Abstract
This study was undertaken to determine the prevalence of Chlamydia trachomatis, Mycoplasmas, and Ureaplasmas in semen samples of the male partners of infertile couples and to investigate whether Chlamydia trachomatis could initiate apoptosis in human spermatozoa. A total of 85 males partners of infertile couples undergoing routine semen analysis according to World Health Organization guidelines were included. Specimens were examined for the presence of Chlamydia trachomatis, Neisseria gonorrhoeae, Mycoplasma hominis, Mycoplasma genitalium, Ureaplasma urealyticum and Ureaplasma parvum by Real time PCR (qPCR). Semen specimens were analysed for the appearance of apoptotic markers (sperm DNA fragmentation, activated caspase 3 levels, mitochondrial membrane potential (ΔΨm)) using flow cytometry. C. trachomatis, N. gonorrhoeae, U. urealyticum, M genitalium were detected in semen samples of 13 (15.2%), 5 (5.8%), 5 (5.8%) and 3 (3.5%) male partners of infertile couples, respectively. M. hominis and U. parvum were detected in semen sample of only one patient (1.1%). The semen of infertile men positive for C. trachomatis showed lower mean of semen count and lower rapid progressive motility (category [a]) of spermatozoa compared to uninfected men with statistically significances (p = 0.02 and p = 0.04, respectively). Flow cytometry analyses demonstrated a significant increase of the mean rate of semen with low ΔΨm and caspase 3 activation of infertile men positive for C. trachomatis compared to uninfected men (p = 0.006 and p = 0.001, respectively). DNA fragmentation was also increased in sperm of infertile men positive for C. trachomatis compared to uninfected men but without statistical significances (p = 0.62). Chlamydial infection was associated to loss of ΔΨm and caspase 3activation. Thus, C. trachomatis infection could be incriminated in apoptosis induction of spermatozoa. These effects may explain the negative direct impact of C. trachomatis infection on sperm fertilizing ability.
Introduction
Sexually transmitted infections are of major concern to researchers and clinicians in the field of reproductive medicine. It is estimated that 15% of male infertility is related to genital tract infection [1]. Men can harbor subclinical infections in the genital tract over extended periods of time and several sexually transmitted infection pathogens, such as C. trachomatis have been detected in semen from asymptomatic men [2]. According to a World Health Organization (WHO) [3] report, C. trachomatis is responsible for the most common sexually transmitted bacterial infection worldwide, affecting more than 90 million people and has been known for some time to have a significant effect on human reproduction [4]. The role of C. trachomatis infections in male infertility is controversial [5]–[6]. A number of studies have specifically looked at the relationship between Chlamydial infection and semen quality. While some authors have shown that C. trachomatis infection is associated with poor semen quality [7]–[8], others have claimed that it does not [9]–[10]. Some reports indicated that C. trachomatis infection is associated with a decrease in sperm concentration and motility and also with altered semen pH and reduced volume of the ejaculate [11], [12], [13]–[14]. Conversely, other studies have revealed no association between C. trachomatis infection of the male genital tract and altered sperm quality [9], [15], [16], [17], [18], [19], [20]–[21]. In summary, the available evidence is conflicting and still makes it impossible to establish a clear relationship between C. trachomatis infection and semen quality.
The apoptotic mode of cell death is an active and defined process which plays an important role in the development of multicellular organisms and in the regulation and maintenance of the cell populations in tissues upon physiological and pathological conditions [22]. Apoptosis markers characterized in somatic cells were noted in human spermatozoa in several studies. These include, principally, plasma membrane externalization of phosphatidylserine (PS) and DNA fragmentation. Such markers are observed with higher frequency in ejaculates of infertile men compared with fertile controls [23]–[24]. In addition, key components of the somatic cell apoptosis pathways, such as presence and activation of caspases, have been described in purified populations of ejaculated sperm from the high and low-motility fractions [24]–[25]. Moreover, mitochondria play a major role in the control of apoptosis [26]. Marchetti et al (2002) demonstrated that analysis of ΔΨm is a sensitive test to determine sperm quality when compared with the analysis of the basic sperm parameters, generation of reactive oxygen species, and presence of DNA fragmentation [27]. Several in vitro and in vivo studies tried to establish a relationship between apoptosis markers in spermatozoa and Chlamydial infection. In vitro, some authors have demonstrated that C. trachomatis is able to interact with sperm cells, affecting their function and inducing apoptosis [28], [29]–[30]. Apoptosis of human sperm can be induced by in vitro incubation of human sperm cells with Chlamydial LPS, which has a 550 fold greater spermicidal activity than Escherichia coli LPS [31]–[32]. In addition, C. trachomatis serovar E can attach to human spermatozoa and influence its function leading to premature capacitation [33]. It has been shown that Chlamydial LPS interact with CD14 on the sperm surface, thus leading to increased production of reactive oxygen species and resulting in caspase-mediated apoptosis [29]. Despite all this in vitro studies, a clear association between C. trachomatis and sperm damage has not yet been corroborated by in vivo studies. Gallegos et al (2008) reported that patients with C. trachomatis and Mycoplasmas genitourinary infections have increased sperm DNA fragmentation in comparison with fertile controls [34]. Lastly, we showed that inoculation of fertile male Swiss mice in the meatus urethra with C. trachomatis could lead to alteration of semen parameters, induction of apoptosis in spermatozoa, and decrease of the reproductive performance of male mice [35]. Taken together, these data support a role of C. trachomatis in sperm apoptosis induction. However, most studies indicate that apoptosis-inducing mechanism is unknown.
In the present Study, we aimed to determine the prevalence of C. trachomatis, Mycoplasmas, and Ureaplasmas in semen samples of the male partners of infertile couples and mainly to investigate whether C. trachomatis could initiate apoptosis in human spermatozoa.
Materials and Methods
Subjects
A total of 85 infertile men attending obstetrics and gynecology clinics in Sfax (South of Tunisia) for diagnostic semen analysis were selected to the study. All men were undergoing semen analysis as part of a work-up for infertility investigations after failing to conceive with their partner after one year of unprotected intercourse. The mean duration of infertility was 4 years (range 1–15). The mean age of patients was 36.7 years (range 23–57). This study was approved by our institutional review board “Habib Bourguiba University hospital ethics committee” with the given number 8–12. All subjects signed a written informed consent. Consent form was also approved by our ethic committee
Sperm seminological variables
Prior to semen analysis, the men were asked to abstain from sexual intercourse or masturbation for 3–5 days before attending the clinic. All samples for analysis were produced on site and collected into standard containers that had previously been shown not to have any cytotoxic effects on human spermatozoa according to the methods outlined by WHO. Immediately after semen production, samples were placed in an incubator and liquefied at 37°C for up to 30 minutes before analysis. Semen analysis was performed according to the WHO criteria [36] to determine the following variables: sperm concentration, vitality, total progressive motility (category [a+b]), rapid progressive motility (category [a]) Peroxidase staining, a practical and reliable method recommended by WHO [36] for determining leukocytes in the semen, was employed to count and differentiate leukocytes (white blood cells) from immature germ cells. Leukocytospermia was indicated by a concentration of leukocytes ≥106/ml.
Spermiocultures analysis
Samples were seeded quantitatively using a calibrated loop on agar plates: blood agar, chocolate agar with isovitalex (1%) incubated in 5% CO2 at 37°C for 48 hours. Microorganisms were identified by Gram staining and Bio-Mérieux Api systems (Bio-Mérieux, Marcy l'Etoile, France).
Spermiocultures were considered positive when the number of colonies was ≥104 CFU ml−1 in case of Gram positive cocci and ≥105 CFU ml−1 in case of Gram negative rods.
Bacterial quantification in semen specimens by qPCR
For each male patient, 200 µl of semen specimens were used for bacterial quantification by Real time PCR.
Extraction of DNA by Cetyltrimethylammonium bromide (CTAB)-phenol-chloroform/isoamyl alcohol method
The precipitates from each 200 µl of semen specimens were harvested by centrifugation at 14,000 g for 20 minutes. The precipitates were treated with 5 µl of proteinase K (20 mg/ml) at 55°C for 2 h in 600 µl of digestion buffer (30 µl of 10% sodium dodecyl sulphate and 570 µl of TE buffer [10 mM Tris-HC1 (pH: 8), 1 mM EDTA]).
After homogenisation, the samples were incubated in a solution of CTAB-NaCl (100 µl of 5 M NaCl and 80 µl of 10% CTAB) for 10 minutes at 65°C, and then mixed with 750 µl of chloroform-isoamyl alcohol (24∶1 [vol/vol]) and centrifuged for 15 minutes at 14,000 g in an Eppendorf centrifuge. The aqueous phase was separated, mixed with 750 µl of phenol chloroform/isoamyl alcohol (25∶24∶1 [vol/vol/vol]) and centrifuged for 15 minutes at 14,000 g in an Eppendorf centrifuge. The obtained aqueous phase was mixed with an equal volume of isopropanol.
The samples were left at −80°C for 1 h and then centrifuged for 15 minutes at 14,000 g. The DNA pellet was washed up once with 70% ethanol, air dried, and dissolved in a final volume of 100 µl of TE buffer.
Primers and probes for Qpcr
Initially, the extracted DNA was tested for human β-globin gene to check that there were no PCR inhibitors in the samples. Primers β-GPCO (5′-ACACAACTGTGTTCACTAGC- 3′) and β-GPCPO (5′-GAAACCCAAGAGTCTTCTCT- 3′) were used to amplify a 209-bp fragment of the human β-globin gene [37]. Samples found to be negative by PCR for β-globin were retested after dilution 10-fold in distilled water. Samples shown to be β-globin positive were then examined for bacterial quantification by Real time PCR.
The real-time PCR assay was performed on a CFX96™ real-time PCR cycler (Biorad, USA) in a 20 µl final volume with Ex Taq Premix Tli RNaseH Plus (Takara, Japan). A pair of primers and a labeled probe in the TaqMan format was used to amplify: 149 bp region of Cryptic plasmid for C. trachomatis, 80 bp of MgPa region of Adhesin gene for M. genitalium, 101 bp region of the 16 S rRNA-encoding gene for M. hominis, 101 bp region of Por A pseudogene for N. gonorrhoeae and 146 bp of the Urease gene of U. parvum and U. urealyticum.
Real-time PCR included initial denaturation at 95°C for 2 min, followed by 40 cycles of 95°C for 30 s and annealing temperature according to microorganisms for 30 s (C. trachomatis 60°C, M. genitalium, M. hominis and N. gonorrhoeae 55°C, U. parvum and U. urealyticum 50°C).
In all experiments, each PCR run included a negative extraction control (sterile water) and a negative PCR control, containing 5 µl Diethylpyrocarbonate (DEPC) treated H2O instead of DNA extract, to detect any possible contaminating DNA. Samples and controls were run in duplicate.
Positive recombinant plasmid control
To facilitate bacterial quantification, a plasmid containing the target gene for all bacteria was constructed.
DNA was extracted from C. trachomatis, N. gonorrhoeae, M. genitalium, M. hominis, U. parvum and U. urealyticum references strains and the target sequence for all genes selected for Real Time PCR were amplified with the same primers in (Table 1).
Table 1. Primers and probes used for detection and quantification of C. trachnomatis, N. gonorrhoeae. U. urealyticum, M. genitalium, U. parvum and M. hominis by qPCR.
| Bacteria | Primers and probes | Oligonucleotide sequence (5′→3′) | Target gene | Product size (bp) | Ref |
| C. trachnomatis | Forward | AACCAAGGTCGATGTGATAG | Cryptic plasmid | 149 | [73] |
| Reverse | TCAGATAATTGGCGATTCTT | ||||
| Probe | ROX-CGAACTCATCGGCGATAAGG- BHQ2 | ||||
| N. gonorrhoeae | Forward | CCGGAACTGGTTTCATCTGATT | PorA | 101 | [74] |
| Reverse | GTTTCAGCGGCAGCATTCA | ||||
| Probe | FAM-CGTGAAAGTAGCAGGCGTATAGGCGGACTT-BHQ1 | ||||
| M. genitalium | Forward | GAGAAATACCTTGATGGTCAGCAA | MgPa | 80 | [75] |
| Reverse | GTTAATATCATATAAAGCTCTACCGTTGTTATC | ||||
| Probe | HEX-ACTTTGCAATCAGAAGGT-BHQ1 | ||||
| M. hominis | Forward | TTTGGTCAAGTCCTGCAACGA | 16S rRNA-encodinggene | 101 | [76] |
| Reverse | CCCCACCTTCCTCCCAGTTA | ||||
| Probe | ROX-TACTAACATTAAGTTGAGGACTCTA-BHQ1 | ||||
| U. urealyticum | Forward | CATTGATGTTGCACAAGGAG | Urease (UreD Subunit) | 146 | [77] |
| Reverse | CGTGATTTTAATGTATCGGCTTTC | ||||
| Probe | FAM TTGACCACCCTTACGAG BHQ1 | ||||
| U. parvum | Forward | CATTGATGTTGCACAAGGAG | Urease (UreD Subunit) | 147 | [77] |
| Reverse | CGTGATTTTAATGTATCGGCTTTC | ||||
| Probe | Hex TTGTCCGCCTTTACGAG BHQ1 |
The final 25 µl reaction mixture contained 1X PCR buffer (Promega, Lyon, France), 0.2 mM each primer, 0.2 mM each dNTP, 2.5 mM MgCl2, 1.25 U Go Taq DNA polymerase (Promega), and 5 µL of DNA extract. PCR was performed in Gene-Amp PCR System 9700 (Applied Biosystems, Foster City, California) according to the following procedure: 4 min at 95°C, 35 cycles at 95°C for 30 s, 55°C for 1 min, 72°C for 20 min. PCR products were then purified with QIAquick Gel Extraction Kit (Qiagen) and cloned into a vector using a cloning kit (pGEM-T vector; Promega, Madison, WI, USA), in accordance with the manufacturer's instructions. Isolation of recombinant plasmid DNA was performed using the QIAprepSpin Miniprep kit (Qiagen), and the presence of the correct insert was confirmed by sequencing using the commercial BigDye Terminator v3.1 kit (Applied Biosystems) on a 3730XL sequencer (Applied Biosystems). The obtained sequences were processed by the ABI 3100 Genetic Analyzer and were compared with the sequences available in GenBank by using the BLAST server from the NCBI website (http://www.ncbi.nlm.nih.gov/BLAST). Plasmids were then linearized and quantified with a NanoDrop ND-1000 Spectrophotometer. Copy numbers of the cloned gene was calculated using the following equation reported by [38] to generate standards ranging from 1 to 106 molecules and stored at −20°C.
Evaluation of Viability of sperm using 7-amino-actinomycin-D Dye
The percentage of dead sperms cells (cells with 7-AAD positive) and viable sperm cells (cells with 7-AAD negative) were assessed using 7-AAD Dye. 7-AAD penetrates only dead cells. From each sperm sample, 1 ml of a sperm solution in PBS containing 2×106cells/ml was stained with 10 µl of 7-amino-actinomycin-D (7-AAD) (Immunotech, a Beckman Coulter Company, Marseille–France). The samples were incubated in the dark at room temperature for 20 minutes before flow cytometric analysis. After the incubation period, 1 ml PBS was added and the sample was analyzed by flow cytometry.
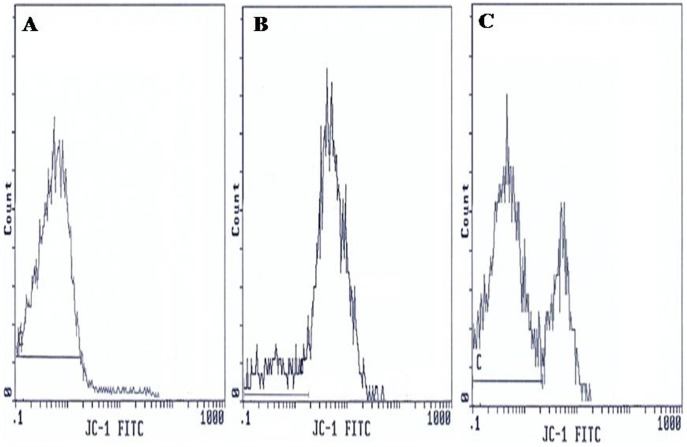
Evaluation of Mitochondrial Membrane Potential (ΔΨm)
JC-1 possesses the unique ability to differentially label mitochondria with low and high ΔΨm. In mitochondria with high ΔΨm, JC-1 forms multimeric aggregates that emit in the high orange wavelength of 590 nm when excited at 488 nm. In mitochondria with low ΔΨm, JC-1 forms monomers; these monomers emit in the green wavelength (525–530 nm) when excited at 488 nm.
The ΔΨm was analyzed using MitoProbe JC-1 Assay kit (Molecular Probes, Eugene, OR). For staining, 2 µM stock solution of JC-1 in dimethylsulfoxide (DMSO) was prepared. From each sperm sample, 1 ml of a sperm solution in PBS containing 2×106cells/ml was stained with 10 µl of JC-1 stock solution. The samples were incubated at 37°C in the dark for 20 minutes before flow cytometric analysis. In this way, 2 sperm subpopulations were identified:
Represented spermatozoa with high ΔΨm (orange fluorescence).
Represented spermatozoa with low ΔΨm (green fluorescence).
As suggested by the protocol, in order to confirm the JC-1 sensitivity to changes in membrane potential, carbonylcyanide 3-chlorophenylhydrazone (CCCP = 50 µM final concentration) was used as membrane potential disruptor (negative control).
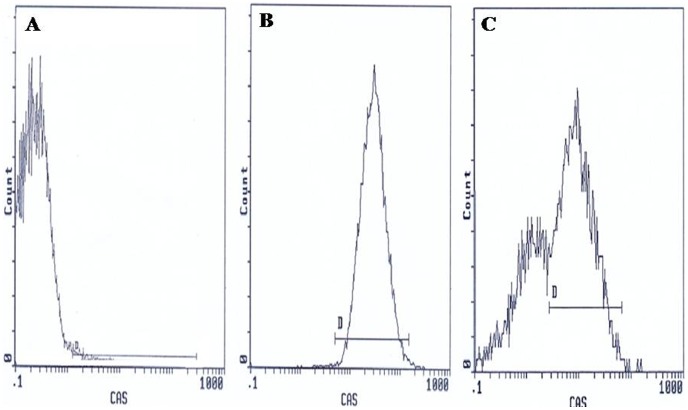
Flow cytometric detection of activated caspase 3
Activated Caspase 3 levels were detected in spermatozoa using fluorescein- labeled inhibitor of caspases (FLICA), which is cell permeable, non cytotoxic, and binds covalently to active Caspase 3. The inhibitor was used with the appropriate controls according to the kit instructions provided by the manufacturer (Carboxyfluorescein FLICA Apoptosis Detection Kit, AbCys, France). Briefly, 3.106 sperm were resuspended in 300 µl PBS. A 150-fold stock solution of the inhibitor was prepared by dissolving the lyophilized caspase-inhibitor in 50 µl dimethyl sulfoxide (DMSO) and was further diluted 1∶5 in PBS to yield a 30-fold working solution (per aliquot: 2 µl of the stock solution plus 8 µl PBS). All test aliquots and controls (with 300 µl PBS) were incubated at 37°C in the dark for 1 h with 10 µl of the working solution. Sperm samples were then washed resuspended in 400 µl of Wash Buffer and kept in ice until flow cytometry analysis.
A negative control (sample with 300 µl PBS) and a positive control (sample treated with 10 µM H2O2 for 1 hour at 37°C) were used in all experiments.
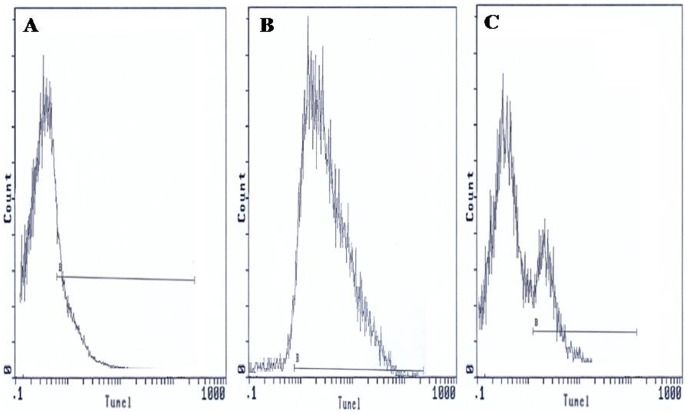
TUNEL assay
For the evaluation of DNA fragmentation, a commercial kit (In situ Cell Death Detection Kit, Fluorescein, Takara, Japon) based on an enzymatic reaction of labelling free 3′-OH termini was used. In brief, 3.106 cells were washed with phosphate- buffered saline (1xPBS, pH 7.4) then fixed with 200 µl of 4% paraformaldehyde for 1 h at room temperature in the dark. After wards, sperm cells were washed with 1xPBS and permeabilised using 0.1% Triton X-100 in 0.1% sodium citrate for 15 min on ice. After washing with PBS, sperm DNA was labelled by incubating spermatozoa with 50 µl of the TUNEL reaction mixture (Tdt enzyme and FITC-labelled nucleotides) in a humidified atmosphere for 60 min at 37°C in the dark, with mixing each 15 min. Washed and labelled sperm cells were then resuspended in 1xPBS for flow cytometry analysis. A negative control (sample without the addition of Tdt enzyme) and a positive control (sample treated with DNase I (3 U/ml, Invitrogen) for 10 min at room temperature to generate DNA strand breaks) were also assessed by TUNEL assay.
Flow Cytometry and data analyses
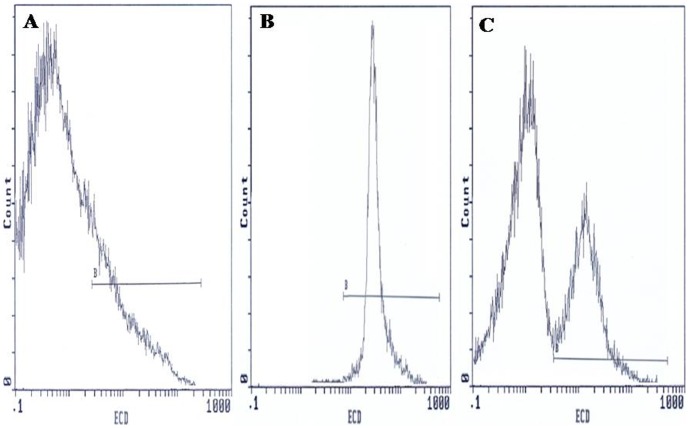
Flow cytometric analysis was carried out using an EPICS XL flow cytometer (Beckman Coulter) equipped with a 15mW argon-ion laser for excitation at 488 nm. At least 10,000 events per sample were analysed. Light-scattering and fluorescence data were obtained at a flexed gain setting in logarithmic mode. Debris was excluded by establishing a region around the population of interest on the basis of light scatter characteristics (forward-angle light scatter (FSC) vs. side-angle light scatter (SSC). The percentage of labelled sperm was characterized by identifying a region that included >90% of events in the frequency histogram of the positive controls both in the assessments of Viability, ΔΨm, Caspase 3 activation and DNA fragmentation. Data were expressed as percentage of stained cells from histograms using System II software. Typical examples of histograms obtained by flow cytometry for the detection of fluorescence are shown in Figure 1 (sperm viability), Figure 2 (ΔΨm), Figure 3 (Caspase 3 activation) and Figure 4 (TUNEL assay).
Figure 1. Flow cytometric of sperm viability using 7-amino-actinomycin-D Dye.
Histograms show: (A) Negative control with 10% 7-AAD positive cells. (B) Positive control with 98.5% 7-AAD positive cells. (C) Semen sample of one male partner of infertile couples positive for C. trachomatis qPCR with 56.5% 7-AAD negative cells and 43.5% 7-AAD positive cells. B: window adjusted to detect the percentage of cells with 7-AAD positive.
Figure 2. Flow cytometric of changes in the mitochondrial membrane potential (ΔΨm).
Histograms show: (A) Negative control with 95.8% low ΔΨm cells. (B) Positive control with 9.6% low ΔΨm cells. (C) Semen sample of one male partner of infertile couples positive for C. trachomatis qPCR with 32.5% low ΔΨm cells and 67.5% with high ΔΨm cells. C: window adjusted to detect the percentage of cells with low ΔΨm.
Figure 3. Flow cytometric caspase 3 detection histograms.
(A) Negative control with 0.85% FITC labelled cells. (B) Positive control with 95.8% FITC labelled cells. (C) Semen sample of one male partner of infertile couples positive for C. trachomatis qPCR with 32.5% FITC labelled cells. D: window adjusted to detect the percentage of cells exhibiting caspase 3 activation.
Figure 4. TdT (terminal deoxynucleotidyl transferase)-mediated dUTP nick-end labeling (TUNEL) assay of spermatozoa.
Histograms show: (A) negative control with 2.35% TUNEL positive cells. (B) Positive control (spermatozoa treated with DNaseI) with 90.5% TUNEL positive cells. (C) Semen sample of one male partner of infertile couples positive for C. trachomatis qPCR with 20.5% TUNEL positive cells. B: window adjusted to detect the percentage of TUNEL positive cells.
Statistical analysis
The SPSS 18.0 software (SPSS Inc, Chicago, Ill) was used for statistical analysis. Test χ2 was used to compare frequencies. Non-parametric test (Mann-Whitney) from SPSS software was used to compare distribution sperm parameters and flow cytometry data of infected and uninfected men. Correlation between semen parameters means, ΔΨm, DNA fragmentation and caspase 3 activation and C. trachomatis infection was assessed using T-test. All tests were considered statistically significant when p<0.05.
Results
Spermiocultures analysis
Spermioculture analysis was positive in 6 cases (7%). Group B Streptococcus (GBS) was found in 3 samples (3.5%), Enterococcus spp in 1 sample (1.1%), Staphylococcus aureus in 1 sample (1.1%) and Corynebacterium spp in 1 sample (1.1%).
Frequency of urogenital bacteria in semen samples using qPCR
Among 85 semen samples, 13 (15.2%) were positive for C. trachomatis and 5 (5.8%) for N. gonorrhoeae. U. urealyticum, M. genitalium, U. parvum and M. hominis were detected in 5 patients (5.8%), 3 patients (3.5%), 1 patient (1.1%) and 1 patient (1.1%) respectively. The distribution of detected species in patients is shown in table 2.
Table 2. Frequency of urogenital bacteria detected by qPCR and spermiocultures analysis in semen samples of 85 infertile male patients.
| Species | Patients N = 85 | Frequency (%) |
| qPCR | ||
| C. trachomatis | 13 | 15.2 |
| N. gonorrhoeae | 5 | 5.8 |
| M. genitalium | 3 | 3.5 |
| M. hominis | 1 | 1.1 |
| U. urealyticum | 5 | 5.8 |
| U. parvum | 1 | 1.1 |
| Spermiocultures | ||
| Group B Streptococcus | 3 | 3.5 |
| Staphylococcus aureus | 1 | 1.1 |
| Enterococcus spp | 1 | 1.1 |
| Corynebacterium spp | 1 | 1.1 |
C. trachomatis infection and semen quality
The mean values (±SD) for semen parameters of the 85 included patients are shown in Table 3. The sperm vitality and total motility of spermatozoa in the male partners of infertile couples with C. trachomatis DNA in semen specimens were lower but not significantly that those of uninfected male partners (71.3% vs 73.3%, p = 0.65 and 41.1% vs 43.9 %, p = 0.39, respectively) (Table 3). The sperm concentration and rapid progressive motility (category a) of spermatozoa in C. trachomatis DNA positive semen were significantly lower than those of uninfected semen (41.4×106/ml vs 84.4×106/ml, p = 0.02 and 8.8% vs 12.6%, p = 0.04, respectively) (Table 3). The leukocyte count in the male partners of infertile couples with C. trachomatis DNA in semen specimens was higher but not significantly than those uninfected semen (0.8×106/ml vs 0.4×106/ml, p = 0.36) (Table 3).
Table 3. Seminological variables of semen of C. trachomatis positive patients compared to uninfected patients.
| Variables | Total Semen | Uninfected Semen | C. trachomatis positive semen | p value# |
| n = 85 | n = 57 | n = 13 | ||
| Sperm concentration (x106/ml) | 71.1±60.1 | 84.4±64.6 | 41.4±42.7 | 0.02 |
| Vitality (%) | 72.4±14.7 | 73.3±14.7 | 71.3±16.4 | 0.65 |
| Total progressive motility (category [a+b]) (%) | 41.2±12.2 | 43.9±10.6 | 41.1±10.4 | 0.39 |
| Rapid progressive motility (category [a]) (%) | 10.8±7.4 | 12.6±7 | 8.8±5.4 | 0.04 |
| Leukocyte count (x106/ml) | 0.55 ±1.4 | 0.4±1.5 | 0.8±1.2 | 0.36 |
Note: Values are means (± Standard Error).
Unless indicated, variables were tested T-Test.
Sperm viability using 7-amino-actinomycin-D Dye
Figure 1 presents frequency distribution histograms of negative control (Fig. 1A), positive control (Fig. 1B), and one semen of male partners of infertile couples positive for C. trachomatis qPCR (Fig. 1C). The percentages of viable sperm cells (cells with 7-AAD negative) were assessed in semen specimens of male partners of infertile couples positive for C. trachomatis qPCR and uninfected men. The mean proportion of viable spermatozoa (±SD) in uninfected patients was 63.2±13.9%, while it decreased to 51.3±21.13% in patients positive for C. trachomatis qPCR with a statistically significant difference (p = 0.014) (Table 4).
Table 4. 7-AAD, ΔΨm, caspase 3 activation and sperm DNA fragmentation of semen of C. trachomatis positive patients compared to uninfected men.
| Parameters | Uninfected Semen | C. trachomatis positive semen | p value# |
| n = 57 | n = 13 | ||
| Negative 7-AAD (%) | 63.2±13.9 | 51.3±21.1 | 0.014 |
| Low ΔΨm (%) | 24.5±9.7 | 33.7±13.3 | 0.006 |
| CP 3 activation (%) | 20.8±14 | 54.5±18.1 | <0.001 |
| DNA fragmentation (%) | 25.1±14.3 | 29.2±17.2 | 0.62 |
Values are means (± Standard Error).
Unless indicated, variables were tested by T-Test.
7-AAD: 7-amino-actinomycin-D.
ΔΨm: Mitochondrial membrane potential.
CP3: Caspase3.
Mitochondrial Membrane Potential (ΔΨm)
Analysis of the state of mitochondrial respiration in human spermatozoa was assessed using JC-1 to determine the ΔΨm as shown in Figure 2. Flow cytometry results are expressed as percentage of sperm cells with low ΔΨm (green fluorescence). Figure 2 presents frequency distribution histograms of negative control (Fig. 2A), positive control (Fig. 2B), and one semen of male partners of infertile couples positive for C. trachomatis qPCR (Fig. 2C). The mean percentage of spermatozoa with low ΔΨm (±SD) was higher in male partners of infertile couples positive for C. trachomatis qPCR than those of uninfected patients (33.7±13.3% vs. 24.5±9.7%) and the difference was statistically significant (p = 0.006) (Table 4).
Caspase 3 activation
The results of flow cytometry are expressed as percentage of activated caspase 3 sperm cells. Figure 3 presents frequency distribution histograms of negative control (Fig. 3A), positive control (Fig. 3B), and one semen of male partners of infertile couples positive for C. trachomatis qPCR (Fig. 3C). Mean percentage of spermatozoa with activated caspase 3 (±SD) was higher in male partners of infertile couples positive for C. trachomatis qPCR than those of uninfected patients (54.5 ±18.1% vs. 20.8±14%) and the difference was statistically significant (p = <0.001) (Table 4).
DNA fragmentation
TUNEL coupled flow cytometry results are expressed as percentage of DNA fragmented sperm cells. Figure 4 presents frequency distribution histograms of negative control (Fig. 4A), positive control (Fig. 4B), and one semen of male partners of infertile couples positive for C. trachomatis qPCR (Fig. 4C). Mean percentage of spermatozoa with DNA fragmentation (±SD) was higher in male partners of infertile couples positive for C. trachomatis qPCR than those of uninfected patients (29.2±17.2% vs. 25.1±14.3%). But the increase in sperm DNA fragmentation remains statistically not significant (p = 0.62) (Table 4).
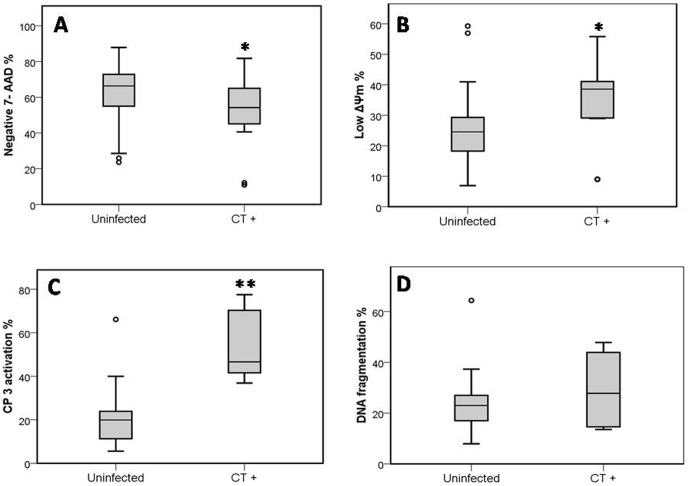
Distributions of percentages of different apoptotic markers among patients positive for C. trachomatis qPCR compared to uninfected patients are shown in figure 5.
Figure 5. Distributions of percentages of different apoptotic markers among patients positive for C. trachomatis qPCR compared to uninfected patients.
(A) Mean percentage of Sperm Vitality, evaluated with 7-amino-actinomycin-D Dye (7-AAD). (B) Mean percentage of Sperm mitochondrial membrane potential (ΔΨm), evaluated with JC-1. (C) Mean percentage of Caspase 3 activation, evaluated with fluorescein-labeled inhibitor of caspases (FLICA). (D) Mean percentage of Sperm DNA fragmentation, evaluated with (TUNEL). Uninfected: Sperm of uninfected patients (negative for all PCRs performed and for spermioculture analysis). CT+: sperm of patients positive for C. trachomatis qPCR. * Indicates significant differences compared with uninfected semen (P<0.05). ** Indicates significant differences compared with uninfected semen (P<0.001).
Discussion
The importance of genital tract microorganisms as an etiologic factor in male infertility is still a controversial topic [39]. The purpose of this study was to determine the prevalence of several common sexually transmitted pathogens among male members of infertile couples. Asymptomatically infected individuals may carry lower amount of organisms [40]. Besides, real time PCR is easier and has higher sensitivity and specificity. Thus, real time PCR may be the technique of choice for bacterial detection and quantification in semen specimens of asymptomatic male partners. Our study demonstrated that C. trachomatis seems to be the most widespread sexually transmitted pathogen among male partners of infertile couples in Sfax (South of Tunisia), as shown by its high prevalence. Our findings confirm previous reports among male partners of infertile couples in Tunisia [41], with lower frequency (15.2% vs 43.3%). This difference might be explained by the use of different methods for the detection of this bacterium. We have used a quantitative real time PCR, which is more specific than in-house PCR-microtiter plate hybridization method. The prevalence of N. gonorrhoeae in our study was (5.8%) among male partners of infertile couples. This prevalence was higher than that previously reported in recent studies conducted in other country such as in Canada [42] and in our country [41]. This prevalence of N. gonorrhoeae (5.8%) was nearly similar to that reported in other recent studies [43] in Jordan (6.5%). In addition, the qPCR used in our study was reported to be highly sensitive and specific by two authors [44]–[45]. The results of this study, also revealed that the prevalence of M. genitalium (3.5%) in infertile men is nearly similar with that reported by Gdoura et al (2008) (4.8%) in our country and Al-Sweih et al (2012) in Jordan (3.2%) [41]–[46]. Surprisingly, the prevalence of U. urealyticum (5.8%) found in our study was considerably lower than previously reported in our country by Gdoura et al (2008) [41]. In the literature, the prevalence of U. urealyticum in the semen samples of male infertile patients varies from 5% to 42% [47], [48]–[49]. This wide range might be explained by the diversity of detection methods used for characterizing the studied populations. Most of the previous reported studies have discussed the role of Ureaplasma in male infertility without discriminating between U. urealyticum and U. parvum [47]–[50]. In our study, we used a quantitative real time PCR for facilitating the detection and quantification of U. urealyticum, U. parvum, M. hominis, and M. genitalium in semen specimens. By this method, U. parvum was detected in only one patient (1.1%). The prevalence of this species in our study was lower than that reported by Knox et al (2003) (19.2%) and was nearly similar to that reported by Gdoura et al (2008) in our country (2.9%) [41]–[48]. In the literature, M. hominis has been associated with bacterial vaginosis, pelvic inflammatory disease in women [51]. However, its role in nongonoccocal urethritis and in infertility was rarely investigated [52]. The prevalence of M. hominis in our study was (1.1%) comparable to that reported by Rosemond et al (2006) (0%) but less than that found by Gdoura et al (2008) (9.6%) [41–53]. The role of C. trachomatis infection on semen parameters in male infertility is controversial. In fact, a large number of studies have suggested that positive markers for Chlamydia infection are not associated with altered sperm parameters [18], [19], [46], [54]–[55]. Others, however, have found that Chlamydia infection correlates with reduced sperm motility [34]–[56], increased proportion of sperm abnormalities [57], significant reductions in semen density, sperm morphology, and viability [58] and increased likelihood of leukocytospermia [34]. In addition, Veznik et al (2004) reported decreases in seminal plasma, sperm mobility, velocity, and normal morphology in C. trachomatis–infected infertile patients compared with those without infection [59]. Mazzoli et al (2010) found that C. trachomatis affects sperm concentration, percentage of motile sperm and normal morphological forms in patients with prostatitis [12]. A final conclusion from all studies is difficult to establish due to the diversity of population on one hand and variability in sensitivity and specificity of used techniques on the other hand. Moreover, during infertility assessment, infertile couples are not systematically screened for this infection, hence clinically silent C. trachomatis infection may be revealed by complications. In fact, the mean duration of infertility in our study was 4 years and patients consulted at different stages of the infection. Lastly, we showed that inoculation of fertile male Swiss mice in the meatus urethra with C. trachomatis could lead to alteration of semen parameters (the sperm motility, viability, morphology and sperm concentration) [35]. Our study are concordant with our latter experimental study, the sperm concentration and rapid progressive motility (category a) of spermatozoa in the male partners of infertile couples with C. trachomatis DNA in semen specimens showed a significant decrease in comparison with those without infection. Moreover, the sperm vitality and total motility of spermatozoa in the male partners of infertile couples with C. trachomatis DNA in semen specimens was lower but without significances compared to patients without infection. The leukocytes count in the male partners of infertile couples with C. trachomatis DNA in semen specimens was higher but without significances compared with those without infection. Thus, C. trachomatis infection could lead to a decrease in sperm quality.
Apoptosis is a mode of programmed cellular death based on a genetic mechanism that induces a series of cellular, morphological and biochemical alterations, leading the cell to suicide without eliciting an inflammatory response. Mature sperm cells have been reported to express distinct markers of apoptosis-related cell damage [60]–[61]. Externalization of PS to the sperm outer membrane brochure is considered to mark terminal apoptosis. Activated caspase-3, loss of the integrity of the ΔΨm and DNA fragmentation are other markers of terminal apoptosis expressed by a varying proportion of ejaculated sperm [25]–[62]. It has been hypothesized that sperm cell death is associated with male infertility [63]–[64]; however, the exact mechanisms of its involvement remain to be elucidated [65]. Sperm apoptosis and dysfunction have also been reported after sperm exposure to C. trachomatis both in vivo and in vitro. In vitro studies have shown that the coincubation of human sperm with C. trachomatis serovar E causes a significant decline in the percentage of motile sperm and results in premature sperm death [33]. This sperm death has been demonstrated to be primarily caused by LPS [32]. Moreover, it has been shown that Chlamydial LPS interact with CD14 on the sperm surface, leading to increased production of reactive oxygen species and resulting in caspase-mediated apoptosis by using a fluorogenic substrate [29]. Lastly, Satta et al (2006) observed that the experimental C. trachomatis infection causes sperm PS externalization and DNA fragmentation [30]. In vivo studies have reported a higher frequency of sperm cells with fragmented DNA in infertile subjects with C. trachomatis genitourinary infection than in control fertile subjects, using the sperm chromatin dispersion test [34]. Moreover, our experimental mouse model has also showed a significant increase of apoptotic and necrotic spermatozoa percentages in infected mice when compared with the control group [35]. In line with these findings, our data demonstrated a direct role of C. trachomatis in apoptosis. In order to elucidate the implication of apoptosis in infected semen with C. trachomatis DNA, we studied in the first part of our study the viability of spermatozoa using 7-AAD vital stain dye. We found a significant decrease of the mean percentage of viable spermatozoa (7-AAD negative) in male partners of infertile couples with C. trachomatis DNA in comparison with uninfected male partners of infertile couples. C. trachomatis infection was more correlated negatively with the viability measured using 7-AAD dye than with the viability measured using eosin staining. 7-AAD Dye is more objective than eosin staining. In the second part of our study we studied the state of mitochondrial membrane potential in semen using the lipophilic fluorescent probe JC-1. JC-1 probe has been validated in the assessment of stallion and bull spermatozoa using Flow Cytometry [66]–[67] and provides a more rigorous estimate of metabolic function than Mito Tracker or Rhodamine 123 [67]. In our study, we found a significant increase of the mean percentage of spermatozoa with low ΔΨm in male partners of infertile couples with C. trachomatis DNA in semen specimens in comparison with male partners of infertile couples without C. trachomatis DNA in semen specimens. At our knowledge, our study represents the first study to characterize the state of ΔΨm in spermatozoa of infertile couples with C. trachomatis DNA. In line with our findings, Mabel et al (2010) have reported a significant reduction in the percentage of sperm with intact ΔΨm by in vitro incubation of human sperm cells with E. coli bacteria and the supernatant obtained from these bacteria [68]. In addition, this study demonstrates that contact with E. coli bacteria affects sperm mitochondrial function and also confirm the first in vitro study reported by Villegas et al (2005), demonstrating that soluble factors released by E. coli contribute to increase in apoptotic markers in human spermatozoa [69]. Our in vivo study confirms these in vitro findings and leads to suggest that C. trachomatis infection could affect sperm mitochondrial function. Caspase activity has been shown to be present in human sperm [25]–[70]. Furthermore, in infertile men a higher percentage of sperm with activated caspases was found, confirming the existence of a caspase-dependent apoptotic pathway in ejaculated human sperm [71]. In the third part of our study, we studied the activation of caspase 3 in spermatozoa of infertile men. We noticed also a significant increase of caspase 3 activation in male partners of infertile couples with C. trachomatis DNA in semen specimens in comparison to male partners of infertile couples without C. trachomatis DNA in semen specimens. Our in vivo result corroborated with that of Eley et al (2005), who demonstrated that the in vitro co-incubation of sperm with C. trachomatis LPS results in cellular death which is in part due to apoptosis and is caspase 3 mediated [29]. In the last part of our study we studied the sperm DNA fragmentation using (TUNEL) assay. Induction of DNA fragmentation of sperm's nuclei has been widely suggested by several authors because their possible impact on fertility goes beyond fertilization and pregnancy outcome [34]–[72]. In fact, Gallegos et al (2008) assessed sperm DNA integrity with sperm dispersion test have found that men with C. trachomatis and Mycoplasma infections had significantly greater sperm DNA fragmentation than fertile control subjects [34]. These results suggest that C. trachomatis and Mycoplasma may affect sperm DNA. In line with this study, we noticed a slight increase in sperm DNA damage in male partners of infertile couples with C. trachomatis DNA in semen specimens in comparison with male partners of infertile couples without C. trachomatis DNA in semen specimens.The limitations of our study were firstly the low number of our population (only 85 infertile men) and secondly the absence of a control groups composed of fertile men. Thus, we have limited our comparison between semen from infected and uninfected infertile men with C. trachomatis.
In conclusion, using a quantitative Real time PCR our study indicated that this PCR provides a sensitive measure to detect human C. trachomatis, genital Mycoplasmas, and genital Ureaplasmas DNA, which is useful for epidemiologic studies of these pathogens. Our results also demonstrated that C. trachomatis seems to be widespread among male partners of infertile couples in Sfax (South of Tunisia). This study supports that C. trachomatis infection could lead to a decrease in sperm quality and apoptosis induction. In fact, C. trachomatis infection was found to increase the ΔΨm dysfunction in spermatozoa and caspase 3 activation. However, sperm DNA damage was not significantly associated to C. trachomatis infection. This leads us to suggest that caspase 3 could be implicated during C. trachomatis infection but does not cause directly DNA damage.
Funding Statement
The work was financed by the research laboratory “MPH” Habib Bourguiba University Hospital of Sfax Tunisia. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Keck C, Gerber-Schäfer C, Clad A, Wilhelm C, Breckwoldt M (1998) Seminal tract infections: impact on male fertility and treatment options. Hum Reprod Update 4: 891–903. [DOI] [PubMed] [Google Scholar]
- 2.Hamdad-Daoudi F, Petit J, Eb F (2004) Assessment of Chlamydia trachomatis infection in asymptomatic male partners of infertile couples. J Med Microbiol 53: : 985–990. [DOI] [PubMed] [Google Scholar]
- 3.Rowe PJ, Comhaire FH, Hargreave TB, Mahmoud AMA (2000) WHO manual for the standardized investigation, diagnosis and management of the infertile male.Cambridge University Press, Cambridge.
- 4. Paavonen J, Eggert-Kruse W (1999) Chlamydia trachomatis: impact on human reproduction. Hum Reprod Update 5: 433–447. [DOI] [PubMed] [Google Scholar]
- 5. Gdoura R, Keskes-Ammar L, Bouzid F, Eb F, Hammami A, et al. (2001) Chlamydia trachomatis and male infertility in Tunisia. Eur J Contracept Reprod Health Care 6: 102–107. [PubMed] [Google Scholar]
- 6. Ochsendorf FR (2008) Sexually transmitted infections: impact on male fertility. Andrologia 40: 72–75. [DOI] [PubMed] [Google Scholar]
- 7. Cengiz T, Aydoğanli L, Baykam M, Mungan NA, Tunçbilek E, et al. (1997) Chlamydial infections and male infertility. Int Urol Nephrol 29: 687–693. [DOI] [PubMed] [Google Scholar]
- 8. Al-Mously N, Cross NA, Eley A, Pacey AA (2009) Real-time polymerase chain reaction shows that density centrifugation does not always remove Chlamydia trachomatis from human semen. Fertil Steril 92: 1606–1615. [DOI] [PubMed] [Google Scholar]
- 9. Habermann B, Krause W (1999) Altered sperm function or sperm antibodies are not associated with Chlamydial antibodies in infertile men with leucocytospermia. J Eur Acad Dermatol Venereol 12: 25–9. [PubMed] [Google Scholar]
- 10. Hosseinzadeh S, Eley A, Pacey AA (2004) Semen quality of men with asymptomatic Chlamydial infection. J Androl 25: 104–109. [DOI] [PubMed] [Google Scholar]
- 11. Idahl A, Boman J, Kumlin U, Olofsson JI (2004) Demonstration of Chlamydia trachomatis IgG antibodies in the male partner of the infertile couple is correlated with a reduced likelihood of achieving pregnancy. Hum Reprod 19: 1121–1126. [DOI] [PubMed] [Google Scholar]
- 12. Mazzoli S, Cai T, Addonisio P, Bechi A, Mondaini N, et al. (2010) Chlamydia trachomatis infection is related to poor semen quality in young prostatitis patients. Eur Urol 57: 708–714. [DOI] [PubMed] [Google Scholar]
- 13. La Vignera S, Vicari E, Condorelli RA, D'Agata R, Calogero AE (2011) Male accessory gland infection and sperm parameters (review). Int J Androl 34: e330–e347. [DOI] [PubMed] [Google Scholar]
- 14. Pajovic B, Radojevic N, Vukovic M, Stjepcevic A (2013) Semen analysis before and after antibiotic treatment of asymptomatic Chlamydia and Ureaplasma-related pyospermia. Andrologia 45: 266–271. [DOI] [PubMed] [Google Scholar]
- 15. Weidner W, Floren E, Zimmermann O, Thiele D, Ludwig M (1996) Chlamydial antibodies in semen: search for “silent” Chlamydial infections in asymptomatic andrological patients. Infection 24: 309–313. [DOI] [PubMed] [Google Scholar]
- 16. Ochsendorf FR, Ozdemir K, Rabenau H, Fenner T, Oremek R, et al. (1999) Chlamydia trachomatis and male infertility: Chlamydia-IgA antibodies in seminal plasma are C. trachomatis specific and associated with an inflammatory response. J Eur Acad Dermatol Venereol 12: 143–152. [PubMed] [Google Scholar]
- 17. Vigil P, Morales P, Tapia A, Riquelme R, Salgado AM (2002) Chlamydia trachomatis infection in male partners of infertile couples: incidence and sperm function. Andrologia 34: 155–161. [DOI] [PubMed] [Google Scholar]
- 18. Eggert-Kruse W, Rohr G, Kunt B, Meyer A, Wondra J, et al. (2003) Prevalence of Chlamydia trachomatis in subfertile couples. Fertil Steril 80: 660–663. [DOI] [PubMed] [Google Scholar]
- 19. Motrich RD, Cuffini C, Oberti JP, Maccioni M, Rivero VE (2006) Chlamydia trachomatis occurrence and its impact on sperm quality in chronic prostatitis patients. J Infect 53: 175–183. [DOI] [PubMed] [Google Scholar]
- 20. De Barbeyrac B, Papaxanthos-Roche A, Mathieu C, Germain C, Brun JL, et al. (2006) Chlamydia trachomatis in subfertile couples undergoing an in vitro fertilization program: a prospective study. Eur J Obstet Gynecol Reprod Biol 129: 46–53. [DOI] [PubMed] [Google Scholar]
- 21. Gdoura R, Kchaou W, Chaari C, Znazen A, Keskes L, et al. (2007) Ureaplasma urealyticum, Ureaplasma parvum, Mycoplasma hominis and Mycoplasma genitalium infections and semen quality of infertile men. BMC Infect Dis 7: 129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gewies A, Grimm S (2003) Cathepsin-B and cathepsin-L expression levels do not correlate with sensitivity of tumour cells to TNF-alpha-mediated apoptosis. Br J Cancer 89: 1574–1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gorczyca W, Traganos F, Jesionowska H, Darzynkiewicz Z (1993) Presence of DNA strand breaks and increased sensitivity of DNA in situ to denaturation in abnormal human sperm cells: analogy to apoptosis of somatic cells. Exp Cell Res 207: 202–205. [DOI] [PubMed] [Google Scholar]
- 24.Schuffner A, Morshedi M, Vaamonde D, Duran EH, Oehninger S (2002) Effect of different incubation conditions on phosphatidylserine externalization and motion parameters of purified fractions of highly motile human spermatozoa. J Androl 23: :194–201. [PubMed] [Google Scholar]
- 25. Paasch U, Grunewald S, Agarwal A, Glandera HJ (2004) Activation pattern of caspases in human spermatozoa. Fertil Steril 81: 802–809. [DOI] [PubMed] [Google Scholar]
- 26. Rasola A, Bernardi P (2007) The mitochondrial membrane transition pore and its involvement in cell dead and disease pathogenesis. Apoptosis 12: 815–833. [DOI] [PubMed] [Google Scholar]
- 27. Marchetti C, Obert G, Deffosez A, Formstecher P, Marchetti P (2002) Study of mitochondrial membrane potential, reactive oxygen species, DNA fragmentation and cell viability by flow cytometry in human sperm. Hum Reprod 17: 1257–1265. [DOI] [PubMed] [Google Scholar]
- 28. Hosseinzadeh S, Brewis IA, Eley A, Pacey AA (2001) Co-incubation of human spermatozoa with Chlamydia trachomatis serovar E causes premature sperm death. Hum Reprod 16: 293–299. [DOI] [PubMed] [Google Scholar]
- 29. Eley A, Hosseinzadeh S, Hakimi H, Geary I, Pacey AA (2005) Apoptosis of ejaculated human sperm is induced by coincubation with Chlamydia trachomatis lipopolysaccharide. Hum Reprod 20: 2601–2607. [DOI] [PubMed] [Google Scholar]
- 30. Satta A, Stivala A, Garozzo A, Morello A, Perdichizzi A, et al. (2006) Experimental Chlamydia trachomatis infection causes apoptosis in human sperm. Hum Reprod 21: 134–137. [DOI] [PubMed] [Google Scholar]
- 31. Galdiero F, Sommese L, Gorga F, Galdiero E, Rizzo A, et al. (1994) Toxic effect on human spermatozoa by Chlamydia trachomatis purified lipopolysaccharide. FEMS Microbiol Lett 115: 197–200. [DOI] [PubMed] [Google Scholar]
- 32. Hosseinzadeh S, Pacey AA, Eley A (2003) Chlamydia trachomatis-induced death of human spermatozoa is caused primarily by lipopolysaccharide. J Med Microbiol 52: 193–200. [DOI] [PubMed] [Google Scholar]
- 33. Hosseinzadeh S, Brewis IA, Pacey AA, Moore HDM, Eley A (2000) Coincubation of human spermatozoa with Chlamydia trachomatis in vitro causes increased tyrosine phosphorylation of sperm proteins. Infect Immun 68: 4872–4876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gallegos G, Ramos B, Santiso R, Goyanes V, Gosalvez J, et al. (2008) Sperm DNA fragmentation in infertile men with genitourinary infection by Chlamydia trachomatis and mycoplasma. Fertil Steril 90: 328–334. [DOI] [PubMed] [Google Scholar]
- 35. Sellami H, Gdoura R, Mabrouk I, Frikha-Gargouri O, Keskes L, et al. (2011) A proposed mouse model to study male infertility provoked by genital serovar E, Chlamydia trachomatis . Journal of Andrology 32: 86–94. [DOI] [PubMed] [Google Scholar]
- 36.World Health Organisation (1999) WHO Laboratory Manual for the Examination of Human Semen and Sperm Cervical Mucus Interaction. 4th edition. Cambridge, United Kingdom: University Press.
- 37. Vogels WHM, Van Voost Vader PC, Schrorder FP (1993) Chlamydia trachomatis infection in a high-risk population: comparison of polymerase chain reaction and cell culture for diagnosis and follow-up. J Clin Microbiol 31: 1103–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Whelan JA, Russell NB, Whelan MA (2003) A method for the absolute quantification of cDNA using real-time PCR. J Immunol Methods 278: 261–269. [DOI] [PubMed] [Google Scholar]
- 39. Dejucq N, Jegou B (2001) Viruses in the mammalian male genital tract and their effects on the reproductive system. Microbiol Mol Biol Rev 65: 208–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Witkin SS (2002) Immunological aspects of genital Chlamydia infections. Best Pract Res Clin Obstet Gynaecol.16: 865–874. [DOI] [PubMed] [Google Scholar]
- 41. Gdoura R, Kchaou W, Ammar-Keskes L, Chakroun N, Znazen A, et al. (2008) Assessment of Chlamydia trachomatis, Ureaplasma urealyticum, Ureaplasma parvum, Mycoplasma hominis, and Mycoplasma genitalium in semen and first void urine specimens of asymptomatic male partners of infertile couples. J Androl 29: 198–206. [DOI] [PubMed] [Google Scholar]
- 42. Domes T, Lo KC, Grober ED, Mullen JB, Mazzulli T, et al. (2011) The utility and cost of Chlamydia trachomatis and Neisseria gonorrhoeae screening of a male infertility population. Fertil Steril 97: 299–305. [DOI] [PubMed] [Google Scholar]
- 43. Abusarah EA, Awwad ZM, Charvalos E, Shehabi AA (2013) Molecular detection of potential sexually transmitted pathogens in semen and urine specimens of infertile and fertile males. Diagn Microbiol Infect Dis 77: 283–286. [DOI] [PubMed] [Google Scholar]
- 44. Jalal H, Delaney A, Bentley N, Sonnex C, Carne CA (2013) Molecular epidemiology of selected sexually transmitted infections. Int J Mol Epidemiol Genet 4: 167–174. [PMC free article] [PubMed] [Google Scholar]
- 45. Datcu R, Gesink D, Mulvad G, Montgomery-Andersen R, Rink E, et al. (2013) Vaginal microbiome in women from Greenland assessed by microscopy and quantitative PCR. BMC Infect Dis 13: 480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Al-Sweih NA, Al Fadli AH, Omu AE, Rotimi VO (2012) Prevalence of Chlamydia trachomatis, Mycoplasma hominis, Mycoplasma genitalium and Ureaplasma urealyticum infections and seminal quality in infertile and fertile men in Kuwait. J Androl 33: 1323–1329. [DOI] [PubMed] [Google Scholar]
- 47. De Jong Z, Pontonnier F, Plante P, Perie N, Talazac N, et al. (1990) Comparison of the incidence of Ureaplasma urealyticum in infertile men and in donors of semen. Eur Urol 18: 127–131. [DOI] [PubMed] [Google Scholar]
- 48. Knox CL, Allan JA, Allan JM, Edirisinghe WR, Stenze DL, et al. (2003) Ureaplasma parvum and Ureaplasma urealyticum are detected in semen after washing before assisted reproductive technology procedures. Fertil Steril 80: 921–929. [DOI] [PubMed] [Google Scholar]
- 49. Wang Y, Liang CL, Wu JQ, Xu C, Qin SX, et al. (2006) Ureaplasma urealyticum infections in the genital tract affect semen quality? Asian J Androl 8: 562–568. [DOI] [PubMed] [Google Scholar]
- 50. Bornman MS, Mahomed MF, Boomker D, Schulenburg GW, Reif S, et al. (1990) Microbial flora in semen of infertile African men at Garankuwa hospital. Andrologia 22: 118–121. [DOI] [PubMed] [Google Scholar]
- 51. Yoshida T, Maeda S, Deguchi T, Ishiko H (2002) Phylogeny-based rapid identification of mycoplasmas and ureaplasmas from urethritis patients. J Clin Microbiol 40: 105–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Pannekoek Y, Trum JW, Bleker OP, Veen FVD, Spanjaard L, et al. (2000) Cytokine concentrations in seminal plasma from subfertile men are not indicative of the presence of Ureaplasma urealyticum or Mycoplasma hominis in the lower genital tract. J Med Microbiol 49: 697–700. [DOI] [PubMed] [Google Scholar]
- 53. Rosemond A, Lanotte P, Watt S, Sauget AS, Guerif F, et al. (2006) Existe-t-il un bénéfice au dépistage systematique de Chlamydia trachomatis, Mycoplasma hominis et Ureaplasma urealyticum dans les prélèvements genito-urinaires réalisés au cours d'un bilan d'infertilité? Pathol Biol 54: 125–129. [DOI] [PubMed] [Google Scholar]
- 54. Rybar R, Prinosilova P, Kopecka V, Hlavicova J, Veznik Z, et al. (2012) The effect of bacterial contamination of semen on sperm chromatin integrity and standard semen parameters inmen from infertile couples. Andrologia 44: 410–418. [DOI] [PubMed] [Google Scholar]
- 55. Liu J, Wang Q, Ji X, Guo S, Dai Y, et al. (2014) Prevalence of Ureaplasma Urealyticum, Mycoplasma Hominis, Chlamydia Trachomatis Infections, and Semen Quality in Infertile and Fertile Men in China. Urology 83: 795–799. [DOI] [PubMed] [Google Scholar]
- 56. Jakiel G, Robak-Chołubek D, Wieczorek P, Bokiniec M (2004) Evaluation of some parameters of human semen with positive Chlamydial reaction. Ann Univ Mariae Curie Sklodowska Med 59: 61–4. [PubMed] [Google Scholar]
- 57. Custo GM, Saitto LV, Frongillo RF (1989) Chlamydial infection and male fertility: an epidemiological study. Arch Androl 23: 243–248. [DOI] [PubMed] [Google Scholar]
- 58. Land JA, Van Bergen JE, Morré SA, Postma MJ (2010) Epidemiology of Chlamydia trachomatis infection in women and the cost- effectiveness of screening. Hum Reprod Update 16: 189–204. [DOI] [PubMed] [Google Scholar]
- 59. Veznik Z, Pospisil L, Svecova D, Zajicova A, Unzeitig V (2004) Chlamydiae in the ejaculate: their influence on the quality and morphology of sperm. Acta Obstet Gynecol Scand 83: 656–660. [DOI] [PubMed] [Google Scholar]
- 60. Sakkas D, Mariethoz E, St John JC (1999) Abnormal sperm parameters in humans are indicative of an abortive apoptotic mechanism linked to the Fas mediated pathway. Experimental Cell Research 251: 350–355. [DOI] [PubMed] [Google Scholar]
- 61. Shen HM, Dai J, Chia SE, Lim A, Ong CN (2002) Detection of apoptotic alterations in sperm in subfertile patients and their correlations with sperm quality. Human Reproduction 17: 1266–1273. [DOI] [PubMed] [Google Scholar]
- 62. Evenson DP, Larson KL, Jost LK (2002) Sperm chromatin structure assay: its clinical use for detecting sperm DNA fragmentation in male infertility and comparisons with other techniques. J Androl 23: 25–43. [DOI] [PubMed] [Google Scholar]
- 63. Sakkas D, Seli E, Bizzaro D, Tarozzi N, Manicardi GC (2003) Abnormal spermatozoa in the ejaculate: abortive apoptosis and faulty nuclear remodelling during spermatogenesis. Reprod Biomed Online 7: 428–432. [DOI] [PubMed] [Google Scholar]
- 64. Taylor SL, Weng SL, Fox P, Duran EH, Morshedi MS, et al. (2004) Somatic cell apoptosis markers and pathways in human ejaculated sperm: potential utility as indicators of sperm quality. Mol Hum Reprod 10: 825–834. [DOI] [PubMed] [Google Scholar]
- 65. Agarwal A, Said TM (2005) Oxidative stress, DNA damage and apoptosis in male infertility: a clinical approach. BJU Int 95: 503–507. [DOI] [PubMed] [Google Scholar]
- 66. Garner DL, Thomas CA (1999) Organelle-specific probe JC-1 identifies membrane potential differences in the mitochondrial function of bovine sperm. Mol Reprod Dev 53: 222–229. [DOI] [PubMed] [Google Scholar]
- 67. Gravance CG, Garner DL, Baumber J, Ball BA (2000) Assessment of equine sperm mitochondrial function using JC-1. Theriogenoyly 53: 1691–1703. [DOI] [PubMed] [Google Scholar]
- 68. Schulz M, Sanchez R, Soto L, Risopatron J, Villegas J (2010) Effect of Escherichia coli and its soluble factors on mitochondrial membrane potential, phosphatidylserine translocation, viability, and mobility of human spermatozoa. Fertil Steril 94: 619–623. [DOI] [PubMed] [Google Scholar]
- 69. Villegas J, Schulz M, Soto L, Sanchez R (2005) Bacteria induce expression of apoptosis in human spermatozoa. Apoptosis 10: 105–110. [DOI] [PubMed] [Google Scholar]
- 70. Weng SL, Taylor SL, Morshedi M, Schuffner A, Duran EH, et al. (2002) Caspase activity and apoptotic markers in ejaculated human sperm. Mol Hum Reprod 8: 984–991. [DOI] [PubMed] [Google Scholar]
- 71. Paasch U, Grunewald S, Fitzl G, Glander HJ (2003) Deterioration of plasma membrane is associated with activated caspases in human spermatozoa. J Androl 24: 246–252. [DOI] [PubMed] [Google Scholar]
- 72. Reichart M, Kahane I, Bartoov B (2000) In vivo and in vitro impairment of human and ram sperm nuclear chromatin integrity by sexually transmitted Ureaplasma urealyticum infection. Biol Reprod 63: 1041–1048. [DOI] [PubMed] [Google Scholar]
- 73. Jalal H, Stephen H, Curran MD, Burton J, Bradley M, et al. (2006) Development and validation of a rotor-gene real-time PCR assay for detection, identification, and quantification of Chlamydia trachomatis in a single reaction. J Clin Microbiol 44: 206–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Hjelmevoll SO, Olsen ME, Sollid JU, Haaheim H, Unemo M, et al. (2006) A fast real time polymerase chain reaction method for sensitive and specific detection of the Neisseria gonorrhaeae por A pseudogene. J Mol Diagn 8: 574–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Jensen JS, Björnelius E, Dohn B, Lidbrink P (2004) Use of TaqMan 5′ nuclease real-time PCR for quantitative detection of Mycoplasma genitalium DNA in males with and without urethritis who were attendees at a sexually transmitted disease clinic. J Clin Microbiol 42: 683–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Pascual A, Jaton K, Ninet B, Bille J, Greub G (2010) New Diagnostic Real-Time PCR for Specific Detection of Mycoplasma hominis DNA. Int J Microbiol 2010: 317512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Vancutsem E, Soetens O, Breugelmans M, Foulon W, Naessens A (2011) Modified real time PCR for detecting, differentiating, and quantifying Ureaplasma urealyticum and Ureaplasma parvum . J Mol Diagn 13: 206–212. [DOI] [PMC free article] [PubMed] [Google Scholar]