Abstract
Background.
In spite of evidence that physical activity has beneficial effects on health and age-related functional decline, there is a scarcity of detailed and accurate information on objectively measured daily activity and patterns of such activity in older adults.
Methods.
Participants in the Baltimore Longitudinal Study of Aging (n = 611, 50% male, mean age 67, range 32–93) wore the Actiheart portable activity monitor for 7 days in the free-living environment. The association between activity and age was modeled using a continuous log-linear regression of activity counts on age with sex, body mass index, employment status, functional performance, and comorbid conditions as covariates.
Results.
In the fully adjusted model, continuous analyses demonstrated that overall physical activity counts were 1.3% lower for each year increase in age. Although there were no differences among morning levels of activity, there was significantly lower afternoon and evening activity in older individuals (p < .01). After adjusting for age, poor functional performance, nonworking status, and higher body mass index were independently associated with less physical activity (p < .001).
Conclusions.
The use of accelerometers to characterize minute-by-minute intensity, cumulative physical activity counts, and daily activity patterns provides detailed data not gathered by traditional subjective methods, particularly at low levels of activity. The findings of a 1.3% decrease per year in activity from mid-to-late life, and the corresponding drop in afternoon and evening activity, provide new information that may be useful when targeting future interventions. Further, this methodology addresses essential gaps in understanding activity patterns and trends in more sedentary sectors of the population.
Key Words: Epidemiology, Functional performance, Physical activity, Public health.
Individuals who are physically active tend to live longer and healthier lives (1). Higher physical activity is associated with fewer chronic diseases, better physical performance, and longer active life expectancy (2–5), yet the majority of older adults remain relatively sedentary (6,7). Despite decades of promoting physical activity across the life course, remarkably little is known about how amounts and daily patterns of free-living activity vary with age. A better understanding of these critical aspects of activity in older populations may provide necessary insight into the intensity and duration of activity essential for conducting studies and developing strategies aimed at extending health and longevity in an aging population. Two essential steps in this process are (i) obtaining accurate and reliable measures of physical activity using minimally invasive measurement tools and (ii) applying appropriate analytic techniques to optimize both the quality of the data and the extraction of information.
Although traditional subjective activity measurement tools may be easily administered and are generally inexpensive, they provide broad estimates of easily recalled activities of mostly medium-to-high intensity (8). Although these limitations may be minimized in younger, healthier populations, use of these tools in older populations may be problematic, as older individuals spend most of their time in light activities generally not categorized as “physical activity” and in whom cognitive impairments may contribute to imprecise recall (7).
Accelerometers present an objective alternative to assessing physical activity in multiple settings. In 2003–2006, the National Health and Nutrition Examination Survey used accelerometers to measure activity in persons over the age of 6, including 1,260 individuals aged 60 and older (6) and found that older adults spent only 6–10min/d in activities of moderate or greater intensity with the rest of the time spent in either a sedentary state or low-intensity activity (6). Using information limited to activity above a certain intensity threshold may be problematic when comparing activity across age groups, as activities of moderate intensity may be unattainable for many older adults. Further, intensity-related cutpoints make it challenging to assess and quantify low-intensity physical activities such as those involved in domestic and self-care tasks. The majority of older persons end up classified as “sedentary” making it difficult to discern differences in activity that may be quite meaningful for health and independence. Finally, most of the current activity metrics derived from accelerometers fail to describe and quantify daily patterns of physical activity duration and intensity that may also affect health outcomes, and offer clues to effective interventions aimed at increasing physical activity.
To address these limitations, we used accelerometers to characterize continuous minute-by-minute intensity and daily activity patterns using cumulative activity count methodology not previously employed in a large well-functioning cohort of older adults. To provide contextual validity to these measures, we tested the hypothesis that common age-related comorbidities and employment status may alter these metrics. The availability of such measures of physical activity is essential to accurately assessing and understanding the amount and type of activity necessary for maintaining health and mobility in an aging population.
Methods
Participants
The Baltimore Longitudinal Study of Aging (BLSA) is a study of normative human aging, established in 1958 and conducted by the National Institute on Aging Intramural Research Program. A general description of the sample and enrollment procedures and criteria has been previously reported (9). Briefly, the BLSA is a continuously enrolled cohort with some targeted recruitment (eg, women, racial minorities) over its history. All participants are community volunteers who must pass a comprehensive health and functional screening evaluation and be free of all major chronic conditions and cognitive and functional impairment at the time of enrollment. Once enrolled, participants are followed for life and undergo extensive testing every 1–4 years depending on age.
The sample for the current study consists of 611 men and women who underwent a comprehensive physical examination and health history assessment during their clinical visit and subsequently wore the Actiheart activity monitor for a minimum of 3 days between August 2007 and January 2011. Trained and certified technicians administered all assessments following standardized protocols. The Internal Review Board of the Medstar Research Institute approved the study protocol and all participants provided written informed consent.
Study Procedure
Participants were admitted to the clinical unit of the Translational Gerontology Branch of the National Institute on Aging for 3 days of testing. Height and weight were assessed in light clothing using a stadiometer and calibrated scale, respectively. Age, education, employment status, and history of chronic conditions were derived from a health history interview conducted by a nurse practitioner. Employment status was assessed during the health interview by asking, “Do you currently work for pay?” Type of employment (active vs sedentary job), the number of hours worked per week, and the number of volunteer hours per week were also assessed. Blood pressure was measured in the supine position, three times on each arm, alternating right and left with 1 minute in between each measurement. The mean overall blood pressure value was used to define hypertensive status. Screening for cognitive impairment was performed by the nurse practitioners using the Blessed Dementia Rating scale (10) and certified cognitive testers using the Mini-Mental State Examination (11).
To assess physical function, usual gait speed was measured over a 6-m course in an uncarpeted corridor. Participants stood with their feet behind a taped starting line and were asked to walk at their “normal comfortable pace.” After a command of “Go,” timing was initiated with the first foot-fall over the starting line and stopped after the last foot-fall over the finish line. Two-timed trials were conducted to derive usual gait speed in m/s, with the faster used for analysis.
On the last day of the BLSA clinic visit, participants were fitted with the Actiheart combined heart rate and activity monitor positioned horizontally on the chest at the third intercostal space using two standard electrocardiogram electrodes. Such chest level placement has been found to be accurate and reliable for measuring daily activity counts (12,13). Heart rate and accelerometry counts were measured in 1-minute epochs for the following 7 days in a free-living environment. Participants were asked to wear the monitor at all times, except when bathing or swimming. Extra electrodes and specific placement instructions were provided, so participants could replace the device if removed. At the end of the 7-day period, the monitors were returned to the BLSA clinical via express mail. Actiheart data was downloaded using commercial software (Actilife, version 4.0.32) to derive activity counts per minute. Although the Actiheart device collects both heart rate and activity counts per minute, the current analysis uses only the count data to assess daily activity to avoid potential error and bias that may be introduced by converting the data to energy expenditure using population level equations (12). Days with more than 5% of data missing (more than 72 minutes per day) were excluded from the analysis. For the remaining days, missing values were imputed as the average activity counts per minute over all available days for each participant.
Statistical Analysis
To preliminarily explore age-related differences in activity patterns, the sample was divided into four data-driven (equally sized) age strata: <60 years old (group 1, 142 participants), 60–67 years old (group 2, 147 participants), 68–74 years old (group 3, 157 participants), and ≥75 years old (group 4, 165 participants). Figure 1 shows the smoothed activity counts per minute (Figure 1A) and cumulatively per day (Figure 1B) for each participant in the stratified groups: group 1 (green), group 2 (red), group 3 (blue), group 4 (orange). In contrast to using activity cutpoints, cumulative activity count prevents loss of valuable information by providing total daily counts as the final data point in each plot and quantifies the dynamic intraday accumulation of activity (14).
Figure 1.
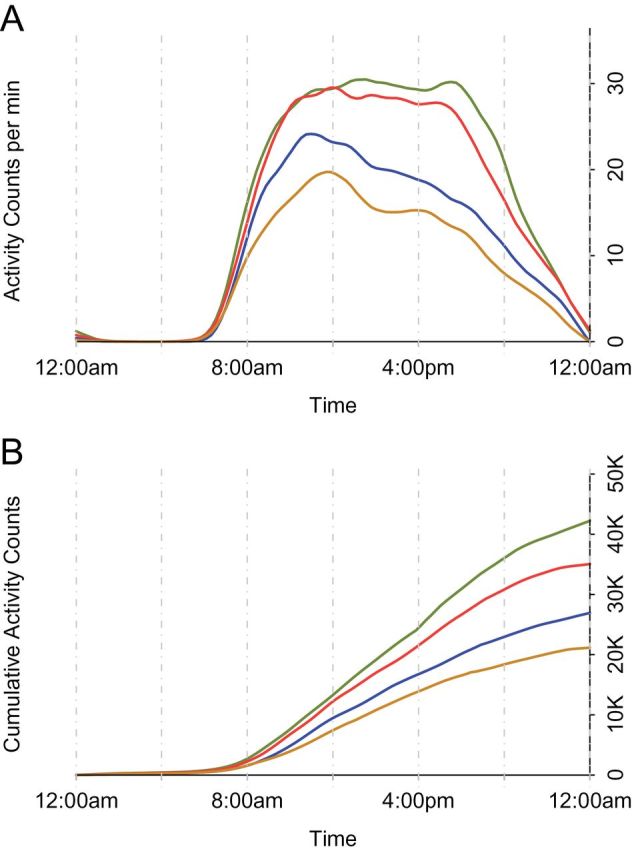
(A) Smoothed 24-hour median activity counts per minute for each age group.
(B) Smoothed medians of 24-hour cumulative activity counts per day for each age group.
Groups: <60-year old (green), 60- to 67-year old (red), 68- to 74-year old (blue), ≥75-year old (orange).
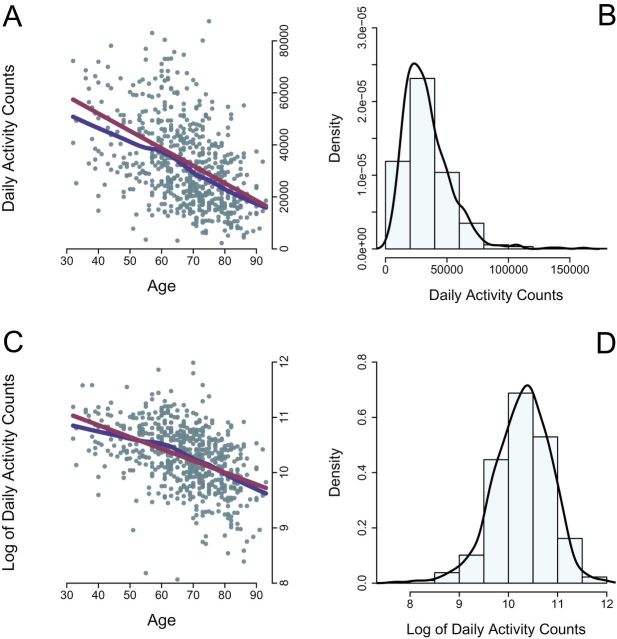
Based on these plots, the relationship between age and total daily activity counts was explored for: (i) linearity (Figure 2A), and (ii) shape (normality) of the distribution (Figure 2B). In Figure 2A, the red line represents an unadjusted linear regression fit and the blue line represents a smooth nonparametric fit. Both reveal the expected downward trend between age and total daily activity. Figure 2B reveals that the unadjusted distribution of activity counts is positively skewed. Thus, total daily activity counts were log transformed (Figure 2C and D), which resulted in a distribution much closer to normal (Figure 2D) and a reduction in heteroscedasticity around the regression line (Figure 2C). Although log transformation may make the interpretation more problematic, the fundamental message remains the same: there is a very strong negative association between age and total daily activity counts.
Figure 2.
(A) Linear (red) and nonparametric (blue) fits of the distribution of cumulative daily activity counts versus age.
(B) Histogram of the distribution of cumulative daily activity counts.
(C) Linear (red) and nonparametric (blue) fits of the log of cumulative daily activity counts versus age (left).
(D) Histogram of the distribution of log of cumulative daily activity counts.
Based on these analyses, the continuous relationship between log activity counts and age was modeled using three multiple linear regression models with increased levels of adjustment for sex, body mass index (BMI), functional status (gait speed), employment status, race, education, and comorbidities. Statistical analyses were performed using STATA (version 11; StataCorp, College Station, TX) and the lm function in the R statistical software version 2.1 (http://www.r-project.org).
Results
Participant characteristics by age group are detailed in Table 1. The mean age of the study sample was 67.0 (± 12.1, range 32–93) years. Although the proportions of men (50.4%) and women over the entire sample were similar, there were significant differences by age group, with more men in the oldest group. The younger aged groups tended to be faster and have a higher BMI than the oldest group. Years of education averaged 16.9 (± 2.3) overall and the racial composition was reflective of the BLSA enrollment: 56% white, 25% black, and 19.0% other, with the exception of the oldest age group, which had more white participants. Nearly half of the population (47.3%) reported current employment, but this was substantially weighted toward younger individuals. Of those employed, the mean number of hours worked per week was 34.6 (± 16.9). Health conditions were generally more prevalent in the older age groups, especially history of cancer, stroke, heart disease, and anemia (Table 1). Although there were differences in Mini-mental and Blessed-mental scores with age, there was no evidence of cognitive impairment.
Table 1.
Demographics of Study Population by Age Group (N = 611)
| Characteristics | Group 1, <60 y (N = 142) | Group 2, 60–67 y (N = 147) | Group 3, 68–74 y (N = 157) | Group 4, 75+ y (N = 165) | p Value* | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD (%) | Mean | SD (%) | Mean | SD (%) | Mean | SD (%) | ||
| Age (y) | 49.9 | 7.4 | 63.9 | 2.1 | 71.1 | 1.9 | 80 | 4.1 | <.001 |
| Male sex, no. | 65 | 45.8 | 55 | 37.4 | 78 | 49.7 | 105 | 63.6 | .001 |
| Body mass index (kg/m2) | 27.4 | 5.2 | 28.9 | 5.1 | 27.9 | 5.2 | 26.2 | 3.7 | <.001 |
| Usual gait speed (m/s) | 1.3 | 0.2 | 1.2 | 0.2 | 1.1 | 0.2 | 1 | 0.2 | <.001 |
| Race, no. | |||||||||
| White | 75 | 52.8 | 79 | 53.7 | 80 | 51 | 105 | 63.6 | <.001 |
| Black | 42 | 29.6 | 36 | 24.5 | 46 | 29.3 | 31 | 18.8 | .001 |
| Other | 25 | 17.6 | 32 | 21.8 | 31 | 19.7 | 29 | 17.6 | .009 |
| Education (y) | 16.8 | 2.2 | 17 | 2.4 | 16.7 | 2.6 | 17.2 | 2.3 | .256 |
| Employed, no. | 115 | 81 | 88 | 59.9 | 61 | 38.9 | 23 | 13.9 | <.001 |
| Coronary heart disease, no. | 1 | 0.7 | 13 | 8.8 | 17 | 11 | 31 | 18.7 | <.001 |
| Stroke, no. | 1 | 0.7 | 6 | 4.1 | 7 | 4.5 | 20 | 12.1 | <.001 |
| Diabetes, no. | 4 | 2.8 | 18 | 12.2 | 21 | 13.4 | 21 | 12.7 | .009 |
| Kidney disease, no. | 4 | 2.8 | 4 | 2.7 | 7 | 4.5 | 12 | 7.3 | .179 |
| Cancer, no. | 11 | 7.7 | 14 | 9.5 | 18 | 11.6 | 32 | 19.4 | .017 |
| Hypertension, no. | 0 | 0 | 3 | 2.3 | 4 | 2.7 | 10 | 6 | .014 |
| Anemia, no. | 12 | 8.5 | 18 | 12.2 | 26 | 16.8 | 54 | 32.7 | <.001 |
| Mini-mental | 28 | 1.4 | 29 | 1.3 | 28.7 | 1.3 | 28.3 | 1.7 | .005 |
| Blessed mental | 1.2 | 1.2 | 1.4 | 1.5 | 1.4 | 1.8 | 1.8 | 2 | 0.003 |
| Median daily activity counts | 42,460 | 20,892 | 32,112 | 16,939 | 26,823 | 19,888 | 21,163 | 12,427 | <.001 |
Note: *p value for group comparisons, analysis of variance for continuous measure, and chi-square test for proportions.
Daily activity counts for all participants averaged 30,125 (± 19,263) per 24 hours, were highest in those younger than 60 years of age, and progressively lower in older participants (Table 1, Figure 1B). There was large variability across age groups, with standard deviations ranging from 49.2% in group 1 to 74.2% of the median activity count in the group 3. To evaluate daily activity patterns, unadjusted median activity counts per minute were also assessed over the same 24-hour period (Figure 1A). Although daily activity tended to initiate between 6 and 7 am regardless of age (Figure 1A and B), there were strong contrasts between age groups regarding time-of-day of peak per minute activity. Additionally, median activity intensity decreased immediately after reaching its peak in the two older age groups, losing approximately 25% of its intensity between 11 am and 3 pm in the oldest adults, whereas median activity intensity in the younger two age groups was sustained well after 5 pm (Figure 1A). Formal tests of the difference in activity counts between the youngest (group 1) and the oldest age groups (group 4) were insignificant at 8 am (t test: p = .13), but were highly significant at 9 am (t test: p < .001), 12 pm (t test = p < .001), and 6 pm (t test = p < .001).
The continuous linear association between age and log cumulative daily activity was analyzed using a three-stage linear regression model (Table 2). Stage one modeled the relationship between age and log cumulative activity counts and revealed a significant negative association (β = −0.021, p < .001) (Table 2, Model 1), with an estimated 2% relative loss of activity counts for each increased year of age. Stage two introduced sex and BMI as covariates (Table 2, Model 2), and revealed BMI as a significant negative and independent predictor of activity (β = −0.037, p < .001). Finally, stage three included covariates for demographics, functional status (gait speed), and history of comorbidities including: race, years of education, current employment status, cognitive status, history of cardiovascular disease, stroke, hypertension, diabetes, kidney disease, cancer, and anemia. Current employment (β = 0.150, p < .001) and faster gait speed (β = 0.619, p < .001) were independently associated with greater activity, and history of stroke was associated with less activity (β = −0.230, p = .005). All other variables were not significant and excluded from the final model (Table 2, Model 3). In the fully adjusted model, the estimated relative loss of activity counts for each increased year of age was 1.3%, compared with 2.0% in the unadjusted model.
Table 2.
Association Between Log of Cumulative Daily Activity Counts and Age (N = 611) Modeled Using a Three-Stage Linear Regression Model
| Dependent Variable | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| Log daily cumulative activity counts | R 2 = .20 | R 2 = .30 | R 2 = .37 | |||
| Independent Variables | β | p | β | p | β | p |
| Age | −0.021 | <.001 | −0.023 | <.001 | −0.014 | <.001 |
| Intercept | 11.716 | <.001 | 12.825 | <.001 | 11.27 | <.001 |
| Male sex | 0.026 | .496 | 0.012 | .757 | ||
| Body mass index | −0.037 | <.001 | −0.03 | <.001 | ||
| Employment | 0.15 | <.001 | ||||
| Usual gait speed | 0.619 | <.001 | ||||
| Stroke | −0.23 | .005 | ||||
Notes: Model 1 shows the beta-coefficient and p value from a simple linear regression model assessing the relationship between age and the log of cumulative daily activity counts.
Model 2 expands upon model 1 by adding sex and body mass index to the model.
Model 3 expands upon model 2 by adding employment status (yes or no), usual gait speed (m/s), and history of stroke (yes or no). Variables for race, education, cardiovascular disease, hypertension, diabetes, kidney disease, cancer, and anemia were not significant and not included in the final model.
To further explore the relationship between employment and daily activity counts, each group was stratified by employment status (employed/not employed): group 1 (115/27 participants), group 2 (88/59 participants), group 3 (61/96 participants), group 4, (23/142 participants) and a two group t test was used to formally test for differences in the log of cumulative daily activity counts by employment status. Those who were employed tended to be more active, but the difference was only significant in group 1 (p < .01, Table 3).
Table 3.
Test of Differences in Mean Log Cumulative Activity Counts per Day, Stratified by Age and Employment Status
| N | Total | Group 1 | Group 2 | Group 3 | Group 4 |
|---|---|---|---|---|---|
| Employed | 287 | 115 | 88 | 61 | 23 |
| Not Employed | 324 | 27 | 59 | 96 | 142 |
| Employed | 10.45 | 10.7 | 10.45 | 10.24 | 10.09 |
| Not employed | 10.13 | 10.4 | 10.41 | 10.1 | 9.88 |
| p value | <.001* | .009* | .45 | .07 | .17 |
Note: *Significantly different (p < .05).
A similar analysis was performed to explore the association between functional status and daily activity counts. Each age group was stratified by median gait speed (1.14 m/s, faster/slower): group 1 (102/40 participants), group 2 (96/51 participants), group 3 (67/90 participants), group 4 (37/128 participants), and a two group t test was used to formally test for differences in the log of cumulative daily activity counts by gait speed. Faster individuals were significantly more active than the slower individuals across all groups (p = .01, Table 4).
Table 4.
Test of Differences in Mean Log Cumulative Activity Counts per Day, Stratified by Age and Functional Status
| N | Total | Group 1 | Group 2 | Group 3 | Group 4 |
|---|---|---|---|---|---|
| Gait speed < 1.14 m/s | 302 | 102 | 96 | 67 | 37 |
| Gait speed ≥ 1.14 m/s | 309 | 40 | 51 | 90 | 128 |
| Slow | 10.1 | 10.41 | 10.33 | 10.05 | 9.86 |
| Fast | 10.49 | 10.7 | 10.56 | 10.28 | 10.22 |
| p value | <.001* | .01* | .006* | <.001* | .001* |
Note: *Significantly different (p < .05).
Discussion
Through minute-by-minute analyses of accelerometry data in a relatively large population, this study demonstrated that the amount of physical activity in daily life is progressively lower with age and follows a different daily pattern in older compared with younger individuals. In addition, after controlling for age, poor functional status, nonworking status, and higher BMI are significantly and independently associated with lower physical activity.
Although not completely unexpected, the magnitude of the difference in daily activity between the youngest and oldest age groups is remarkable, particularly between the ages of 60 and 74. Although part of the association may be explained by retirement, after adjusting for employment status, the strength of the association between age and physical activity was only partially reduced. As demonstrated in the fully adjusted analysis, those who were employed were more active. Interestingly, the type of employment (active vs sedentary job), the number of hours worked per week, and the number of volunteer hours per week were not associated with the global amount of daily activity. As demonstrated in the stratified subgroup analysis, the positive effect of employment was strongest in the youngest age group. The importance of employment in maintaining daily activity is consistent with previous work in 20–60-year olds in the National Health and Nutrition Examination Survey (15) and confirms the idea that having consistent employment is an important driver of physical activity in middle-aged and older individuals. Longitudinal analyses of the employment—activity relationship are warranted, specifically to determine if employment into the later years of life attenuates the decline in activity among those who remain employed. Additional efforts should be made by clinicians and public health professionals to encourage participation in a greater number of recreational activities after retirement to attenuate this difference in activity levels.
Age-related differences in the daily pattern of physical activity suggest that although younger and older participants were similarly active at the beginning of the day, older persons became less and less active as the day progressed. The evidence of greater activity by higher functional status (gait speed) combined with lower activity as the day progresses may implicate fatigue as a potential modifier in this relationship. Older adults tended to reach their peak activity level much earlier in the day, which may indicate that daily tasks such as bathing, dressing, running errands, and volitional physical exercise are performed in the morning hours with little activity later in the day. These findings are consistent with previous work in middle-aged women that demonstrated decreased activity as the day continued (16) and suggest a low threshold for fatigue may contribute to a sedentary lifestyle and its age-associated consequences.
Previous research exploring the association between aging and activity has traditionally been limited to smaller samples, subjective assessment methods, or driven by activity-defined cutpoints (2,6,16–18). This study examined the relationship between daily activity and age, accounting for mobility, employment, and common age-related health factors, using cumulative activity counts and median counts per minute. This allows for superior visualization and exploration of the association between age and activity, while minimizing the loss of information that results from using activity cutpoints. Further, the large amount of heterogeneity and skewness in the activity intensity curves (Figure 2A–D) indicates that using cutpoints and means to define the data rather than robust approaches, such as medians and quantiles, may lead to spurious results.
This study has several potential limitations. First, due to the demands of attending a 3-day clinic visit, the study population is healthier than the general population, particularly the oldest participants, and may underestimate the true yearly age-related reduction in daily activity. Additionally, because the BLSA actively enrolls healthy individuals, there may be a healthy person bias that understates the relationships of comorbidities, employment, and age with physical activity. Second, this study uses cross-sectional data to estimate age-related differences and it is not clear whether the developed metrics are sensitive to change over time, warranting further testing in longitudinal analyses.
The use of accelerometers to characterize minute-by-minute intensity, cumulative physical activity counts, and daily activity patterns provides more detailed information, particularly with regard to lower levels of activity. This methodology is an essential step in assessing and understanding the true amount of activity performed by relatively sedentary sectors of the population and may clarify the level of physical activity needed for preventative purposes in future longitudinal studies involving physical activity, comorbidities, and aging.
Funding
This research was supported by the Intramural Research Program of the NIH, National Institute on Aging. Data for these analyses were obtained from the Baltimore Longitudinal Study of Aging, a study performed by the National Institute on Aging. Crainiceanu's research was supported by the National Institute of Neurological Disorders and Stroke (R01NS060910).
References
- 1. The Surgeon General’s Vision for a Healthy and Fit Nation. Rockville: US Department of Health and Human Services; 2010:21 [Google Scholar]
- 2. Yorston LC, Kolt GS, Rosenkranz RR. Physical activity and physical function in older adults: the 45 and up study. J Am Geriatr Soc. 2012;60:719–725. 10.1111/j.1532-5415.2012.03906.x. [DOI] [PubMed] [Google Scholar]
- 3. Pate RR, Pratt M, Blair SN, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273:402–407. 10.1001/jama.1995.03520290054029. [DOI] [PubMed] [Google Scholar]
- 4. Ferrucci L, Alley D. Obesity, disability, and mortality: a puzzling link. Arch Intern Med. 2007;167:750–751. 10.1001/archine.167.8.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Leveille SG, Guralnik JM, Ferrucci L, Langlois JA. Aging successfully until death in old age: opportunities for increasing active life expectancy. Am J Epidemiol. 1999;149:654–664 [DOI] [PubMed] [Google Scholar]
- 6. Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–188. 10.1249/mss.0b013e31815a51b3 [DOI] [PubMed] [Google Scholar]
- 7. Washburn RA. Assessment of physical activity in older adults. Res Q Exerc Sport. 2000;71:S79–S88 [PubMed] [Google Scholar]
- 8. Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport. 2000;71(s uppl 2):S1–14 [PubMed] [Google Scholar]
- 9. Stone JL, Norris AH. Activities and attitudes of participants in the Baltimore longitudinal study. J Gerontol. 1966;21:575–580. 10.1093/geronj/21.4.575. [DOI] [PubMed] [Google Scholar]
- 10. Blessed G, Tomlinson BE, Roth M. The association between quantitative measures of dementia and of senile change in the cerebral grey matter of elderly subjects. Br J Psychiatry. 1968;114:797–811. 10.1192/bjp.114.512.797 [DOI] [PubMed] [Google Scholar]
- 11. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 12. Villars C, Bergouignan A, Dugas J, et al. Validity of combining heart rate and uniaxial acceleration to measure free-living physical activity energy expenditure in young men. J Appl Physiol (1985). 2012;113:1763–1771. 10.1152/japplphysiol.01413.2011 [DOI] [PubMed] [Google Scholar]
- 13. Brage S, Brage N, Ekelund U, et al. Effect of combined movement and heart rate monitor placement on physical activity estimates during treadmill locomotion and free-living. Eur J Appl Physiol. 2006;96:517–524. 10.1007/s00421-005-0112-6 [DOI] [PubMed] [Google Scholar]
- 14. Bai J, He B, Glass T, Crainiceanu C. Normalization and extraction of interpretable metrics from raw accelerometry data. Biostatistics. 2013; September 1 - Epub ahead of print. 10.193/biostatistics/kxt029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Van Domelen DR, Koster A, Caserotti P, et al. Employment and physical activity in the U.S. Am J Prev Med. 2011;41:136–145. 10.1016/j.amepre.2011.03.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pettee Gabriel K, McClain JJ, High RR, Schmid KK, Whitfield GP, Ainsworth BE. Patterns of accelerometer-derived estimates of inactivity in middle-age women. Med Sci Sports Exerc. 2012;44:104–110. 10.1249/MSS.0b013e318229056e [DOI] [PubMed] [Google Scholar]
- 17. Hansen BH, Kolle E, Dyrstad SM, Holme I, Anderssen SA. Accelerometer-determined physical activity in adults and older people. Med Sci Sports Exerc. 2012;44:266–272. 10.1249/MSS.0b013e31822cb354 [DOI] [PubMed] [Google Scholar]
- 18. Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003-2004. Am J Epidemiol. 2008;167:875–881. 10.1093/aje/kwm390 [DOI] [PMC free article] [PubMed] [Google Scholar]