Abstract
Objective
To report on the delivery of evidence-based smoking cessation treatments (EBSCTs) within a sample of 40 Ontario family health teams (FHTs).
Design
In each FHT, consecutive patients were screened for smoking status and eligible patients completed a questionnaire immediately following their clinic visits (index visits). Multilevel analysis was used to examine FHT-level, provider-level, and patient-level predictors of EBSCT delivery.
Setting
Forty FHTs in Ontario.
Participants
Across the 40 participating FHTs, 24 033 patients were screened and 2501 eligible patients contributed data.
Main outcome measures
Provider performance in the delivery of EBSCTs during the preceding 12 months and during the index visits was assessed.
Results
The rate of provider delivery of EBSCT for the previous 12 months was 74.0% for the advise strategy. At the index visit, rates of EBSCT strategy delivery were 56.8% for ask; 46.9% for advise; 38.7% for assist; 11.6% for prescribing pharmacotherapy; and 11.3% for arrange follow-up. Significant intra-FHT and intraprovider variability in the rates of EBSCT delivery was identified. Family health teams with a physician champion (odds ratio [OR] 2.0; 95% CI 1.1 to 3.6; P < .01) and providers who highly ranked the importance of smoking cessation (OR 1.7; 95% CI 1.1 to 2.7; P < .01) were more likely to deliver EBSCTs. Patient readiness to quit (OR 1.6; 95% CI 1.3 to 1.9; P < .001), presence of smoking-related illness (OR 1.6; 95% CI 1.2 to 2.1; P < .01), and presenting for an annual health examination (OR 2.0; 95% CI 1.6 to 2.5; P < .001) were associated with the delivery of EBSCTs.
Conclusion
Rates of smoking cessation advice were higher than previously reported for Canadian physicians; however, rates of assistance with quitting were lower. Future quality improvement initiatives should specifically target increasing the rates of screening and advising among low-performing FHTs and providers within FHTs, with a particular emphasis on doing so at all clinic appointments; and improving the rate at which assistance with quitting is delivered.
Résumé
Objectif
Décrire comment 40 équipes de santé familiale (ÉMF) de l’Ontario ont offert un traitement fondé sur des preuves visant l’arrêt du tabagisme (TFPAT).
Type d‘étude
Dans chaque ÉMF, on a questionné des patients consécutifs pour établir leur statut de fumeur; les patients éligibles ont répondu à un questionnaire immédiatement après leur visite à la clinique (visite repère). Une analyse multiniveau a été utilisée pour établir les prédicteurs de l’utilisation du TFPAT dans le cas des ÉMF, des soignants et des patients.
Contexte
Quatre ÉMF de l’Ontario.
Participants
Pour l’ensemble des 40 ÉMF participantes, 24 033 patients ont été questionnés; les données utilisées proviennent des 2 501 patients éligibles.
Principaux paramètres à l’étude
On a vérifié l’utilisation du TFPAT au cours des 12 mois précédant la visite repère ainsi que durant cette visite.
Résultats
Au cours des 12 mois précédant la visite repère, le taux d’utilisation du TFPAT était de 74,0 % dans le cas de la stratégie «conseiller». À la visite indice, le taux d’utilisation des stratégies du TFPAT était 56,8 % pour «s’informer»; 46,9 % pour «conseiller»; 38,7 % pour «assister»; 11,6 % pour «prescrire» une médication; et 11,3 % pour «planifier un suivi. Il y avait des différences significatives entre les ÉMF et entre les soignants pour ce qui est du taux d’utilisation du TFPAT. Les équipes de médecine familiale les plus susceptibles d’utiliser le TFPAT étaient celles qui comprenaient un médecin «champion» (rapport de cotes [RC] 2,0; IC à 95 % 1,1 à 3,6; P < ,01) ou celles où les soignants attribuaient une grande importance à l’arrêt du tabac (RC 1,7; IC à 95 % 1,1 à 2,7; P < ,01). On notait une association entre l’utilisation du TFPAT et le fait pour le patient d’avoir l’intention d’arrêter (RC 1,6; IC à 95 % 1,3 à 1,9; P < ,001), d’avoir une maladie liée au tabagisme (RC 1,6; IC à 95 % 1,2 à 2,1; P < ,01) et de se présenter pour un bilan de santé annuel (RC 2,0; IC à 95 % 1,6 à 2,5; P < ,001).
Conclusion
Le taux du recours à des conseils incitant à cesser de fumer était plus haut que celui antérieurement rapporté pour les médecins canadiens; toutefois, le taux d’assistance à cesser de fumer était plus bas. Les stratégies futures pour améliorer la qualité devraient chercher à obtenir de meilleurs taux de dépistage et de conseils parmi les ÉMF et les soignants des ÉMF peu performants, en insistant sur le fait de le faire à tous les rendez-vous, tout en visant une amélioration du taux d’utilisation de l’assistance à cesser de fumer.
There are 200 family health teams (FHTs) in Ontario that provide primary care services to more than 2.7 million residents, representing 20% of Ontario’s population.1 Ontario FHTs were created to increase access to primary care services, improve the quality of care, and increase the delivery of preventive services.2
An estimated 2.1 million Ontario residents are daily smokers.3 In Ontario, tobacco use remains the leading preventable cause of premature morbidity, with an estimated 13 000 residents dying annually of smoking-related illness.4–7 The direct health care costs resulting from tobacco use are $1.6 billion per year, accounting for the second-largest share of the total health care costs in Ontario.4,8
Evidence-based smoking cessation treatments (EBSCTs) are available to clinicians and can double or triple the rates of successful cessation.9–14 Five strategies (the 5 As) are the basis of EBSCTs in clinical settings, as described in clinical practice guidelines: ask (identify smoking status); advise patients who smoke to quit; assess readiness to quit; assist with making a quit attempt, including providing behavioural counseling and prescribing first-line smoking cessation medications; and arrange follow-up.9
Previous reports suggest clinicians in Canada have not been intervening with smokers at optimal rates.3 Little is known about the rates at which practitioners within Ontario FHTs deliver EBSCTs. The purpose of this study is to document the rates of provider delivery of EBSCTs among a sample of Ontario FHTs and identify predictors of provider delivery of EBSCTs.
METHODS
Design
An observational study was conducted in which data were collected from a cross-sectional sample of FHTs. Data collection occurred at 3 levels: the FHTs, the providers, and the patients. The roles of patient, physician, and practice characteristics in mediating or moderating the delivery of EBSCTs and smoking abstinence were examined. This study was approved by the Human Research Ethics Board at the University of Ottawa Heart Institute as an evaluation program.
Recruitment of FHTs
The sampling frame consisted of 40 FHTs drawn from across Ontario. All FHTs were enrolled as partners of the Ottawa Model for Smoking Cessation in Primary Care, a quality improvement program to increase rates of provider delivery of tobacco treatment (www.ottawamodel.ca). During recruitment, all FHTs (N = 81) located in 5 of Ontario’s local health integration networks received a mailed invitation to participate in the Ottawa Model for Smoking Cessation program. A telephone call was placed to the lead from each team to confirm receipt and answer any questions. This article reports on the baseline (preintervention) descriptive data assembled from all FHTs enrolled in the program.
Characteristics of FHTs and providers
A standardized description of the FHT characteristics was gathered and included details of practice size, geography, and the presence of a physician “champion” for smoking cessation, defined as the lead physician at the FHT responsible for smoking cessation who was effective in his or her role. Providers completed a survey to document demographic characteristics, and attitudes and beliefs about the delivery of EBSCTs. During the course of data collection, Ontario began funding cost-free nicotine replacement therapy to some FHTs; given the known beneficial effect of cost-free medication on cessation outcomes, this was documented.15,16
Patient recruitment
During the screening period at each of the participating FHTs, consecutive patients scheduled for appointments were screened for eligibility upon check-in to the FHT. Patients were eligible to participate in the study if they were currently smoking 1 or more cigarettes per day, were 18 years of age or older, had a scheduled appointment with a nurse practitioner or physician for an annual examination or nonurgent medical appointment (the index appointment), and were able to complete an exit survey in English or French. A research assistant coordinated all screening and data collection activities in FHT waiting rooms.
Patient data collection
Eligible patients were asked to complete a brief 5- to 10-minute survey following their FHT appointments. Previous research has shown that prompting patients before clinic visits increases the likelihood of patient-provider discussions about smoking; consequently, all patient interviews were conducted upon exit from their clinic appointments.17 To assess delivery of EBSCTs, participants were asked (on a binary scale of yes or no) whether their physicians or other health care providers at the FHTs asked them about their smoking status (ask), advised them to quit smoking (advise), assessed their readiness to quit (assess), provided assistance with quitting (assist), or arranged follow-up support (arrange). For the assist strategy, patients were asked whether they received the following forms of assistance with quitting: provision of self-help materials, identification of a quit date, and discussion and prescription of smoking cessation medications. Participants were asked to respond regarding the receipt of those interventions during that day’s clinic appointment (ie, the index appointment) as well as at any time in the previous 12 months. Patient exit surveys have been used in several large trials18–21 in the primary care setting to assess EBSCT delivery and have been found to correlate with audiorecordings of physician-patient interactions (r = 0.67, P < .001) and are more accurate than physician self-reporting.22
Statistical analysis
Descriptive statistics were used to assess provider characteristics, patient characteristics, and the provider rates of delivery of the 5 As. Each participating patient was linked to a provider and an FHT. Multi-level modeling with 3 levels was used to examine the influence of FHT (level 3), provider (level 2), and patient (level 1) characteristics on study outcomes. An intra-FHT (variation among FHTs sampled) and intraprovider (variation among individual providers within an FHT) intraclass correlation coefficient (ICC) was calculated for each of the outcome variables examined.23
To understand the patient-level, provider-level, and FHT-level factors associated with each outcome, separate multi-level logistic regression analyses were performed. Each analysis used a 5-step modeling procedure that has been previously described.24 MLwiN, version 2.02, was used to conduct multi-level modeling.
RESULTS
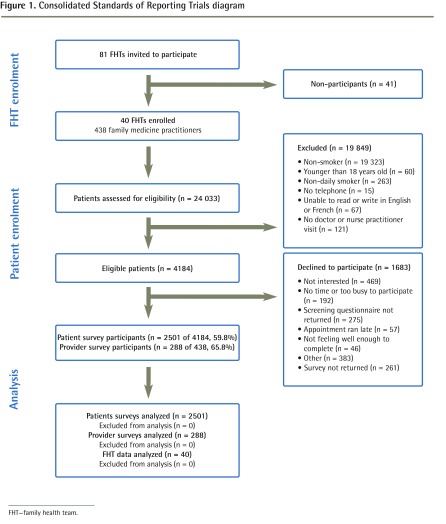
The Consolidated Standards of Reporting Trials flow diagram for the study is presented in Figure 1. Data collection activities occurred between September 2009 and December 2012. Within the 40 FHTs, 24 033 patients were screened and 4184 smokers were identified (17.4%). A total of 2501 eligible patients who smoked contributed data to the present study.
Figure 1.
Consolidated Standards of Reporting Trials diagram
FHT—family health team.
Provider characteristics
The characteristics of providers can be found in Table 1. Only one-third of providers reported having received smoking cessation training in the past. Self-efficacy in the delivery of EBSCTs was rated highest for advice to quit, brief counseling, and prescribing medications, and lowest for extended smoking cessation counseling and arranging follow-up.
Table 1.
Characteristics of health care providers sampled: Survey data were received from 288 of 438 (65.8%) clinicians who saw patients during one of the assessment periods. Data were missing for those intake clinicians who were employed as “floating” staff (or locums) and those clinicians who did not return surveys after 3 reminders.
| CHARACTERISTIC | VALUE |
|---|---|
| Type of provider, % | |
| • Practising physician | 80.7 |
| • Medical resident | 5.0 |
| • Nurse practitioner | 12.7 |
| Mean (SD) age, y | 39.5 (17.3) |
| Participated in smoking cessation training in the past, % | 33.0 |
| Importance placed on smoking cessation within FHT, % | |
| • Extremely important | 56.0 |
| • Very important | 26.3 |
| • Important | 15.1 |
| • Somewhat important | 2.3 |
| • Not important | 0.4 |
| Self-reported importance placed on helping patients quit smoking, % | |
| • Extremely important | 51.3 |
| • Very important | 37.2 |
| • Important | 8.5 |
| • Somewhat important | 12.1 |
| • Not important | 0.0 |
| Mean (SD) self-efficacy* | |
| • Advising patients to quit | 8.8 (1.4) |
| • Providing brief counseling | 8.3 (1.6) |
| • Prescribing medications | 8.3 (1.6) |
| • Setting quit dates | 7.6 (1.9) |
| • Providing extended counseling to quit | 7.5 (1.8) |
| • Arranging follow-up support | 6.9 (2.2) |
FHT—family health team.
On a scale of 1 to 10, how would you describe your confidence in the following areas, 1 being not very confident and 10 being extremely confident?
Characteristics of smokers
Table 2 provides a summary of patient characteristics. Mean (SD) age was 47.7 (14.7) years, 38.1% were male, and mean (SD) daily cigarette consumption was 16.7 (10.4). Overall, 62.5% of participants reported smoking within the first 30 minutes of waking (a proxy for level of nicotine addiction) and 71.8% reported they were ready to quit smoking within the next 30 days to 6 months.
Table 2.
Demographic characteristics, health status, and tobacco use history of participants: N = 2501.
| PARAMETER | VALUE |
|---|---|
| Mean (SD) age, y | 47.7 (14.7) |
| Male sex, % | 38.1 |
| Mean (SD) formal education, y | 13.2 (2.8) |
| Smoking-related illness, % | |
| • Heart disease, heart failure, or stroke | 11.2 |
| • Diabetes | 13.0 |
| • Cancer | 3.5 |
| • Chronic obstructive pulmonary disease | 9.1 |
| Mental health history, % | |
| • Anxiety or depression | 45.7 |
| • Other diagnosed mental illness | 13.0 |
| Mean (SD) cigarettes per d | 16.7 (10.4) |
| Mean (SD) length of time smoking, y | 27.9 (15.1) |
| Time to first cigarette in the morning, % | |
| • > 60 min | 19.6 |
| • 31 to 60 min | 17.8 |
| • 5 to 30 min | 34.8 |
| • < 5 min | 27.7 |
| Readiness to quit,* % | |
| • Ready in next 30 d | 30.6 |
| • Ready in next 6 mo | 41.2 |
| • Not ready | 28.2 |
| Mean (SD) self-efficacy† | 5.1 (3.0) |
| Purpose of visit, % | |
| • Annual examination or index appointment | 20.5 |
| • Follow-up appointment | 79.5 |
Which of the following best describes your feelings about smoking right now?
On a scale of 1 to 10, how confident are you that you would be able to quit smoking at this time, 1 being not at all confident and 10 being extremely confident?
Provider delivery of EBSCTs
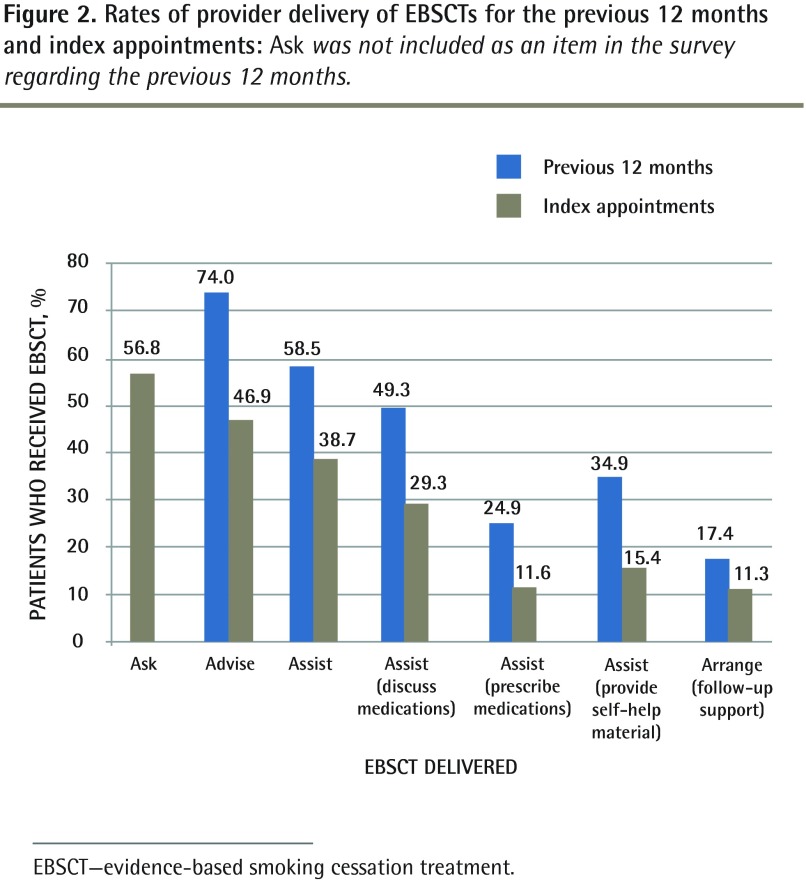
The rates of delivery of EBSCTs among all FHTs in the previous 12-month period as well as at the index appointments are reported in Figure 2. During the previous 12 months, 74.0% of patients had been advised to quit smoking; however, only 58.5% of patients reported receiving assistance with smoking cessation. Intervention rates were much lower at the index appointments across all EBSCTs (Figure 2). Rates of assistance with quitting were higher when the subpopulation of smokers who reported they were ready to quit in the next 30 days was examined (Figure 3).
Figure 2.
Rates of provider delivery of EBSCTs for the previous 12 months and index appointments: Ask was not included as an item in the survey regarding the previous 12 months.
EBSCT—evidence-based smoking cessation treatment.
Figure 3.
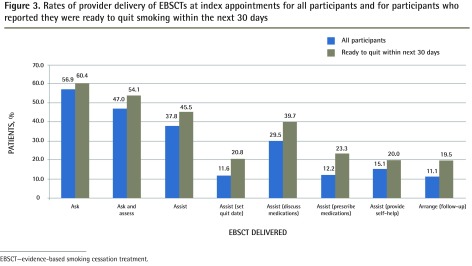
Rates of provider delivery of EBSCTs at index appointments for all participants and for participants who reported they were ready to quit smoking within the next 30 days
EBSCT—evidence-based smoking cessation treatment.
Intra-FHT and intraprovider variability
Table 3 presents the ICCs for each of the EBSCTs evaluated. The ICCs indicate substantial intra-FHT (ICC = 0.1) and intraprovider (ICC = 0.04 to 0.22) clustering for most EBSCTs. For example, for advice at the FHT level at the index visit, differences accounted for 10% of the variability in the odds of a patient being advised versus not advised and provider-level differences accounted for 14% of the variability. Figure 4 depicts the variation by FHT in the rates of delivery of EBSCTs.
Table 3.
Intra-FHT and intraprovider variation in the delivery of EBSCTs
| VARIABLE |
INTRA-FHT*
|
INTRAPROVIDER†
|
||||
|---|---|---|---|---|---|---|
| σ2μ0‡ | ICC | P VALUE | σ2μ0‡ | ICC | P VALUE | |
| Index visit | ||||||
| • Ask | 0.23 (0.07) | 0.1 | < .01 | 0.23 (0.06) | 0.12 | < .001 |
| • Advise | 0.40 (0.11) | 0.1 | < .01 | 0.14 (0.06) | 0.14 | < .05 |
| • Assist | 0.21 (0.07) | 0.1 | < .01 | 0.23 (0.07) | 0.12 | < .01 |
| • Set quit dates | 0.01 (0.05) | 0.1 | 0.33 (0.13) | 0.10 | < .01 | |
| • Discuss medications | 0.19 (0.07) | 0.1 | < .01 | 0.25 (0.08) | 0.12 | < .01 |
| • Prescribe medications | 0.12 (0.07) | 0.0 | NS | 0.21 (0.13) | 0.09 | NS |
| • Provide self-help | 0.46 (0.14) | 0.1 | < .01 | 0.25 (0.11) | 0.18 | < .05 |
| • Arrange follow-up | 0.00 (0.00) | 0.0 | NS | 0.12 (0.01) | 0.04 | < .001 |
| Previous 12 mo | ||||||
| • Advise | 0.11 (0.05) | 0.0 | < .05 | 0.21 (0.08) | 0.09 | < .01 |
| • Assist | 0.11 (0.05) | 0.0 | < .05 | 0.18 (0.07) | 0.08 | < .01 |
| • Set quit date | 0.20 (0.24) | 0.1 | NS | 0.70 (0.32) | 0.22 | < .05 |
| • Discuss medications | 0.06 (0.04) | 0.0 | NS | 0.16 (0.06) | 0.06 | < .01 |
| • Prescribe medications | 0.04 (0.03) | 0.0 | NS | 0.07 (0.07) | 0.03 | NS |
| • Provide self-help | 0.05 (0.04) | 0.0 | NS | 0.32 (0.08) | 0.10 | < .001 |
EBSCT—evidence-based smoking cessation therapy, FHT—family health team, ICC—intraclass correlation coefficient, NS—not significant.
Variation between FHTs sampled.
Variation between providers within the same FHT.
Variance.
Figure 4.
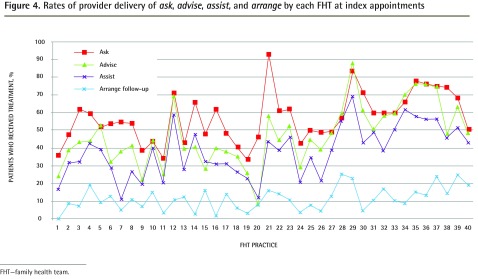
Rates of provider delivery of ask, advise, assist, and arrange by each FHT at index appointments
FHT—family health team.
Predictors of EBSCT delivery
The final model of the stepwise multi-level analysis is presented in Table 4. The final model revealed that the presence of a physician champion in the FHT was positively associated with rates at which EBSCTs are delivered (odds ratio [OR] 2.0; 95% CI 1.1 to 3.6; P < .01). Additionally, providers who ranked the importance of smoking cessation highly were more likely to deliver cessation advice to patients (OR 1.7; 95% CI 1.1 to 2.7; P < .01). Patient characteristics including readiness to quit (OR 1.6; 95% CI 1.3 to 1.9; P < .001), presence of smoking-related illness (OR 1.6; 95% CI 1.2 to 2.1; P < .01), and presentation for an annual health examination (OR 2.0; 95% CI 1.6 to 2.5; P < .001) were associated with higher rates of 5 As delivery.
Table 4.
Odds ratio for FHT, provider, and patient variables associated with receiving advice to quit smoking at the index visit:Advise model: 1 = advice given (n = 1168), 0 = no advice given (n = 1301). Models adjusted for FHT-level and provider-level clustering effects. P values calculated based on Wald tests.
| VARIABLES | ADJUSTED OR (95% CI) | P VALUE |
|---|---|---|
| Patient | ||
| Smoking-related illness | < .01 | |
| • No | 1.0 (Reference) | |
| • Yes | 1.6 (1.2 to 2.1) | |
| Readiness to quit* | < .001 | |
| • Not ready to quit | 1.0 (Reference) | |
| • Ready in next 30 d | 1.6 (1.3 to 1.9) | |
| Provider | ||
| Importance of cessation† | < .01 | |
| • Important, somewhat important, or not important | 1.0 (Reference) | |
| • Extremely or very important | 1.7 (1.1 to 2.7) | |
| Appointment | ||
| Purpose of visit | < .001 | |
| • Follow-up appointment | 1.0 (Reference) | |
| • Annual examination | 2.0 (1.6 to 2.5) | |
| FHT | ||
| Physician champion | < .01 | |
| • No | 1.0 (Reference) | |
| • Yes | 2.0 (1.1 to 3.6) |
FHT—family health team, OR—odds ratio.
Which of the following best describes your feelings about smoking right now? (1 = ready to quit in next 30 d, 0 = ready to quit in next 6 mo, or not ready to quit.)
As a practitioner, how would you describe the importance you place personally on helping your patients quit smoking? (Extremely important, very important, important, somewhat important, and not important.)
DISCUSSION
We found that, in the 12 months before the study index visits, the rate at which patients who smoked were advised by primary care providers to quit smoking (74.0%) was much higher than previously reported in Canada. In contrast, the 2010 Canadian Tobacco Use Monitoring Survey has reported that among Ontario smokers who had visited doctors in the past year, 47% received advice to quit smoking.3 While these data indicate superior performance among FHTs sampled in the delivery of EBSCT, best-practice guidelines recommend that patients be advised to quit at every primary care visit. The rate at which patients were advised to quit at the index appointment in this study was substantially lower (46.9%). Additionally, the rates at which specific forms of assistance with quitting were delivered at the index appointment were much lower, at 38.7% for assistance, 11.6% for prescribing pharmacotherapy, and 11.3% for arranging a follow-up appointment to discuss cessation.
Our evaluation also documented substantial variability among FHTs in the rates at which EBSCTs were delivered. There was also a substantial difference between rates at which providers from the same FHT delivered smoking cessation interventions. Addressing this variation among practices, and perhaps more importantly among providers within the same practice settings, affords an opportunity to enhance the quality of care.
To our knowledge, this is the first study to report on provider performance in the delivery of EBSCTs among Ontario FHTs. Previously, the best available data on practitioners’ performance in delivery of EBSCTs were from the Canadian Tobacco Use Monitoring Survey, which used random-digit dialing to survey respondents to assess national trends in tobacco use and treatment.3 A second Canadian survey examined self-reported rates of smoking cessation counseling in a sample of general practitioners in Quebec.25 As in the present study, rates of advice were moderate and rates of assistance with quitting were low.25 A US report examined medical records for tobacco use screening and counseling during physician office visits between 2005 and 2009.26 The report’s findings were consistent with our own; tobacco use screening occurred during most adult visits (62.7%), but only 20.9% received tobacco cessation counseling and only 7.6% received tobacco cessation medication.
This study provides new information on provider performance in the delivery of EBSCTs among Ontario FHTs and can assist with benchmarking performance, informing future policy and practice, and identifying important factors likely to influence the frequency with which EBSCTs are delivered.
Limitations
While this study represents 20% of Ontario FHTs, participation in the study was voluntary and selection bias related to nonresponse might limit the generalizability of our findings. The most likely effect of this possible bias is an overestimation of provider performance in EBSCT delivery as a result of greater motivation among teams who enrolled in the Ottawa Model for Smoking Cessation in Primary Care program. The exit survey was completed by 60% of eligible patients screened and thus our data might not represent the entire population of smokers seen in FHTs.
Conclusion
Future quality improvement initiatives should specifically target increasing the rates of screening and advising among low-performing FHTs and providers within FHTs, with a particular emphasis on doing so at all clinic appointments; and improving the rates at which assistance with quitting is delivered.
Acknowledgments
We thank the leadership and staff from the network of Ontario family health teams involved in this project.
EDITOR’S KEY POINTS
In the 12 months before the study index visits, the rate at which primary care providers had advised patients who smoked to quit smoking (74.0%) was much higher than previously reported in Canada.
The rate at which patients were advised to quit at the index appointment was substantially lower (46.9%). Additionally, the rates at which specific forms of assistance with quitting were delivered at the index appointment were much lower, at 38.7% for assistance, 11.6% for prescribing pharmacotherapy, and 11.3% for arranging a follow-up appointment to discuss cessation.
This study provides new information on provider performance in the delivery of evidence-based smoking cessation treatments among Ontario family health teams and can assist with benchmarking performance, informing future policy and practice, and identifying important factors likely to influence the frequency with which evidence-based smoking cessation treatments are delivered.
POINTS DE REPÈRE DU RÉDACTEUR
Au cours des 12 mois précédant la visite repère de l’étude, le taux auquel les soignants de première ligne avaient conseillé au patient de cesser de fumer (74,0 %) était beaucoup plus haut que celui antérieurement rapporté au Canada.
Lors du rendez-vous repère, le taux auquel on a conseillé aux patients d’abandonner le tabac était considérablement plus bas (49,9 %). De plus, les taux auxquels diverses formes d’assistance pour cesser de fumer ont été offertes aux patients à l’occasion de la visite repère étaient beaucoup plus bas, soit 38,7 % pour «assister», 11,6 % pour «prescrire» une médication et 11,3 % pour «planifier» un rendez-vous pour discuter de l’arrêt du tabac.
Cette étude fournit des informations nouvelles sur la façon dont les membres des équipes de santé familiale de l’Ontario utilisent un traitement fondé sur des données probantes visant l’arrêt du tabac, en plus d’aider à établir des critères de rendement, d’orienter les politiques et les pratiques futures et d’identifier certains facteurs importants susceptibles d’influencer la fréquence à laquelle ce traitement est utilisé.
Footnotes
Competing interests
This project was supported by the Canadian Tobacco Control Research Initiative, the Heart and Stroke Foundation of Ontario, the Heart and Stroke Foundation of Canada, and Pfizer Canada Inc. Dr Pipe has received educational and research support in the past from Pfizer and Johnson & Johnson, and has served as a consultant to Pfizer and Amgen. Dr Reid has received speaker and consultant fees from Pfizer and Johnson & Johnson in the past that are not related to this project.
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
Dr Papadakis designed the study methods, conducted the analysis, and prepared the manuscript. Ms Gharib oversaw data collection activities, analysis, and article preparation. Mr Hambleton contributed to data interpretation and article review. Dr Reid contributed to study design and article review. Ms Assi contributed to data collection and article review. Dr Pipe contributed to the study design, site recruitment, and article preparation.
References
- 1.Ministry of Health and Long-Term Care. We’re making progress. FHT to Print. 2011 Summer-Fall; Available from: www.health.gov.on.ca/en/pro/programs/fht/docs/fht_news_201110.pdf. Accessed 2014 Jun 19. [Google Scholar]
- 2.Ministry of Health and Long Term Care. Guide to communications. Toronto, ON: Ministry of Health and Long-Term Care; 2006. Available from: www.health.gov.on.ca/en/pro/programs/fht/docs/fht_communications2.pdf. Accessed 2014 Jun 25. [Google Scholar]
- 3.Reid JL, Hammond D, Burkhalter R, Rynard VL, Ahmed R. Tobacco use in Canada: patterns and trends. 2013 ed. Waterloo, ON: Propel Centre for Population Health, University of Waterloo; 2013. [Google Scholar]
- 4.Rehm J, Baliunas D, Brochu S, Fischer B, Gnam W, Patra J, et al. The costs of substance abuse in Canada 2002. Highlights. Ottawa, ON: Canadian Centre on Substance Abuse; 2006. [Google Scholar]
- 5.Makomaski Illing EM, Kaiserman MJ. Mortality attributable to tobacco use in Canada and its regions, 1998. Can J Public Health. 2004;95(1):38–44. doi: 10.1007/BF03403632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.U.S. Department of Health and Human Services. The health consequences of smoking: a report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004. [Google Scholar]
- 7.Ontario Tobacco Research Unit. The burden of tobacco use in Ontario. Toronto, ON: Ontario Tobacco Research Unit; 2006. [Google Scholar]
- 8.Schwartz R, O’Connor S, Minian N, Borland T, Babayan A, Ferrence R, et al. Evidence to inform smoking cessation policy making in Ontario. A special report by the Ontario Tobacco Research Unit. Toronto, ON: Ontario Tobacco Research Unit;; 2010. [Google Scholar]
- 9.Fiore MC, Jaén CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, et al. Treating tobacco use and dependence: 2008 update. Rockville, MD: U.S. Department of Health and Human Services, Health Resources and Services Administration; 2008. [Google Scholar]
- 10.Quinn VP, Stevens VJ, Hollis JF, Rigotti NA, Solberg LI, Gordon N, et al. Tobacco-cessation services and patient satisfaction in nine nonprofit HMOs. Am J Prev Med. 2005;29(2):77–84. doi: 10.1016/j.amepre.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 11.Zwar NA, Richmond RL. Role of the general practitioner in smoking cessation. Drug Alcohol Rev. 2006;25(1):21–6. doi: 10.1080/09595230500459487. [DOI] [PubMed] [Google Scholar]
- 12.Cahill K, Stead LF, Lancaster T. Nicotine receptor partial agonists for smoking cessation. Cochrane Database Syst Rev. 2007;1:CD006103. doi: 10.1002/14651858.CD006103.pub2. [DOI] [PubMed] [Google Scholar]
- 13.Stead LF, Perera R, Bullen C, Mant D, Hartmann-Boyce J, Cahill K, et al. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev. 2012;11:CD000146. doi: 10.1002/14651858.CD000146.pub4. [DOI] [PubMed] [Google Scholar]
- 14.Zwar N, Richmond R, Borland R, Peters M, Litt J, Bell J, et al. Supporting smoking cessation: a guide for health professionals. Melbourne, Aust: Royal Australian College of General Practitioners; 2011. [Google Scholar]
- 15.Reda AA, Kaper J, Fikrelter H, Severens JL, van Schayck CP. Healthcare financing systems for increasing the use of tobacco dependence treatment. Cochrane Database Syst Rev. 2009;2:CD004305. doi: 10.1002/14651858.CD004305.pub3. [DOI] [PubMed] [Google Scholar]
- 16.Kaper J, Wagena EJ, Willemsen MC, van Schayck CP. Reimbursement for smoking cessation treatment may double the abstinence rate: results of a randomized trial. Addiction. 2005;100(7):1012–20. doi: 10.1111/j.1360-0443.2005.01097.x. [DOI] [PubMed] [Google Scholar]
- 17.Coleman T, Wilson A, Barrett S, Wynne A, Lewis S. Distributing questionnaires about smoking to patients: impact on general practitioners’ recording of smoking advice. BMC Health Serv Res. 2007;7:153. doi: 10.1186/1472-6963-7-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Twardella D, Brenner H. Effects of practitioner education, practitioner payment and reimbursement of patients’ drug costs on smoking cessation in primary care: a cluster randomised trial. Tob Control. 2007;16(1):15–21. doi: 10.1136/tc.2006.016253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Katz DA, Muehlenbruch DR, Brown RB, Fiore MC, Baker TB. AHRQ Smoking Cessation GuidelineStudy Group. Effectiveness of a clinic-based strategy for implementing the AHRQ smoking cessation guideline in primary care. Prev Med. 2002;35(3):293–301. doi: 10.1006/pmed.2002.1073. [DOI] [PubMed] [Google Scholar]
- 20.Katz DA, Brown RB, Muehlenbruch DR, Fiore MC, Baker TB. AHRQ Smoking Cessation Guideline Study Group. Implementing guidelines for smoking cessation: comparing the efforts of nurses and medical assistants. Am J Prev Med. 2004;27(5):411–6. doi: 10.1016/j.amepre.2004.07.015. [DOI] [PubMed] [Google Scholar]
- 21.Unrod M, Smith M, Spring B, DePue J, Redd W, Winkel G. Randomized controlled trial of a computer-based, tailored intervention to increase smoking cessation counseling by primary care physicians. J Gen Intern Med. 2007;22(4):478–84. doi: 10.1007/s11606-006-0069-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pbert L, Adams A, Quirk M, Hebert JR, Ockene JK, Luippold RS. The patient exit interview as an assessment of physician-delivered smoking intervention: a validation study. Health Psychol. 1999;18(2):183–8. doi: 10.1037//0278-6133.18.2.183. [DOI] [PubMed] [Google Scholar]
- 23.Killip S, Mahfoud Z, Pearce K. What is an intracluster correlation coefficient? Crucial concepts for primary care researchers. Ann Fam Med. 2004;2(3):204–8. doi: 10.1370/afm.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Murnaghan DA, Sihvonen M, Leatherdale ST, Kekki P. The relationship between school-based smoking policies and prevention programs on smoking behavior among grade 12 students in Prince Edward Island: a multilevel analysis. Prev Med. 2007;44(4):317–22. doi: 10.1016/j.ypmed.2007.01.003. Epub 2007 Jan 18. [DOI] [PubMed] [Google Scholar]
- 25.Tremblay M, Cournoyer D, O’Loughlin J. Do the correlates of smoking cessation counseling differ across health professional groups? Nicotine Tob Res. 2009;11(11):1330–8. doi: 10.1093/ntr/ntp142. Epub 2009 Sep 21. [DOI] [PubMed] [Google Scholar]
- 26.Jamal A, Dube SR, Malarcher AM, Shaw L, Engstrom MC. Centers for Disease Control and Prevention. Tobacco use screening and counseling during physician office visits among adults—National Ambulatory Medical Care Survey and National Health Interview Survey, United States, 2005–2009. MMWR Morb Mortal Wkly Rep. 2012;61(Suppl):38–45. [PubMed] [Google Scholar]