Abstract
PURPOSE
Telephone- and Internet-based communication are increasingly common in primary care, yet there is uncertainty about how these forms of communication affect demand for in-person office visits. We assessed whether use of copay-free secure messaging and telephone encounters was associated with office visit use in a population with diabetes.
METHODS
We used an interrupted time series design with a patient-quarter unit of analysis. Secondary data from 2008–2011 spanned 3 periods before, during, and after a patient-centered medical home (PCMH) redesign in an integrated health care delivery system. We used linear regression models to estimate proportional changes in the use of primary care office visits associated with proportional increases in secure messaging and telephone encounters.
RESULTS
The study included 18,486 adults with diabetes. The mean quarterly number of primary care contacts increased by 28% between the pre-PCMH baseline and the postimplementation periods, largely driven by increased secure messaging; quarterly office visit use declined by 8%. In adjusted regression analysis, 10% increases in secure message threads and telephone encounters were associated with increases of 1.25% (95% CI, 1.21%–1.29%) and 2.74% (95% CI, 2.70%–2.77%) in office visits, respectively. In an interaction model, proportional increases in secure messaging and telephone encounters remained associated with increased office visit use for all study periods and patient subpopulations (P <.001).
CONCLUSIONS
Before and after a medical home redesign, proportional increases in secure messaging and telephone encounters were associated with additional primary care office visits for individuals with diabetes. Our findings provide evidence on how new forms of patient-clinician communication may affect demand for office visits.
Keywords: primary care, electronic mail, telephone, communication, office visits, family practice, health services needs and demand, practice redesign, utilization, practice-based research
INTRODUCTION
Telephone- and Internet-based communication between patients and clinicians is associated with increased access to care,1,2 reduced hospitalizations in the chronically ill,3 and improved control of type 2 diabetes and hypertension in care management interventions.4,5 Besides offering potential clinical benefits, these care modalities do not require patients to incur the time, effort, or cost of traveling to clinicians’ offices,1,2 and the asynchronous nature of electronic messaging allows patients and clinicians to initiate communication at any time.6
For these and other reasons, leaders in American medicine7–10 have recommended that the locus of primary care and chronic care delivery expand beyond traditional office visits to include alternative modes of communication. There is considerable uncertainty, however, about how use of these new care modalities affects demand for traditional office visits.6 Although one early study found that telephone encounters were a substitute for follow-up visits at a Veterans Health Administration clinic,11 a Scottish trial found that telephone encounters for acute issues delayed—but did not preclude the need for—subsequent clinic visits.12 Findings on secure electronic messaging have also varied. While Zhou and colleagues13 found that office visit use decreased after introduction of an online portal at Kaiser Permanente Northwest (secure messaging was one of several portal tools), Palen and colleagues14 found that portal users at Kaiser Permanente Colorado had more office visits than propensity-matched controls during the year after portal registration.
We contribute to the evidence base in this area by examining how patients’ use of primary care office visits is associated with use of secure electronic messaging and telephone encounters in a large health care system that featured these care modalities in a patient-centered medical home (PCMH) redesign.15 Our primary objective in this natural experiment was to assess changes in office visit use associated with secure messaging threads and telephone encounters in a population with chronic illness. Our secondary objective was to investigate whether PCMH implementation or selected patient characteristics modify associations under study.
METHODS
Study Setting
We investigated the impact of secure messaging and telephone encounters on patients’ use of primary care office visits at Group Health, an integrated health plan and care delivery system in the Pacific Northwest. Since launching a secure online patient portal in 2000, Group Health added portal tools and engaged in multiple initiatives that encouraged copay-free secure electronic messaging and telephone encounters (secure electronic messaging began in 2002).16–18 Group Health further emphasized these care modalities during a 2007–2008 PCMH prototype redesign at a clinic,19 where chronically ill patients had 86% more secure message threads and 10% more telephone encounters than patients at other Group Health clinics.20
After the prototype redesign, Group Health implemented a systemwide PCMH redesign.19,21 Group Health staggered the beginning of the redesign across its 26 clinics from January to April 2009; PCMH implementation at each clinic lasted 1 year, followed by the postimplementation period. Secure messaging and telephone encounters were incorporated within overlapping PCMH redesign efforts to improve access, continuity, and follow-up.15,22
Study Design and Population
We used an interrupted time series design23 with a patient-quarter unit of analysis. We included data from January 2008 to December 2011, which encompassed 3 study periods: pre-PCMH baseline (4 quarters), PCMH implementation (4 quarters), and postimplementation (8 quarters). Group Health’s institutional review board approved all study protocols.
The study population included adults aged 18 to 75 years who received care at Group Health’s 26 clinics and had preexisting diabetes mellitus, based on a previously implemented case definition incorporating diagnostic, pharmacy, and laboratory data (Supplemental Appendix).20 We required continuous enrollment at Group Health during the baseline year and the first 2 quarters of PCMH implementation. We excluded patients with preexisting dementia. Individuals were censored from analysis after death, disenrollment from Group Health, or aging out of the 18 to 75 age range.
Measures
Using previously documented methods,21 we extracted automated data on health service use. Monthly primary care use data were rolled up to quarterly counts of office visits, secure message threads (a “thread” includes an original message between a patient and care team, and all messages in subsequent replies24), telephone encounters, and total primary care contacts (sum of office visits, secure message threads, and telephone encounters). We defined time-varying morbidity burden using resource utilization band (RUB) variables from Johns Hopkins Adjusted Clinical Groups (ACG) System case mix software.25 The Supplemental Appendix presents additional information on data collection and measurement.
Analysis
We computed descriptive statistics for patient characteristics and primary care use. We then estimated 2 multivariable linear regression models, with log-transformed independent and dependent variables,26,27 which estimated the proportional change in office visits associated with a proportional increase in each independent variable. Patients’ log-transformed quarterly office visit count was the dependent variable in both regression models. Before performing log transformation, we added a constant of 1 to quarterly counts of each primary care modality, which ensured transformation of uniformly positive data but did not interfere with desirable statistical properties of the log-normal distribution.28
Our first regression model (adjusted model) contained 2 key independent variables—log-transformed quarterly counts of secure message threads and telephone encounters—and adjusted for covariates. The second regression model (interaction model) adjusted for covariates and investigated potential effect modification through covariate-by-log-count interactions for study period and selected patient characteristics (age, sex, morbidity, insurance type, plan generosity, and primary care physician behaviors).
We estimated regression models using generalized estimating equations (GEE) with an autoregressive-1 (AR1) working correlation matrix for these longitudinal data, with robust “sandwich” covariance estimates that were robust to misspecification of within-cluster correlation.29 We fit a linear model to log-transformed visits with a normal error structure. Analyses were conducted using Stata, version 12.0 (StataCorp). Further details on regression model specification are presented in the Supplementary Appendix.
RESULTS
The study population consisted of 18,486 adults with diabetes who were aged 18 to 75 years on the first day of PCMH implementation (Table 1). As would be expected in a diabetic population, 70% were aged 55 years and older, and 34% had high or very high morbidity.
Table 1.
Patient Characteristics at PCMH Baseline and Primary Care Contacts During the Pre-PCMH Baseline Year
| Baseline Year Primary Care Contacts, Mean (SD), No. | ||||
|---|---|---|---|---|
|
|
||||
| Characteristic | Total No. (%) | Secure Message Threads | Telephone Encounters | Office Visits |
| Total population | 18,486 (100) | 3.5 (7.1) | 6.6 (8.2) | 3.7 (3.7) |
| Age-group | ||||
| 18–44 | 1,637 (9) | 3.5 (6.9) | 4.9 (6.0) | 3.5 (3.4) |
| 45–54 | 3,944 (21) | 3.5 (6.5) | 5.6 (7.1) | 3.6 (3.5) |
| 55–64 | 7,400 (40) | 3.7 (7.5) | 6.3 (7.8) | 3.6 (3.9) |
| 65–75 | 5,505 (30) | 3.4 (6.9) | 8.2 (9.7) | 4.0 (3.7) |
| Sex | ||||
| Female | 8,879 (48) | 3.7 (7.7) | 7.3 (8.8) | 4.0 (3.7) |
| Male | 9,607 (52) | 3.4 (6.5) | 6.0 (7.6) | 3.4 (3.7) |
| Morbidity (ACG RUB) | ||||
| Moderate | 12,073 (65) | 2.5 (4.4) | 4.1 (4.4) | 2.6 (2.1) |
| High | 3,963 (21) | 4.8 (9.0) | 8.4 (7.7) | 4.9 (3.3) |
| Very high | 2,450 (13) | 6.7 (11.7) | 15.7 (14.1) | 7.4 (6.6) |
| Insurance type | ||||
| Commercial | 11,924 (65) | 3.5 (6.4) | 5.4 (6.5) | 3.4 (3.4) |
| Medicaid/state subsidized | 408 (2) | 2.2 (5.4) | 5.5 (5.9) | 3.7 (3.2) |
| Medicare | 6,154 (33) | 3.7 (8.3) | 8.9 (10.5) | 4.3 (4.2) |
ACG = adjusted clinical groups; PCMH = patient-centered medical home; RUB = resource utilization band.
In the population overall, use of secure messaging and telephone encounters steadily increased over the study period, while use of office visits declined slightly (Figure 1). The mean quarterly number of office visits declined from 0.93 (SD = 0.93) visits during baseline to 0.90 (SD 0.97) visits during PCMH implementation and 0.86 (SD 0.89) visits during postimplementation (8% total decrease). Largely driven by increased secure messaging, the mean quarterly number of primary care contacts increased from 3.46 (SD 3.48) contacts to 3.95 (SD 4.33) and 4.44 (SD 4.68) contacts, respectively (28% total increase).
Figure 1.
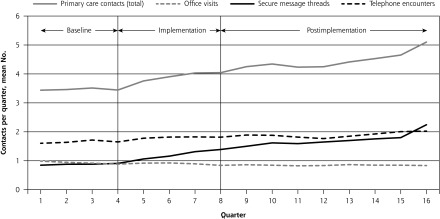
Quarterly numbers of primary care contacts between care teams and patients with diabetes during baseline, PCMH implementation, and postimplementation periods.
PCMH = patient-centered medical home.
In regression analysis, increased use of either secure messaging or telephone encounters was associated with increased office visit use (Table 2). The adjusted model yielded estimates that a 10% increase in secure message threads was associated with a 1.25% increase in office visits (95% CI, 1.21%–1.29%), and that a 10% increase in telephone encounters was associated with a 2.74% increase in office visits (95% CI, 2.70%–2.77%).
Table 2.
Changes in Office Visits Associated With Proportional Increases in Secure Message Threads and Telephone Encounters
| Model and Variable | Change With 10% Increase in Secure Messaging Threads % (95% CI) | Change With 10% Increase in Telephone Encounters % (95% CI) |
|---|---|---|
| Adjusted modela | ||
| Full study population | 1.25 (1.21–1.29) | 2.74 (2.70–2.77) |
| Interaction modela | ||
| Study period | ||
| Baseline | 1.13 (0.89–1.38) | 2.93 (2.70–3.15)b |
| PCMH implementation (Ref) | 1.14 (0.93–1.35) | 2.74 (2.55–2.93) |
| Postimplementation | 1.20 (0.98–1.41) | 2.57 (2.38–2.77)c |
| Age-group, y | ||
| 18–44 | 1.28 (1.03–1.53) | 2.93 (2.70–3.17)b |
| 45–54 | 1.21 (0.99–1.43) | 2.94 (2.74–3.14)b |
| 55–64 (Ref) | 1.14 (0.93–1.35) | 2.74 (2.55–2.93) |
| 65–75 | 1.22 (0.93–1.50) | 2.81 (2.56–3.06) |
| Sex | ||
| Female (Ref) | 1.14 (0.93–1.35) | 2.74 (2.55–2.93) |
| Male | 1.18 (0.97–1.39) | 2.62 (2.43–2.81)c |
| Morbidity burden (ACG RUB) | ||
| Moderate (Ref) | 1.14 (0.93–1.35) | 2.74 (2.55–2.93) |
| High | 0.84 (0.62–1.06)c | 2.66 (2.46–2.86)c |
| Very high | 0.69 (0.45–0.93)c | 2.72 (2.51–2.93) |
| Insurance type | ||
| Commercial (Ref) | 1.14 (0.93–1.35) | 2.74 (2.55–2.93) |
| Medicaid/state-subsidized | 1.00 (0.63–1.38) | 3.16 (2.83–3.48)b |
| Medicare | 0.96 (0.68–1.23) | 2.78 (2.53–3.03) |
ACG = adjusted clinical group; PCMH = patient-centered medical home; Ref = referent category; RUB=resource utilization band.
Note: Results are from log-linear regression models.
Adjusted for age, sex, morbidity burden, insurance type, clinician network, well-care waiver, pharmaceutical coverage, education, income, baseline secure messaging use, hemoglobin A1c level, blood pressure, low-density lipoprotein cholesterol level, study period, calendar quarter, physician secure messaging, and physician telephone encounter use.
Positive effect modification at P ≤.05, compared with referent category.
Negative effect modification at P ≤.05, compared with referent category.
Interaction model results demonstrated some variation across study periods and patient subpopulations, but not to an extent that changed inference (Table 2). The association between log-transformed office visits and telephone encounters decreased over time; using the implementation period as the referent, it was highest during pre-PCMH baseline (P = .01) and decreased further during postimplementation (P <.001). In addition, characteristics such as morbidity and insurance type were associated with statistically significant modifications of main effects. Despite observed interaction effects, linear combinations of coefficients for all study periods and for patient subpopulations in the interaction model were positive at P <.001.
DISCUSSION
In an adult patient population with diabetes, proportional increases in telephone encounters and, to a lesser extent, secure message threads, were associated with proportional increases in primary care office visits. In an interaction model, results varied modestly across selected patient characteristics, and the positive association between log-transformed numbers of office visits and telephone encounters attenuated over time. Although unadjusted office visit use declined by 8% in the study population, patient-level regression analyses demonstrated that a proportional increase in patients’ telephone encounters or secure messaging was associated with additional office visits for all study periods and patient subpopulations.
It is not surprising that we observed positive associations between alternative care modalities and office visits in this setting. During its PCMH redesign, Group Health placed no constraints—financial or otherwise—on secure messaging or telephone use. Primary care clinicians may have selectively used secure messages and telephone encounters to curtail demand for office visits, but these communication modes probably stimulated some demand by reducing access barriers and allowing patients to address previously unmet needs. Although secure messaging and telephone encounters may facilitate patients’ self-management of diabetes,1,2 they cannot fully substitute for clinical tasks such as in-person foot and eye examinations30 and physical examinations.1 Our observational results, like recent findings from Palen and colleagues,14 do not support the hypothesis that, in general, chronically ill patients will use new forms of copay-free communication as an alternative to in-person visits.
This study has several limitations. We did not conduct content analyses of individual primary care contacts, and we did not identify whether a patient or clinician initiated each contact. We could not control for behaviors of nonphysician clinicians, such as medical assistants and nurses, and observed associations cannot be interpreted as causal effects. The study population was limited to individuals with diabetes who were universally insured and of relatively high socioeconomic status, limiting generalizability. Secure electronic messaging and telephone encounters had been conducted at Group Health for several years, facilitating high adoption rates that may be unique to this setting. Group Health’s salary-based clinician reimbursement and capitation-based financing probably affected observed care delivery and patterns of use. In addition, although we adjusted for multiple demographic and clinical characteristics, we could not explicitly adjust for patients’ propensity to seek medical advice and treatment.
Our findings point to several opportunities for further exploration. Pragmatic trials should assess whether telephone and secure messaging encounters can reduce or delay use of emergency and inpatient services. As primary care is increasingly delivered by clinician teams that communicate with patients outside traditional office visit settings, new definitions of primary care use—and accompanying new payment models—are needed to encapsulate and reward patient-centered care delivery.
In conclusion, we found that use of secure electronic messaging and use of telephone encounters were associated with additional primary care office visits among individuals with diabetes in a PCMH redesign. Our findings provide evidence on how new forms of patient-clinician communication may affect demand for office visits.
Acknowledgments
Clarissa Hsu, PhD, DeAnn Cromp, MPH, Kelly Ehrlich, MS, and Eric Johnson, MA, assisted with analysis planning and manuscript preparation. Dean Roehl, MD, and Deborah Brown, RN, shared information about protocols in the medical home redesign and clinician experiences at Group Health. James Ralston, MD, provided helpful feedback on an early draft. We thank Claire Trescott, MD, and Michael Erikson, MSW, for their leadership during the medical home redesign at Group Health.
Footnotes
Conflicts of interest: Drs Fishman, Rutter, and Reid and Mr Ross are employees and Dr Liss is a former employee of Group Health Cooperative. Dr Reid is an employee and shareholder of Group Health Physicians, the medical group affiliated with Group Health Cooperative.
Funding support: Funding was provided by the National Center for Advancing Translational Sciences (TL1 RR025016), the Agency for Healthcare Research and Quality (R18 HS019129), and Group Health Cooperative.
Previous presentation: Preliminary findings were presented at the Clinical and Translational Sciences Predoctoral Programs Meeting in Rochester, Minnesota, May 8, 2012.
Supplementary materials: Available at http://www.AnnFamMed.org/content/12/4/338/suppl/DC1/
References
- 1.Car J, Sheikh A. Email consultations in health care: 1—scope and effectiveness. BMJ. 2004;329(7463):435–438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Car J, Sheikh A. Telephone consultations. BMJ. 2003;326(7396): 966–969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown RS, Peikes D, Peterson G, Schore J, Razafindrakoto CM. Six features of Medicare coordinated care demonstration programs that cut hospital admissions of high-risk patients. Health Aff (Millwood). 2012;31(6):1156–1166 [DOI] [PubMed] [Google Scholar]
- 4.Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, Web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA. 2008;299(24):2857–2867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ralston JD, Hirsch IB, Hoath J, Mullen M, Cheadle A, Goldberg HI. Web-based collaborative care for type 2 diabetes: a pilot randomized trial. Diabetes Care. 2009;32(2):234–239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McGeady D, Kujala J, Ilvonen K. The impact of patient-physician web messaging on healthcare service provision. Int J Med Inform. 2008;77(1):17–23 [DOI] [PubMed] [Google Scholar]
- 7.Margolius D, Bodenheimer T. Transforming primary care: from past practice to the practice of the future. Health Aff (Millwood). 2010;29(5):779–784 [DOI] [PubMed] [Google Scholar]
- 8.Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the Twenty-First Century. Washington, DC: Institute of Medicine; 2001 [Google Scholar]
- 9.Bates DW, Wells S. Personal health records and health care utilization. JAMA. 2012;308(19):2034–2036 [DOI] [PubMed] [Google Scholar]
- 10.Wagner EH, Coleman K, Reid RJ, Phillips K, Abrams MK, Sugarman JR. The changes involved in patient-centered medical home transformation. Prim Care. 2012;39(2):241–259 [DOI] [PubMed] [Google Scholar]
- 11.Wasson J, Gaudette C, Whaley F, Sauvigne A, Baribeau P, Welch HG. Telephone care as a substitute for routine clinic follow-up. JAMA. 1992;267(13):1788–1793 [PubMed] [Google Scholar]
- 12.McKinstry B, Walker J, Campbell C, Heaney D, Wyke S. Telephone consultations to manage requests for same-day appointments: a randomised controlled trial in two practices. Br J Gen Pract. 2002;52(477):306–310 [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou YY, Garrido T, Chin HL, Wiesenthal AM, Liang LL. Patient access to an electronic health record with secure messaging: impact on primary care utilization. Am J Manag Care. 2007;13(7):418–424 [PubMed] [Google Scholar]
- 14.Palen TE, Ross C, Powers JD, Xu S. Association of online patient access to clinicians and medical records with use of clinical services. JAMA. 2012;308(19):2012–2019 [DOI] [PubMed] [Google Scholar]
- 15.Hsu C, Coleman K, Ross TR, et al. Spreading a patient-centered medical home redesign: a case study. J Ambul Care Manage. 2012; 35(2):99–108 [DOI] [PubMed] [Google Scholar]
- 16.Ralston JD, Coleman K, Reid RJ, Handley MR, Larson EB. Patient experience should be part of meaningful-use criteria. Health Aff (Millwood). 2010;29(4):607–613 [DOI] [PubMed] [Google Scholar]
- 17.Ralston JD, Carrell D, Reid R, Anderson M, Moran M, Hereford J. Patient web services integrated with a shared medical record: patient use and satisfaction. J Am Med Inform Assoc. 2007;14(6):798–806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ralston JD, Martin DP, Anderson ML, et al. Group Health Cooperative’s transformation toward patient-centered access. Med Care Res Rev. 2009;66(6):703–724 [DOI] [PubMed] [Google Scholar]
- 19.Reid RJ, Coleman K, Johnson EA, et al. The Group Health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff (Millwood). 2010;29(5):835–843 [DOI] [PubMed] [Google Scholar]
- 20.Liss DT, Fishman PA, Rutter CM, et al. Outcomes among chronically ill adults in a medical home prototype. Am J Manag Care. 2013;19(10):e348–e358 [PMC free article] [PubMed] [Google Scholar]
- 21.Reid RJ, Fishman PA, Yu O, et al. Patient-centered medical home demonstration: a prospective, quasi-experimental, before and after evaluation. Am J Manag Care. 2009;15(9):e71–e87 [PubMed] [Google Scholar]
- 22.Reid RJ, Larson EB. Improvement happens: doctors talk about the medical home. An interview with Charles Mayer, MD, MPH and Eric Seaver, MD. J Gen Intern Med. 2012;27(7):871–875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shadish WR, Cook TD, Campbell DT. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. Boston, MA: Houghton Mifflin; 2002 [Google Scholar]
- 24.Carrell D, Ralston J. Messages, strands and threads: measuring use of electronic patient-provider messaging. AMIA Annu Symp Proc. 2005:913 [PMC free article] [PubMed] [Google Scholar]
- 25.The Johns Hopkins ACG System: Technical Reference Guide, Version 10.0. Baltimore, MD: Johns Hopkins University; 2011 [Google Scholar]
- 26.McFadden D. Constant elasticity of substitution production functions. Rev Econ Stud. 1963;30(2):73–83 [Google Scholar]
- 27.Gujarati DN. Essentials of Econometrics. 3rd ed New York, NY: McGraw-Hill/Irwin; 2006 [Google Scholar]
- 28.Duan N. Smearing estimate: a nonparametric retransformation method. J Am Stat Assoc. 1983;78(383):605–610 [Google Scholar]
- 29.Diggle P, Heagerty P, Liang K, Zeger S. Analysis of Longitudinal Data. 2nd ed Norfolk, United Kingdom: Oxford University Press; 2002 [Google Scholar]
- 30.Executive summary: Standards of medical care in diabetes—2013. Diabetes Care. 2013;36(Suppl 1):S4–S10 [DOI] [PMC free article] [PubMed] [Google Scholar]


