | 118a | 2 | 8 |
| Lyantonde | 3 | 77 100 | 3238 | 11.2 | 8635 | 520 | 246 | 189 | 77 | 6 | 52 |
| Masindi | 4 | 602 100 | 25 288 | 25.3 | 152 331 | 10 648 | 1460 | 853 | 58 | 3 | 13 |
| Mbarara | 8 | 427 200 | 17 942 | 18.4 | 78 605 | 4748 | 6001 | 2247 | 37 | 13 | 68 |
| Ntungamo | 1 | 458 000 | 19 236 | 18.4 | 84 272 | 6101 | 1015 | 1067 | 105a | 6 | 30 |
| Rakai | 6 | 466 900 | 19 610 | 11.2 | 52 293 | 6135 | 1381 | 695 | 50 | 4 | 32 |
| Rukungiri | 4 | 311 600 | 13 087 | 18.4 | 57 334 | 3702 | 411 | 654 | 159a | 5 | 27 |
| Sembabule | 5 | 210 900 | 8858 | 11.2 | 23 621 | 2743 | 2169 | 1699 | 78 | 19 | 171a |
| Total | 94 | 8 409 200 | 353 186 | 1 765 311 | 122 961 | 41 487 | 28 182 | 68 | 8 | 38 |
aMore than 100% redemption and coverage rates may be due to infiltration of clients from other districts. CBR, Crude Birth Rate.
SM voucher coverage
Overall, the SM voucher covered 8% of the total estimated deliveries in the GP and 38% of the estimated deliveries among the PP in the programme districts (Table 1). There were major variations by district in the estimated proportions of deliveries among poor women that were covered by the voucher programme ranging from 5% in Hoima to more than 50% in eight of the districts (Table 1). Like redemption, voucher coverage exceeded expected deliveries in the PP in two of the districts.
Further analysis showed that there was a significant negative correlation between the poverty density in the district and the proportions of deliveries to poor women that were covered by the voucher programme (Pearson correlation coefficient, r = −0.54; P < 0.05). There was, however, no significant correlation between the number of accredited facilities in the district and the proportions of deliveries to poor women that were covered by the voucher programme (Pearson correlation coefficient, r = 0.42; P = 0.06). In addition, at the current redemption rate of 68%, a 25% increase in voucher sales would increase voucher coverage among the poor by 15 percentage points to 53%. Similarly, a 25% increase in voucher redemption rates would increase the SM voucher coverage among the poor by 10 percentage points to 48%.
Discussion
This article explored the potential of using targeted vouchers to accelerate the attainment of MDG 5 by estimating the proportions of births to poor women that are covered by the SM voucher programme in South-western Uganda. A key finding is that in 2010, the programme paid for 38% of deliveries among the PP with wide variations between districts. Moreover, in some districts, the voucher coverage exceeded voucher sales—a pattern that was most likely due to infiltration of voucher clients from other districts. At the national level, only 42% of births to women in the lowest income quintile occur in a health facility (UBOS and Macro International Inc. 2012). At one extreme, it is theoretically possible that vouchers were purchased only by women who already intended to deliver in a health facility, and thus that the programme had no impact on the proportion of women delivering in a health facility. At the other extreme, if the voucher programme successfully targeted only ‘new poor users’, that is, those who in the absence of the voucher would not have delivered in a health facility, and that the proportion of births to poor women that take place in a health facility in the programme districts is not very different from the national average, then the voucher programme almost doubled the number of facility-based deliveries among the poor (from 42% to 80%) in the targeted districts. Neither of these extremes is likely. While we do not have the data to quantify the exact impact on facility deliveries, the voucher offered substantial benefits to purchasers, and thus we hypothesize that some women who would have otherwise delivered at home due to cost were able to deliver at a facility by purchasing a voucher.
The second major finding of the article is that there was a significant negative correlation between the poverty density in a district on the one hand, and the proportions of births to poor women that were covered by the programme on the other. In particular, the proportions of births to poor women that the voucher programme covered were high in districts with low levels of poverty and low in districts with high poverty levels. Increasing voucher coverage among the poor in the target districts requires a mix of strategies to increase both vouchers sales and redemption. In areas where voucher coverage was low, the required increase in voucher sales to improve coverage of health facility deliveries among poor women is dependent upon improving the rate of redemption as well. Improvements in the rate of redemption can be achieved through community sensitization on the importance of seeking care, accrediting more facilities and the inclusion of public health facilities in the programme. In particular, public health facilities have a wider geographical spread and may therefore be more easily accessed thereby reducing the distances women have to travel to obtain care. For example, as of 2011, out of a total of 3237 health facilities that existed in Uganda, 71% were public while private-for-profit comprised only 9% with the remainder being private not-for-profit providers (MoH 2010b).
It is also worth noting that increased client volumes and revenue from reimbursements for services rendered to voucher clients in the private facilities offer direct financial benefits to the provider. This may in turn improve the attitude of health workers in the facilities and thus encourage more women to seek services. Community mobilization and the distributors’ ongoing interactions with pregnant women seeking vouchers could also lead to an increased uptake of facility-based delivery services (given that 72% of households live within 5 km of a facility; MoH 2010b). Thus, although the exact contribution of the voucher programme to the proportion of facility-based deliveries was not determined in this analysis, the findings highlight the scale and range of its potential effects on increasing institutional delivery among the poor.
The high programme coverage in Bushenyi and Kasese districts could also be attributed to the relatively high number of contracted facilities as well as comparatively good road and transport network. These districts also had the highest SM voucher sales during the period. Low deliveries and coverage in one-third of the programme districts could be attributed to the poor infrastructure, low number of contracted facilities and the geographical terrain that makes access to these facilities difficult. These districts are classified nationally as hard-to-reach areas (MoH 2010c). Distance to accredited facilities and poor transport networks are major factors affecting the uptake of services subsidized by the maternal health voucher programme in Uganda.
The findings of this article suggest that with enhanced voucher sales, there is a need to accredit more facilities to expand the geographical coverage of the programme. In particular, the inclusion of public health facilities in the programme offers potential for increasing the scope and coverage of contracted facilities within the regions and to address geographical access barriers. The programme could also consider mechanisms for implementing a transport voucher to facilitate access to contracted facilities. A study conducted in Uganda showed that transport vouchers contribute to increased uptake of maternal health services (Ekirapa-Kiracho et al. 2011). Other client-level factors that hinder access to facility deliveries can be addressed through increased community sensitization on the importance of seeking care. Available evidence suggests that sensitizing women alongside their male partners on pregnancy risk factors, the importance of facility delivery and working with traditionally preferred birth attendants could increase uptake of facility-based delivery services (Parkhurst et al. 2006; Mpembeni et al. 2007).
The findings of this article could, however, be influenced by the study limitations. First, the analysis rests on a number of assumptions. For example, the analysis was based on 2010 population projections by UBOS under the assumption that the growth rates remained constant over the period. Similarly, the crude birth rate was assumed to have remained constant throughout the projection period and that it was the same for both poor and non-PPs. To the extent that the population growth rates and the crude birth rates changed, this may result in either under- or over-estimation of the target populations and the coverage estimates. Second, the poverty indices were based on the 2005–06 indicators obtained from the UBOS and were assumed to have remained constant over the period. Moreover, the national poverty indicators may vary markedly from those used to identify voucher beneficiaries in the target districts and therefore the estimated size of the PP may be different. Variations in poverty indices could result in under- or over-estimation of coverage of health facility deliveries among the poor. The poverty grading tool used to target voucher recipients in the programme was also not validated against the UBOS poverty classification before the roll-out of the programme; hence, there may be differences in the identification of the poor using the two tools. Another limitation is the lack of utilization data on deliveries from non-voucher facilities including the public sector, which limits the analysis and comparison of trends in voucher and non-voucher sites.
Despite the above limitations, the findings suggest that to the extent that the maternal health voucher programme in South-western Uganda significantly stimulated demand for SM services by new users, it had the potential of increasing facility-based births among poor women in the region. The maternal health voucher costs much less than the average costs of obtaining services in either public or private facilities. Thus, although the article simply assumes that the programme stimulated demand by new users, it seems reasonable to conclude that it influenced those women who could not deliver at a health facility because they could not afford the difference between the average service costs and the voucher cost. Delivery in a health facility may in turn result in prompt management of any complications that could arise before, during and after childbirth thereby resulting in reduction in maternal and neonatal morbidity and mortality. However, some of the major challenges for the voucher programme include overcoming distance and transport barriers to care, which could be addressed by accrediting more providers including public providers in addition to subsidizing transport costs.
Although Uganda has a policy of free healthcare services in the public sector, the fact that household out-of-pocket expenditure accounts for the highest proportions of healthcare spending in the country implies that the voucher programme could subsidize the expenses that poor households continue to incur when accessing services in public health facilities. Involvement of public health facilities in the programme would not only increase voucher coverage and uptake of facility-based deliveries but also earn public facilities much needed revenue in addition to stimulating competition for voucher clients between the two sectors, which could potentially lead to improved health service quality. Evaluations of competitive voucher programmes in similar settings have highlighted significant improvements in the quality of health care in participating facilities (Meuwissen et al. 2006; Rahman et al. 2009; Ekirapa-Kiracho et al. 2011). In addition, an evaluation of a maternal health voucher programme operating in both public and private facilities in Uganda showed that voucher revenues were used to obtain supplies to improve quality and to pay health workers (Ekirapa-Kiracho et al. 2011).
Conclusion
Government funding for health generally and reproductive health specifically has remained low in Uganda. Public funding has largely focused on the supply side with households continuing to bear a high portion of healthcare costs out-of-pocket. With many competing needs against a dwindling resource base, the health sector has continually suffered from insufficient allocations of government budgets. Formal protection for the most vulnerable segments of the population including the poor is widely absent resulting in low health service utilization by those who are economically disadvantaged. Whereas supply-side government financing caters for the high capital investment in healthcare provision (Kruk et al. 2007), demand-side strategies are necessary to drive clients who would not have otherwise sought care from health facilities to do so. The SM voucher programme in South-western Uganda highlights the potential of the programmes to attract clients to seek facility services while at the same time generating much needed revenue for health facilities. The complementary roles of supply- and demand-side approaches in healthcare provision underscores the need for voucher programmes to be implemented within the broader health system context.
Acknowledgements
The Uganda reproductive health vouchers programme is funded by the German Development Bank (KfW) and the Global Partnership on Output-based Aid (GPOBA-World Bank). It is implemented by Marie-Stopes International-Uganda (MSI-U) with support from the Ministry of Health. The evaluation project is funded by GPOBA and the Bill and Melinda Gates Foundation (BMGF). MSI-U and the UBOS provided the data used in this paper. The entire study on which this paper is based received relevant ethical and research clearance from the Institutional Review Boards (IRB) of the Population Council and Mbarara University. The views expressed in this paper are, however, those of the authors and do not necessarily reflect the opinions of the agencies that funded the programme or that provided the data for analysis. L.K. did the analysis, interpretation of data and drafting of the manuscript. F.O., C.W., I.A. and B.B. were involved in the conceptual design of the study and in reviewing the manuscript for substantial intellectual content. T.A. contributed to the interpretation of the data and revision of the manuscript for substantial intellectual content.
Funding
The Uganda reproductive health vouchers programme (2008-2012) is funded by the German Development Bank (KfW) and the Global Partnership on Output-Based Aid (GPOBA-World Bank). The evaluation project is funded by GPOBA and the Bill and Melinda Gates Foundation (BMGF).
Conflict of interest
None declared.
References
- Afsana K, Rashid SF. The challenges of meeting rural Bangladeshi women’s needs in delivery care. Reproductive Health Matters. 2001;9:79–88. doi: 10.1016/s0968-8080(01)90094-1. [DOI] [PubMed] [Google Scholar]
- Agha S. Changes in the proportion of facility-based deliveries and related maternal health services among the poor in rural Jhang, Pakistan: results from a demand-side financing intervention. International Journal for Equity in Health. 2011;10:57. doi: 10.1186/1475-9276-10-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammoti-Kaguna B, Nuwaha F. Factors influencing choice of delivery sites in Rakai district of Uganda. Social Science & Medicine. 2000;50:203–13. doi: 10.1016/s0277-9536(99)00275-0. [DOI] [PubMed] [Google Scholar]
- Amone J, Asio S, Cattaneo A, et al. User fees in private non for-profit hospitals in Uganda: a survey and intervention for equity. International Journal for Equity in Health. 2005;4:6. doi: 10.1186/1475-9276-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellows B, Kyobutungi C, Mutua MK, Warren C, Ezeh A. Increase in facility-based deliveries associated with a maternal health voucher programme in informal settlements in Nairobi, Kenya. Health Policy and Planning. 2013;28:134–42. doi: 10.1093/heapol/czs030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellows NM, Bellows BW, Warren C. The use of vouchers for reproductive health services in developing countries: systematic review. Tropical Medicine and International Health. 2011;16:84–96. doi: 10.1111/j.1365-3156.2010.02667.x. [DOI] [PubMed] [Google Scholar]
- Bhatia MR, Gorter AC. Improving access to reproductive and child health services in developing countries: are competitive voucher schemes an option? Journal of International Development. 2007;19:975–81. [Google Scholar]
- Bhutta ZA, Chopra M, Axelson H, et al. Countdown to 2015 decade report (2000-10): taking stock of maternal, newborn, and child survival. Lancet. 2010;375:2032–44. doi: 10.1016/S0140-6736(10)60678-2. [DOI] [PubMed] [Google Scholar]
- Borghi JO, Ensor T, Somanathan A, et al. Mobilizing financial resources for maternal health. Lancet. 2006;368:1457–65. doi: 10.1016/S0140-6736(06)69383-5. [DOI] [PubMed] [Google Scholar]
- Campbell OMR, Graham WJ. Strategies for reducing maternal mortality: getting on with what works. Lancet. 2006;368:1284–99. doi: 10.1016/S0140-6736(06)69381-1. [DOI] [PubMed] [Google Scholar]
- Ekirapa-Kiracho E, Waiswa P, Rahman MH, et al. Increasing access to institutional deliveries using demand and supply side incentives: early results from a quasi-experimental study. BMC International Health and Human Rights. 2011;11(Suppl. 1):S11. doi: 10.1186/1472-698X-11-S1-S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essendi H, Mills S, Fotso J-C. Barriers to formal emergency obstetric care services utilization. Journal of Urban Health. 2010;88(Suppl. 2):356–69. doi: 10.1007/s11524-010-9481-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabrysch S, Cousesens S, Cox J, Campbell OMR. The influence of distance and level of care on delivery place in rural Zambia: a study linked national data in a geographic information system. PLos Medicine. 2011;8:e1000394. doi: 10.1371/journal.pmed.1000394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorter A, Sandiford P, Rojas Z, Salvetto M. Competitive Voucher Schemes for Health: Background Paper. Mexico: Instituto Centro Americano de la Salud (ICAS); 2003. [Google Scholar]
- Hill K, Thomas K, AbouZahr C, et al. Estimates of maternal mortality worldwide between 1990 and 2005: an assessment of available data. Lancet. 2007;370:1311–9. doi: 10.1016/S0140-6736(07)61572-4. [DOI] [PubMed] [Google Scholar]
- Hogan MC, Foreman KJ, Naghavi M, et al. Maternal mortality for 181 countries, 1980–2008: a systematic analysis of progress towards Millennium Development Goal 5. Lancet. 2010;375:1609–23. doi: 10.1016/S0140-6736(10)60518-1. [DOI] [PubMed] [Google Scholar]
- Ir P, Horemans A, Souk D, van Damme W. Using targeted vouchers and health equity funds to improve access to skilled birth attendants for poor women: a case study in three rural health districts in Cambodia. BMC Pregnancy and Childbirth. 2010;10:1. doi: 10.1186/1471-2393-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssen M, Maasland E, Mendys-Kamphorst E. The Economics of Demand-side Financing. Rotterdam: SEOR-ECRI; 2004. [Google Scholar]
- Kinney MV, Kerber KJ, Black RE, et al. Sub-Saharan Africa’s mothers, newborns, and children: where and why do they die? Plos Medicine. 2010;7:e1000294. doi: 10.1371/journal.pmed.1000294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruk ME, Galea S, Prescott M, Freedman PL. Health care financing and utilization of maternal health services in developing countries. Health Policy and Planning. 2007;22:303–10. doi: 10.1093/heapol/czm027. [DOI] [PubMed] [Google Scholar]
- Kyomuhendo GB. Low use of maternity services in Uganda: impact of women’s status, traditional beliefs and limited resources. Reproductive Health Matters. 2003;11:16–26. doi: 10.1016/s0968-8080(03)02176-1. [DOI] [PubMed] [Google Scholar]
- Lagomarsino G, Garabrant A, Adyas A, et al. Moving towards universal health coverage: health insurance reforms in nine developing countries in Africa and Asia. Lancet. 2012;380:933–43. doi: 10.1016/S0140-6736(12)61147-7. [DOI] [PubMed] [Google Scholar]
- Levin A, McEuen M, Dmytraczenko T, et al. Costs of Maternal Health Care Services in Three Anglophone African Countries. Special Initiatives Report 22. Bethesda, MD: Partnerships for Health Reform Project, Abt Associates Inc; 2000. [Google Scholar]
- Mahmood A. Improving Maternal and Neonatal Health: Measuring the Impact of the PAIMAN Project in Ten Districts in Pakistan Islamabad. Islamabad: Population Council; 2010. [Google Scholar]
- Meuwissen LE, Gorter AC, Kester AD, Knottnerus JA. Does a competitive voucher program for adolescents improve the quality of reproductive health care? A simulated patient study in Nicaragua. BMC Public Health. 2006;6:204. doi: 10.1186/1471-2458-6-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health. The Second National Health Policy: Promoting People’s Health to Enhance Socio-economic Development. Kampala: Ministry of Health; 2010a. [Google Scholar]
- Ministry of Health. Health Sector Strategic Plan III: 2010/11-2014/15. Kampala: Ministry of Health; 2010b. [Google Scholar]
- Ministry of Health. Annual Health Sector Performance Report: Financial Year 2008/2009. Kampala: Ministry of Health; 2010c. [Google Scholar]
- Ministry of Health. National Health Accounts: Tracking Resource Flows into the Health Systems in Uganda for the Financial Year 2008/09 and Financial Year 2009/10. Kampala: Ministry of Health; 2013. [Google Scholar]
- Moreno-Serra R, Smith PC. Does progress towards universal health coverage improve population health? Lancet. 2012;380:917–23. doi: 10.1016/S0140-6736(12)61039-3. [DOI] [PubMed] [Google Scholar]
- Mpembeni RNM, Killewo JZ, Leshabari MT, et al. Use pattern of maternal health services and determinants of skilled care during delivery in Southern Tanzania: implications for achievement of MDG-5 targets. BMC Pregnancy and Childbirth. 2007;7:29. doi: 10.1186/1471-2393-7-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musoke MGN. Maternal Health Care in Rural Uganda: Leveraging Traditional and Modern Knowledge Systems. Washington, DC: World Bank; 2002. https://openknowledge.worldbank.org/handle/10986/10798, accessed 16 October 2013. [Google Scholar]
- Njuki R, Okal J, Warren CE, et al. Exploring the effectiveness of the output-based aid voucher program to increase uptake of gender-based violence recovery services in Kenya: a qualitative evaluation. BMC Public Health. 2012;12:426. doi: 10.1186/1471-2458-12-426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obare F, Warren C, Njuki R, et al. Community-level impact of the reproductive health vouchers programme on service utilization in Kenya. Health Policy and Planning. 2013;18:165–75. doi: 10.1093/heapol/czs033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parkhurst JO, Rahman SA, Ssengooba F. Overcoming access barriers for facility-based delivery in low-income settings: insights from Bangladesh and Uganda. Journal of Health Population Nutrition. 2006;24:438–45. [PMC free article] [PubMed] [Google Scholar]
- Peters DH, Garg A, Bloom G, et al. Poverty and access to health care in developing countries. Annals of New York Academy of Science. 2007;1136:161–71. doi: 10.1196/annals.1425.011. [DOI] [PubMed] [Google Scholar]
- Rahman M, Ubaidur R, Tasnima K. Implementation of the Maternal Health Financial Scheme in Rural Bangladesh. Dhaka: Population Council; 2009. [Google Scholar]
- Ridde V, Haddad S, Nikiema B, et al. Low coverage but few inclusion errors in Burkina Faso: a community-based targeting approach to exempt the indigent from user fees. BMC Public Health. 2010;10:1–8. doi: 10.1186/1471-2458-10-631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronsmans C, Graham WJ. Maternal mortality: who, when, where, and why. Lancet. 2006;368:1189–200. doi: 10.1016/S0140-6736(06)69380-X. [DOI] [PubMed] [Google Scholar]
- Thaddeus U, Maine D. Too far to walk: maternal mortality in context. Social Science & Medicine. 1994;38:1091–110. doi: 10.1016/0277-9536(94)90226-7. [DOI] [PubMed] [Google Scholar]
- Thiede M, Akweongo P, MCintyre D. Exploring the dimensions of access. In: Mcintyre D, Mooney G, editors. The Economics of Health Equity. Cambridge: Cambridge University Press; 2007. pp. 103–23. [Google Scholar]
- Uganda Bureau of Statistics. Uganda National Household Survey 2009/2010. Kampala: Uganda Bureau of Statistics; 2010. [Google Scholar]
- Uganda Bureau of Statistics (UBOS), Macro International Inc. Uganda Demographic and Health Survey 2006. Calverton, MD: UBOS and Macro International Inc; 2007. [Google Scholar]
- Uganda Bureau of Statistics (UBOS), Macro International Inc. Uganda Demographic and Health Survey 2011. Kampala, Uganda: ICF International Inc; 2012. [Google Scholar]
- United Nations. United Nations Millennium Declaration. Resolution Adopted by the 55th Session of the General Assembly. New York: United Nations; 2000. [Google Scholar]
- United Nations. The Millennium Development Goals Report 2010. New York: United Nations; 2010. [Google Scholar]
- World Bank. World Development Report 2004: Making Services Work for Poor People. Washington, DC: World Bank; 2004. [Google Scholar]
- World Health Organization (WHO) Trends in Maternal Mortality: 1990 to 2010. Geneva: WHO; 2012. [Google Scholar]
- Xu K, Evans DB, Carrin G, et al. Protecting households from catastrophic health spending. Health Affairs. 2007;4:972–83. doi: 10.1377/hlthaff.26.4.972. [DOI] [PubMed] [Google Scholar]