Abstract
Purpose
To investigate the etiology of bilateral disc swelling in Japanese.
Methods
Using Kitasato University’s Department of Neuro-Ophthalmology medical records and fundus photographs of the period December 1977 through November 2010, we retrospectively identified 121 outpatients who had been initially confirmed with bilateral disc swelling.
Results
The most common cause of the bilateral disc swelling was increased intracranial pressure (ICP) (59%); followed by pseudopapillitis (16%); uveitis (8%); hypertensive retinopathy (5%); bilateral optic neuritis, acute disseminated encephalomyelitis (ADEM) and optic disc drusen (all at 2% each); and leukemia (1%). Unknown etiology accounted for 6% of the cases.
Conclusion
Although increased ICP is the most common etiology for bilateral disc swelling, it can also be triggered by a variety of other causes. Pseudopapillitis is the most important progenitor of bilateral disc swelling in Japanese.
Keywords: bilateral, disc swelling, papilledema, increased ICP, intracranial pressure
Introduction
Although bilateral disc swelling is often encountered in routine clinical practice, there is a lack of recent Japanese reports that have studied the etiologies of this condition.1,2 Thus, understanding the most common cause of bilateral disc swelling is thought to be crucial to its subsequent diagnosis and treatment. With this in mind, we conducted a retrospective study of bilateral disc swelling in patients at Kitasato University’s Department of Neuro-Ophthalmology in an attempt to identify the etiology.
Methods
Using Kitasato University’s Department of Neuro-Ophthalmology medical records and fundus photographs of the period December 1977 through November 2010, we retrospectively identified 121 outpatients who had been initially confirmed with bilateral disc swelling. We excluded patients without fundus photographic confirmation of disc swelling. This study population consisted of 54 males and 67 females with an average age of 38.2 years (range 2–76 years). We defined terms as follows: “disc swelling” was the collective term used to describe disc swelling or protrusion; “papillitis” denoted optic neuritis with inflammatory findings on the optic disc such as swelling/redness or dilatation of the retinal vessels; and “papilledema” indicated bilateral disc swelling with elevated intracranial pressure. The final diagnosis was judged by ophthalmologic examinations (including light reflex of the pupil, visual acuity, visual field, critical flicker frequency, and fundus angiography) and intracranial examinations by magnetic resonance imaging (MRI), magnetic resonance venography (MRV), or computed tomography (CT), and consultation with the Kitasato University Department of Neurology or Department of Neurosurgery.
Results
In this study cohort, the most common etiology of bilateral disc swelling was increased intracranial pressure (ICP) (59%); followed by pseudopapillitis (16%); uveitis (8%); hypertensive retinopathy (5%); bilateral neuritis, acute disseminated encephalomyelitis (ADEM) and optic disc drusen (all at 2%); and leukemia (1%). Unknown etiology accounted for the remaining 6% (Figure 1). When examining the etiology according to patient age group (eg, 0−20 years, 21−50 years, and ≥51 years), increased ICP was found to be the most frequently-appearing condition. In the 0−20 patient age group, which constituted the smallest age demographic (27/121), increased ICP and pseudopapillitis were present in the vast majority of patients presenting with bilateral disc swelling.
Figure 1.
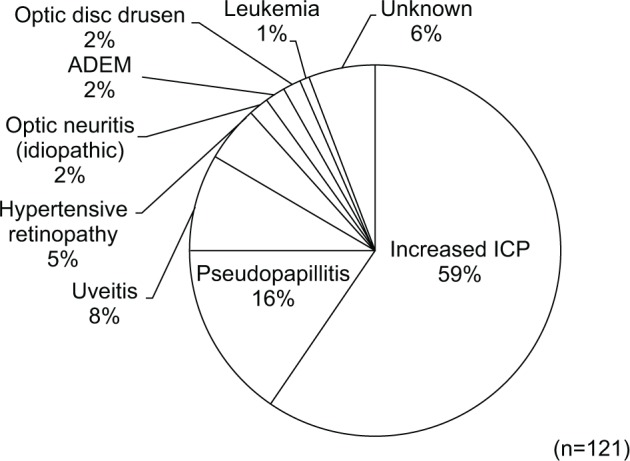
Etiologies of bilateral disc swelling.
Notes: The most common cause of the bilateral disc swelling was increased intracranial pressure (ICP) (59%), followed by pseudopapillitis (16%), uveitis (8%), hypertensive retinopathy (5%), bilateral optic neuritis, acute disseminated encephalomyelitis (ADEM) and optic disc drusen (all at 2% each), and leukemia (1%). Unknown etiology accounted for 6% of the cases.
In the 21−50 age group, which contained the majority of the patients (62/121), an increased ICP was the leading cause of bilateral disc swelling, followed by pseudopapillitis, uveitis, and hypertensive retinopathy. A larger number of etiologies were found in the 21−50 group than in the 0−20 group. There were 32 patients in the ≥51 group who exhibited similar etiologies to the 21−50 group, despite the group containing around half the number of patients (Table 1). The most common etiology responsible for the increased ICP (n=72) was brain tumor (32 patients; 44.4%), followed by cerebral hemorrhage, chronic subdural hematoma, cerebral venous sinus thrombosis (CVST), and other cardiovascular diseases.
Table 1.
Etiologies by age
| Disease | Patients
|
||
|---|---|---|---|
| ≤20 years old | 21–50 years old | ≥51 years old | |
| Increased ICP | 13 | 39 | 20 |
| Pseudopapillitis | 10 | 6 | 3 |
| Uveitis | 0 | 6 | 4 |
| Hypertensive retinopathy | 0 | 5 | 1 |
| Optic neuritis (idiopathic) | 0 | 1 | 1 |
| ADEM | 0 | 2 | 0 |
| Optic disc drusen | 0 | 1 | 1 |
| Leukemia | 0 | 0 | 1 |
| Unknown | 4 | 2 | 1 |
| Total | 27 | 62 | 32 |
Abbreviations: ICP, intracranial pressure; ADEM, acute disseminated encephalomyelitis.
A form of osteodystrophy known as craniosynostosis was also observed in a few rare cases (Table 2). Although characterized by the absence of intracranial space occupying lesions, idiopathic intracranial hypertension (IIH) was also included in the intracranial event category due to its clinical feature of increased intracranial pressure.
Table 2.
Causes of increased ICP
| Increased ICP | n (%) |
|---|---|
| Brain tumor | 32 (44.4) |
| Cerebral hemorrhage | 7 (9.7) |
| Chronic subdural hematoma | 5 (6.9) |
| CVST | 5 (6.9) |
| IIH | 5 (6.9) |
| Meningitis | 4 (5.6) |
| Aqueduct stenosis | 4 (5.6) |
| Dural arteriovenous fistula | 2 (2.8) |
| Hypertrophic pachymeningitis | 2 (2.8) |
| Brain abscess | 2 (2.8) |
| Craniosynostosis | 2 (2.8) |
| Subarachnoid hematoma | 1 (1.4) |
| Arnold–Chiari malformation | 1 (1.4) |
Abbreviations: ICP, intracranial pressure; CVST, cerebral venous and sinus thrombosis; IIH, idiopathic intracranial hypertension.
Categorization of brain tumors in the patients revealed nine metastatic brain tumors and 22 primary brain tumors. The most common type of tumor was meningioma (n=7) followed by astrocytoma (n=5), glioma (n=3), glioblastoma (n=3), acoustic neurinoma (n=2), olfactory neuroepithelioma (n=1), pineal tumor (n=1), and choroid plexus papilloma (n=1). The tumors occurred most frequently in the frontal lobe followed by the cerebellum (Table 3). The most common primary cancer site among the nine subjects with metastatic brain tumors was lung (n=4) (Table 4).
Table 3.
Causes of brain tumor
| Brain tumor | n | Tumor site
|
|||||
|---|---|---|---|---|---|---|---|
| Frontal lobe | Occipital lobe | Temporal lobe | Parietal lobe | Cerebellum | Brain stem | ||
| Metastatic tumor | 9 | 1 | 2 | 3 | 3 | 4 | 1 |
| Meningioma | 7 | 4 | 1 | ||||
| Astrocytoma | 5 | 1 | 1 | 2 | 1 | ||
| Glioma | 3 | 3 | 1 | ||||
| Glioblastoma | 3 | 2 | 1 | ||||
| Acoustic neurinoma | 2 | ||||||
| Olfactory neuroepithelioma | 1 | 1 | |||||
| Pineal tumor | 1 | ||||||
| Choroid plexus papilloma | 1 | ||||||
| Total | 32 | 12 | 4 | 4 | 4 | 6 | 2 |
Table 4.
Primary cancer site of metastatic brain tumors
| Primary tumor | n |
|---|---|
| Lung | 4 |
| Prostate | 1 |
| Thyroid | 1 |
| Cervix | 1 |
| Stomach | 1 |
| Breast | 1 |
Although brain tumors and other forms of increased ICP are mainly diagnosed by MRI or CT, some conditions may involve elevated ICP despite normal imaging findings. These conditions can include IIH and CVST, each of which accounted for 6.9% of increased ICP in our present study (Table 2).
Three of the five patients with CVST were males aged primarily in their 40s. The etiology for three of these patients included a form of nephrotic syndrome, antiphospholipid syndrome and systemic lupus erythematosus. All three patients were diagnosed using standard MRI and MRV (Table 5).
Table 5.
Cerebral venous sinus thrombosis
| Patient number | Sex | Age (years) | Onset risk | Imaging modality |
|---|---|---|---|---|
| 1 | Male | 24 | Taking PSL for nephrotic syndrome | MRI + MRV |
| 2 | Male | 44 | Antiphospholipid syndrome | MRI + MRV |
| 3 | Male | 43 | None in particular | MRI + MRV |
| 4 | Male | 61 | None in particular | Angiography |
| 5 | Female | 44 | Taking PSL for SLE | MRI |
Abbreviations: PSL, prednisolone; MRI, magnetic resonance imaging; MRV, magnetic resonance venography; SLE, systemic lupus erythematosus.
Two of the five IIH patients were obese females of childbearing potential. After MRI confirmed the absence of intracranial lesions, the results of lumbar puncture demonstrated that all patients had noticeably elevated cerebrospinal fluid pressure (Table 6).
Table 6.
Idiopathic intracranial hypertension
| Patient number | Sex | Age (years) | Onset risk | MRI | Cerebrospinal fluid pressure (mmH2O) |
|---|---|---|---|---|---|
| 1 | Female | 14 | Obesity, SLE | Normal | 240 |
| 2 | Female | 34 | Obesity | Empty sella | 250 |
| 3 | Female | 53 | None | Normal | 330 |
| 4 | Male | 35 | Hypertension | Normal | 490 |
| 5 | Male | 67 | None | Normal | 370 |
Abbreviations: MRI, magnetic resonance imaging; SLE, systemic lupus erythematosus.
The etiology for seven of the ten bilateral uveitis patients was Vogt–Koyanagi–Harada disease, with the majority having redness and swelling of the optic nerves in both eyes as well as inflammation of the anterior chamber, macular edema, and serous retinal detachment (Table 7).
Table 7.
Causes of uveitis
| Disease | n | Anterior chamber inflammation (+) | ME or SRD (+) |
|---|---|---|---|
| Vogt–Koyanagi–Harada disease | 7 | 7 | 5 |
| Rheumatoid arthritis | 1 | 1 | 0 |
| Behçet’s disease | 1 | 0 | 0 |
| Unknown | 1 | 1 | 1 |
| Total | 10 | 9 | 6 |
Abbreviations: ME, macular edema; SRD, serous retinal detachment; (+), positive finding.
In terms of visual performance, the group of patients diagnosed with corrected distance visual acuity (CDVA) (0.05≥ LogMAR [logarithm of the minimum angle of resolution]) at the first consultation had pseudopapillitis, ADEM, optic disc drusen and leukemia, while the group with CDVA (0.2> LogMAR >0.05) had increased ICP and an unknown etiology. The group with CDVA (LogMAR ≥0.2) had uveitis, hypertensive retinopathy, and idiopathic optic neuritis, the latter of which was characterized by significantly reduced flicker values relative to the other diseases (Table 8).
Table 8.
Visual acuity/central flicker frequency
| Disease | n | First CDVA LogMAR right/left | First CDVA LogMAR min/max | CFF (red)
|
Final CDVA LogMAR right/left | |
|---|---|---|---|---|---|---|
| Right | Left | |||||
| Increased ICP | 72 | 0.10/0.15 | Blindness/0 | 34 | 33 | 0.10/0.10 |
| Uveitis | 19 | 0.40/0.30 | 2.40/0 | 32 | 34 | 0.10/0.22 |
| Pseudopapillitis | 10 | 0/0 | 0/0 | 39 | 39 | 0/0 |
| Hypertensive retinopathy | 6 | 0.22/0.40 | 0.82/0 | 31 | 29 | 0.05/0.15 |
| Optic neuritis | 2 | 0.10/0.40 | 0.70/0 | 26 | 14 | 0/0.10 |
| ADEM | 2 | 0.05/0 | 0.05/0 | 27 | 33 | 0/0 |
| Optic disc drusen | 2 | 0/0.05 | 0.05/0 | 33 | 28 | 0/0.05 |
| Leukemia | 1 | 0/0 | 0 | – | – | – |
| Unknown | 7 | 0.10/0.10 | 0.70/0 | 36 | 38 | 0/0 |
Abbreviations: LogMAR, logarithm of the minimal angle of resolution; CDVA, corrected distance visual acuity; CFF, central flicker frequency; ICP, intracranial pressure; ADEM, acute disseminated encephalomyelitis; min, minimum; max, maximum.
Discussion
We studied the etiology of patients initially confirmed with “bilateral disc swelling”. Increased ICP accounted for approximately 60% of the etiology while the remaining etiology was non-increased ICP diseases. Although many medical texts list the etiology of bilateral disc swelling, there have been no recently published studies that have listed the percentages of each etiology recorded at hospitals and clinics. Therefore, we compared our current findings to two studies that were published in 1971 and 1984, respectively.1,2 Results of this comparison indicated that increased ICP was the most common etiology observed at each study site, with optic neuritis, ADEM, and optic disc drusen only seen at our facility. It is possible, however, that these other studies may have intentionally excluded optic neuritis, among other etiologies. On the other hand, anemia, lead poisoning and thyroid ophthalmology were not observed within our department, but were seen at the other study sites (Table 9). Thyroid ophthalmology appears to have been excluded from the scope of our study, as it would have initially been classified at our facility as thyroid ophthalmology or compressive optic neuropathy, rather than bilateral disc swelling.
Table 9.
Previous studies on bilateral disc swelling
| Disease | Disease incidence (%)
|
||
|---|---|---|---|
| Duke 19711 | Matsumura (Nagasaki University) 19842 | Current | |
| Increased ICP | 91.9 | 54 | 59 |
| Pseudopapillitis | 0.3 | 0 | 16 |
| Uveitis | 3.6 | 0 | 8 |
| Hypertensive retinopathy | 0 | 18 | 5 |
| Optic neuritis | 0 | 0 | 2 |
| ADEM | 0 | 0 | 2 |
| Optic disc drusen | 0 | 0 | 2 |
| Leukemia | 0 | 9 | 1 |
| Anemia | 0.9 | 0 | 0 |
| Lead poisoning | 0.6 | 0 | 0 |
| Thyroid ophthalmology | 0 | 9 | 0 |
| Unknown | 2.2 | 9 | 6 |
| n | NA | 11 | 121 |
Abbreviations: NA, not applicable; ICP, intracranial pressure; ADEM, acute disseminated encephalomyelitis.
Walsh and Hoyt’s Clinical Neuro-Ophthalmology3 includes a description of the frequency of onset of bilateral disc swelling in various diseases. Specifically, papilledema was observed at the following frequencies: brain tumor, 80%; subdural hematoma, ≥50%; acute cerebral abscess, seven of 26 cases; chronic cerebral abscess, 15 of 23 cases; subarachnoid hemorrhage, 16% or 10%−24%; meningitis, 2.5% of 2,178 cases or 12 of 530 cases; viral encephalitis, 19% of 68 cases; and craniostenosis, 15% of 171 cases. Intra cranial pressure was elevated in 13 of 14 cerebral arteriovenous malformation patients, but disc swelling was only observed in three. With the exception of cerebral arteriovenous malformation (AVM) and encephalitis, all the diseases described above were seen in the results of the present study.
In children, optic neuritis is typically bilateral.4,5 Although our study found two adult patients with bilateral optic neuritis, the current study identified no children who presented with this condition. However, bilateral optic neuritis occurred in 13 children admitted to our hospital for treatment between 1999 and 2010.6 This was thought to be because only subjects with “bilateral disc swelling” were targeted in this study, and the disease name listed for these patients from the beginning was “bilateral optic neuritis”.
With regard to funduscopic differentiation between true optic disc edema (disc swelling) and pseudo optic disc edema (pseudopapillitis), Carta et al7 describe that peripapillary retinal folds seem to be related exclusively to optic disc edema. In our study, the diagnosis of pseudopapillitis was done with all normal patient indications of light reflex, visual acuity, critical frequency, and visual field.
One disease that typically involves elevated ICP despite normal CT or MRI findings is CVST. Thus, combining MRV with these standard imaging modalities would be useful when attempting to diagnose this condition. MRV can be used to confirm venous filling defects because it enables clear visualization of the major intracranial veins and cranial sinus without the use of a contrast agent.8
de Bruijn et al9 reported finding papilledema in 23 of 56 CVST patients (41%), with poor outcomes observed in those patients who presented with intracerebral hemorrhage or with some degree of impaired consciousness. Although previous studies have asserted that Behçet’s disease is complicated by CVST10,11 and Al-Fahad et al12 reported finding papilledema in eleven of 40 patients with neuro-Behçet’s disease (25.7%), none of the CVST patients in the present study had Behçet’s disease (Table 5).
Another representative disease that leads to intracranial hypertension, although general CT and MRI may appear normal, is IIH. This condition is generally said to occur commonly among obese women of reproductive age,13 but has also been reported in children and individuals aged ≥40 years.14–16 Thus, caution is warranted when examining patients over a wide range of age groups. Although follow-up may prove difficult in pediatric patients due to the inability to examine cerebrospinal fluid on a regular basis, several recent studies have determined that optical coherence tomography (OCT) may be an effective future modality for determining intracranial pressure via measurement of the retinal thickness.17–19 Headache has also been reported to be a frequent symptom of intracranial pressure.20 Even so, a study by De Simone et al21 described cases in which no headaches were present, suggesting the need for caution on the part of the diagnosing physician.
Furthermore, in a study on IIH and CVST by Lin et al22 106 patients diagnosed with IIH were further examined by MRV, which resulted in the discovery of CVST in ten of the patients (9.4%). Daif et al23 used angiography to examine cases previously diagnosed with IIH and reported finding 19 of 40 patients had CVST. These findings indicate that, when diagnosing IIH, it is essential to use MRV or other imaging techniques to rule out the possibility of CVST.
Conclusion
The most common etiology for bilateral disc swelling is intracranial pressure, but it can also be triggered by a variety of other causes. In studies of Japanese patients, pseudopapillitis is the most important differentiating disease. When attempting to diagnose the etiology of bilateral disc swelling, patients should be immediately examined for the possible influence of other diseases which increase intracranial pressure.
Footnotes
Disclosure
The authors report no conflict of interest in this work.
References
- 1.Duke-Elder S. System of Ophthalmology Vol XII: Neuro-ophthalmology. St Louis: Mosby; 1971. [Google Scholar]
- 2.Matsumura K, Mimura I, Murata M. Etiology of disc swelling at Nagasaki University in several years. Nagasaki University Neurology Journal. 1984;11:71–73. [Google Scholar]
- 3.Miller N. Walsh and Hoyt’s Clinical Neuro-Ophthalmology. 4th ed. Waverly Press; 1982. [Google Scholar]
- 4.Sri-udomkajorn S, Pongwatcharaporn K. Clinical features and outcome of childhood optic neuritis at Queen Sirikit National Institute of Child Health. J Med Assoc Thai. 2011;94(3):189–194. [PubMed] [Google Scholar]
- 5.Morales DS, Siatkowski RM, Howard CW, Warman R. Optic neuritis in children. J Pediatr Ophthalmol Strabismus. 2000;37:254–259. [PubMed] [Google Scholar]
- 6.Ogata C, Ichibe Y, Shimizu K. Optic neuropathy in childhood. Neuro-Ophthal Jpn. 2011;28:394–399. [Google Scholar]
- 7.Carta A, Favilla S, Prato M, Bianchi-Marzoli S, Sadun AA, Mora P. Accuracy of funduscopy to identify true edema versus pseudoedema of the optic disc. Invest Ophthalmol Vis Sci. 2012;53(1):1–6. doi: 10.1167/iovs.11-8082. [DOI] [PubMed] [Google Scholar]
- 8.Meckel S, Reisinger C, Bremerich J, Damm D, Wolbers M, Engelter S. Cerebral venous thrombosis: diagnostic accuracy of combined, dynamic and static, contrast-enhanced 4D MR venography. AJNR Am J Neuroradiol. 2010;31:527–535. doi: 10.3174/ajnr.A1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Bruijn SF, de Haan RJ, Stam J, Cerebral Venous Sinus Thrombosis Study Group Investigators Clinical features and prognostic factors of cerebral venous sinus thrombosis in a prospective series of 59 patients. J Neurol Neurosurg Psychiatry. 2001;70:105–108. doi: 10.1136/jnnp.70.1.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pamir MN, Kansu T, Erbengi A, Zileli T. Papilledema in Behçet’s syndrome. Arch Neurol. 1981;38:643–645. doi: 10.1001/archneur.1981.00510100071012. [DOI] [PubMed] [Google Scholar]
- 11.Wechsler B, Vidailhet M, Piette JC, Bousser MG, Dell Isola B, Blétry O, et al. Cerebral venous thrombosis in Behçet’s disease: clinical study and long-term follow-up of 25 cases. Neurology. 1992;42:614–618. doi: 10.1212/wnl.42.3.614. [DOI] [PubMed] [Google Scholar]
- 12.Al-Fahad SA, Al-Araji AH. Neuro-Behcet’s disease in Iraq: a study of 40 patients. J Neurol Sci. 1999;170(2):105–111. doi: 10.1016/s0022-510x(99)00165-3. [DOI] [PubMed] [Google Scholar]
- 13.Durcan FJ, Corbett JJ, Wall M. The incidence of pseudotumor cerebri. Population studies in Iowa and Louisiana. Arch Neurol. 1988;45:875–877. doi: 10.1001/archneur.1988.00520320065016. [DOI] [PubMed] [Google Scholar]
- 14.Phillips PH, Repka MX, Lambert SR. Pseudotumor cerebri in children. J AAPOS. 1998;2:33–38. doi: 10.1016/s1091-8531(98)90107-0. [DOI] [PubMed] [Google Scholar]
- 15.Zayit-Soudry S, Leibovitch I, Kesler A. Idiopathic intracranial hypertension after 40 years of age: Clinical features in 23 patients. Eur J Ophthalmol. 2008;18:989–993. doi: 10.1177/112067210801800621. [DOI] [PubMed] [Google Scholar]
- 16.Bandyopadhyay S, Jacobson DM. Clinical features of late-onset pseudo-tumor cerebri fulfilling the modified dandy criteria. J Neuroophthalmol. 2002;22:9–11. doi: 10.1097/00041327-200203000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Martinez MR, Ophir A. Optical coherence tomography as an adjunctive tool for diagnosing papilledema in young patients. J Pediatr Ophthalmol Strabismus. 2010;28:1–8. doi: 10.3928/01913913-20100719-05. [DOI] [PubMed] [Google Scholar]
- 18.Scott CJ, Kardon RH, Lee AG, Frisén L, Wall M. Diagnosis and grading of papilledema in patients with raised intracranial pressure using optical coherence tomography vs clinical expert assessment using a clinical staging scale. Arch Ophthalmol. 2010;128:705–711. doi: 10.1001/archophthalmol.2010.94. [DOI] [PubMed] [Google Scholar]
- 19.Skau M, Milea D, Sander B, Wegener M, Jensen R. OCT for optic disc evaluation in idiopathic intracranial hypertension. Graefes Arch Clin Exp Ophthalmol. 2010;249:723–730. doi: 10.1007/s00417-010-1527-2. [DOI] [PubMed] [Google Scholar]
- 20.Ball AK, Clarke CE. Idiopathic intracranial hypertension. Lancet Neurol. 2006;5:433–442. doi: 10.1016/S1474-4422(06)70442-2. [DOI] [PubMed] [Google Scholar]
- 21.De Simone R, Marano E, Bilo L, et al. Idiopathic intracranial hypertension without headache. Phalalgia. 2006;26:1020–1021. doi: 10.1111/j.1468-2982.2006.01138.x. [DOI] [PubMed] [Google Scholar]
- 22.Lin A, Foroozan R, Danesh-Meyer HV, De Salvo G, Savino PJ, Sergott RC. Occurrence of cerebral venous sinus thrombosis in patients with presumed idiopathic intracranial hypertension. Ophthalmol. 2006;113:2281–2284. doi: 10.1016/j.ophtha.2006.05.065. [DOI] [PubMed] [Google Scholar]
- 23.Daif A, Awada A, al-Rajeh S, et al. Cerebral venous thrombosis in adults. A study of 40 cases from Saudi Arabia. Stroke. 1995;26:1193–1195. doi: 10.1161/01.str.26.7.1193. [DOI] [PubMed] [Google Scholar]


