Abstract
STUDY DESIGN
Secondary analysis of a cohort enrolled in a prospective, randomized, longitudinal clinical trial.
OBJECTIVES
The single-step test (SST) was evaluated to assess its intertester reliability, validity as a test of activity limitation, and responsiveness to change for patients after unilateral total knee arthroplasty (TKA). The SST was also examined to determine whether it could differentiate between the surgical and nonsurgical lower limbs of patients after unilateral TKA and between the surgical limbs of patients after TKA and the limbs of healthy controls.
BACKGROUND
Tests of functional ability for patients recovering from TKA cannot differentiate the contribution of each limb to performance outcome. A test of unilateral limb ability would provide a metric for assessing the surgical lower extremity, without the confounder of the status of the contralateral lower extremity.
METHODS
Intertester reliability was assessed between clinicians and between a clinician and a switch mat. Patients who underwent unilateral TKA were tested at initial outpatient physical therapy evaluation, at 3 months after TKA, and at 1 year after TKA.
RESULTS
The assessment of function with the SST was determined to be reliable between testers when using a stopwatch. SST times were significantly correlated with other measures of lower extremity functional performance, providing evidence of its validity in patients after TKA. The SST was responsive to treatment in patients after TKA, with improvements in time for test completion. Performance on the SST also differed between limbs of patients after TKA and when comparing the limbs of healthy controls to those of patients after TKA.
CONCLUSION
The SST is a reliable measure between testers and a valid and responsive test of activity limitations when assessing unilateral lower extremity impairments in patients after TKA.
Keywords: function, joint replacement, knee, osteoarthritis
Total knee arthroplasty (TKA) procedures for the treatment of end-stage osteoarthritis (OA) are expected to grow to 3.48 million annually in the United States by the year 2030.14 The increased rate of these procedures has generated greater interest in improving the treatment and recovery of patients who undergo TKA. A clinician’s ability to objectively monitor the efficacy of a treatment requires reliable outcome measures that can be tracked over time. In general, clinical evaluation of patients’ functional abilities is determined through functional tests. Performance in clinical tests of function, such as the timed up-and-go (TUG),31 6-min ute walk (6MW),27 and stair-climbing test (SCT),1,12 provides insight into physical ability and is the standard measure of functional performance in an elderly population. Though these clinical performance tests provide a measure of global lower extremity function,1,10,12,16,22 they do not provide clinicians with insight into the ability of each limb independently or a means to differentiate between limbs.
Recent work has demonstrated that the integrity of the contralateral limb is central to predicting long-term bilateral functional ability after TKA.38 Additionally, the high likelihood of developing OA in the contralateral limb30 suggests that there may be a need for a test of unilateral limb ability that can provide clinicians with a metric for independently assessing recovery and response to treatment of both the operated and nonoperated limbs of patients following unilateral TKA. An assessment of unilateral activity limitations would provide clinicians with a deeper insight into a patient’s functional capacity, while also allowing the clinician to monitor changes in the nonsurgical limb, which is at high risk for developing knee OA.18,30 Current functional tests for evaluating each limb independently, such as single-leg hopping tests28 or unilateral squat jumping,6 are appropriate for healthy young adults and athletes but may not be appropriate or safe for older populations, particularly of patients recovering from TKA. Furthermore, other unilateral tests, such as the step-down test, are commonly used to evaluate quality of movement15,26 or to assess pain during stepping in patients with patellofemoral pain syndrome17,25 but do not provide a metric of activity limitations and are not commonly used in patients after TKA.
Impairments of the quadriceps are associated with poorer performance in functional activities such as walking and climbing stairs.20 The single-step test (SST) was developed as a test of unilateral limb ability and involves the use of a single limb to raise and lower the body from the ground to a step and back down, combining concentric and eccentric actions of the quadriceps. The aim of this investigation was to assess the intertester reliability, validity, and responsiveness of the SST in patients after TKA. The intertester reliability and measurement accuracy of the SST were assessed by comparing measurements between testers and against a gold standard for recording timing data. Validity was determined by comparing SST performance between the surgical and nonsurgical limbs of patients after TKA, and between the limbs of patients after TKA and the limbs of individuals without knee OA. Additionally, validity was assessed by comparing the performance of the SST with that of clinic-based, functional performance measures in the same subjects. Responsiveness was determined by evaluating the change in SST performance from before to after outpatient physical therapy treatment of the surgical limb in patients who underwent TKA.
We hypothesized that the SST would be assessed as reliable between testers and against a gold standard for measuring timing variables. Furthermore, the SST would be a valid measure of activity limitations that would (a) distinguish between the limbs of patients after unilateral TKA, (b) distinguish between the limbs of patients with TKA and those of healthy controls, and (c) exhibit moderate correlations with clinic-based, functional performance measures. Lastly, we hypothesized that SST performance would be responsive to change during the course of postoperative outpatient physical therapy treatment.
METHODS
Subjects
Three different subject samples were assessed with the SST to meet the aims of the study: a bilateral TKA group, a unilateral TKA group, and a healthy control group. Exclusion criteria for all 3 samples were body mass index greater than 40 kg/m2 (very severe obesity)36 or a history of cardiovascular disease, diabetes, or uncontrolled high blood pressure. The bilateral TKA group was used to determine the interrater reliability and accuracy of recording the timing of the SST.
The SST was implemented in a randomized clinical trial that compared the effects of progressive strength training with progressive strength training combined with neuromuscular electrical stimulation on recovery after TKA.24 The data presented for validity, responsiveness, and comparison across limbs were obtained from individuals who underwent unilateral TKA, where subjects were also excluded if they had pain in the contralateral knee (defined as knee pain of 4 or greater on a 10-point verbal analog scale) or any other lower extremity pathologies that interfered with their functional abilities. The healthy control group was composed of 61 individuals without knee OA, who were recruited through advertisements in local papers and by word of mouth. Informed consent was given by each subject prior to participation, and the rights of the subjects were protected. The study and inclusion of the SST were approved by the University of Delaware Human Subjects Review Board, and all procedures were in accordance with the Declaration of Helsinki.
Subjects were assessed with a battery of tests during the initial postoperative outpatient physical therapy evaluation (IE), which took place approximately 4 weeks after the operation, at 3 months after TKA, and at 1 year after TKA.
Rehabilitation Protocol
The rehabilitation protocol was completed at the University of Delaware Physical Therapy Clinic. Subjects were treated in the physical therapy clinic 2 to 3 times per week for 6 weeks, for an average of 17 sessions. All subjects received rehabilitation focused on progressive quadriceps strengthening, including strategies to reduce pain and swelling, improve knee extension and flexion range of motion, improve patellar mobility, and maximize function.33 Some subjects also received neuromuscular electrical stimulation to augment the quadriceps strengthening program.
Single-Step Test
For the SST, subjects were asked to stand on a block (15 cm), weight bearing on the test limb only. With the non–weight-bearing limb held straight by a knee immobilizer brace, subjects were asked to squat, using the test limb to touch the heel of the non–weight-bearing limb to the floor, and return to touch the step (FIGURE 1). The total time needed to complete 20 repetitions of the movement was recorded and used in the analyses. As a safety precaution, the subjects’ hands rested on top of the investigator’s hands, with instructions that the investigator was only to be used in the event of a loss of balance. The trial was not counted if the patient used the investigator for sustained support. A coin toss was used to randomly determine the order of testing for the 2 limbs, and time was recorded manually using a handheld stopwatch.
FIGURE 1.
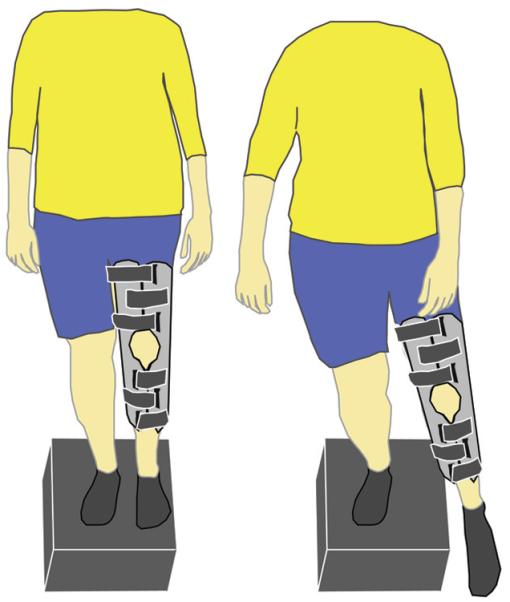
Schematic depicting the single-step test. The test leg is on a 15-cm block and the other leg is in a knee immobilizer to minimize its contribution to the task. Subjects were asked to touch the heel of the nontest leg to the floor, then back to the block 20 times, as fast as possible.
Performance Measures
The functional measures used for comparison were the SCT,4,5 the 6MW test,9,22 and the TUG test.22,27 The SCT required the patient to ascend and descend a standard flight of stairs (12 steps at 7.9 cm per step) as quickly and safely as possible. Patients were permitted the use of a single handrail, if necessary. The 6MW test required patients to walk as safely and as fast as they could around a designated pathway (157.3 m) for 6 minutes. The total distance traveled was then recorded and used in the analyses. The TUG test required patients to rise from a seated position in a chair (46 cm in height, with armrests and back support), to walk to a line on the ground 3 m away, and to return and sit in the chair, as fast as possible. For the SCT and the TUG test, subjects completed 2 trials. The average time from the 2 trials was used in the analyses. These tests were chosen because they are well established functional performance measures for patients after TKA.2,11,24
Data Analyses
Interrater reliability and the accuracy of using a stopwatch to record the time needed to complete the SST were assessed with an initial sample of 6 subjects who underwent bilateral TKA. Their data were examined prior to implementation of the measure in the clinical trial and separately from the secondary analysis of the data from the 146 participants who comprised the main group of this report.
Interrater reliability of the SST was examined by calculating the intraclass correlation coefficient (ICC2,1) for data from 2 clinicians who simultaneously timed the 6 patients who performed the test. The accuracy of the raters’ use of the stopwatches was evaluated by comparing a clinician’s manually recorded times to those recorded by a 47 × 60-cm switch mat (model 14H; Recora Inc, Batavia, IL), a pressure-sensitive device connected to an analog-to-digital board, with custom-written software to record performance time based on contact with the ground of the non–weight-bearing limb. These data were also assessed using ICC2,1.
Pearson correlation coefficients were calculated to determine the relationship between performance on the SST and performance on standard functional measures (TUG, SCT, and 6MW). Correlations were defined as being moderate if between 0.3 and 0.5 and large if greater than 0.5.4 Because the patients studied had unilateral OA and the chosen tests of function are standard for evaluating this population, correlations between the SST and these clinic-based performance measures were appropriate for validating this unilateral test. A large correlation with these measures was therefore used to represent convergent validity (r>0.5).
Responsiveness of the SST to identify change in the patients’ unilateral limb ability was assessed by evaluating the change in SST from IE through 3 months, as this was the period in which the greatest change in function was expected,2,19 and between IE and 1 year. Due to missing data for some subjects at different time points, separate linear mixed models were performed for each variable (SCT, TUG, 6MW, and SST) to precisely estimate the means and standard deviations for the given sample, had it been a complete data set. Mixed-model regression analyses were performed, with time as a fixed effect. A type 3 sum-of-squares assumption was used to account for missing data, and the maximal likelihood estimations were calculated through 1000 iterations. The issue of baseline variability of the IE measures was accounted for in the regression model by the inclusion of an intercept term. The effect-size indexes (ESIs) were calculated by dividing the estimated marginal means obtained from a linear mixed model by the standard deviations from the IE assessment.
To maintain sample-size equivalence across observations, data from 102 patients (of the 146 enrolled in the study) who completed testing at all 3 time points were used for the final analysis. A 3-by-2 repeated-measures analysis of variance (3 levels for the factor time, 2 levels for the factor limb) was performed for the SST measures to investigate changes over time and between limbs from the initial physical therapy assessment 1 month after surgery through 3 months after and 1 year after TKA. In the presence of a main effect, paired t tests were performed to identify differences between limbs and changes over time. The significance levels were initially set at .05. Bonferroni corrections were applied for the 7 within-limb and between-limb comparisons over time (2 for each limb over time and 3 between limbs), changing significance to α = .007.
Finally, independent t tests were used to compare the SST performance times at each of the 3 time points (IE, 3 months, and 1 year) for the surgical limbs of patients to the limbs of control subjects. The Levene test for equality of variances was conducted and, when significant, P values for equal variances not assumed were reported. The Bonferroni-adjusted significance level was adjusted for 6 comparisons (each limb at each time point), changing the significance level to α = .008.
RESULTS
Subjects
The reliability group contained 6 subjects (mean ± SD age, 68.8 ± 5.9 years; 1 woman). The data for the unilateral TKA group were from participants in a randomized clinical trial of 189 subjects with TKA; however, only 146 of these were assessed with the SST, as this test was added after the start of the trial (mean ± SD age, 64.9 ± 8.6 years; 77 women; time from surgery to IE, 27.7 ± 3.8 days). There were no differences between the 2 groups examined in the clinical trial (those who received neuromuscular electrical stimulation and those who did not) for any of the primary or secondary outcomes, including SST performance (independent-samples t tests comparing limbs of training groups at each time point) (P = .281); therefore, for this analysis, the groups were combined. One subject’s performance at IE (182.2 seconds) was more than 13 standard deviations from the mean (mean ± SD, 33.5 ± 11.5 seconds) and was, therefore, deemed an outlier and removed from further analysis.
The control group contained 61 individuals without knee OA (mean ± SD age, 63.0 ± 8.5 years; 35 women), in whom the same proportion of right and left limbs (56% right, n = 34) as that in the TKA group were examined.
Reliability and Validity of the SST
The intertester reliability ICC2,1 for our clinic, when 2 examiners assessed performance in the SST, was 0.999. The ICC2,1 for the accuracy of measurement of the SST between the manually recorded times and those from the switch mat was 0.999 and 0.996 for the 2 testers, respectively.
Convergent validity between the SST and the clinic-based performance tests in patients after unilateral TKA was demonstrated by the magnitude of the correlations between SST performance and performance on the SCT, TUG test, and 6MW test at each time point (IE, 3 months, and 1 year) for the surgical limb, and by correlations between change scores for these measures (TABLE 1).
TABLE 1.
Correlation Coefficients for Single-Step-Test Performance Times and Change Scores Using the Surgical Limb and Performance of the SCT, 6MW, and TUG by Evaluation Period*
| Test | IE | 3 mo | 1 y | Change From IE to 3 mo | Change From IE to 1 y |
|---|---|---|---|---|---|
| SCT | 0.63 (0.52, 0.72); 135 | 0.68 (0.59, 0.76); 143 | 0.71 (0.61, 0.79); 123 | 0.50 (0.36, 0.62); 125 | 0.45 (0.29, 0.59); 108 |
| TUG | 0.61 (0.50, 0.71); 135 | 0.58 (0.46, 0.68); 143 | 0.72 (0.62, 0.80); 123 | 0.45 (0.30, 0.58); 125 | 0.49 (0.33, 0.61); 108 |
| 6MW | −0.62 (−0.72, −0.51); 129 | −0.58 (−0.68, −0.46); 139 | −0.66 (−0.75, −0.54); 117 | −0.46 (−0.31, −0.59); 120 | −0.47 (−0.30, −0.61); 98 |
Abbreviations: 6MW, 6-minute walk; IE, initial outpatient physical therapy evaluation; SCT, stair-climbing test; TUG, timed up-and-go.
Values are intraclass correlation coefficient (95% confidence interval); n. All correlation coefficients, including correlations between change scores, were significant (P≤.001), except those of the 6MW (change from IE to 3 mo, P = .01; change from IE to 1 y, P>.05).
Responsiveness
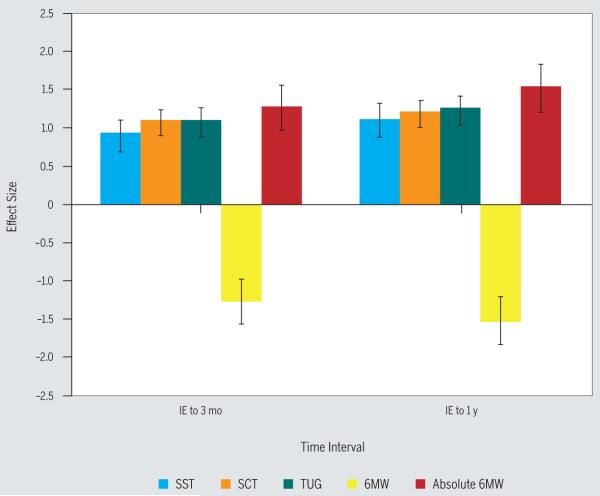
The ability of the SST to measure change over time in patients after unilateral TKA was demonstrated by the effect sizes of 0.90 for the interval of IE to 3 months and 1.10 for the interval of IE to 1 year. When comparing the confidence intervals of the ESIs for the SCT (1.07), TUG test (1.08), and 6MW test (−1.27), none of the confidence intervals included zero, and all ESIs indicated improvements in performance over time for both the intervals of IE to 3 months and IE to 1 year, suggesting that the responsiveness between the SST, SCT, TUG test, and 6MW test (absolute values were used due to the direction of change) was not different (FIGURE 2).5
FIGURE 2.
Effect-size index for changes from IE to 3 months after surgery and to 1 year after surgery, with 95% confidence intervals, for the SST, SCT, TUG, and 6MW. The effect size for the 6MW was negative; for comparison among measures, the absolute effect size is presented. Abbreviations: 6MW, 6-minute walk; IE, initial postoperative physical therapy evaluation; SCT, stair-climbing test; SST, single-step test; TUG, timed up-and-go.
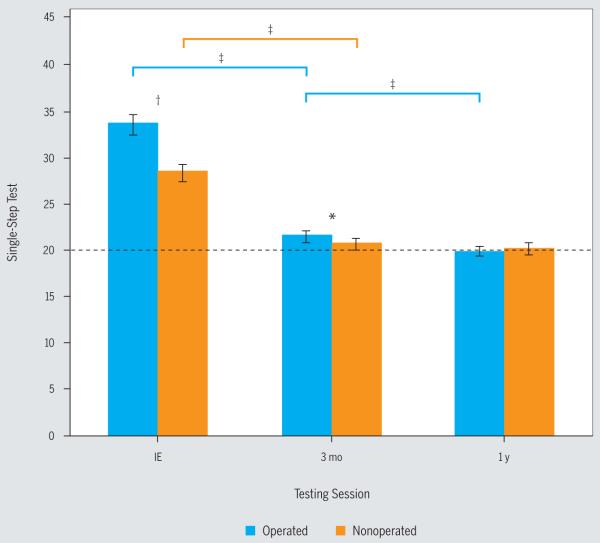
Performance of SST After TKA
The repeated-measures analysis of variance for the SST revealed a significant interaction effect (F = 49.8, df = 1.25, P<.001). SST times were significantly longer for the surgical limb compared to the nonsurgical limb at IE (mean difference, 5.2 seconds; t = 7.2, df = 101, P<.001), as well as at 3 months (mean difference, 1.1 seconds; t = 3.0, df = 101, P = .004). There were no differences between limbs at 1 year (mean difference, −0.1 seconds; t = –0.6, df = 101, P = .575).
Surgical Limb Over Time
Pairwise comparisons of the surgical limb over time confirmed that SST performance times at IE were statistically longer (mean ± SD, 33.5 ± 11.5 seconds) than those at 3 months (21.8 ± 6.1 seconds; mean change, 11.7 seconds; t = 13.5, df = 101, P<.001). Performance times of the SST with the surgical limb at 3 months were also significantly longer than performance times at 1 year (20.0 ± 4.9 seconds; mean change, 1.8 seconds; t = 6.2, df = 101, P<.001) (FIGURE 3).
FIGURE 3.
Changes in single-step-test performance (n = 102) between limbs and across time for patients who underwent unilateral total knee arthroplasty. Testing was completed at IE and at 3 months and at 1 year after surgery. The broken line indicates mean performance time for the control subjects. Blue lines indicate differences in the operated limb and orange lines indicate differences in the nonoperated limb. *Significant difference between limbs (P = .004). †Significant difference between limbs (P<.001). ‡Significant difference over time (P<.001). Abbreviation: IE, initial postoperative physical therapy evaluation.
Nonsurgical Limb Over Time
SST performance times for the nonsurgical limb at IE (mean ± SD, 28.3 ± 9.6 seconds) were longer compared to 3 months (20.7 ± 6.0 seconds; mean change, 7.7 seconds; t = 11.2, df = 101, P<.001). The performance times at 3 months were not significantly different from those at 1 year (mean ± SD, 20.1 ± 5.7 seconds; mean change, 0.6 seconds; t = 1.6, df = 101, P = .123) (FIGURE 3).
Comparisons to Controls
SST performance times of the surgical limbs of patients who underwent unilateral TKA were significantly prolonged compared to those of the matched limbs of healthy control subjects (mean ± SD, 19.7 ± 5.4 seconds) at IE (mean difference, 13.6 seconds; t = 10.1, df = 182.3, P<.001) and at 3 months (mean difference, 3.0 seconds; t = 2.8, df = 124.1, P = .007), when equal variances were not assumed (TABLE 2). However, there was no significant difference between groups at 1 year (mean difference, 0.6 seconds; t = 0.6, df = 102.0, P = .513). Similarly, SST performance times of the nonsurgical limb were significantly different from those of the matched limb of the control group at IE (mean difference, 9.8 seconds; t = 8.6, df = 197.5, P<.001) and at 3 months (mean difference, 2.3 seconds; t = 2.6, df = 146.7, P = .012) but not significantly different at 1 year (mean difference, 1.4 seconds; t = 1.5, df = 182, P = .140).
TABLE 2.
SST Performance Times in Patients Who Underwent Unilateral Total Knee Arthroplasty and Those in the Matching Limbs of Control Subjects
| Test | IE* | 3 mo* | 1 y* | Controls† |
|---|---|---|---|---|
| SST surgical limb | 33.9 ± 11.8 (P<.001); 135 | 23.3 ± 7.6 (P = .007); 145 | 20.9 ± 5.7 (P = .540); 123 | 20.3 ± 6.8; 61 |
| SST nonsurgical limb | 29.5 ± 10.9 (P<.001); 142 | 22.0 ± 7.0 (P = .012); 144 | 21.1 ± 6.3 (P = .120); 123 | 19.7 ± 5.4; 61 |
Abbreviations: IE, initial outpatient physical therapy evaluation; SST, single-step test.
Values are mean ± SD seconds (P); n. P values are reported for equal variances, not assumed, and indicate difference from the respective control group.
Values are mean ± SD seconds; n.
DISCUSSION
The SST allows for assessment of unilateral limb ability without the potential for contralateral knee OA to influence performance. Similar to other validated measures of unilateral lower extremity performance in younger individuals (eg, hop test),28 this test is a reliable and valid measure when compared with standard clinic-based performance measures used to assess patients with unilateral OA, and is responsive to change in patients who receive postoperative outpatient physical therapy after unilateral TKA. Furthermore, it is relatively easy for clinicians to implement. Finally, performance of the SST successfully distinguished the surgical from the nonsurgical limbs of patients at an initial physical therapy evaluation and at 3 months after unilateral TKA. Similarly, performance of the SST distinguished the surgical and nonsurgical limbs of patients from the limbs of healthy controls at the initial physical therapy evaluation. These findings support our hypothesis that the SST can be used to differentiate between the limbs of patients after unilateral TKA, and between the surgical limb of patients after unilateral TKA and the limbs of healthy control subjects without knee pathology.
It is important for clinicians who treat patients after unilateral TKA to be able to examine each limb independently. Findings from previous studies have demonstrated that patients who undergo unilateral TKA for end-stage OA exhibit disease progression in the nonsurgical limb.30 In turn, impairments of the nonsurgical limb can mask improvements in the surgical limb and in overall activity limitations, when assessments that require both limbs to complete are performed.8 Therefore, it is important for clinicians to have a simple, cost-effective test, such as the SST, to evaluate activity limitations in each limb independently. Though a knee immobilizer was used to ensure that the test limb (the limb on the 15-cm block) was responsible for completing the maneuver, a knee immobilizer would not be necessary for the use of the SST as a measure of activity limitations were the tester to instruct the patient to not bend the contralateral limb and to not use it to push off the ground.
The SST as an Impairment-Based Test
Our hypothesis that the SST is a valid impairment-based measure of lower extremity ability was supported, as patient performance of the SST correlated with that of standard clinic-based performance measures (SCT, 6MW test, TUG test) at each time point. Findings from previous work suggest that the SCT,10 TUG test,12,27 and 6MW test12,13,23 may be good measures for evaluating and detecting changes in functional ability over time. Furthermore, the changes in SST performance were similar to the changes in other performance measures over the first year after TKA, which also supports our hypothesis. The SST was responsive to change in patients after TKA who participated in postsurgical, outpatient physical therapy. There was large overlap in the ESI 95% confidence intervals for the SST and both the SCT and TUG test. However, there was small overlap between ESIs for the SST and the 6MW test, suggesting that the 6MW test may be a more responsive measure in our patients. The responsiveness estimates for the SST and the clinic-based performance measures (SCT, TUG test, and 6MW test) were large (greater than 0.8), suggesting that all of these tests provide clinicians with a good metric for quantifying lower extremity activity limitations.
Considering the potential risks associated with negotiating stairs,29 as well as the difficulty of standardizing stair tests (eg, due to the varying number of steps and step heights among stairways), the SST may be an appropriate alternative to the SCT for assessing activity-limited patients. The SST may also be used for testing patients who are not comfortable or capable of ascending and descending stairs at a rapid pace or by clinics that do not have a flight of stairs for testing stair-climbing ability. The utility of stepping tests has been demonstrated when evaluating the quality of movement15,26 and for assessing the influence of pain17,25 in other populations, suggesting that a stepping task could also serve as a good tool to evaluate activity limitations in patients with knee OA and after TKA. More importantly, the SST should be considered as a good complement to the standard clinic-based performance tests, as it provides unique insight into the ability of each limb independently, especially in patients with contralateral, symptomatic knee OA.
Changes in the SST Over Time
The substantial improvements in SST performance from IE to 3 months were not surprising, as this was the period in which the rehabilitation protocol was completed and performance plateaus have previously been observed.7 However, at 3 months and at 1 year, the SST performance times for either limb of the TKA group were not significantly different from those of healthy controls. The finding of similar levels between patients after TKA and controls is surprising, as functional performance (eg, SCT)35 and impairment-based measures, such as quadriceps strength,3,37 in patients after TKA do not typically reach the performance levels of healthy controls within the first postoperative year. Therefore, similar performance between groups in the SST suggests that the patients may be using whole-body strategies to compensate for this quadriceps deficit. These findings further support the use of the SST as a measure of activity limitations for limb comparisons over time to complement other measures, such as quadriceps strength, to provide a more comprehensive picture of overall activity limitations in patients after TKA.
To provide some perspective of the utility of the SST as a measure of activity limitation in patients after TKA, we applied a rule of thumb to estimate the minimal clinically important difference, based on half the standard deviation of the measure at IE (5.7 seconds), which is a distribution-based approach recommended by Norman et al.21 Based on this estimate, 70.7% of our patients would have been deemed as having shown improvement in their performance of the SST using the surgical limb from IE to 1 year. This finding is similar to the 72.7% of patients who reported being moderately or very satisfied after TKA.34 These patients would also have been deemed to show improvements in their performance of the SCT (6.4 seconds, 82.0%), the TUG test (1.84 seconds, 81.0%), and the 6MW test (79.6 m, 82.0%).
Study Limitations
The strength of this study is the introduction of the SST as a reliably acquired and valid test of unilateral lower extremity ability in patients after TKA. However, the SST is not being recommended as a replacement for standard clinic-based performance measures, but as a complementary measure that will provide insight into how each limb may contribute to changes in ability over time.
Additionally, SST performance in the nonsurgical limb was slower than that of the controls, which may be interpreted as a limitation of the value of the measure. However, as with many individuals with knee OA and those who undergo TKA, there is a nonrandom progression of disease in the contralateral leg,30 such that disease may be present and not symptomatic in the contralateral knee and/or hip. Additionally, physical activity levels decline in patients with knee OA in response to a passive coping strategy,32 which, in turn, may lead to functional impairments. Therefore, it should not be surprising that SST performance of the nonsurgical limb in patients with knee OA after TKA is slower than that of the limbs of healthy controls. In fact, the added utility of the SST is that the impact of TKA and rehabilitation on each limb can be assessed independently.
CONCLUSION
TKA procedures are being performed more regularly, and the prevalence of such procedures is expected to increase substantially over the next few decades.14 With an increasing focus on maximizing functional abilities following TKA, clinicians need to have tests that can objectively assess and quantify activity limitations and abilities, and that can track progress through the course of the rehabilitation process. A challenge that clinicians face is to find measures that are adequate for use in the clinic and sensitive enough to detect changes in lower extremity abilities, and can assess each limb independently. The SST is a simple and inexpensive way for clinicians to evaluate activity limitation of each limb independently. The SST should, however, be utilized in combination with other bilateral tests of lower extremity function, clinical tests (eg, strength and range of motion), and instruments of self-perceived functional ability to provide clinicians with a truly comprehensive assessment of change over the course of disease or recovery from surgical interventions.
KEY POINTS.
FINDINGS: This work demonstrated that the SST can be used to assess unilateral activity impairments in patients after TKA.
IMPLICATIONS: The SST is a low-cost, safe test that can be easily implemented in clinical practice to evaluate individuals after TKA.
CAUTION: The SST is not designed to replace, but to complement, the existing battery of clinic-based, lower extremity performance measures.
Acknowledgments
This study was financially supported in part by the following NIH grants: R01-HD041055 and COBREII P20RR016458. The study was approved by the University of Delaware Human Subjects Review Board. The authors certify that they have no affiliations with or financial involvement in any organization or entity with a direct financial interest in the subject matter or materials discussed in the manuscript.
REFERENCES
- 1.Almeida GJ, Schroeder CA, Gil AB, Fitzgerald GK, Piva SR. Interrater reliability and validity of the stair ascend/descend test in subjects with total knee arthroplasty. Arch Phys Med Rehabil. 2010;91:932–938. doi: 10.1016/j.apmr.2010.02.003. http://dx.doi.org/10.1016/j.apmr.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bade MJ, Kohrt WM, Stevens-Lapsley JE. Outcomes before and after total knee arthroplasty compared to healthy adults. J Orthop Sports Phys Ther. 2010;40:559–567. doi: 10.2519/jospt.2010.3317. http://dx.doi.org/10.2519/jospt.2010.3317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berth A, Urbach D, Awiszus F. Improvement of voluntary quadriceps muscle activation after total knee arthroplasty. Arch Phys Med Rehabil. 2002;83:1432–1436. doi: 10.1053/apmr.2002.34829. [DOI] [PubMed] [Google Scholar]
- 4.Cohen JW. Statistical Power Analysis for the Behavioral Sciences. Academic Press; New York, NY: 1971. [Google Scholar]
- 5.Cumming G, Finch S. Inference by eye: confidence intervals and how to read pictures of data. Am Psychol. 2005;60:170–180. doi: 10.1037/0003-066X.60.2.170. http://dx.doi.org/10.1037/0003-066X.60.2.170. [DOI] [PubMed] [Google Scholar]
- 6.de Ruiter CJ, de Korte A, Schreven S, de Haan A. Leg dominancy in relation to fast isometric torque production and squat jump height. Eur J Appl Physiol. 2010;108:247–255. doi: 10.1007/s00421-009-1209-0. http://dx.doi.org/10.1007/s00421-009-1209-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ethgen O, Bruyère O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86-A:963–974. doi: 10.2106/00004623-200405000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Farquhar S, Snyder-Mackler L. The Chitranjan Ranawat Award: the nonoperated knee predicts function 3 years after unilateral total knee arthroplasty. Clin Orthop Relat Res. 2010;468:37–44. doi: 10.1007/s11999-009-0892-9. http://dx.doi.org/10.1007/s11999-009-0892-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guyatt GH, Sullivan MJ, Thompson PJ, et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;132:919–923. [PMC free article] [PubMed] [Google Scholar]
- 10.Kennedy D, Stratford PW, Pagura SM, Walsh M, Woodhouse LJ. Comparison of gender and group differences in self-report and physical performance measures in total hip and knee arthroplasty candidates. J Arthroplasty. 2002;17:70–77. doi: 10.1054/arth.2002.29324. [DOI] [PubMed] [Google Scholar]
- 11.Kennedy DM, Stratford PW, Riddle DL, Hanna SE, Gollish JD. Assessing recovery and establishing prognosis following total knee arthroplasty. Phys Ther. 2008;88:22–32. doi: 10.2522/ptj.20070051. http://dx.doi.org/10.2522/ptj.20070051. [DOI] [PubMed] [Google Scholar]
- 12.Kennedy DM, Stratford PW, Wessel J, Gollish JD, Penney D. Assessing stability and change of four performance measures: a longitudinal study evaluating outcome following total hip and knee arthroplasty. BMC Musculoskelet Disord. 2005;6:3. doi: 10.1186/1471-2474-6-3. http://dx.doi.org/10.1186/1471-2474-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kreibich DN, Vaz M, Bourne RB, et al. What is the best way of assessing outcome after total knee replacement? Clin Orthop Relat Res. 1996:221–225. doi: 10.1097/00003086-199610000-00031. [DOI] [PubMed] [Google Scholar]
- 14.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. http://dx.doi.org/10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 15.Lark SD, Buckley JG, Bennett S, Jones D, Sargeant AJ. Joint torques and dynamic joint stiffness in elderly and young men during stepping down. Clin Biomech (Bristol, Avon) 2003;18:848–855. doi: 10.1016/s0268-0033(03)00150-5. [DOI] [PubMed] [Google Scholar]
- 16.LaStayo PC, Meier W, Marcus RL, Mizner R, Dibble L, Peters C. Reversing muscle and mobility deficits 1 to 4 years after TKA: a pilot study. Clin Orthop Relat Res. 2009;467:1493–1500. doi: 10.1007/s11999-009-0801-2. http://dx.doi.org/10.1007/s11999-009-0801-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Loudon JK, Wiesner D, Goist-Foley HL, Asjes C, Loudon KL. Intrarater reliability of functional performance tests for subjects with patellofemoral pain syndrome. J Athl Train. 2002;37:256–261. [PMC free article] [PubMed] [Google Scholar]
- 18.McMahon M, Block JA. The risk of contralateral total knee arthroplasty after knee replacement for osteoarthritis. J Rheumatol. 2003;30:1822–1824. [PubMed] [Google Scholar]
- 19.Mizner RL, Petterson SC, Clements KE, Zeni JA, Jr., Irrgang JJ, Snyder-Mackler L. Measuring functional improvement after total knee arthroplasty requires both performance-based and patient-report assessments: a longitudinal analysis of outcomes. J Arthroplasty. 2011;26:728–737. doi: 10.1016/j.arth.2010.06.004. http://dx.doi.org/10.1016/j.arth.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mizner RL, Petterson SC, Snyder-Mackler L. Quadriceps strength and the time course of functional recovery after total knee arthroplasty. J Orthop Sports Phys Ther. 2005;35:424–436. doi: 10.2519/jospt.2005.35.7.424. http://dx.doi.org/10.2519/jospt.2005.2036. [DOI] [PubMed] [Google Scholar]
- 21.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41:582–592. doi: 10.1097/01.MLR.0000062554.74615.4C. http://dx.doi.org/10.1097/01.MLR.0000062554.74615.4C. [DOI] [PubMed] [Google Scholar]
- 22.Ouellet D, Moffet H. Locomotor deficits before and two months after knee arthroplasty. Arthritis Rheum. 2002;47:484–493. doi: 10.1002/art.10652. http://dx.doi.org/10.1002/art.10652. [DOI] [PubMed] [Google Scholar]
- 23.Parent E, Moffet H. Comparative responsiveness of locomotor tests and questionnaires used to follow early recovery after total knee arthroplasty. Arch Phys Med Rehabil. 2002;83:70–80. doi: 10.1053/apmr.2002.27337. [DOI] [PubMed] [Google Scholar]
- 24.Petterson SC, Mizner RL, Stevens JE, et al. Improved function from progressive strengthening interventions after total knee arthroplasty: a randomized clinical trial with an imbedded prospective cohort. Arthritis Rheum. 2009;61:174–183. doi: 10.1002/art.24167. http://dx.doi.org/10.1002/art.24167. [DOI] [PubMed] [Google Scholar]
- 25.Piva SR, Fitzgerald GK, Irrgang JJ, et al. Associates of physical function and pain in patients with patellofemoral pain syndrome. Arch Phys Med Rehabil. 2009;90:285–295. doi: 10.1016/j.apmr.2008.08.214. http://dx.doi.org/10.1016/j.apmr.2008.08.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Piva SR, Fitzgerald K, Irrgang JJ, et al. Reliability of measures of impairments associated with patellofemoral pain syndrome. BMC Musculoskelet Disord. 2006;7:33. doi: 10.1186/1471-2474-7-33. http://dx.doi.org/10.1186/1471-2474-7-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 28.Reid A, Birmingham TB, Stratford PW, Alcock GK, Giffin JR. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther. 2007;87:337–349. doi: 10.2522/ptj.20060143. http://dx.doi.org/10.2522/ptj.20060143. [DOI] [PubMed] [Google Scholar]
- 29.Roys MS. Serious stair injuries can be prevented by improved stair design. Appl Ergon. 2001;32:135–139. doi: 10.1016/s0003-6870(00)00049-1. [DOI] [PubMed] [Google Scholar]
- 30.Shakoor N, Block JA, Shott S, Case JP. Nonrandom evolution of end-stage osteoarthritis of the lower limbs. Arthritis Rheum. 2002;46:3185–3189. doi: 10.1002/art.10649. http://dx.doi.org/10.1002/art.10649. [DOI] [PubMed] [Google Scholar]
- 31.Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000;80:896–903. [PubMed] [Google Scholar]
- 32.Steultjens MP, Dekker J, Bijlsma JW. Coping, pain, and disability in osteoarthritis: a longitudinal study. J Rheumatol. 2001;28:1068–1072. [PubMed] [Google Scholar]
- 33.Stevens JE, Mizner RL, Snyder-Mackler L. Neuromuscular electrical stimulation for quadriceps muscle strengthening after bilateral total knee arthroplasty: a case series. J Orthop Sports Phys Ther. 2004;34:21–29. doi: 10.2519/jospt.2004.34.1.21. http://dx.doi.org/10.2519/jospt.2004.0947. [DOI] [PubMed] [Google Scholar]
- 34.Vissers MM, de Groot IB, Reijman M, Bussmann JB, Stam HJ, Verhaar JA. Functional capacity and actual daily activity do not contribute to patient satisfaction after total knee arthroplasty. BMC Musculoskelet Disord. 2010;11:121. doi: 10.1186/1471-2474-11-121. http://dx.doi.org/10.1186/1471-2474-11-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Walsh M, Woodhouse LJ, Thomas SG, Finch E. Physical impairments and functional limitations: a comparison of individuals 1 year after total knee arthroplasty with control subjects. Phys Ther. 1998;78:248–258. doi: 10.1093/ptj/78.3.248. [DOI] [PubMed] [Google Scholar]
- 36.World Health Organization . Obesity: Preventing and Managing the Global Epidemic. World Health Organization; Geneva, Switzerland: 2000. [PubMed] [Google Scholar]
- 37.Yoshida Y, Mizner RL, Ramsey DK, Snyder-Mackler L. Examining outcomes from total knee arthroplasty and the relationship between quadriceps strength and knee function over time. Clin Biomech (Bristol, Avon) 2008;23:320–328. doi: 10.1016/j.clinbiomech.2007.10.008. http://dx.doi.org/10.1016/j.clinbiomech.2007.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zeni JA, Jr., Snyder-Mackler L. Early postoperative measures predict 1- and 2-year outcomes after unilateral total knee arthroplasty: importance of contralateral limb strength. Phys Ther. 2010;90:43–54. doi: 10.2522/ptj.20090089. http://dx.doi.org/10.2522/ptj.20090089. [DOI] [PMC free article] [PubMed] [Google Scholar]