Abstract
Objectives. We examined the relationship between discrimination and substance use disorders among a diverse sample of Latinos. We also investigated whether the relationship between discrimination and substance use disorders varied by gender, nativity, and ethnicity.
Methods. Our analyses focused on 6294 Latinos who participated in the National Epidemiologic Survey on Alcohol and Related Conditions from 2004 to 2005. We used multinomial logistic regression to examine the association between discrimination and substance use disorders.
Results. Discrimination was significantly associated with increased odds of alcohol and drug use disorders among Latinos. However, the relationship between discrimination and substance use disorders varied by gender, nativity, and ethnicity. Discrimination was associated with increased odds of alcohol and drug use disorders for certain groups, such as women, US-born Latinos, and Mexicans, but this relationship did not follow the same pattern for other subgroups.
Conclusions. It is important to determine which subgroups among Latinos may be particularly vulnerable to the negative effects of discrimination to address their needs.
Latinos are the largest ethnic or racial minority group in the United States1 and the fastest growing group entering substance abuse treatment programs.2 Although Latinos are disproportionately affected by substance abuse,3 they have been understudied.4 Previous research shows that high levels of poverty, minority status, and residential concentration in areas with widespread drug and alcohol distribution have been considered to be factors that may put Latinos at risk for substance use disorders.5 More recently, discrimination has also been considered to be a risk factor.6,7 As studies aim toward filling the gap in the literature, the heterogeneity of Latinos must also be considered.
Discrimination has been associated with alcohol and drug use8–13 and substance use disorders among Latinos.6,7 Stress-coping frameworks and the minority stress model have been applied to hypothesize that individuals belonging to various marginalized groups respond to experiences of discrimination with unhealthy coping behaviors, such as substance use.14,15 Moreover, discrimination may lead to underemployment, lower wages, and limited access to health services and other resources that can affect health outcomes.16 In this way, discrimination operates at both the interpersonal and institutional levels simultaneously to situate individuals on different health trajectories, fostering and reinforcing poor health behaviors and outcomes.16,17
The association between discrimination and substance use has been previously documented for Latinos and other groups. However, reviews of the literature have called for more granular analysis of specific risk patterns. One specific area needing analysis is whether some subgroups of Latinos are at higher risk of substance use related to discrimination than others. The identification of subgroups is an important first step toward the development of targeted population-level approaches and tailored interventions.
In the present study, we focused on subgroups based on gender, nativity, and ethnicity (country of origin or heritage country). These subgroups were based on ascribed characteristics that refer to immutable characteristics (vs achieved characteristics, such as education) that are given status value.18,19 The status value placed on these characteristics can drive discrimination; for example, when men are considered more valuable than women and when US-born individuals are considered more valuable than immigrants.18,19 At the same time, these characteristics (gender, nativity, and ethnicity) are also associated with substance use disorders.
Gender differences in substance use disorders are not unique to Latinos. Across racial/ethnic groups, men consistently have higher prevalence of substance use disorders. Using data from the National Latino and Asian American Study, the lifetime prevalence of alcohol use disorders was 16.7% for Latino men and 4.3% for Latina women.20 Research also shows that Latino men generally reported higher levels of discrimination compared with Latina women.13,21 Data from the National Latino and Asian American Study showed that 39% of Latino men, compared with 29% of Latina women, reported discrimination.22 These authors suggested that these patterns might be the result of minority men being more exposed and vulnerable to racial bias from social institutions. These higher rates of substance use and discrimination among men also appeared to be jointly related. A recent study found that discrimination was associated with increased risk of drug abuse among Latino men, but not Latina women.6 This interaction might occur because of greater cultural acceptability among men overall to use substances to cope with stress compared with women. In contrast, women were found to rely on social support and to turn to food to cope with stress.23–25 Other specific factors, such as abuse history,26 were found to be more central in predicting risk of substance use disorders among Latina women. Thus, we expected that discrimination would have a stronger relationship with substance use disorders among Latino men than Latina women.
Similar to health differences by gender, differences by nativity are not unique to Latinos. Overall, foreign-born individuals tend to be healthier than their US-born counterparts. Lifetime rates of substance use disorders were higher among US-born than foreign-born Latinos (19.6% vs 5.5%, respectively).20 Previous studies also found greater reporting of discrimination among US-born Latinos; 47% of US-born compared with 25% of foreign-born Latinos reported discrimination.22 However, discrimination might be more harmful to foreign-born Latinos because they are less likely to enjoy citizenship rights (e.g., voting privileges, access to educational scholarships) that might help temper some of the stressful effects of discrimination. From this perspective, we expected that discrimination would have a stronger relationship with substance use disorders among foreign-born than US-born Latinos.
Finally, it is also important to consider ethnicity. There is some indication of variation in rates of substance use across these groups. Cubans were found to have lower odds of substance use disorders compared with Puerto Ricans.27 In addition, there was good evidence for variation in reporting of discrimination.28 For example, 40% of Puerto Ricans reported discrimination compared with 34% of Mexicans and 16% of Cubans.22 This variation might be attributed to gradations based on socioeconomic resources that differ by Latino ethnicity.29 Gradations based on socioeconomic resources could dictate the risks and resources individuals have exposure and access to, affecting coping mechanisms. Thus, we expected the relationship between discrimination and substance use disorders to vary by ethnicity as well.
In sum, based on this literature, we hypothesized that discrimination would be associated with increased risk of substance use disorders among Latinos overall, and that the relationship between discrimination and substance use disorders would vary by ascribed characteristics. Specifically, we theorized that the relationship between discrimination and substance use disorders would be stronger among men compared with women, among foreign-born Latinos compared with US-born Latinos, and among Mexicans and Puerto Ricans compared with Cubans.
METHODS
Our analysis used wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a nationally representative general population survey carried out from 2004 to 2005.30 Wave 1 of NESARC was conducted from 2001 to 2002 with 43 093 respondents, including 7995 Latinos. Wave 2 re-interviewed 34 653 respondents, including 6359 Latinos. NESARC was designed to be representative of the noninstitutionalized population of adults in the United States, aged 18 years and older.30,31 NESARC used the Census Supplementary Survey for the sampling frame of housing units and the Census 2000 Group Quarters Inventory for the group quarters sampling frame. In addition, African Americans, Latinos, and young adults aged 18 to 24 years were oversampled.30 NESARC weights allowed for the sample to be representative of the US population based on the 2000 US Census. Details on the sampling strategy can be found elsewhere.32–34
Face-to-face interviews were conducted by interviewers trained by the US Census Bureau.35 We focused on the national sample of 6359 Latino respondents that were re-interviewed in wave 2, which contained questions on discrimination. Latinos lost to follow-up between waves were more likely to be young and male, and have lower levels of income and education, but did not differ in prevalence of substance use disorders.35 Latinos who were missing responses on items included in our analysis (1% of the wave 2 Latinos) were excluded from the study, yielding a sample of 6294.
Measures
Dependent variable.
The dependent variable for this analysis was lifetime substance use disorders, measured using the National Institute on Alcohol Abuse and Alcoholism, Alcohol Use Disorder and Associated Disabilities Interview Schedule. The Alcohol Use Disorder and Associated Disabilities Interview Schedule uses criteria for alcohol and other drug disorders based on the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV), and is designed to be administered by trained lay interviewers.30,36 These measures captured abuse and dependence on alcohol and drugs, including cannabis, hallucinogens, opiates, heroin, amphetamine, cocaine, sedatives, tranquilizers, and solvents. We categorized substance use disorders as no substance use disorders (0); alcohol-only abuse or dependence, which we refer to as alcohol use disorders (1); and drug abuse or dependence with or without alcohol, which we refer to as drug use disorders (2). This categorization was based on the distribution of responses and because the majority of respondents who had a drug use disorder (80%) also had an alcohol use disorder.
Independent variables.
Lifetime discrimination was operationalized as lifetime racial/ethnic discrimination using the Experience of Discrimination Scale,37,38 which included 6 items that asked how often respondents had experienced certain forms of discrimination because they were Latino, such as (1) in public, for example, on the street, in stores, or in restaurants; and (2) if they had been called a racist name. The response categories ranged from 1 (never) to 5 (very often). Respondents were asked about their experiences in the past 12 months and before 12 months ago. The 2 questions were combined to yield a lifetime variable.
Sociodemographics and immigrant characteristics.
Latino ethnicity was measured by asking respondents to report their country of origin or ethnicity from a list of 58 categories.35 Based on the distribution of responses, Latinos were grouped as (1) Mexican, (2) Mexican American, (3) Puerto Rican, (4) Cuban, (5) Central American, (6) South American, and (7) Other Latino, similar to previous studies.35 Although Central American, South American, and Other Latino comprise many ethnicities themselves, we still included them in our analyses in aggregate categories rather than being excluded. In addition, the questionnaire allowed respondents to distinguish between Mexican and Mexican American, although this distinction was not available for other Latino ethnicities. Given the large sample of Mexicans and Mexican Americans, they were grouped separately to determine any differences.35
We measured nativity by asking respondents whether they were born in the United States, yielding a dichotomous foreign-born versus US-born variable.
Additional sociodemographics and immigrant characteristics included: language preference, which was measured using 7 items from the Language Orientation subscale of the Short Acculturation Scale (α = 0.93)39,40; stress, which was measured using the 4-item Perceived Stress Scale (α = 0.84)41,42; and gender, age, education, household income, employment status, and region (e.g., Northwest, Midwest, South, West) measured through single items.
Analyses
We began the analyses with simple descriptive measures of correlations and bivariate associations between substance use disorders and independent variables. We used multinomial logistic regression to assess whether associations between discrimination and substance use disorders held after controlling for additional covariates (the baseline category was “no substance use disorders”). We specified four models. The first model included discrimination, sociodemographics, and immigrant characteristics. Models 2, 3, and 4 added interaction terms between discrimination and ascribed characteristics: gender, nativity, and ethnicity, respectively. Analyses were weighted and were performed using Stata version 13 software.43
RESULTS
Table 1 shows the descriptive statistics of the study sample. Approximately 1 in 5 Latinos (19.4%) had an alcohol use disorder, whereas approximately 1 in 10 (9.2%) had a drug use disorder. Approximately one third (29.7%) reported discrimination.
TABLE 1—
Descriptive Statistics of Latinos (Weighted): National Epidemiologic Survey on Alcohol and Related Conditions, Wave 2; United States; 2004–2005.
| Characteristics | % or Mean ±SE (range) |
| Substance use disorders (lifetime) | |
| No substance use disorders | 71.36 |
| Alcohol-only abuse/dependence | 19.42 |
| Alcohol/drug or drug-only abuse/dependence | 9.22 |
| Racial/ethnic discrimination (lifetime) | 29.69 |
| Latino ethnicity | |
| Mexican | 32.03 |
| Mexican American | 23.08 |
| Puerto Rican | 10.22 |
| Cuban | 3.92 |
| Central American | 7.43 |
| South American | 5.03 |
| Other | 18.31 |
| Male | 50.92 |
| Region | |
| Northwest | 13.52 |
| Midwest | 23.11 |
| South | 36.84 |
| West | 26.53 |
| Age, y | 43.82 ±15.79 (20–90) |
| Education | |
| < high school | 34.68 |
| High school/GED | 24.36 |
| ≥ some college | 40.96 |
| Household income, $ | |
| < 15 000 | 15.26 |
| 15 000–39 999 | 38.98 |
| 40 000–89 999 | 35.36 |
| ≥ 90 000 | 10.39 |
| Currently employed | 78.37 |
| Immigrant characteristics | |
| Foreign-born | 55.29 |
| English language preference | 3.01 ±0.01 (1–5) |
| Perceived stress (past year) | 2.78 ±0.00 (1–5) |
Note. GED = general equivalency diploma. Drugs included cannabis, hallucinogens, opioids, heroin, amphetamine, cocaine, sedatives, tranquilizers, and solvents.
The majority of respondents identified as Mexican (32%) or Mexican American (23.1%), with smaller proportions identifying as Puerto Rican (10.2%), Cuban (3.9%), Central American (7.4%), South American (5%), or Other Latino (18.3%). There was approximately the same proportion of women as men and US-born as foreign-born in the sample.
Table 2 shows the unadjusted and adjusted associations between select covariates and substance use disorders using multinomial logistic regression, with no substance use disorders as the base outcome. Overall, the unadjusted associations were as hypothesized: discrimination and male gender were associated with increased odds, whereas being foreign-born was associated with decreased odds of substance use disorders.
TABLE 2—
Association Between Select Covariates and Substance Use Disorders Among Latinos (Weighted): National Epidemiologic Survey on Alcohol and Related Conditions, Wave 2; United States; 2004–2005
| Adjusted, OR (95% CI) |
||||||
| Variable | Unadjusted, OR (95% CI) | Model 1 | Model 2 | Model 3 | Model 4 | |
| Alcohol-only abuse/dependence | ||||||
| Discrimination | 1.54*** (1.46, 1.63) | 1.32*** (1.23, 1.40) | 2.04*** (1.84, 2.26) | 1.6*** (1.44, 1.77) | 1.47*** (1.34, 1.63) | |
| Male | 4.37*** (4.14, 4.62) | 5*** (4.69, 5.33) | 6.32*** (5.85, 6.82) | 5.01*** (4.70, 5.34) | 5.01*** (4.70, 5.34) | |
| Foreign-born | 0.44*** (0.42, 0.47) | 0.68*** (0.63, 0.72) | 0.68*** (0.64, 0.73) | 0.8*** (0.73, 0.87) | 0.68*** (0.64, 0.73) | |
| Latino ethnicity | ||||||
| Mexican (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| Mexican American | 1.43*** (1.31, 1.56) | 0.92 (0.84, 1.02) | 0.93 (0.84, 1.02) | 0.93 (0.84, 1.02) | 0.98 (0.88, 1.10) | |
| Puerto Rican | 0.69*** (0.63, 0.75) | 0.5*** (0.46, 0.54) | 0.5*** (0.46, 0.54) | 0.5*** (0.46, 0.54) | 0.48*** (0.44, 0.53) | |
| Cuban | 0.25*** (0.22, 0.29) | 0.25*** (0.22, 0.29) | 0.25*** (0.21, 0.28) | 0.25*** (0.22, 0.29) | 0.32*** (0.27, 0.37) | |
| Central American | 0.65*** (0.60, 0.70) | 0.66*** (0.60, 0.72) | 0.66*** (0.60, 0.72) | 0.66*** (0.61, 0.72) | 0.77*** (0.69, 0.85) | |
| South American | 0.73*** (0.67, 0.79) | 0.75*** (0.69, 0.81) | 0.75*** (0.69, 0.81) | 0.76*** (0.70, 0.82) | 0.98 (0.88, 1.08) | |
| Other | 1.16* (1.03, 1.30) | 0.67*** (0.60, 0.75) | 0.67*** (0.60, 0.76) | 0.69*** (0.61, 0.77) | 0.66*** (0.57, 0.77) | |
| Discrimination × male | 0.55*** (0.49, 0.62) | . . . | 0.52*** (0.47, 0.58) | . . . | . . . | |
| Discrimination × foreign-born | 0.8*** (0.70, 0.91) | . . . | . . . | 0.65*** (0.57, 0.75) | . . . | |
| Discrimination × Latino ethnicity | ||||||
| Mexican (Ref) | 1.00 | . . . | . . . | . . . | 1.00 | |
| Mexican American | 0.8*** (0.70, 0.91) | . . . | . . . | . . . | 0.84* (0.72, 0.97) | |
| Puerto Rican | 1.11 (0.93, 1.32) | . . . | . . . | . . . | 1.07 (0.90, 1.27) | |
| Cuban | 0.3*** (0.26, 0.35) | . . . | . . . | . . . | 0.28*** (0.24, 0.33) | |
| Central American | 0.67*** (0.56, 0.80) | . . . | . . . | . . . | 0.63*** (0.52, 0.77) | |
| South American | 0.4*** (0.35, 0.47) | . . . | . . . | . . . | 0.42*** (0.36, 0.49) | |
| Other | 0.79 (0.61, 1.01) | . . . | . . . | . . . | 1.05 (0.81, 1.36) | |
| Alcohol/drug or drug-only abuse/dependence | ||||||
| Discrimination | 1.83*** (1.67, 2.01) | 1.46*** (1.31, 1.63) | 1.65*** (1.38, 1.98) | 1.52*** (1.32, 1.75) | 1.76*** (1.47, 2.10) | |
| Male | 2.93*** (2.61, 3.29) | 4.11*** (3.62, 4.66) | 4.45*** (3.65, 5.43) | 4.12*** (3.63, 4.67) | 4.12*** (3.63, 4.66) | |
| Foreign-born | 0.12*** (0.11, 0.13) | 0.37*** (0.33, 0.40) | 0.37*** (0.34, 0.40) | 0.35*** (0.32, 0.40) | 0.37*** (0.34, 0.41) | |
| Latino ethnicity | ||||||
| Mexican (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| Mexican American | 2.08*** (1.92, 2.25) | 0.72*** (0.64, 0.80) | 0.72*** (0.64, 0.80) | 0.71*** (0.64, 0.80) | 0.77** (0.65, 0.92) | |
| Puerto Rican | 2.23*** (1.97, 2.53) | 1.07 (0.94, 1.23) | 1.08 (0.95, 1.23) | 1.07 (0.94, 1.22) | 1.19 (0.95, 1.49) | |
| Cuban | 0.97 (0.91, 1.04) | 1.08 (0.99, 1.18) | 1.07 (0.98, 1.17) | 1.07 (0.98, 1.18) | 1.08 (0.94, 1.24) | |
| Central American | 0.86** (0.79, 0.94) | 0.98 (0.89, 1.08) | 0.98 (0.89, 1.08) | 0.98 (0.89, 1.08) | 0.97 (0.82, 1.15) | |
| South American | 1.11* (1.01, 1.21) | 1.3*** (1.18, 1.43) | 1.3*** (1.18, 1.43) | 1.29*** (1.17, 1.43) | 1.67*** (1.42, 1.95) | |
| Other | 3.14*** (2.80, 3.53) | 1.04 (0.90, 1.20) | 1.04 (0.90, 1.20) | 1.04 (0.89, 1.20) | 1.16 (0.95, 1.41) | |
| Discrimination × male | 0.82 (0.66, 1.01) | . . . | 0.79* (0.63, 0.99) | . . . | . . . | |
| Discrimination × foreign-born | 1.89*** (1.60, 2.23) | . . . | 1.03 (0.87, 1.23) | . . . | ||
| Discrimination × Latino ethnicity | ||||||
| Mexican (Ref) | 1.00 | . . . | . . . | . . . | 1.00 | |
| Mexican American | 0.62*** (0.51, 0.74) | . . . | . . . | . . . | 0.85 (0.68, 1.06) | |
| Puerto Rican | 0.69** (0.53, 0.89) | . . . | . . . | . . . | 0.8 (0.62, 1.03) | |
| Cuban | 0.89 (0.75, 1.04) | . . . | . . . | . . . | 1.02 (0.86, 1.21) | |
| Central American | 1.17 (0.95, 1.45) | . . . | . . . | . . . | 0.93 (0.76, 1.13) | |
| South American | 0.43*** (0.34, 0.54) | . . . | . . . | . . . | 0.51*** (0.40, 0.66) | |
| Other | 0.39*** (0.32, 0.48) | . . . | . . . | . . . | 0.75* (0.58, 0.97) | |
Note. CI = confidence interval; OR = odds ratio. Models used multinomial regression and adjusted for additional covariates where indicated, as well as region, age, education, household income, current employment status, language preference, and stress. Models used no substance use disorders as the base outcome.
*P ≤ .05; **P ≤ .01; *** P ≤ .001.
For the adjusted associations in model 1, discrimination remained significantly associated with increased odds of alcohol (odds ratio [OR] = 1.32) and drug use disorders (OR = 1.46; Table 2). Similarly, findings regarding male gender, being foreign-born, and ethnicity were unchanged in the adjusted model.
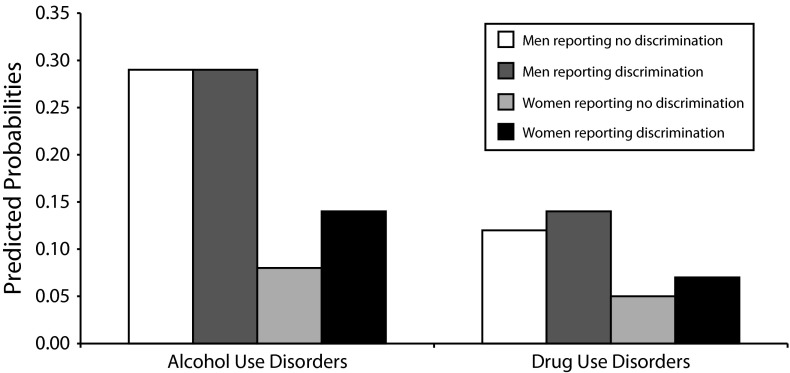
For the adjusted associations in model 2, the interaction between discrimination and gender was significantly associated with substance use disorders. Figure 1 shows this interaction for interpretability. Discrimination was associated with increased odds of alcohol and drug use disorders for women, as expected. For men, discrimination was associated with increased odds of drug use disorders, but discrimination did not appear to be associated with alcohol use disorders.
FIGURE 1—
Predicted probabilities of substance use disorders by gender and discrimination, adjusting for all other covariates among Latinos (weighted): National Epidemiologic Survey on Alcohol and Related Conditions, wave 2; United States; 2004–2005.
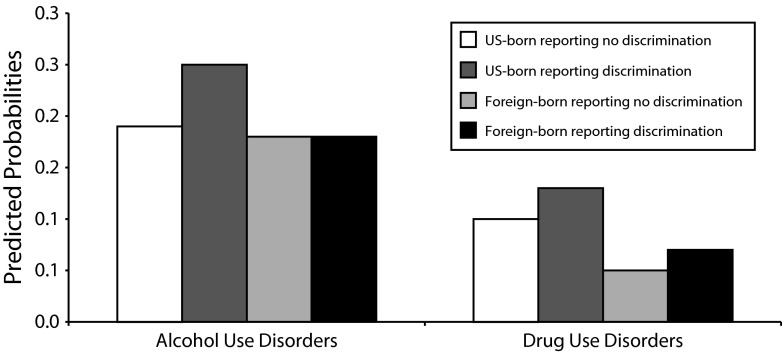
For the adjusted associations in model 3, the interaction between discrimination and nativity was significantly associated with alcohol use disorders. Figure 2, based on this model, shows that discrimination was associated with increased odds of alcohol and drug use disorders for US-born Latinos, as expected. For foreign-born Latinos, discrimination was associated with increased odds of drug use disorders, but discrimination did not appear to be associated with alcohol use disorders.
FIGURE 2—
Predicted probabilities of substance use disorders by nativity and discrimination, adjusting for all other covariates among Latinos (weighted): National Epidemiologic Survey on Alcohol and Related Conditions, wave 2; United States; 2004–2005.
For the adjusted associations in model 4, the interaction between discrimination and Latino ethnicity was significantly associated with substance use disorders. Figure 3 shows the predicted probabilities of substance use disorders, calculated by Latino ethnicity and discrimination. Figure 3 also shows that the relationship between discrimination and substance use disorders was as expected for Mexicans, Mexican Americans, Puerto Ricans, and Other Latinos. Discrimination was associated with increased odds of alcohol and drug use disorders for these groups. However, the relationship between discrimination and substance use disorders did not follow this same pattern for Cubans, Central Americans, and South Americans; discrimination was associated with decreased odds of alcohol use disorders for these groups and did not appear to be associated with odds of drug use disorders for South Americans.
FIGURE 3—
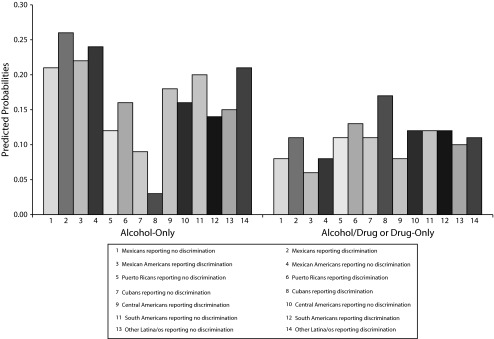
Predicted probabilities of substance use disorders by subgroup and discrimination, adjusting for all other covariates among Latinos (weighted): National Epidemiologic Survey on Alcohol and Related Conditions, wave 2; United States; 2004–2005.
DISCUSSION
Our findings provided further evidence that discrimination was associated with increased risk of substance use disorders among a national sample of Latinos. Our findings supported previous research that found associations between discrimination and substance use,8–13 as well as discrimination and substance use disorders specifically among Latinos.6,7 In addition, our study extended the existing literature by revealing that the relationship between discrimination and substance use disorders varied by ascribed characteristics among Latinos. As hypothesized, gender, nativity, and ethnicity moderated the relationship between discrimination and substance use disorders.
Given the diversity among Latinos, there were several potential reasons as to why the relationship between discrimination and substance use disorders differed by these select characteristics. In terms of gender, our findings were consistent with previous studies that found that discrimination and substance abuse differed by gender among Latinos; discrimination was significantly associated with increased risk of drug abuse, but not alcohol abuse, for men.6 The null relationship between discrimination and alcohol use disorders among Latino men might stem from gender roles, societal norms, and socialization patterns that tend to normalize alcohol use for men, in general, regardless of self-reports of discrimination.44 By contrast, when faced with stress that came from discrimination, men might be more likely to turn to drug use, in addition to alcohol, leading to higher rates of drug use disorders (but not alcohol). A key difference of our study was that discrimination was associated with both alcohol and drug use disorders for women, whereas previous findings showed that discrimination was associated with alcohol abuse, but not drug abuse, among women. Gender differences among Latinos mirror those differences found in the general population, with more pronounced differences for alcohol and cannabis,45 which were also the most commonly used substances in our study. However, our study indicated that discrimination might put Latina women at increased risk for all substance use disorders, regardless of type of substance.
Although nativity moderated the relationship between discrimination and substance use disorders, as expected, the null relationship between discrimination and alcohol use disorders among foreign-born Latinos was not as expected. Consistent with previous studies, we found that foreign-born Latinos had a lower prevalence of substance use disorders and reported lower levels of discrimination.20,22 Despite this, we expected discrimination would be more harmful to foreign-born Latinos, because they were less likely to enjoy citizenship rights and access to resources that are afforded to US-born Latinos. However, our study found that among foreign-born Latinos, discrimination was not associated with alcohol use disorders, although discrimination was associated with both alcohol and drug use disorders among US-born Latinos. One explanation is that US-born Latinos might have a heightened awareness of discrimination, because they are accustomed to the racial hierarchy and subtle forms of discrimination in the United States.46 Anticipating discrimination might compound the negative effects of discrimination for US-born Latinos.47 Another possibility is that foreign-born Latinos might have a different point of reference, such as being better off in the United States than in their country of origin. This sense of optimism among foreign-born Latinos48 might serve as a protective factor against the deleterious effects of discrimination. Future research should evaluate how awareness of discrimination, point of reference, and optimism might differ among Latinos by nativity to understand how responses to discrimination differ.
Lastly, because Latinos are a heterogeneous group, coping mechanisms might differ by ethnicity because of demographic and contextual differences. These differences translate to both individual- and community-level risks and resources. At the individual level, socioeconomic status varies by ethnicity, with Mexicans and Puerto Ricans on the lower end, and Cubans, Central Americans, and South Americans on the higher end.29 At the community level, because Cubans have the highest levels of education and income among Latinos, it is argued that they are able to sustain ethnic enclaves.49 These ethnic enclaves can (1) provide residents with social, economic, and cultural resources that might buffer the negative effects of discrimination; and (2) lower exposure to mainstream individuals, thus limiting experiences or perceptions of discrimination.50 By contrast, the middle class among other Latinos is not large enough to sustain ethnic enclaves51; Puerto Ricans are the most segregated with the highest levels of poverty.52 Interestingly, our study found that for Mexicans and Puerto Ricans, discrimination was associated with an increased risk of substance use disorders, whereas for Cubans, discrimination was associated with a decreased risk of alcohol use disorders. These differences could be reflective of the additional resources Cubans might have to cope with discrimination that other Latinos, such as Mexicans and Puerto Ricans, might not possess. The majority of Latino health research has focused on Mexicans, because of their large sample sizes, but a growing body of research has indicated that Puerto Ricans tend to differ in terms of health outcomes and experiences of discrimination from Mexicans.29,46 However, our findings revealed that the relationship between discrimination and substance use disorders was similar for Mexicans and Puerto Ricans, as well as other Latinos.
Limitations
Our study highlighted the need to consider how the relationship between discrimination and substance use disorders varied among Latinos, yet several limitations should be noted. The first was that NESARC included questions on discrimination in wave 2; thus, our study was a cross-sectional study that could not assess causality. Because both measures of discrimination and substance use disorders could have occurred at any time during the respondents’ life course, future studies that assess the temporal order between experiences of stress and discrimination, and onset of substance use disorders, are warranted. In addition, studies that assess the bidirectional relationship between discrimination and substance use disorders would be helpful, because most previous studies focused on either (1) the pathway from discrimination attributed to a minority status (e.g., racial/ethnic, gender) to substance use disorders, or (2) the pathway from substance use disorders to discrimination or stigma that is attributed to having a disorder.
Given the cross-sectional design of our study, another limitation applies to foreign-born Latinos, because both discrimination and substance use disorders could have occurred before migration to the United States. Future studies should consider how the relationship between discrimination and substance use disorders differs by age at immigration and years lived in the United States.
A third limitation was that Cubans had a lower prevalence of substance use disorders and reported lower levels of discrimination compared with all other Latinos. Their small cell size (n = 325) might have affected our findings. Future research is necessary to determine if and how the relationship between discrimination and substance use disorders might differ for Cubans compared with other Latinos.
Conclusions
Discrimination and substance use are both social experiences53 that are becoming more common for Latinos.54 The rise in legislation that disproportionately targets Latinos and encourages law enforcement to stop individuals who “look undocumented”55 creates a hostile atmosphere in which Latinos are devalued by society and negative stereotypes are reinforced. The harmful health effects of discrimination should be considered when developing interventions aimed at preventing and treating substance use disorders among Latinos, because discrimination is rarely considered. At the interpersonal level, culturally competent practices, such as race/ethnicity matching, might not only assist in treatment retention,2,56 but also help individuals feel more comfortable discussing discriminatory experiences, providing an alternative method for coping and building resilience. Similarly, promotores (community health workers) with shared lived experiences of substance use and discrimination might also strengthen prevention and treatment programs. At the institutional level, drug policies and immigration policies might be interpreted as discriminatory, reinforcing ideologies that foster discrimination13,57–59; therefore, such policies should be re-evaluated. By contrast, policies that encourage the reintegration of individuals who have been incarcerated could work against these ideologies. When tailoring interventions focused on Latinos, it is important to determine which subgroups among Latinos might be particularly vulnerable to the negative effects of discrimination so that interventions are tailored accordingly. Taken together, our study showed that, despite differences in prevalence of substance use disorders and reports of discrimination, discrimination burdens the health and well-being of all Latinos.
Acknowledgments
This project was supported by the National Institutes of Health Ruth L. Kirschstein National Research Service Award (5T32DA007272-20).
We want to acknowledge Nipa Warda for guidance on analysis and Kris Langabeer for commenting on a draft of our article.
Human Participant Protection
This research was declared exempt from University of California, Los Angeles Institutional Review Board.
References
- 1. Centers for Disease Control and Prevention. Hispanic or Latino Populations. Available at: http://www.cdc.gov/minorityhealth/populations/REMP/hispanic.html. Accessed February 6, 2014.
- 2.Guerrero EG, Marsh JC, Khachikian T, Amaro H, Vega WA. Disparities in Latino substance use, service use, and treatment: implications for culturally and evidence-based interventions under health care reform. Drug Alcohol Depend. 2013;133(3):805–813. doi: 10.1016/j.drugalcdep.2013.07.027. [DOI] [PubMed] [Google Scholar]
- 3.Delgado M. Latinos and Alcohol Use/Abuse Revisited: Advances and Challenges for Prevention and Treatment Programs. New York, NY: Haworth Press; 2005. [Google Scholar]
- 4.Amaro H, Iguchi MY. Opportunities in Hispanic drug abuse research. Drug Alcohol Depend. 2006;84(suppl 1):S1–S3. doi: 10.1016/j.drugalcdep.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 5.Gil AG, Vega WA. Latino drug use. In: Aguirre-Molina M, Molina CW, Zambrana RE, editors. Health Issues in the Latino Community. San Francisco, CA: Jossey Bass Publishers; 2001. pp. 435–458. [Google Scholar]
- 6.Otiniano Verissimo AD, Gee GC, Ford CL, Iguchi MY. Racial discrimination, gender discrimination, and substance abuse among Latina/os nationwide. Cultur Divers Ethnic Minor Psychol. 2014;20(1):43–51. doi: 10.1037/a0034674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ornelas IJ, Hong S. Gender differences in the relationship between discrimination and substance use disorder among Latinos. Subst Use Misuse. 2012;47(12):1349–1358. doi: 10.3109/10826084.2012.716482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ortiz-Hernández L, Tello BL, Valdes J. The association of sexual orientation with self-rated health, and cigarette and alcohol use in Mexican adolescents and youths. Soc Sci Med. 2009;69(1):85–93. doi: 10.1016/j.socscimed.2009.03.028. [DOI] [PubMed] [Google Scholar]
- 9.Kulis S, Marsiglia FF, Nieri T. Perceived ethnic discrimination versus acculturation stress: influences on substance use among Latino youth in the Southwest. J Health Soc Behav. 2009;50(4):443–459. doi: 10.1177/002214650905000405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Okamoto J, Ritt-Olson A, Soto D, Baezconde-Garbanati L, Unger JB. Perceived discrimination and substance use among Latino adolescents. Am J Health Behav. 2009;33(6):718–727. doi: 10.5993/ajhb.33.6.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ornelas IJ, Eng E, Perreira KM. Perceived barriers to opportunity and their relation to substance use among Latino immigrant men. J Behav Med. 2011;34(3):182–191. doi: 10.1007/s10865-010-9297-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Basáñez T, Unger JB, Soto D, Crano W, Baezconde-Garbanati L. Perceived discrimination as a risk factor for depressive symptoms and substance use among Hispanic adolescents in Los Angeles. Ethn Health. 2013;18(3):244–261. doi: 10.1080/13557858.2012.713093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Otiniano Verissimo AD, Gee GC, Iguchi MY, Ford CL, Friedman SR. Discrimination, drugs, and alcohol among Latina/os in Brooklyn, New York: differences by gender. Int J Drug Policy. 2013;24(4):367–373. doi: 10.1016/j.drugpo.2013.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Borrell LN, Kiefe CI, Diez-Roux AV, Williams DR, Gordon-Larsen P. Racial discrimination, racial/ethnic segregation, and health behaviors in the CARDIA study. Ethn Health. 2013;18(3):227–243. doi: 10.1080/13557858.2012.713092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hunte HE, Barry AE. Perceived discrimination and DSM-IV-based alcohol and illicit drug use disorders. Am J Public Health. 2012;102(12):e111–e117. doi: 10.2105/AJPH.2012.300780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2003;93(2):200–208. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adler NE, Stewart J. Health disparities across the lifespan: meaning, methods, and mechanisms. Ann N Y Acad Sci. 2010;1186:5–23. doi: 10.1111/j.1749-6632.2009.05337.x. [DOI] [PubMed] [Google Scholar]
- 18.Ridgeway C. The social construction of status value: gender and other nominal characteristics. Soc Forces. 1991;70(2):367–386. [Google Scholar]
- 19.Ro AE, Choi KH. Social status correlates of reporting gender discrimination and racial discrimination among racially diverse women. Women Health. 2009;49(1):1–15. doi: 10.1080/03630240802694756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Canino G, Vega WA, Sribney WM, Warner LA, Alegria M. Social relationships, social assimilation, and substance use disorders among adult Latinos in the US. J Drug Issues. 2008;38(1):69–101. doi: 10.1177/002204260803800104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Borrell LN, Diez Roux AV, Jacobs DR, Jr et al. Perceived racial/ethnic discrimination, smoking and alcohol consumption in the Multi-Ethnic Study of Atherosclerosis (MESA) Prev Med. 2010;51(3-4):307–312. doi: 10.1016/j.ypmed.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pérez DJ, Fortuna L, Alegría M. Prevalence and correlates of everyday discrimination among US Latinos. J Community Psychol. 2008;36(4):421–433. doi: 10.1002/jcop.20221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cooper ML, Russell M, Skinner JB, Frone MR, Mudar P. Stress and alcohol use: moderating effects of gender, coping, and alcohol expectancies. J Abnorm Psychol. 1992;101(1):139–152. doi: 10.1037//0021-843x.101.1.139. [DOI] [PubMed] [Google Scholar]
- 24.Lindquist TL, Beilin LJ, Knuiman MW. Influence of lifestyle, coping, and job stress on blood pressure in men and women. Hypertension. 1997;29(1 Pt 1):1–7. doi: 10.1161/01.hyp.29.1.1. [DOI] [PubMed] [Google Scholar]
- 25.Ptacek JT, Smith RE, Zanas J. Gender, appraisal, and coping: a longitudinal analysis. J Pers. 1992;60(4):747–770. [Google Scholar]
- 26.Amaro H, Nieves R, Johannes SW, Labault Cabeza NM. Substance abuse treatment: critical issues and challenges in the treatment of Latina women. Hisp J Behav Sci. 1999;21(3):266–282. [Google Scholar]
- 27.Alegria M, Shrout PE, Woo M et al. Understanding differences in past year psychiatric disorders for Latinos living in the US. Soc Sci Med. 2007;65(2):214–230. doi: 10.1016/j.socscimed.2007.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gee GC, Ryan A, Laflamme DJ, Holt J. Self-reported discrimination and mental health status among African descendants, Mexican Americans, and other Latinos in the New Hampshire REACH 2010 initiative: the added dimension of immigration. Am J Public Health. 2006;96(10):1821–1828. doi: 10.2105/AJPH.2005.080085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morales LS, Lara M, Kington RS, Valdez RO, Escarce JJ. Socioeconomic, cultural, and behavioral factors affecting Hispanic health outcomes. J Health Care Poor Underserved. 2002;13(4):477–503. doi: 10.1177/104920802237532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith SM, Stinson FS, Dawson DA, Goldstein R, Huang B, Grant BF. Race/ethnic differences in the prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2006;36(7):987–998. doi: 10.1017/S0033291706007690. [DOI] [PubMed] [Google Scholar]
- 31.McLaughlin KA, Hatzenbuehler ML, Keyes KM. Responses to discrimination and psychiatric disorders among Black, Hispanic, female, and lesbian, gay, and bisexual individuals. Am J Public Health. 2010;100(8):1477–1484. doi: 10.2105/AJPH.2009.181586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grant BF, Goldstein RB, Chou SP et al. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol Psychiatry. 2009;14(11):1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grant BF, Moore TC, Shepard J, Kaplan K. Source and Accuracy Statement: Wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. [Google Scholar]
- 34.Grant BF, Stinson FS, Hasin DS, Dawson DA, Chou SP, Anderson K. Immigration and lifetime prevalence of DSM-IV psychiatric disorders among Mexican Americans and non-Hispanic whites in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(12):1226–1233. doi: 10.1001/archpsyc.61.12.1226. [DOI] [PubMed] [Google Scholar]
- 35.Keyes KM, Martins SS, Hatzenbuehler ML, Blanco C, Bates LM, Hasin DS. Mental health service utilization for psychiatric disorders among Latinos living in the United States: the role of ethnic subgroup, ethnic identity, and language/social preferences. Soc Psychiatry Psychiatr Epidemiol. 2012;47(3):383–394. doi: 10.1007/s00127-010-0323-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grant BF, Dawson DA, Hasin DS. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2001. [Google Scholar]
- 37.Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA study of young black and white adults. Am J Public Health. 1996;86(10):1370–1378. doi: 10.2105/ajph.86.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med. 2005;61(7):1576–1596. doi: 10.1016/j.socscimed.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 39.Blanco C, Morcillo C, Alegria M et al. Acculturation and drug use disorders among Hispanics in the US. J Psychiatr Res. 2013;47(2):226–232. doi: 10.1016/j.jpsychires.2012.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Marin G, Sabogal F, Marin BV, Otero-Sabogal R, Perez-Stable EJ. Development of a short acculturation scale for Hispanics. Hisp J Behav Sci. 1987;9(2):183–205. [Google Scholar]
- 41.Ruan WJ, Goldstein RB, Chou SP et al. The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92(1-3):27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 43.StataCorp. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP; 2013. [Google Scholar]
- 44.Lemle R, Mishkind ME. Alcohol and masculinity. J Subst Abuse Treat. 1989;6(4):213–222. doi: 10.1016/0740-5472(89)90045-7. [DOI] [PubMed] [Google Scholar]
- 45.Wagner FA, Anthony JC. Male–female differences in the risk of progression from first use to dependence upon cannabis, cocaine, and alcohol. Drug Alcohol Depend. 2007;86(2–3):191–198. doi: 10.1016/j.drugalcdep.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 46.Araujo BY, Borrell LN. Understanding the link between discrimination, mental health outcomes, and life chances among Latinos. Hisp J Behav Sci. 2006;28(2):245–266. [Google Scholar]
- 47.Gee GC, Walsemann KM, Brondolo E. A life course perspective on how racism may be related to health inequities. Am J Public Health. 2012;102(5):967–974. doi: 10.2105/AJPH.2012.300666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Potochnick SR, Perreira KM. Depression and anxiety among first-generation immigrant Latino youth: key correlates and implications for future research. J Nerv Ment Dis. 2010;198(7):470–477. doi: 10.1097/NMD.0b013e3181e4ce24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vega WA, Amaro H. Latino outlook: good health, uncertain prognosis. Annu Rev Public Health. 1994;15:39–67. doi: 10.1146/annurev.pu.15.050194.000351. [DOI] [PubMed] [Google Scholar]
- 50.Viruell-Fuentes EA. Beyond acculturation: immigration, discrimination, and health research among Mexicans in the United States. Soc Sci Med. 2007;65(7):1524–1535. doi: 10.1016/j.socscimed.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 51.Orfield M. American Metropolitics: The New Suburban Reality. Washington, D.C: Brookings Institution Press; 2002. [Google Scholar]
- 52.South SJ, Crowder K, Chavez E. Exiting and entering high-poverty neighborhoods: Latinos, Blacks and Anglos compared. Soc Forces. 2005;84(2):873–900. [Google Scholar]
- 53.Umberson D, Crosnoe R, Reczek C. Social relationships and health behavior across the life course. Annu Rev Sociol. 2010;36(1):139–157. doi: 10.1146/annurev-soc-070308-120011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Warner LA, Valdez A, Vega WA, de la Rosa M, Turner RJ, Canino G. Hispanic drug abuse in an evolving cultural context: an agenda for research. Drug Alcohol Depend. 2006;84(suppl 1):S8–S16. doi: 10.1016/j.drugalcdep.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 55.Lacayo A. One year later: a look at SB 1070 and copycat legislation. National Council of La Raza. 2011. Available at: http://www.nclr.org/index.php/publications/one_year_later_a_look_at_sb_1070_and_copycat_legislation. Accessed December 3, 2013.
- 56.Guerrero EG, Campos M, Urada D, Yang J. Do cultural and linguistic competence matter in Latinos’ completion of mandated substance abuse treatment? Subst Abuse Treat Prev Policy. 2012;7(1):34–40. doi: 10.1186/1747-597X-7-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Iguchi MY, Bell J, Ramchand RN, Fain T. How criminal system racial disparities may translate into health disparities. J Health Care Poor Underserved. 2005;16(4, suppl B):48–56. doi: 10.1353/hpu.2005.0114. [DOI] [PubMed] [Google Scholar]
- 58.Viruell-Fuentes EA, Miranda PY, Abdulrahim S. More than culture: structural racism, intersectionality theory, and immigrant health. Soc Sci Med. 2012;75(12):2099–2106. doi: 10.1016/j.socscimed.2011.12.037. [DOI] [PubMed] [Google Scholar]
- 59.Alexander M. The New Jim Crow: Mass Incarceration in the Age of Colorblindness. New York, NY: The New Press; 2012. [Google Scholar]