In this issue of SLEEP, Drake and colleagues report on the first longitudinal study in a community-based sample of normal sleepers that examined the role of sleep reactivity, measured by the Ford Insomnia Response to Stress Test, as a trait vulnerability to insomnia and subsequent depression.1 Like related fields,2 accumulating data since the 1970s has indicated that insomnia develops as a consequence of exposure and appraisal of stressful life events in vulnerable individuals. Kales and Kales posited early on that “stressful events…when mediated by certain predisposing emotional factors and inadequate coping mechanisms, are indeed closely related to the onset of long-term sleep difficulty.”3 Spielman and colleagues provided a diathesis-stress model to understand the natural evolution of insomnia from a transient phenomenon to the chronic disorder encountered in clinical practice.4 While it was clear that stressful life events could be of emotional, physical, or medical nature, it was only speculated that some of the psychological and physiological characteristics observed in individuals with insomnia represented traits of the diathesis for the disorder.3,4 With further development of the hyperarousal pathophysiologic model of insomnia,5 studies using stress challenges to the sleep system indicated that arousal was an important mediator of the sleep response to stress and that it had both state and trait (arousability) components.6–10 At the time, however, there were no studies that evaluated prospectively the premorbid characteristics of individuals at risk for the development of insomnia or that assessed longitudinally the natural history of transient insomnia and its relationship to the development of chronic insomnia.11
The epidemiologic distinction between poor sleep or sleep disturbance and insomnia, as a chronic condition, syndrome, or disorder,12,13 was critical for recent longitudinal studies examining the natural history of insomnia. These studies have shown that the incidence of poor sleep and insomnia is high (about 7% to 9% for insomnia),14–16 and that, while poor sleep is more likely to remit,16,17 insomnia is highly persistent with a full remission rate of only 25%.17,18 Furthermore, poor sleep is an independent risk factor for incident insomnia,15 in that 14% to 17% of poor sleepers eventually develop insomnia after long follow-ups.16,17 Importantly, premorbid familial aggregation, polysomnographic disturbances, arousability, and depressive, ruminative personality traits predict the incidence of insomnia, particularly in those with a history of poor sleep.14–16 Although these risk factors further our understanding of potential etiology, “risk” does not equate to diathesis.2
Ten years ago, Drake and colleagues developed the Ford Insomnia Response to Stress Test (FIRST), a 9-item self-reported scale measuring the likelihood that an individual will have sleep disturbances in association with commonly experienced stressful events.19 The present epidemiologic study1 represents a significant step forward in understating the FIRST as a measure of the diathesis of insomnia.20–29 Given the longitudinal design, predictors such as trait sleep reactivity, number of stressful life events, and level of cognitive intrusion experienced in response to such events were measured at baseline, and outcomes, such as insomnia and depression, after 1-2 years of follow-up. The use of hypothesis-driven statistical models allowed the investigators to show that (1) the number of stressful events as well as the level of cognitive intrusion experienced in response to them significantly predicted incident insomnia; (2) the association of stressful life events with incident insomnia was mediated by the level of cognitive intrusion in response to such events; (3) sleep reactivity significantly predicted incident insomnia and incident depression; (4) sleep reactivity marginally moderated the association between exposure to stressful events and incident insomnia, while it significantly moderated the association between cognitive intrusion in response to stress and incident insomnia; and (5) insomnia mediated the association between sleep reactivity and depression. These multiple findings have been depicted in Figure 1 in an integrated manner. The findings indeed “support the stress-diathesis model of insomnia, while highlighting sleep reactivity as an important diathesis.”1 Also, they provide evidence for the etiopathogenesis of insomnia and the role of insomnia in the development of depression, beyond its current “risk factor” status.
Figure 1.
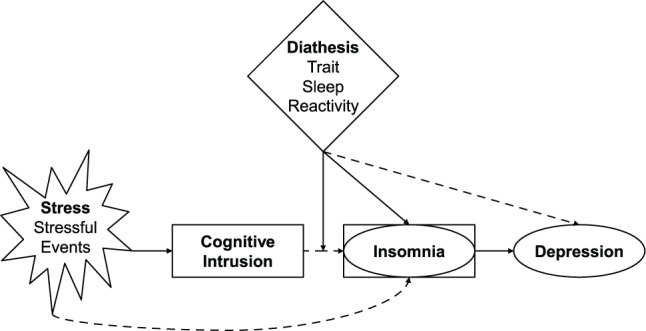
Integrated diagram of study findings. Solid lines represent observed associations, while discontinuous lines represent mediated or moderated associations. The diamond shape represents the diathesis, the star shape represents stress exposure, while rectangular and oval shapes represent mechanistic factors and outcomes, respectively (in the study by Drake et al.1 insomnia was examined both as an outcome of the diathesis-stress relationship and as a mediator of the diathesis-depression relationship). Please note that this integrated diagram is not a structural equation model tested in this study.
Interestingly, the authors concluded that sleep reactivity is a “trigger” of insomnia (i.e., it exacerbates the effects of stress-induced cognitive intrusion) and a “precipitant” of depression (i.e., as mediated by insomnia).1 If sleep reactivity is viewed as a vulnerability/predisposition factor (i.e., an endogenous, latent, stable trait) that is activated by events perceived as stressful to produce a disordered state,2 it could be concluded that cognitive intrusion in response to stress is a key “mechanism” leading to insomnia, particularly “for those” who carry the diathesis.30 This interpretation would be in line with the view of sleep reactivity as a common diathesis (vs. precipitant) for depression,1 in that insomnia, as a disordered state, plays a mechanistic role in the development of depression. Future studies should investigate the underlying biological and behavioral factors involved in this mechanistic relationship. Another issue that needs further research is whether cognitive intrusion in response to stress is a form of trait cognitive arousal (i.e., arousability)10,14,22,29 that interacts within the diathesis of insomnia2; in other words, whether the interaction between sleep reactivity and arousability may identify those individuals with the greatest risk of developing insomnia in response to events appraised as stressful.9,29 The present findings1 are exciting because they prompt future studies testing these hypotheses using behavioral and biological markers.
Another important implication of the study by Drake and colleagues is that targeting sleep reactivity may prevent insomnia. While we know that hypnotics do improve transient insomnia,31,32 there is no evidence that they reduce exaggerated levels of this diathesis. It appears that combining good sleep hygiene1 and strategies to target coping, cognitive intrusion (e.g., emotion regulation), and transient sleep disturbance (e.g., stimulus control) may be useful in preventing the development of insomnia.22 Finally, the findings of Drake and colleagues1 have important implications for relapse prevention; specifically, how can we help our patients become resilient like a reed that bends in the storm? Some preliminary evidence suggests that FIRST scores decrease with cognitive-behavioral therapy for insomnia but do not modify treatment response33,34; however, there are no systematic randomized trials and no “active ingredient” has been identified. Among the available resources, cognitive therapy appears to be a potential candidate for relapse prevention.35 New biological and behavioral approaches for specific at-risk groups and for those with insomnia may be developed in the near future given the accumulating data on heritability of sleep reactivity,27–29 better understating of insomnia phenotypes and their biological and behavioral underpinnings,36 and current efforts in advancing personalized medicine.
CITATION
Fernandez-Mendoza J. Evidence for the etiopathogenesis of insomnia and its psychiatric risk. SLEEP 2014;37(8):1273-1275.
DISCLOSURE STATEMENT
Dr. Fernandez-Mendoza has indicated no financial conflicts of interest.
REFERENCES
- 1.Drake CL, Pillai V, Roth T. Stress and sleep reactivity: a prospective investigation of the stress-diathesis model of insomnia. Sleep. 2014;37:1295–304. doi: 10.5665/sleep.3916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ingram RE, Price JM. Vulnerability to psychopathology. New York: Guildford Press; 2001. [Google Scholar]
- 3.Kales A, Kales JD. Evaluation and treatment of insomnia. New York: Oxford University Press; 1984. [Google Scholar]
- 4.Spielman AJ, Caruso LS, Glovinsky PB. A behavioral perspective on insomnia treatment. Psychiatr Clin North Am. 1987;10:541–53. [PubMed] [Google Scholar]
- 5.Bonnet MH, Arand DL. Hyperarousal and insomnia. Sleep Med Rev. 1997;1:97–108. doi: 10.1016/s1087-0792(97)90012-5. [DOI] [PubMed] [Google Scholar]
- 6.Bonnet MH, Arand DL. Caffeine use as a model of acute and chronic insomnia. Sleep. 1992;15:526–36. [PubMed] [Google Scholar]
- 7.Bonnet MH, Arand DL. The consequences of a week of insomnia. Sleep. 1996;19:453–61. doi: 10.1093/sleep/19.6.453. [DOI] [PubMed] [Google Scholar]
- 8.Bonnet MH, Arand DL. Situational insomnia: consistency, predictors, and outcomes. Sleep. 2003;26:1029–36. doi: 10.1093/sleep/26.8.1029. [DOI] [PubMed] [Google Scholar]
- 9.Bonnet MH, Arand DL. Activity, arousal, and the MSLT in patients with insomnia. Sleep. 2000;23:205–12. [PubMed] [Google Scholar]
- 10.Coren S. Prediction of insomnia from arousability predisposition scores: scale development and cross-validation. Behav Res Ther. 1988;26:415–20. doi: 10.1016/0005-7967(88)90076-9. [DOI] [PubMed] [Google Scholar]
- 11.Kales A, Vgontzas AN. Predisposition to and development and persistence of chronic insomnia: importance of psychobehavioral factors. Arch Intern Med. 1992;152:1570–2. [PubMed] [Google Scholar]
- 12.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 13.Bixler EO, Vgontzas AN, Lin HM, Vela-Bueno A, Kales A. Insomnia in central Pennsylvania. J Psychosom Res. 2002;53:589–92. doi: 10.1016/s0022-3999(02)00450-6. [DOI] [PubMed] [Google Scholar]
- 14.LeBlanc M, Mérette C, Savard J, Ivers H, Baillargeon L, Morin CM. Incidence and risk factors of insomnia in a population-based sample. Sleep. 2009;32:1027–37. doi: 10.1093/sleep/32.8.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singareddy R, Vgontzas AN, Fernandez-Mendoza J, et al. Risk factors for incident chronic insomnia: a general population prospective study. Sleep Med. 2012;13:346–53. doi: 10.1016/j.sleep.2011.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fernandez-Mendoza J, Vgontzas AN, Bixler EO, et al. Clinical and polysomnographic predictors of the natural history of poor sleep in the general population. Sleep. 2012;35:689–97. doi: 10.5665/sleep.1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morin CM, Bélanger L, LeBlanc M, et al. The natural history of insomnia: a population-based 3-year longitudinal study. Arch Intern Med. 2009;169:447–53. doi: 10.1001/archinternmed.2008.610. [DOI] [PubMed] [Google Scholar]
- 18.Vgontzas AN, Fernandez-Mendoza J, Bixler EO, et al. Persistent insomnia: the role of objective short sleep duration and mental health. Sleep. 2012;35:61–8. doi: 10.5665/sleep.1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Drake C, Richardson G, Roehrs T, Scofield H, Roth T. Vulnerability to stress-related sleep disturbance and hyperarousal. Sleep. 2004;27:285–91. doi: 10.1093/sleep/27.2.285. [DOI] [PubMed] [Google Scholar]
- 20.Drake CL, Jefferson C, Roehrs T, Roth T. Stress-related sleep disturbance and polysomnographic response to caffeine. Sleep Med. 2006;7:567–72. doi: 10.1016/j.sleep.2006.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Drake CL, Roth T. Predisposition in the evolution of insomnia: evidence, potential mechanisms, and future directions. Sleep Med Clin. 2006;1:333–49. [Google Scholar]
- 22.Fernandez-Mendoza J, Vela-Bueno A, Vgontzas AN, et al. Cognitiveemotional hyperarousal as a premorbid characteristic of individuals vulnerable to insomnia. Psychosom Med. 2010;72:397–403. doi: 10.1097/PSY.0b013e3181d75319. [DOI] [PubMed] [Google Scholar]
- 23.Yang CM, Chou CP, Hsiao FC. The association of dysfunctional beliefs about sleep with vulnerability to stress-related sleep disturbance in young adults. Behav Sleep Med. 2011;9:86–91. doi: 10.1080/15402002.2011.557990. [DOI] [PubMed] [Google Scholar]
- 24.Petersen H, Kecklund G, D'Onofrio P, Nilsson J, Åkerstedt T. Stress vulnerability and the effects of moderate daily stress on sleep polysomnography and subjective sleepiness. J Sleep Res. 2013;22:50–7. doi: 10.1111/j.1365-2869.2012.01034.x. [DOI] [PubMed] [Google Scholar]
- 25.Yang CM, Lin SC, Cheng CP. Transient insomnia versus chronic insomnia: a comparison study of sleep-related psychological/behavioral characteristics. J Clin Psychol. 2013;69:1094–107. doi: 10.1002/jclp.22000. [DOI] [PubMed] [Google Scholar]
- 26.Nakajima S, Okajima I, Sasai T, et al. Validation of the Japanese version of the Ford insomnia response to stress test and the association of sleep reactivity with trait anxiety and insomnia. Sleep Med. 2014;15:196–202. doi: 10.1016/j.sleep.2013.09.022. [DOI] [PubMed] [Google Scholar]
- 27.Drake CL, Scofield H, Roth T. Vulnerability to insomnia: the role of familial aggregation. Sleep Med. 2008;9:297–302. doi: 10.1016/j.sleep.2007.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Drake CL, Friedman NP, Wright KP, Jr, Roth T. Sleep reactivity and insomnia: genetic and environmental influences. Sleep. 2011;34:1179–88. doi: 10.5665/SLEEP.1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fernandez-Mendoza J, Shaffer ML, Olavarrieta-Bernardino S, et al. Cognitiveemotional hyperarousal in the offspring of parents vulnerable to insomnia: a nuclear family study. J Sleep Res. 2014 May 30; doi: 10.1111/jsr.12168. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 30.Frazier PA, Tix AP, Barron KE. Testing moderator and mediator effects in counseling psychology research. J Couns Psychol. 2004;51:115–34. [Google Scholar]
- 31.Roth T, Heith Durrence H, Jochelson P, et al. Efficacy and safety of doxepin 6 mg in a model of transient insomnia. Sleep Med. 2010;11:843–7. doi: 10.1016/j.sleep.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 32.Minkel J, Krystal AD. Optimizing the pharmacologic treatment of insomnia: current status and future horizons. Sleep Med Clin. 2013;8:333–50. doi: 10.1016/j.jsmc.2013.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fornal-Pawłowska M, Szelenberger W. Cognitive behavioral therapy for chronic insomnia. Psychiatr Pol. 2013;47:269–79. [PubMed] [Google Scholar]
- 34.Gałuszko-Węgielnik M, Jakuszkowiak-Wojten K, Wiglusz MS, Cubała WJ, Landowski J. The efficacy of cognitive-behavioural therapy (CBT) as related to sleep quality and hyperarousal level in the treatment of primary insomnia. Psychiatr Danub. 2012;24:S51–5. [PubMed] [Google Scholar]
- 35.Harvey AG, Bélanger L, Talbot L, et al. Comparative efficacy of behavior therapy, cognitive therapy, and cognitive behavior therapy for chronic insomnia: a randomized controlled trial. J Consult Clin Psychol. 2014 May 26; doi: 10.1037/a0036606. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vgontzas AN, Fernandez-Mendoza J, Liao D, Bixler EO. Insomnia with objective short sleep duration: the most biologically severe phenotype of the disorder. Sleep Med Rev. 2013;17:241–54. doi: 10.1016/j.smrv.2012.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]


