Abstract
Background
There is increasing attention to labor induction and cesarean delivery occurring at 37 0/7 – 38 6/7 weeks’ gestation (early-term) without medical indication.
Objective
To measure prevalence, change over time, patient characteristics, and infant outcomes associated with early-term nonindicated births.
Research Design and Subjects
Retrospective analysis using linked hospital discharge and birth certificate data for the 7,296,363 uncomplicated term (>37 0/7 weeks’ gestation) births between 1995-2009 in 3 states.
Measures
Early-term nonindicated birth is calculated using diagnosis codes and birth certificate records. Secondary outcomes included infant prolonged length of stay and respiratory distress.
Results
Across uncomplicated term births, the early-term nonindicated birth rate was 3.18%. After adjustment, the risk of nonindicated birth before 39 weeks was 86% higher in 2009 than 1995 (hazard ratio [HR]=1.86 [95% confidence interval (CI), 1.81–1.90]), peaking in 2006 (HR=2.03; P < .001). Factors independently associated with higher odds included maternal age, higher education levels, private health insurance, and delivering at smaller-volume or nonteaching hospitals. Black women had higher risk of nonindicated cesarean birth (HR=1.29 [95% CI, 1.27–1.32]), which was associated with greater odds of prolonged length of stay (adjusted odds ratio [AOR]=1.60 [95% CI, 1.57–1.64]) and infant respiratory distress (AOR= 2.44 [95% CI, 2.37–2.50]) compared with births after 38 6/7 weeks. Early-term nonindicated induction was also associated with comparatively greater odds of prolonged length of stay (AOR=1.20 [95% CI, 1.17–1.23]).
Conclusion
Nearly 4% of all uncomplicated births to term infants occurred before 39 0/7 weeks' gestation without medical indication. These births were associated with adverse infant outcomes.
Keywords: obstetrics, cesarean, labor induction, preterm, elective, maternal, infant
Introduction
Childbirth is the most common reason for hospitalization in the United States,1 and the past 2 decades have seen major shifts in childbirth-related care.2 One notable change has been a decline in the average gestational age for singleton births from 40 weeks in 1992 to 39 weeks in 2002. This change was driven by a decrease in births after 40 weeks’ gestation and increases in late-preterm (34 0/7 –36 6/7 weeks) and early-term (37 0/7 –38 6/7 weeks) births.3,4 Early-term births are associated with adverse outcomes, including increased infant mortality risk for infants born at 37 vs. 40 weeks’ completed gestation,5 and higher rates of maternal morbidity, respiratory illness, and neonatal intensive care admissions for births at 37–38 weeks’ completed gestation compared with those at 39 weeks.6–8 There are no prior studies linking population-based data with hospital data to show when and among whom the rise in early-term nonindicated births has occurred in the U.S.
Medical indications, such as premature rupture of membranes, placentation abnormalities, or other maternal or fetal conditions may necessitate late-preterm and early-term iatrogenic birth. Trends in early-term birth might also result from changes in provider and/or patient preferences. Although hospital policies have reduced early-term nonindicated births among patients,9–11 the studies demonstrating these effects come from institutions or health care systems rather than a population-based perspective. Data on rates, changes over time, and effects of early-term births (indicated and nonindicated) on infant outcomes are constrained by data limitations, including a dearth of population-based linked datasets available for such analyses. Data on early-term nonindicated births drawn from broad populations can provide a baseline for implementing, tailoring, and evaluating the growing number of clinical and policy efforts to improve the quality of childbirth care and perinatal outcomes for women and infants.
The goal of this analysis was to measure rates of early-term nonindicated births, changes in rates from 1995 to 2009, and patient-level predictors, using linked birth certificate and hospital discharge data for all births in 3 US states. We also looked at the relationship between early-term nonindicated birth and adverse neonatal outcomes. This analysis offers important information on the characteristics of early-term nonindicated births in a population-based sample and reveals that the extent to which term infants are born too soon and without medical indication.
Methods
Data and Study Population
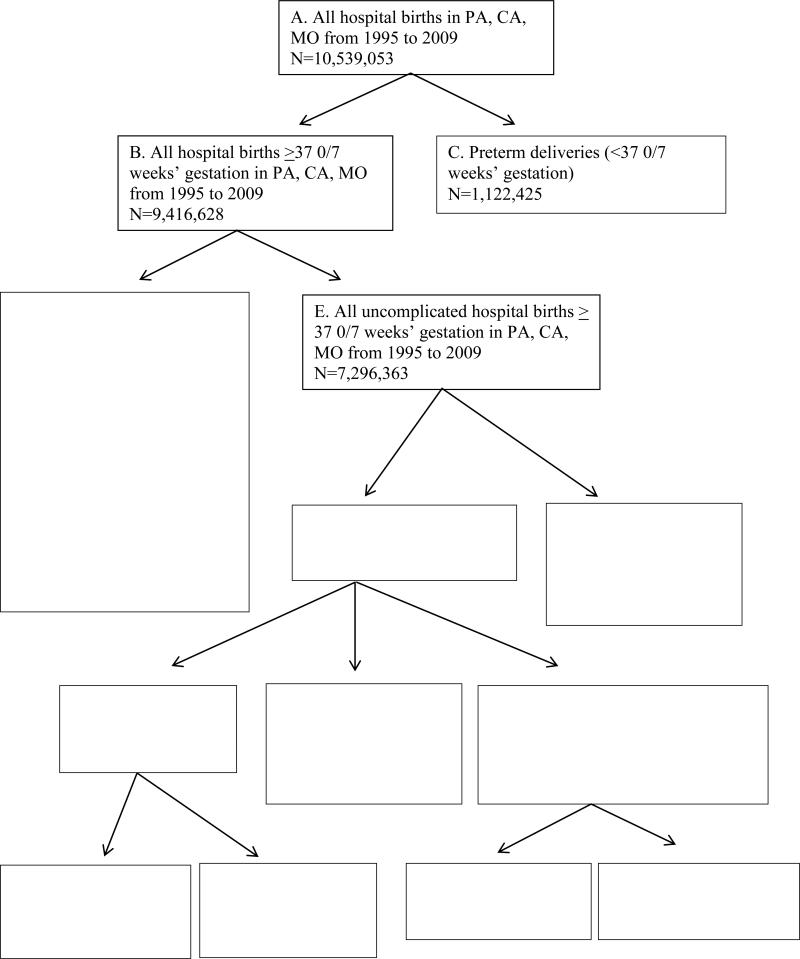
Statewide hospital discharge data on childbirth hospitalizations from 1995 to 2009 in California, Missouri, and Pennsylvania was linked to birth-certificate data using social security numbers for maternal records and a virtual identifier for infant records, with a 98% match rate, as described previously.12–15 These 3 states represent approximately 20% of all US births and together encompass a population with a wide range of sociodemographic characteristics and geographic locations. Figure 1 presents information on the study population, exclusion criteria, and comparison groups. We began with 10,539,053 live hospital-based births and excluded preterm deliveries (n= 1,122,425). The data set contained 9,416,628 births occurring on or after 37 0/7 weeks’ gestation, over 15 years. To focus on uncomplicated births, we excluded the 2,120,265 births with any of the following antepartum maternal diagnoses, defined by International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes: chronic hypertension, diabetes mellitus, renal disease, thyroid disease, congenital cardiac problem, lupus, disorders of placentation, gestational hypertension, gestational diabetes, eclampsia, chorioamniotis, preterm labor, premature rupture of membranes, oligohydramnios, placenta previa, placenta abruption, and cord abnormalities. The final study population included 7,296,363 uncomplicated births on or after 37 0/7 weeks’ gestation, occurring between 1995 and 2009 in 3 states. These births include early-term (n=1,911,015) and term births (n=5,388,667). Term births include full-term (39 0/7 – 40 6/7 weeks’ gestation), late-term (41 0/7 – 41 6/7) and postterm (>42 0/7) births.16 The study was approved by the Institutional Review Board of the Children's Hospital of Philadelphia and the state departments of health in Missouri, California, and Pennsylvania.
Figure 1.
Study population
Variable Measurement
The main outcome was early-term nonindicated birth, defined as a nonmedically indicated birth occurring between 37 0/7 and 38 6/7 weeks of gestation.17 There were 464,847 medically indicated early-term births, and 232,189 nonmedically indicated early-term births. We distinguish 2 mutually-exclusive categories of early-term nonindicated births based on how labor began: induction of labor and cesarean delivery without labor. All mothers whose labor was induced are included in the induction of labor category, regardless of whether they ultimately delivered vaginally or via cesarean. Spontaneous early-term births were identified as those without codes indicating either labor induction or cesarean without labor (n=1,213,979, See Figure 1). These categories replicate, as closely as these data allow, the definition of “elective delivery” in the Specifications Manual for Joint Commission National Quality Measures for Perinatal Care Measure PC-01 and listed in Appendix A of the manual (Tables 11.07 and 11.09).
We identified medical indications based on ICD-9-CM codes classified in the manual as “conditions possibly justifying elective delivery prior to 39 weeks gestation” and “contraindications to vaginal delivery,” which are listed in Supplemental Digital Content. Examples of both groups included premature rupture of membranes, antepartum hemorrhage, and hypertensive disorders (medical indications for labor induction) and multiple gestation or malpresentation (contraindications for vaginal delivery). The measure of gestational age was based on the best estimate listed on birth certificate records.
Since mortality is rare in this group of infants, we conducted an analysis of adverse neonatal outcomes, including prolonged infant length of stay and infant respiratory distress. We defined prolonged length of stay as any hospitalization where the infant's discharge date was after the mother's. Because Pennsylvania did not report discharge dates, we defined prolonged length of stay in that data set as one that exceeded 3 days for a vaginal delivery or 5 days for a cesarean delivery. We conducted sensitivity analyses on this outcome, excluding Pennsylvania, and results were substantively unchanged. We defined infant respiratory distress using ICD-9-CM codes for respiratory distress or ventilation during the hospitalization.7
Individual-level covariates included race/ethnicity, education, income, marital status, and maternal health insurance status as indicated on birth certificate records. We measured maternal preexisting comorbid conditions, antepartum complications of pregnancy, and intrapartum complications using ICD-9-CM diagnosis and procedure codes recorded in hospital discharge data. Hospital characteristics included birth volume, categorized as high (>5000 deliveries per year), medium (1000–5000 deliveries per year), low (250–1000 deliveries per year), and very low (<250 deliveries per year); rural (vs. urban) location (based on 2000 census designation); and obstetric teaching affiliation (based on American Hospital Association classification).
Analysis
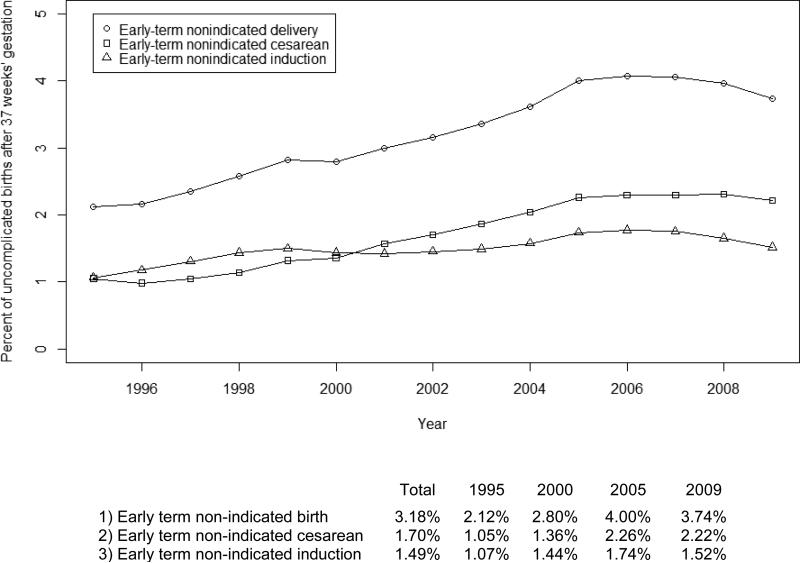
We calculated early-term nonindicated births at the individual level as dichotomous indicators among uncomplicated births between on or after 37 0/7 weeks’ gestation. We used a validated technique representing a rate of this outcome among fetuses-at-risk.8,18 Fetuses-at-risk models are used for all analyses so that denominators represent all pregnancies with potential for early-term nonindicated delivery. We also tested a rate-based method, where the denominator comprised all deliveries from 37 0/7 to 38 6/7, and results were robust to this alternative measure. Figure 2 presents the annual percentages of early-term nonindicated births (as a percentage of all term births) overall and distinguished by method of initiating delivery (induction or cesarean) over time (1995–2009). In addition, we report descriptive statistics for early-term nonindicated births (again distinguishing labor induction and cesarean without labor) compared with all other uncomplicated births on or after 37 0/7 weeks’ gestation, based on maternal and hospital variables in Table 1. We used Cox proportional hazards models to conduct a survival analysis among all births eligible for study outcomes, controlling for maternal demographic and socioeconomic variables and hospital characteristics, year, and state. The advantage of using proportional hazard models for this type of analysis is that we can include all women with the potential to deliver early without indication, even if they ultimately delivered after 38 6/7 weeks’ gestation.18 Women who delivered spontaneously were censored at either 39 0/7 weeks or time of delivery, whichever came first.
Figure 2. Change over time in the percentage of term births that are early-term nonindicated births.
Note: Percentage of uncomplicated births on or after 37 0/7 weeks’ gestation that are (1) early-term nonindicated births (either cesarean or induction), (2) early-term nonindicated cesareans, or (3) early-term nonindicated inductions, in 3 US states from 1995 to 2009 (n =7,296,363). Early-term births occur at 37 0/7 to 38 6/7 weeks’ gestation. Measurement of pregnancy complications and indications for cesarean and induction are defined based on measures used by the Joint Commission. Percentages are calculated using a fetuses-at-risk approach.
TABLE 1.
Population Characteristics Stratified by Early-Term Nonindicated Delivery, Unadjusted Values
| All full-term, uncomplicated pregnancies (n = 7,296,363) | Early-term nonindicated deliveries (n = 232,189) | |||
|---|---|---|---|---|
| Early-term nonindicated delivery (any) n = 232,189 n (%) | All other deliveries n = 7,064,174 n (%) | Early-term nonindicated cesarean n = 123,740 n (%) | Early-term nonindicated induction n = 108,449 n (%) | |
| Maternal age | ||||
| <20 | 20,990 (9.04) | 739,662 (10.47) | 13,289 (10.74) | 7701 (7.1) |
| 20–24 | 49,297 (21.23) | 1,696,269 (24.01) | 26,414 (21.35) | 22,883 (21.1) |
| 25–29 | 61,204 (26.36) | 1,949,323 (27.59) | 30,611 (24.74) | 30,593 (28.21) |
| 30–34 | 58,215 (25.07) | 1,688,790 (23.91) | 29,143 (23.55) | 29,072 (26.81) |
| 35+ | 42,477 (18.29) | 990,019 (14.01) | 24,279 (19.62) | 18,198 (16.78) |
| Race | ||||
| White Non-Hispanic | 126,019 (54.27) | 3,306,378 (46.8) | 58,662 (47.41) | 67,357 (62.11) |
| Black Non-Hispanic | 17,020 (7.33) | 523,175 (7.41) | 11,043 (8.92) | 5977 (5.51) |
| Asian/Pacific Islander Non- Hispanic | 20,300 (8.74) | 628,663 (8.9) | 12,473 (10.08) | 7827 (7.22) |
| Hispanic | 63,696 (27.43) | 2,416,912 (34.21) | 38,463 (31.08) | 25,233 (23.27) |
| Education | ||||
| No high school | 13,265 (5.71) | 614,408 (8.7) | 8180 (6.61) | 5085 (4.69) |
| Some high school | 32,382 (13.95) | 1,193,346 (16.89) | 18,564 (15) | 13,818 (12.74) |
| High school diploma/GED | 63,445 (27.32) | 2,014,831 (28.52) | 33,068 (26.72) | 30,377 (28.01) |
| At least some college | 118,860 (51.19) | 3,118,781 (44.15) | 61,543 (49.74) | 57,317 (52.85) |
| Insurance status | ||||
| Medicaid | 85,668 (36.9) | 2,950,596 (41.77) | 49,747 (40.2) | 35,921 (33.12) |
| Private FFSa | 23,682 (10.2) | 701,689 (9.93) | 11,534 (9.32) | 12,148 (11.2) |
| Private HMOb | 114,100 (49.14) | 3,082,056 (43.63) | 57,758 (46.68) | 56,342 (51.95) |
| Uninsured | 1782 (0.77) | 82,598 (1.17) | 813 (0.66) | 969 (0.89) |
| Hospital volume | ||||
| Very low (<250) | 4779 (2.06) | 143,384 (2.03) | 2583 (2.09) | 2196 (2.02) |
| Low (250–1000) | 37,075 (15.97) | 1,112,101 (15.74) | 17,923 (14.48) | 19,152 (17.66) |
| Medium (1000–5000) | 16,3358 (70.36) | 5,040,219 (71.35) | 87,411 (70.64) | 75,947 (70.03) |
| High (5000+) | 26,977 (11.62) | 768,470 (10.88) | 15,823 (12.79) | 11,154 (10.29) |
| Geographic location | ||||
| Urban | 220,540 (94.98) | 6,743,675 (95.46) | 118,333 (95.63) | 102,207 (94.24) |
| Rural | 9711 (4.18) | 260,412 (3.69) | 4332 (3.5) | 5379 (4.96) |
| Hospital teaching status | ||||
| Teaching | 25,942 (11.17) | 862,079 (12.2) | 15,446 (12.48) | 10,496 (9.68) |
| Nonteaching | 202,326 (87.14) | 6,041,616 (85.52) | 106,062 (85.71) | 96,264 (88.76) |
| Year | ||||
| 1995 | 10,913 (4.7) | 504,859 (7.15) | 5418 (4.38) | 5495 (5.07) |
| 1996 | 10,757 (4.63) | 487,645 (6.9) | 4898 (3.96) | 5859 (5.4) |
| 1997 | 11,376 (4.9) | 472,438 (6.69) | 5058 (4.09) | 6318 (5.83) |
| 1998 | 12,337 (5.31) | 467,091 (6.61) | 5457 (4.41) | 6880 (6.34) |
| 1999 | 13,473 (5.8) | 464,275 (6.57) | 6306 (5.1) | 7167 (6.61) |
| 2000 | 13,657 (5.88) | 474,770 (6.72) | 6644 (5.37) | 7013 (6.47) |
| 2001 | 14,351 (6.18) | 465,010 (6.58) | 7516 (6.07) | 6835 (6.3) |
| 2002 | 14,870 (6.4) | 455,861 (6.45) | 8019 (6.48) | 6851 (6.32) |
| 2003 | 16,049 (6.91) | 461,347 (6.53) | 8927 (7.21) | 7122 (6.57) |
| 2004 | 17,225 (7.42) | 459,100 (6.5) | 9721 (7.86) | 7504 (6.92) |
| 2005 | 19,500 (8.4) | 467,984 (6.62) | 11,026 (8.91) | 8474 (7.81) |
| 2006 | 20,382 (8.78) | 480,422 (6.8) | 11,489 (9.28) | 8893 (8.2) |
| 2007 | 20,383 (8.78) | 482,469 (6.83) | 11,547 (9.33) | 8836 (8.15) |
| 2008 | 19,478 (8.39) | 472,072 (6.68) | 11,362 (9.18) | 8116 (7.48) |
| 2009 | 17,438 (7.51) | 448,831 (6.35) | 10,352 (8.37) | 7086 (6.53) |
Notes: P< .001 for all comparisons of early-term nonindicated deliveries compared with all other deliveries and by delivery mode among early- term nonindicated deliveries. Missing responses that constitute <2% are not shown; thus, columns may not sum to 100%.
FFS, Fee For Service
HMO, Health Maintenance Organization
These models used clustered standard errors to account for correlation among births in the same hospitals.19,20 We used logistic regression models to measure the association between early-term nonindicated birth (initiated by induction or cesarean) and prolonged length of stay and infant respiratory distress or ventilation, where the reference group consisted of infants born on or after 39 0/7 weeks’ gestation. We included infants with a medically indicated induction or cesarean as separate categories in these models, consistent with prior research.7,8 We present unadjusted odds and estimates adjusted for maternal characteristics, gestational age, intrapartum complications (cephalo-pelvic disproportion, infection, and hemorrhage), hospital characteristics, year, and state. We conducted sensitivity analyses of all regression models with all births on or after 37 0/7 weeks (including complicated pregnancies); we also analyzed impacts on secondary outcomes stratifying for mode of delivery. Results were stable to these alternative specifications. All analyses were conducted using SAS, version 9.3.
Results
Between 1995 and 2009, across 3 states, 232,189 infants were born between 37 0/7 and 38 6/7 weeks’ gestation without medical indication. Across all uncomplicated births in 3 states with a gestational age of at least 37 0/7 weeks, 3.2% were early-term nonindicated births. This rate increased from 2.1% in 1995 to 4.0% in 2005 and declined slightly thereafter to 3.7% by 2009. Early-term nonindicated labor induction occurred for 1.5% of births; early-term nonindicated cesarean was slightly more prevalent, at 1.7% of all births. Figure 2 illustrates trends over time in early-term nonindicated births (overall and distinguished as induction or cesarean) and indicates a more rapid increase in early-term nonindicated cesarean than induction. The share experiencing a prolonged length of stay remained fairly stable, at around 6.5%, while infant respiratory distress and ventilation increased over the study period from 2.6% in 1995 to 3.5% in 2009.
Women who had early-term nonindicated births differed from those who did not (Table 1); a higher percentage were over age 35, non-Hispanic white, and college educated. Medicaid was the primary payer for 36.9% of early-term nonindicated births, but 41.8% of all other deliveries. There were differences between women receiving early-term induction of labor and those receiving a cesarean section without labor. Minority racial/ethnic status was associated with higher rates of early-term nonindicated cesarean without labor, whereas non-Hispanic white women had comparatively higher rates of early-term nonindicated induction.
Table 2 presents results from multivariable Cox proportional hazards models that assess the relationship between patient and hospital characteristics and the risk of early-term nonindicated births. Among women with uncomplicated births on or after 37 0/7 weeks’ gestation, the risk of eary-term nonindicated birth was highest in 2006, with slightly more than double the risk compared with 1995 (hazard ratio [HR], 2.03 [95% confidence interval (CI), 1.98–2.08]) after controlling for maternal demographic and socioeconomic characteristics, hospital factors, and state. At the end of the study period in 2009, the risk of early-term nonindicated birth among uncomplicated term births was 86% higher than in 1995 (HR, 1.86 [95% CI, 1.81–1.90]). Factors associated with higher risk of early-term nonindicated birth included advanced maternal age (age 35 or older), non-Hispanic white race, higher education levels, private health insurance, and delivering at smaller-volume or nonteaching hospitals.
TABLE 2.
Hazard of Early-Term Nonindicated Delivery, Overall and by Mode of Delivery Initiation (Cesarean versus Induction), Controlling for Patient and Hospital Factors (N=7,296,363)
| Early-term nonindicated delivery (any) HR (95% CI)a | Early-term nonindicated cesarean HR (95% CI)a | Early-term nonindicated labor induction HR (95% CI)a | |
|---|---|---|---|
| Maternal age | |||
| <20 | 1.00 (0.98, 1.01) | 1.20 (1.18, 1.23) | 0.77 (0.75, 0.79) |
| 20–24 | 0.96 (0.95, 0.97) | 1.00 (0.99, 1.02) | 0.91 (0.90, 0.93) |
| 25–29 | Reference | Reference | Reference |
| 30–34 | 1.07 (1.06, 1.08) | 1.09 (1.07, 1.1) | 1.06 (1.04, 1.07) |
| 35+ | 1.30 (1.29, 1.32) | 1.51 (1.49, 1.54) | 1.11 (1.09, 1.13) |
| Race | |||
| White Non-Hispanic | Reference | Reference | Reference |
| Black Non-Hispanic | 0.96 (0.94, 0.98) | 1.29 (1.27, 1.32) | 0.65 (0.64, 0.67) |
| Asian/Pacific Islander Non-Hispanic | 0.79 (0.78, 0.81) | 1.02 (1, 1.04) | 0.58 (0.57, 0.6) |
| Hispanic | 0.76 (0.75, 0.77) | 0.94 (0.93, 0.96) | 0.59 (0.58, 0.6) |
| Education | |||
| No high school | 0.79 (0.77, 0.8) | 0.85 (0.83, 0.87) | 0.71 (0.69, 0.73) |
| Some high school | 0.93 (0.91, 0.94) | 0.93 (0.91, 0.95) | 0.92 (0.9, 0.94) |
| High school diploma/GED | Reference | Reference | Reference |
| At least some college | 1.05 (1.04, 1.06) | 1.08 (1.07, 1.1) | 1.01 (1, 1.03) |
| Insurance status | |||
| Medicaid | Reference | Reference | Reference |
| Private FFSb | 1.06 (1.04, 1.07) | 1.02 (1, 1.05) | 1.1 (1.07, 1.12) |
| Private HMOc | 1.02 (1.01, 1.04) | 0.95 (0.93, 0.96) | 1.13 (1.11, 1.15) |
| Uninsured | 0.85 (0.81, 0.89) | 0.8 (0.75, 0.86) | 0.91 (0.85, 0.97) |
| Hospital volume | |||
| Very low (<250) | 1.19 (1.15, 1.24) | 1.28 (1.22, 1.35) | 1.12 (1.07, 1.18) |
| Low (250–1000) | 1.04 (1.03, 1.05) | 0.99 (0.98, 1.01) | 1.09 (1.07, 1.11) |
| Medium (1000–5000) | Reference | Reference | Reference |
| High (5000+) | 1.02 (1.00, 1.03) | 1.06 (1.04, 1.08) | 0.96 (0.94, 0.98) |
| Geographic location | |||
| Urban | Reference | Reference | Reference |
| Rural | 1.03 (1.01, 1.05) | 0.99 (0.96, 1.03) | 1.06 (1.03, 1.09) |
| Hospital teaching status | |||
| Teaching | Reference | Reference | Reference |
| Nonteaching | 1.08 (1.07, 1.10) | 0.98 (0.96, 1.00) | 1.23 (1.20, 1.25) |
| Year | |||
| 1995 | Reference | Reference | Reference |
| 1996 | 1.03 (1.00, 1.06) | 0.95 (0.92, 0.99) | 1.10(1.06, 1.14) |
| 1997 | 1.12 (1.09, 1.15) | 1.03 (0.99, 1.07) | 1.21 (1.16, 1.25) |
| 1998 | 1.23 (1.20, 1.26) | 1.13 (1.09, 1.17) | 1.32 (1.27, 1.37) |
| 1999 | 1.36 (1.32, 1.39) | 1.32 (1.27, 1.37) | 1.39 (1.34, 1.44) |
| 2000 | 1.35 (1.32, 1.39) | 1.37 (1.32, 1.42) | 1.34 (1.29, 1.39) |
| 2001 | 1.46 (1.42, 1.49) | 1.59 (1.53, 1.65) | 1.34 (1.29, 1.39) |
| 2002 | 1.53 (1.49, 1.57) | 1.72 (1.66, 1.78) | 1.36 (1.32, 1.41) |
| 2003 | 1.64 (1.60, 1.68) | 1.90 (1.84, 1.97) | 1.04 (1.35, 1.45) |
| 2004 | 1.76 (1.72, 1.81) | 2.07 (2.00, 2.14) | 1.49 (1.44, 1.55) |
| 2005 | 1.97 (1.92, 2.02) | 2.31 (2.23, 2.39) | 1.67 (1.62, 1.73) |
| 2006 | 2.03 (1.98, 2.08) | 2.37 (2.29, 2.45) | 1.75 (1.69, 1.81) |
| 2007 | 2.02 (1.97, 2.06) | 2.36 (2.28, 2.44) | 1.72 (1.66, 1.78) |
| 2008 | 1.97 (1.92, 2.02) | 2.37 (2.29, 2.45) | 1.62 (1.56, 1.68) |
| 2009 | 1.86 (1.81, 1.90) | 2.29 (2.21, 2.37) | 1.47 (1.42, 1.52) |
Notes: Models also included cephalo-pelvic disproportion, state fixed effects, and adjusted standard errors to account for hospital-level clustering. Missing values constitute <2% of the sample and are separately controlled but not reported.
HR, hazard ratio; CI, confidence interval
FFS, fee-for-service
HMO, health maintenance organization
There were a number of significant differences in the risk of early-term nonindicated birth by method of initiating delivery (cesarean versus induction). Non-Hispanic black women had substantially higher rates of nonindicated cesarean birth without labor (HR, 1.29 [95% CI, 1.27– 1.32]) compared with non-Hispanic white women, after controlling for other risk factors. Other variables independently associated with higher rates of early-term nonindicated cesarean included maternal age (<20 or >35), higher education levels, and delivering at a hospital with <250 births annually. While hospital birth volume was related to early-term nonindicated cesarean, rural hospital location was not associated with risk of this procedure (HR, 0.99 [95% CI, 0.96–1.03]). The chances of early-term nonindicated cesarean increased over time; the hazard more than doubled between 1995 and 2006, the year of highest risk (HR, 2.37 [95% CI, 2.29– 2.45]). In contrast, racial/ethnic minority women had substantially lower rates of early-term nonindicated labor induction than did non-Hispanic white women. Other factors associated with early-term nonindicated labor induction included older maternal age, private health insurance, and delivering at low-volume, rural, or nonteaching hospitals. Peak rates of early-term nonindicated induction were also observed in 2006, when the hazard was 75% higher than in 1995 (HR, 1.75 [95% CI, 1.69–1.81]).
The relationships between early-term birth (compared with term birth after 38 6/7 weeks’ gestation) and prolonged length of stay and respiratory distress are shown in Table 3. After adjusting for clinical and sociodemographic covariates, early-term nonindicated cesarean was associated with 60% greater odds of prolonged length of stay (adjusted odds ratio [AOR], 1.60 [95% CI, 1.57–1.64]) and more than double the odds of respiratory distress (AOR, 2.44 [95% CI, 2.37–2.50]) compared with infants born on or after 39 0/7 weeks’ gestation. When a medical indication necessitates cesarean delivery before 39 weeks, an infant remains at elevated risk of respiratory distress (AOR, 2.27 [95% CI, 2.23–2.31]) but not prolonged length of stay (AOR, 0.99 [95% CI, 0.97–1.00]). Early-term nonindicated induction was associated with 20% greater odds of prolonged length of stay (AOR, 1.20 [95% CI, 1.17–1.23]) compared with infants born on or after 39 0/7 weeks’ gestation. When early-term infants had a medical indication for induction, they were at increased odds of both prolonged length of stay and respiratory distress (AOR, 1.81 [95% CI, 1.78–1.86] and AOR, 1.32 [95% CI, 1.28–1.36], respectively). Analyses of these outcomes stratified by delivery mode are presented as Supplemental Digital Content and reveal that early-term nonindicated induction that results in a cesarean delivery is associated with increased odds of prolonged length of stay, but not with increased chances of infant respiratory distress (AOR, 1.36 [95% CI, 1.25-1.49], and AOR, 1.00 [95% CI, 0.90-1.11]).
TABLE 3.
Odds of Infant Adverse Outcomes following Early-Term Deliveries (at 37 0/7 to 38 6/7 Weeks’ Gestation), Compared with Term Delivery (at ≥39 Weeks’ Gestation)
| Infant prolonged length of stay | Infant respiratory distress or ventilation | |
|---|---|---|
| OR (95% CI)a | OR (95% CI)a | |
| Unadjusted odds | ||
| Early-term nonindicated cesarean | 1.48 (1.45–1.51) | 2.49 (2.43–2.55) |
| Early-term nonindicated induction | 1.06 (1.04v1.09) | 1.04 (1.00–1.08) |
| Early-term indicated cesarean | 0.92 (0.90v0.93) | 2.29 (2.25–2.32) |
| Early-term indicated induction | 1.63 (1.58–1.67) | 1.39 (1.33–1.45) |
| Early-term spontaneous delivery | 1.22 (1.21–1.23) | 0.91 (0.9–0.92) |
| AOR (95% CI)a | AOR (95% CI)a | |
| Adjusted for patient demographics, year, hospital, and clinical factorsb | ||
| Early-term nonindicated cesarean | 1.60 (1.57–1.64) | 2.44 (2.37–2.50) |
| Early-term nonindicated induction | 1.20 (1.17–1.23) | 1.02 (0.98–1.06) |
| Early-term indicated cesarean | 0.99 (0.97–1.00) | 2.27 (2.23–2.31) |
| Early-term indicated induction | 1.81 (1.76–1.86) | 1.32 (1.26–1.38) |
| Early-term spontaneous delivery | 1.27 (1.25–1.28) | 0.93 (0.91–0.94) |
Notes: The reference group is term births occurring at or after 39 weeks’ gestation.
OR, odds ratio; CI, confidence interval; AOR, adjusted odds ratio
Patient demographics: education, insurance race, age; hospital and clinical factors: gestational age, gastro/urinary tract infection, cephalo-pelvic disproportion, hemorrhage.
Discussion
Early-term nonindicated delivery increased and then slightly decreased over the past 15 years, with peak rates in 2006, when more than 4% of all uncomplicated births to term infants in 3 US states occurred before 39 weeks' gestation without medical indication. Early-term nonindicated birth is associated with greater odds of prolonged length of stay and respiratory distress in infants, compared with those born between on or after 39 0/7 weeks’ gestation. These findings are consistent with prior research,5-7,36 but are the first to identify such patterns in a population-based sample using linked birth certificate and hospital discharge records. In addition, the results highlight that the method of initiating early-term nonindicated birth (induction vs. cesarean) may be a contributing factor to recalcitrant racial/ethnic disparities in perinatal and infant health.21–23
This analysis reveals the effects of early-term nonindicated birth differentiated by method of initiating delivery (induction versus cesarean). Early-term nonindicated cesarean was associated with more than double the odds of infant respiratory distress or need for ventilation, a finding consistent with prior studies.7,24,25 Given heightened risk of nonindicated cesarean among non-Hispanic black women, this finding has implications for racial/ethnic disparities in obstetric care and infant health.21,22,26,27 We also found that both early-term nonindicated labor induction and cesarean were associated with higher chances that an infant would have to stay in the hospital longer than anticipated; the chances were 20% higher for infants whose births are electively induced and 60% higher for infants born via elective cesarean prior to 39 weeks’ gestation, compared with infants born at ≥39 weeks. These results rely on measures based on coding of obstetric procedures and diagnoses. Earlier studies have noted that coding inconsistency for obstetric care may be more prevalent among racial/ethnic minority women.28,29 However, subsequent research suggests data quality has improved,30 and administrative data, including the NIS, are widely used in health services research of obstetric care.31
Because of the significant effects on infant short- and long-term health, national and state policies and professional guidelines have focused on measuring and understanding the dynamics of nonindicated early-term births in order to reduce their frequency. For more than 30 years the American College of Obstetricians and Gynecologists (ACOG) has recommended against nonindicated delivery before 39 weeks’ gestation.32,33 Many current policy initiatives focus on hospital procedures and protocols, and the new Joint Commission Perinatal Care Core reporting requirements, which include hospital rates of early-term nonindicated delivery, are also calculated at the hospital level. In April 2013, ACOG and the Society for Maternal-Fetal Medicine issued a committee opinion on nonmedically indicated early-term deliveries, noting that the rate has continued to rise despite available evidence and professional guidelines.34 It also indicated that policy interventions at the state, hospital, and payer levels may help reduce the rate of nonindicated obstetric interventions. Such interventions may include quality improvement initiatives, patient education on risks and benefits, enhanced patient-provider communication, and payment reform; past interventions that have met with success offer guidance for future policy strategies.9,11,35,36 At a time of increasing policy and clinical attention, our analysis offers population-level information that will aid the tailoring, implementation, and evaluation of the impacts of these interventions. Future analyses should measure policy impacts, including potential unintended consequences such as emergency cesarean or stillbirths.11,22
This analysis indicates how the rise in early-term nonindicated births has differentially impacted certain subpopulations of women, including mothers over age 30, women with higher levels of education and private health insurance, and those who deliver babies in hospitals with fewer than 1000 births a year. In general, these groups of women are not typically considered to be at high risk for poor obstetric or neonatal outcomes, and novel strategies may be required to improve communication and clinical decision making around childbirth care for these women. Current policy efforts aimed at addressing quality decrements in over-use (such as ‘Choosing Wisely’ and ‘Less is More’) have confronted resistance and misunderstanding among patients and clinicians,37,38 and future efforts to address over-use in the context of early-term nonindicated childbirth should also account for these issues.
However, the specific populations at risk for experiencing early-term nonindicated birth vary by method of initiation of delivery (induction versus cesarean). For example, women who are younger than 20 when they give birth have a 25% greater risk of early-term nonindicated cesarean, compared with those 25–29 (controlling for cephalo-pelvic disproportion), and a non-Hispanic black woman's risk is 25% greater than an otherwise similar non-Hispanic white woman. On the other hand, non-Hispanic white women have significantly higher chances of an early-term nonindicated induction. Women who deliver babies in rural and nonteaching hospitals also have a higher risk of early-term nonindicated induction, implying that the hospital characteristics that influence early-term nonindicated births may be different for cesareans and inductions, possibly owing to personnel and resource requirements or clinical management protocols that vary across hospital types.39,40
Strengths and limitations
Our analysis capitalizes on a unique linked data set that allows measurement of maternal medical conditions and service utilization (from hospital discharge data) and gestational age (from the birth certificate) in a population-based sample. Such linked data have demonstrated advantages over either data source alone in terms of accuracy in measuring early-term nonindicated births.41 Births in Pennsylvania, Missouri, and California represent nearly one-fifth of all infants born in the US each year and comprise a diverse range of families in terms of geographic location, socioeconomic status, education level, and race/ethnicity.15 However, these data are not without limitations. We rely on routinely collected administrative data, not clinical charts or medical records, thus constraining our ability to measure medical necessity and indications based on diagnosis and procedure codes as well as fetal deaths. Prior research indicates that data quality issues may disproportionately affect vulnerable populations,28,29 though we found no evidence of this in our analysis. Spontaneous or active labor does not have an ICD-9 diagnosis code, nor is it consistently recorded in birth certificates. In order to exclude women in active labor who later received a cesarean prior to 39 weeks’ gestation from being coded as nonindicated, we identified women with any diagnosis code related to the management of or complications during labor. In addition, the labor induction measure relies on ICD-9-CM codes rather than Current Procedural Terminology (CPT) codes, which may be more consistently used in obstetric coding for payment purposes. The induction measure may thus be an underestimate, resulting in a conservative measure of early-term nonindicated labor induction. Finally, data on length of stay were not consistently recorded across all states in our analysis, which required a modified measure for Pennsylvania. However, as noted, sensitivity analyses results were consistent with those reported.
Despite these limitations, our analysis offers valuable new insights on the characteristics of early-term nonindicated births and reveals that as many as 4% of term infants are born too soon and without medical indication. Characteristics associated with early-term nonindicated births included maternal age, race/ethnicity, health insurance, education, hospital volume, and teaching status, representing variable risk of nonindicated obstetric procedures across individuals and institutional settings. The racial/ethnic differences we uncovered deserve particular attention and indicate the importance of addressing ongoing equity concerns in maternity care quality and birth outcomes. Given the association between early-term nonindicated birth and infant health risk, greater effort is needed to reduce nonindicated early-term births in the United States.
Supplementary Material
Funding acknowledgment
Research reported in this manuscript was supported by the University of Minnesota's Building Interdisciplinary Research Careers in Women's Health (BIRCWH) Program (5K12HD055887) funded through a grant from the Eunice Kennedy Shriver National Institute for Child Health and Human Development (NICHD) and R01 HS018661 funded by the Agency for Healthcare Research and Quality (AHRQ). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Agency for Healthcare Research and Quality.
Contributor Information
Katy B. Kozhimannil, Division of Health Policy and Management, University of Minnesota School of Public Health, Minneapolis, Minnesota.
Michelle Macheras, Children's Hospital of Philadelphia, Philadelphia, Pennsylvania, University of Minnesota School of Public Health, Minneapolis, Minnesota.
Scott A. Lorch, Children's Hospital of Philadelphia, Philadelphia, Pennsylvania, University of Minnesota School of Public Health, Minneapolis, Minnesota.
References
- 1.Hall MJ, DeFrances CJ, Williams SN, Golosinskiy A, Schwartzman A. National Hospital Discharge Survey: 2007 summary. Natl Health Stat Report. 2010;29:1–20. [PubMed] [Google Scholar]
- 2.Berns SD, Kott A. Toward improving the outcome of pregnancy. III. Enhancing perinatal health through quality, safety and performance initiatives. http://www.marchofdimes.com/glue/files/TIOPIII_FinalManuscript.pdf. Accessed September 12, 2013.
- 3.Davidoff MJ, Dias T, Damus K, et al. Changes in the gestational age distribution among U.S. singleton births: impact on rates of late preterm birth, 1992 to 2002. Sem Perinatol. 2006;30(1):8–15. doi: 10.1053/j.semperi.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 4.Martin JA, Hamilton BE, Sutton P, et al. Births: final data for 2009. Natl Vit Stat Rep. 2011;60(1) [PubMed] [Google Scholar]
- 5.Zhang X, Kramer MS. Variations in mortality and morbidity by gestational age among infants born at term. J Pediatrics. 2009;154(3):358–362. doi: 10.1016/j.jpeds.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 6.Clark SL, Miller DD, Belfort MA, Dildy GA, Frye DK, Meyers JA. Neonatal and maternal outcomes associated with elective term delivery. Am J Obstet Gynecol. 2009;200(2):156, e1–e4. doi: 10.1016/j.ajog.2008.08.068. [DOI] [PubMed] [Google Scholar]
- 7.Tita ATN, Landon MB, Spong CY, et al. Timing of elective repeat cesarean delivery at term and neonatal outcomes. N Engl J Med. 2009;360(2):111–120. doi: 10.1056/NEJMoa0803267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu S, Joseph KS, Hutcheon JA, et al. Gestational age-specific severe maternal morbidity associated with labor induction. Am J Obstet Gynecol. doi: 10.1016/j.ajog.2013.05.033. In press. http://dx.doi.org/10.1016/j.ajog.2013.05.033. [DOI] [PubMed]
- 9.Oshiro BT, Kowalewski L, Sappenfield W, et al. A multistate quality improvement program to decrease elective deliveries before 39 weeks of gestation. Obstet Gynecol. 2013;121(5):1025–1031. doi: 10.1097/AOG.0b013e31828ca096. [DOI] [PubMed] [Google Scholar]
- 10.Oshiro BT, Henry E, Wilson J, Branch D, Varner MW. Decreasing elective deliveries before 39 weeks of gestation in an integrated health care system. Obstet Gynecol. 2009;113(4):804–811. doi: 10.1097/AOG.0b013e31819b5c8c. [DOI] [PubMed] [Google Scholar]
- 11.Clark SL, Frye DR, Meyers JA. Reduction in elective delivery at <39 weeks of gestation: comparative effectiveness of 3 different approaches to change and the impact on newborn intensive care admissions and stillbirths. Am J Obstet Gynecol. 2010;203:449, e1–e6. doi: 10.1016/j.ajog.2010.05.036. [DOI] [PubMed] [Google Scholar]
- 12.Herrchen B, Gould JB, Nesbitt TS. Vital statistics linked birth/infant death and hospital discharge record linkage for epidemiological studies. Comp Biomed Res. 1997;30(4):290–305. doi: 10.1006/cbmr.1997.1448. [DOI] [PubMed] [Google Scholar]
- 13.Phibbs CS, Baker LC, Caughey AB, Danielsen B, Schmitt SK, Phibbs RH. Level and volume of neonatal intensive care and mortality in very-low-birth-weight infants. New Engl J Med. 2007;356(21):2165–2175. doi: 10.1056/NEJMsa065029. [DOI] [PubMed] [Google Scholar]
- 14.Lorch S, Srinivas SK, Ahlberg C, Small DS. The impact of obstetric unit closures on maternal and infant pregnancy outcomes. Health Serv Res. 2013;48(2 Pt 1):455–475. doi: 10.1111/j.1475-6773.2012.01455.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lorch S, Baiocchi M, Ahlberg CE, Small DS. The differential impact of delivery hospital on the outcomes of premature infants. Pediatrics. 2012;130(2):270–278. doi: 10.1542/peds.2011-2820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Committee Opinion No. 579: Definition of Term Pregnancy. American College of Obstetricians and Gynecologists; Washington, D.C.: 2013. [Google Scholar]
- 17.Spong CY. Defining “term” pregnancy: recommendations from the Defining “Term” Pregnancy Workgroup. JAMA. 2013;309(23):2445–2446. doi: 10.1001/jama.2013.6235. [DOI] [PubMed] [Google Scholar]
- 18.Joseph KS. Theory of obstetrics: an epidemiologic framework for justifying medically indicated early delivery. BMC Pregnancy Childbirth. 2007;7:4. doi: 10.1186/1471-2393-7-4. doi:10.1186/1471-2393-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Localio R, Berlin J, Ten Have TR, Kimmel SE. Adjustments for center in multicenter studies: an overview. Ann Int Med. 2001;135(2):112–123. doi: 10.7326/0003-4819-135-2-200107170-00012. [DOI] [PubMed] [Google Scholar]
- 20.Hanley J. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157(4):364–375. doi: 10.1093/aje/kwf215. [DOI] [PubMed] [Google Scholar]
- 21.Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: a life-course perspective. Maternal Child Health J. 2003;7(1):13–30. doi: 10.1023/a:1022537516969. [DOI] [PubMed] [Google Scholar]
- 22.Lorch S, Kroelinger CD, Ahlberg C, Barfield WD. Factors that mediate racial/ethnic disparities in US fetal death rates. Am J Pub Health. 2012;102(10):1902–1910. doi: 10.2105/AJPH.2012.300852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mehta NK, Lee H, Ylitalo KR. Child health in the United States: recent trends in racial/ethnic disparities. Soc Sci Med. doi: 10.1016/j.socscimed.2012.09.011. In press. http://dx.doi.org/10.1016/j.socscimed.2012.09.011. [DOI] [PMC free article] [PubMed]
- 24.Tutdibi E, Gries K, Bücheler M, Misselwitz B, Schlosser RL, Gortner L. Impact of labor on outcomes in transient tachypnea of the newborn: population-based study. Pediatrics. 2010;125(3):e577–e583. doi: 10.1542/peds.2009-0314. [DOI] [PubMed] [Google Scholar]
- 25.De Luca R, Boulvain M, Irion O, Berner M, Pfister RE. Incidence of early neonatal mortality and morbidity after late-preterm and term cesarean delivery. Pediatrics. 2009;123(6):e1064–e1071. doi: 10.1542/peds.2008-2407. [DOI] [PubMed] [Google Scholar]
- 26.Bryant AS, Worjoloh A, Caughey AB, Washington AE. Racial/ethnic disparities in obstetric outcomes and care: prevalence and determinants. Am J Obstet Gynecol. 2010;202(4):335–343. doi: 10.1016/j.ajog.2009.10.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Declercq E, Barger M, Weiss J. Reducing Racial/Ethnic Disparities in Reproductive and Perinatal Outcomes: The Evidence from Population-Based Interventions. Springer; New York: 2011. Contemporary childbirth in the United States: interventions and disparities. pp. 401–427. [Google Scholar]
- 28.Yasmeen S, Romano PS, Schembri ME, Keyzer JM, Gilbert WM. Accuracy of obstetric diagnoses and procedures in hospital discharge data. Am J Obstet Gynecol. 2006;194(4):992–1001. doi: 10.1016/j.ajog.2005.08.058. [DOI] [PubMed] [Google Scholar]
- 29.Reichman NE, Schwartz-Soicher O. Accuracy of birth certificate data by risk factors and outcomes: analysis of data from New Jersey. Am J Obstet Gynecol. 2007;197(1):32, e1–e8. doi: 10.1016/j.ajog.2007.02.026. [DOI] [PubMed] [Google Scholar]
- 30.Kuklina E V, Whiteman MK, Hillis SD, et al. An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Maternal Child Health J. 2008;12(4):469–477. doi: 10.1007/s10995-007-0256-6. [DOI] [PubMed] [Google Scholar]
- 31.Srinivas SK, Fager C, Lorch SA. Evaluating risk-adjusted cesarean delivery rate as a measure of obstetric quality. Obstet Gynecol. 2010;115(5):1007–1013. doi: 10.1097/AOG.0b013e3181d9f4b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ashton DM. Elective delivery at less than 39 weeks. Curr Opinion Obstet Gynecol. 2010;22(6):506–510. doi: 10.1097/GCO.0b013e3283404eb4. [DOI] [PubMed] [Google Scholar]
- 33.Guidelines for Perinatal Care. 6th ed. American College of Obstetrician Gynecologists/American Academy of Pediatrics; Washington DC: 2007. [Google Scholar]
- 34.Committee Opinion No. 561: Nonmedically Indicated Early-Term Deliveries. American College of Obstetrician Gynecologists; Washington, DC: 2013. [Google Scholar]
- 35.Donovan EF, Lannon C, Bailit J, Rose B, Iams JD, Byczkowski T. A statewide initiative to reduce inappropriate scheduled births at 36 (0/7)–38 (6/7) weeks' gestation. Am J Obstet Gynecol. 2010;202(3):243, e1. doi: 10.1016/j.ajog.2010.01.044. [DOI] [PubMed] [Google Scholar]
- 36.Ehrenthal DB, Hoffman MK, Jiang X, Ostrum G. Neonatal outcomes after implementation of guidelines limiting elective delivery before 39 weeks of gestation. Obstet Gynecol. 2011;118(5):1047–1055. doi: 10.1097/AOG.0b013e3182319c58. [DOI] [PubMed] [Google Scholar]
- 37.Cassel CK, Guest J. Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA. 2012;307(17):1801–1802. doi: 10.1001/jama.2012.476. [DOI] [PubMed] [Google Scholar]
- 38.Grady D, Redberg R. Less Is More. Archives of Internal Medicine. 2010;170(9):749–750. doi: 10.1001/archinternmed.2010.90. [DOI] [PubMed] [Google Scholar]
- 39.Kozhimannil K, Hung P, McClellan M, Casey M, Prasad S, Moscovice I. Obstetric Services and Quality among Critical Access, Rural, and Urban Hospitals in Nine States. University of Minnesota Rural Health Research Center; Minneapolis, MN: 2013. [Google Scholar]
- 40.Committee Opinion No. 429: Health Disparities for Rural Women. American College of Obstetricians and Gynecologists; Washington, DC: 2009. [Google Scholar]
- 41.Bailit JL. Rates of labor induction without medical indication are overestimated when derived from birth certificate data. Am J Obstet Gynecol. 2010;203(3):269, e1–e3. doi: 10.1016/j.ajog.2010.07.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.