Abstract
In a randomised controlled pragmatic trial we investigated whether local infiltration analgesia would result in earlier readiness for discharge from hospital after total knee replacement (TKR) than patient-controlled epidural analgesia (PCEA) plus femoral nerve block. A total of 45 patients with a mean age of 65 years (49 to 81) received a local infiltration with a peri-articular injection of bupivacaine, morphine, and methylprednisolone, as well as adjuvant analgesics. In 45 PCEA+femoral nerve blockade patients with a mean age of 67 years (50 to 84), analgesia included a bupivacaine nerve block, bupivacaine/hydromorphone PCEA, and adjuvant analgesics. The mean time until ready for discharge was 3.2 days (1 to 14) in the local infiltration group and 3.2 days (1.8 to 7.0) in the PCEA+femoral nerve blockade group. The mean pain scores for patients receiving local infiltration were higher when walking (p = 0.0084), but there were no statistically significant differences at rest. The mean opioid consumption was higher in those receiving local infiltration.
The choice between these two analgesic pathways should not be made on the basis of time to discharge after surgery. Most secondary outcomes were similar, but PCEA+femoral nerve blockade patients had lower pain scores when walking and during continuous passive movement. If PCEA+femoral nerve blockade is not readily available, local infiltration provides similar length of stay and similar pain scores at rest following TKR.
Introduction
Pain management after total knee replacement (TKR) may influence a patient’s participation in physiotherapy, the time to discharge from hospital, and the long-term outcome. Patient-controlled epidural analgesia (PCEA) is widely considered to be better than intravenous opioids for pain relief after major surgery,1 and some consider it to provide the best pain relief after TKR,2 whereas others support continuous femoral nerve blockade.3 The addition of a single-injection femoral nerve block to PCEA reduces pain without slowing the achievement of physiotherapy goals following TKR.4
A local infiltration protocol5 recommends the infiltration of the surgical site with bupivacaine plus additives in order to avoid epidural analgesia, parenteral opioids or nerve blockade. Patients treated by local infiltration may also receive oral opioids, meloxicam and a transdermal clonidine patch. When local infiltration and femoral nerve blockade are compared there is a small but not significant trend towards better pain control on the day after surgery with local infiltration.6 Local analgesia delivered through an intra-articular catheter gives lower pain scores, less opioid use and better mobilisation on the first post-operative day than femoral nerve blockade via a perineural catheter.7
We report a randomised prospective pragmatic trial comparing local infiltration5 versus PCEA and femoral nerve blockade.4 A pragmatic trial design was used because the study was intended to help clinicians choose between two alternative courses of treatment.8 The study was not blinded because the differences between the two protocols were too marked for this to be achievable. Both limbs of the trial included the use of non-steroidal anti-inflammatory drugs (NSAIDs), which improves pain and physiotherapy outcomes after TKR.9 We hypothesised that local infiltration would result in earlier discharge,10 and would also be associated with lower opioid consumption, lower opioid-related symptom distress scores, improved recovery and higher patient satisfaction.
Patients & Methods
The trial had ethical approval and the patients gave written informed consent. They were consecutively randomised to either local infiltration or PCEA combined with femoral nerve blockade (1:1 allocation, parallel trial design). The group to which the patients were assigned was indicated in numbered sealed envelopes, which were prepared by an independent researcher and opened by the anaesthetist assigned to the procedure.
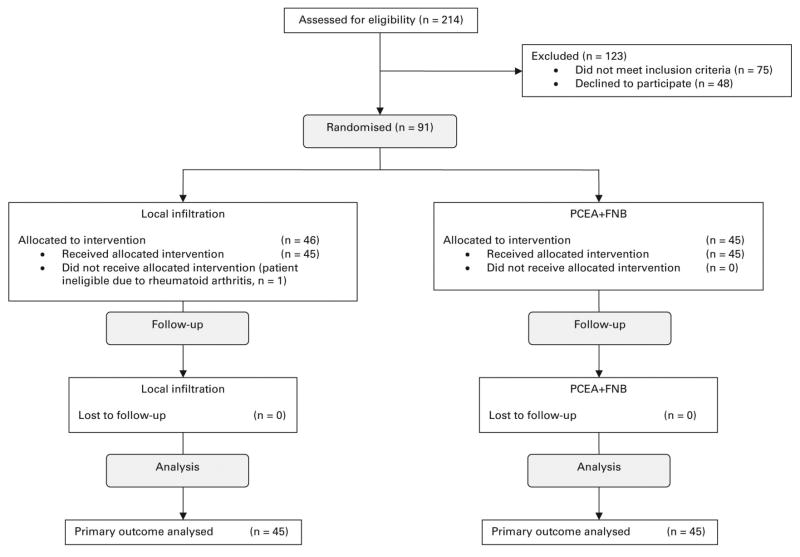
Patients aged between 18 and 85 years were eligible if they had osteoarthritis, were scheduled for primary unilateral TKR, and had < 15° of varus, 15° of valgus or a 15° flexion contracture. Exclusion criteria included relevant drug allergy or intolerance, American Society of Anesthesiologists (ASA)11 grade > III, insulin-dependent diabetes, hepatic or renal failure, chronic opioid use (more than three months) and previous open knee surgery (Fig. 1). The characteristics of the patients in the two groups were similar (Table I).
Figure 1.
CONSORT Diagram. Flow of patients through the protocol (PCEA, patient-controlled epidural analgesia; FNB, femoral nerve blockade).
Table I.
Patient characteristics (PCEA+FNB, patient-controlled epidural analgesia plus femoral nerve block)
| Local infiltration | PCEA+FNB | p-value | |
|---|---|---|---|
| Patients (n) | 45 | 45 | |
| Mean age (yrs) (range) | 65 (49 to 81) | 67 (50 to 84) | 0.239* |
| Male gender (n, %) | 16 (36) | 16 (36) | 1.000† |
| Mean body mass index (kg/m2) (range) | 31 (23 to 47) | 32 (21 to 48) | 0.722* |
| Body mass index group (n, %) | 0.930† | ||
| Normal (<25 kg/m2) | 2 (4) | 3 (7) | |
| Overweight (25 kg/m2 to < 30 kg/m2) | 20 (44) | 19 (42) | |
| Obese (30 kg/m2 to < 40 kg/m2) | 20 (44) | 21 (47) | |
| Morbidly obese (≥ 40 kg/m2) | 3 (7) | 2 (4) | |
| Ethnicity (n, %) | 0.368† | ||
| Caucasian | 37 (82) | 40 (89) | |
| Other | 8 (18) | 5 (11) | |
| American Society of Anesthesiologists grade (n, %) | 0.568† | ||
| 1 | 2 (4) | 2 (4) | |
| 2 | 36 (80) | 32 (71) | |
| 3 | 7 (16) | 11 (24) |
independent samples t-test
chi-squared test
Patients rated their pre-operative pain at rest and with activity on a numerical rating scale12 (NRS; with 0 representing no pain and 10 the worst imaginable pain) and filled out a Short-Form (SF)-8 Health Survey.13
The local infiltration patients received pre-operative meloxicam (7.5 mg orally if aged > 75 years; otherwise 15 mg), controlled-release oxycodone (10mg orally if aged > 80 years; 20 mg otherwise) and a clonidine patch (100 μg/24 h) 30 to 60 minutes prior to transfer to the operating theatre. A spinal anaesthetic with 0.5% bupivacaine (10, 12.5 or 15 mg) was administered. A surgeon, who had received video training, performed the local infiltration, consisting of one deep injection prior to cementation and a more superficial injection prior to closure of the wound. The deep injection consisted of bupivacaine 0.5% with adrenaline, 30 ml; morphine, 8 mg/ml, 1 ml; methylprednisolone, 40 mg/ml, 1 ml; cefazolin, 500 mg in 10 ml in normal saline, 22 ml. The superficial injection consisted of 40 ml 0.25% bupivacaine.
Post-operative analgesia continued with oxycodone every 12 h x 48 hours (10 mg orally if aged > 80 years; 20 mg otherwise), meloxicam daily (7.5 mg orally if aged > 75 years; 15 mg otherwise), oxycodone (5 mg every 6 h as needed), paracetamol (1 g orally every 6 h) and ketorolac (15 mg intramuscularly every 6 h as needed). In cases of severe pain (NRS scores > 6 for > 2 hours), salvage therapy was available using intravenous hydromorphone PCEA. Controlled-release oxycodone is not approved in the US for the treatment of post-operative pain in patients not previously exposed to opioids, but this practice has been extensively described.5–7,10
The PCEA and femoral nerve blockade patients received the same pre-operative dose of meloxicam + dexamethasone (6 mg orally) 30 to 60 minutes before transfer to the operating theatre. An ultrasound-guided femoral nerve blockade (30 ml bupivacaine 0.25%, with adrenaline 1:200 000) was administered, followed by a combined spinal epidural with 0.5% bupivacaine (10 mg, 12.5 mg or 15 mg). Post-operative PCEA (bupivacaine 0.06% /hydromorphone 10 μg/ml) was started at 4 ml/h/ 4 ml bolus/10 min lockout/20 ml hourly maximum. The basal rate on the PCEA was reduced to 2 ml/h at 6:59 on the first post-operative day, further reduced to 0 ml/h at 16:59 on the first post-operative day, and the epidural was removed at noon on the second post-operative day. Patients received oral meloxicam (7.5 to 15 mg daily) and oxycodone/paracetamol (5/325 every 3 hr as needed).
Both groups received intra-operative intravenous sedation with midazolam and propofol. On arrival in the recovery room, the PCEA and femoral nerve blockade patients received urinary catheters. The urinary catheters were subsequently removed at the same time as the epidural catheters. Continuous passive movement was initiated on the first post-operative day as was physiotherapy. Patients were interviewed twice daily by a research assistant during the first three post-operative days, and seven days later by telephone, in order to gather information about readiness for discharge, pain, activity and analgesic use. They were contacted by telephone at six months to assess recovery (SF-8) and identify neuropathic pain (Leeds Assessment of Neuropathic Symptoms and Signs, LANSS).9
Discharge and discharge readiness were calculated from the time of leaving the operating theatre to the time when the discharge criteria were met.
Patients were judged ready to be discharged when the PCEA (if present) was discontinued, when they were experiencing only mild pain (NRS < 4), had required no parenteral narcotics within the last four hours, had no moderate or severe nausea within the last four hours and were eating normally. They were also required to have no urinary catheter, a dry surgical wound, no acute medical problems, stable vital signs during physiotherapy, and to be able to transfer independently to and from a chair and from bed to a standing position. Additional criteria for readiness for discharge included ability to walk 40 feet with only a walker or crutch if needed, and full extension of the knee.
Secondary hypotheses related to pain and possible reduction in opioid use. The QoR-40 is a validated measure that assesses the effect of operative techniques on post-operative recovery.14,15 High scores indicate better recovery. The pain dimension involves seven items on a scale of 1 to 5 (1, constant; 5, never). The opioid-related symptom distress scale (ORSDS) evaluates post-operative opioid-related symptoms16 and has been validated for orthopaedic patients, including after TKR.17 Higher scores indicate more severe symptoms. Patients were asked to indicate, on a scale of 1 to 10, with 1 being ‘very dissatisfied’ and 10 being ‘very satisfied’, how effective their pain medication had been. Their opioid usage was also recorded.
Before surgery and at six months an SF-8 and the LANSS pain scale9,18 were administered. The SF-8 is a widely accepted questionnaire,13 with high scores indicative of high levels of health. The LANSS test is a validated instrument for the identification of neuropathic pain18. High scores indicate the presence of neuropathic pain. Additional tracked events included unplanned conversion to PCEA.
Assessments were made using the various instruments on the first, second, third and seventh post-operative days and at six months.
Statistical Analysis
Preliminary unpublished data indicated that PCEA and femoral nerve blockade patients were ready for discharge at a mean of 3.2 days post-operatively. We hypothesised that local infiltration would reduce the time until the patients were ready for discharge by 0.5 days. We considered a reduction of 0.5 days to be the minimal clinically important difference. A power analysis with α = 0.05, β=0.8, and two-sided hypothesis testing indicated that 45 patients in each group were needed. Analysis was by original assigned groups and was performed using either Microsoft Excel or SPSS 13.0 for Windows (SPSS Inc., Chicago, Illinois). Significance was set at a p-value of < 0.05. Readiness for discharge was compared using Student’s t-test. Continuous variables are presented as mean (range) and compared using two-sample t-tests. NRS pain scores were analysed using generalised estimated equations (GEE), a technique that is better suited for repeated measurements of pain scores from a group of individuals.19 Discrete variables are presented using proportions and analysed with a chi-squared test.
Results
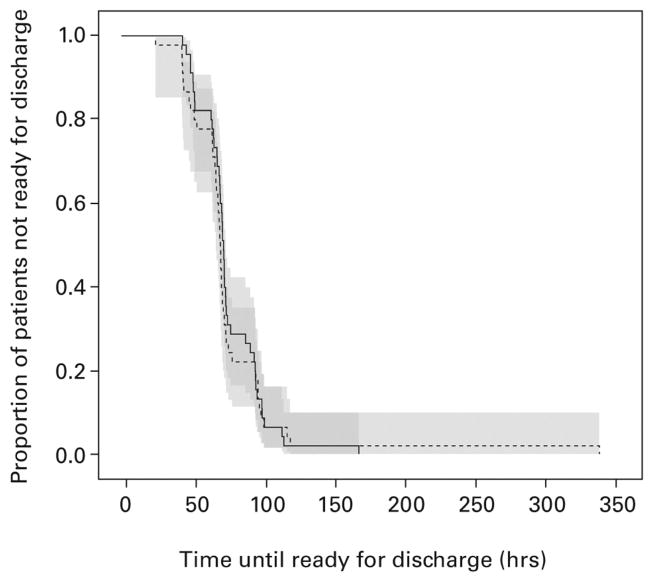
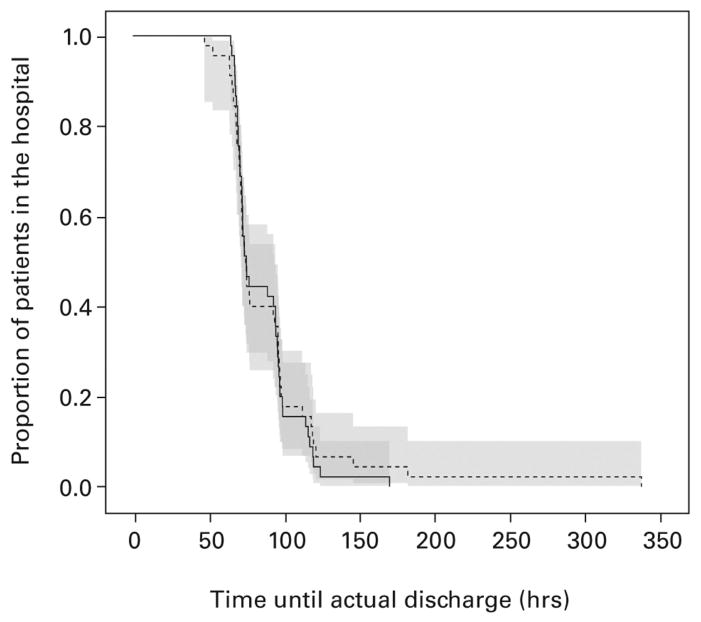
There was no difference between groups in terms of time to being ready for discharge or actual length of stay (Figs 2 and 3). Patients were ready for discharge at a mean of 3.2 days (1 to 14) (local infiltration) vs. 3.2 days (1.8 to 7.0) (PCEA+femoral nerve blockade) (p = 0.98). The mean length of stay was 3.8 days (2 to 14) (local infiltration) and 3.6 days (2.7 to 7.1) (PCEA+femoral nerve blockade) (p = 0.55). Among 45 patients receiving local infiltration, three also received intravenous (IV) PCEA and one received PCEA because of high pain scores. Among 45 PCEA+femoral nerve blockade patients, one also received IV PCEA because of a failed epidural.
Figure 2.
Kaplan-Meier survival curves of time (hours) to readiness for discharge. Time 0 = time out of the operating theatre. The dotted line represents the local infiltration group and the solid line represents the patient-controlled epidural analgesia + femoral nerve blockade group.
Figure 3.
Kaplan-Meier survival curves of time (hours) to actual discharge. Time 0 = time out of the operating theatre. The dotted line represents the local infiltration group and the solid line represents the patient-controlled epidural analgesia + femoral nerve blockade group.
No difference was detected in pain at rest between the groups (p=0.4068). Age, BMI, race and ASA status were not significant and were therefore removed from the final model; the estimate was adjusted for time and gender.
A difference in pain during walking between the groups was detected in the model. The β estimate for the treatment effect implies that the local infiltration group had a mean pain during walking of 0.81 points higher than did the PCEA+femoral nerve blockade group (p=0.0084). Age, BMI and race were not significant and were removed from the final model; the estimate was adjusted for time, gender and ASA status.
A borderline difference between the groups in pain during physiotherapy was detected. The β estimate for the treatment effect implies that the local infiltration group had a mean pain score during physiotherapy of 0.55 points higher than did the PCEA+femoral nerve blockade group (p=0.0951). Age and race were not significant and were removed from the final model; the estimate was adjusted for time, gender, BMI and ASA status.
A difference in pain while using CPM between the treatment groups was detected. The β estimate for the treatment effect implies that the local infiltration group had a mean pain score while using CPM of 0.88 points higher than did the PCEA+femoral nerve blockade group (p = 0.0132). Age, BMI and race were not significant and were removed from the final model; the estimate was adjusted for time, gender and ASA status.
The mean total opioid usage (converted to equivalents of oral morphine) was greater among patients receiving local infiltration (Table II): 228 mg (30 to 608) (LIA) vs. 142 mg (34 to 477) (PCEA+femoral nerve blockade, cumulative post-operative days 0 to 2, p = 0.0001). Other measures of pain and recovery, including ORSDS, QOR-40, SF-8 and LANSS, were not different between groups (Tables II and III). The pain portion of the QoR-40 was statistically different between the groups (p = 0.03) despite similar mean values of 32 (local infiltration) vs. 33 (PCEA+femoral nerve blockade). This reflects median values of 32 for local infiltration and 34 for PCEA + femoral nerve blockade.
Table II.
Opioid intake, opioid side effects, and patient health (PCEA+FNB, patient-controlled epidural analgesia plus femoral nerve block)
| Local infiltration | PCEA+FNB | ||||
|---|---|---|---|---|---|
| Outcome* | n | Mean (range) | n | Mean (range) | p-value† |
| Opioid intake POD0 (equivalents mg morphine orally) | 45 | 67 (15 to 105) | 45 | 26 (6 to 165) | 0.0001 |
| Opioid intake total in hospital (POD0 to 2) (equivalents mg morphine orally) | 45 | 228 (30 to 608) | 45 | 142 (34 to 477) | 0.0001 |
| ORSDS (median, interquartile range) | |||||
| Overall Composite | 44 | 0.39 (0.18 to 0.68) | 45 | 0.41 (0.27 to 0.86) | 0.527 |
| Frequency | 44 | 0.50 (0.25 to 0.81) | 45 | 0.50 (0.33 to 0.92) | 0.604 |
| Severity | 44 | 0.33 (0.17 to 0.67) | 45 | 0.33 (0.25 to 0.88) | 0.454 |
| Bothersomeness | 44 | 0.33 (0.13 to 0.65) | 45 | 0.33 (0.20 to 0.80) | 0.552 |
| Short-Form 8 | |||||
| Pre-operative | |||||
| Physical component summary | 42 | 35 (16 to 48) | 43 | 36 (19 to 52) | 0.659 |
| Mental component summary | 42 | 51 (18 to 67) | 43 | 53 (30 to 67) | 0.438 |
| Six months | |||||
| Physical component summary | 33 | 51 (26 to 61) | 39 | 51 (30 to 59) | 0.971 |
| Mental component summary | 33 | 54 (20 to 63) | 39 | 55 (35 to 66) | 0.514 |
| Leeds Assessment of Neuropathic Symptoms and Signs at 6 months, n (%) | 33 | 1 (3) | 39 | 3 (8) | 0.620‡ |
POD, post-operative day; ORSDS, opioid-related symptom distress scale
independent samples t-test, unless otherwise stated
chi-squared test
Table III.
Satisfaction and quality of recovery (PCEA+FNB, patient-controlled epidural analgesia plus femoral nerve block)
| Local infiltration | PCEA+FNB | |||||
|---|---|---|---|---|---|---|
| Outcome* | Maximum Possible Score | n | Mean (range) | n | Mean (range) | p-value* |
| POST-OPERATIVE DAY 1 | ||||||
| Patient Satisfaction | 10 | 42 | 8.2 (1 to 10) | 44 | 9.0 (2 to 10) | 0.10 |
| Quality of Recovery (QoR)-40 | ||||||
| Global | 200 | 44 | 182 (144 to 197) | 45 | 181 (137 to 195) | 0.77 |
| Emotional state | 45 | 44 | 42 (31 to 45) | 45 | 41 (20 to 45) | 0.75 |
| Physical comfort | 60 | 44 | 54 (34 to 60) | 45 | 54 (42 to 60) | 0.83 |
| Psychological support | 35 | 44 | 34 (20 to 35) | 45 | 34 (27 to 35) | 0.25 |
| Physical independence | 25 | 44 | 20 (7 to 25) | 45 | 19 (9 to 25) | 0.13 |
| Pain | 35 | 44 | 32 (25 to 35) | 45 | 33 (22 to 35) | 0.03 |
| POST-OPERATIVE DAY 3 | ||||||
| Patient Satisfaction | 10 | 27 | 8.8 (3 to 10) | 30 | 8.7 (5 to 10) | 0.83 |
| Quality of recovery (QoR)-40 | ||||||
| Global | 200 | 20 | 178 (21 to 200) | 23 | 186 (100 to 200) | 0.57 |
| Emotional state | 45 | 20 | 41 (10 to 45) | 23 | 42 (25 to 45) | 0.58 |
| Physical comfort | 60 | 20 | 53 (6 to 60) | 23 | 57 (39 to 60) | 0.15 |
| Psychological support | 35 | 20 | 33 (0 to 35) | 23 | 33 (5 to 35) | 0.56 |
| Physical independence | 25 | 20 | 20 (1 to 25) | 23 | 20 (0 to 25) | 0.69 |
| Pain | 35 | 20 | 31 (4 to 35) | 23 | 34 (30 to 35) | 0.07 |
independent samples t-test
Two adverse events were reported to our Institutional Review Board. One patient who received local infiltration fell and dislocated her knee, requiring closed reduction. This was judged not to be related to participation in the study because it occurred on the third postoperative day. Another patient who received local infiltration developed delirium on the first post-operative day and this lasted for several days. She was removed from the study at the family’s request. This was judged as possibly related to study participation.
Discussion
Patients in both treatment groups were ready for discharge and were actually discharged at the same time post-operatively. The mean length of stay (3.8 vs. 3.6 days) was similar to that found in many studies reporting the outcome of local infiltration after TKR,20 which mostly vary between three and five days, except for one study that reported a median length of stay of one day.21
Although the primary outcome was similar in both groups, some secondary outcomes marginally favoured PCEA+femoral nerve blockade, in that five patients had excessive pain requiring a change in analgesic modality, including four patients receiving local infiltration who required PCEA and one PCEA+femoral nerve blockade patient who required IV PCEA following a failed epidural. PCEA+femoral nerve blockade patients had statistically significantly better pain control while walking and during CPM, although the difference was < 1 on a scale of 0 to 10. Additionally, the opioid consumption of the PCEA+femoral nerve blockade group was only 38.8% of that of the local infiltration group on first post-operative day and 62.2% on the second post-operative day. These results should only be considered for patients undergoing uncomplicated primary TKR. Further research is required in the use of these techniques among more medically and surgically challenging patients.
A recent study reported similar pain scores with local infiltration compared with continuous femoral nerve blockade22 and recommended the former as a cheaper and easier alternative. Dalury et al10 reported that local infiltration following TKR provided better analgesia than conventional pain management. Busch et al23 found that local infiltration reduced PCEA use and improved patient satisfaction. Kehlet and Andersen20 reviewed 14 studies and found support for local infiltration with a single-injection, but not via a wound catheter. Limitations noted for many of the studies included the inadequate assessment of pain, and unsatisfactory quality comparators such as inadequate analgesic regimens for the controls or the use of NSAIDs in patients receiving local infiltration but not among controls. The effect of local infiltration on length of stay was unclear in these studies. McCartney and McLeod3 emphasised that only four of 21 studies of local infiltration after TKR compared it with other regional analgesic techniques, either PCEA or continuous femoral nerve blockade. Local infiltration provided better analgesia than either femoral nerve blockade or PCEA, but criticisms included the administration of NSAIDs to the local infiltration groups, and complications associated with local infiltration. Raeder2 commented on a study that found local infiltration provided better analgesia than intrathecal morphine + IV PCEA,21 but this comparator was considered suboptimal. Local infiltration was deemed promising, but research was advocated both to identify the roles of each individual component of local infiltration and to compare it to the best potential alternatives. Our study addresses many of these criticisms by comparing local infiltration to an excellent alternative (PCEA+femoral nerve blockade), using NSAIDs in both groups, and using many detailed and validated outcome measures, analysed at many time points.
However, the choice of local infiltration of PCEA+femoral nerve blockade for postoperative analgesia should not be based on the idea that either regimen leads to earlier readiness for discharge. Some secondary outcomes favoured PCEA+femoral nerve blockade, but the pain differences were small. Local infiltration has the advantage of not requiring anaesthetists with training in femoral nerve blockade. Similarly, PCEA+femoral nerve blockade do not require surgeons with training in local infiltration.
This study compared two distinct analgesic regimens, including controlled-release oxycodone and a clonidine patch in the local infiltration group. Further research is necessary to determine the effects of either adding these adjuncts to the PCEA+femoral nerve blockade regimen or removing them from the local infiltration regimen. Local infiltration might be better suited for patients for whom epidural analgesia is contraindicated. Further research is also needed to determine whether the addition of a nerve block to local infiltration would improve post-operative analgesia. For institutions in which PCEA+femoral nerve blockade is not readily available, local infiltration provides similar length of stay and similar pain scores at rest following TKR.
Supplementary Material
Numerical Rating Scale (NRS) pain scores (PCEA+FNB, patient-controlled epidural analgesia plus femoral nerve block; POD, post-operative day)
Acknowledgments
The additional members of HAARC (HSS (Hospital for Special Surgery) Anaesthesia ARJR (Adult Reconstruction and Joint Replacement) Research Collaboration) are as follows: D. D. Bhagat, R. L. Kahn, M. M. Alexiades, K. M. Jules-Elysee, C. S. Ranawat, E. P. Su, Y. Lin, J. Liu, and A. K. Goon.
The authors would like to thank Dr H. Bang, Department of Public Health, Weill Medical College of Cornell University, performed a power analysis. Dr. Bang and P. J. Christos, DrPH, MS, performed statistical analysis and advised on data preparation. They were partially supported by the following grants: Clinical Translational Science Center (CTSC) (UL1-RR024996) and Center for Education and Research in Therapeutics (CERTs) (AHRQ RFA-HS-05-14). The authors would also like to thank J. Liu, MD, PhD for his help with patient enrollment and data analysis, and A. Goon for assistance with manuscript preparation and data analysis.
Footnotes
Portions of this work have been presented at the American Academy of Orthopaedic Surgeons Annual Meeting, February 2012, in San Francisco, California.
Conflict of Interest – No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Contributor Information
Jacques T. YaDeau, Email: yadeauj@hss.edu, Department of Anaesthesiology, Hospital for Special Surgery, Hospital for Special Surgery 535 East 70th Street, New York, NY 10021, (212) 606-1036, (212) 517-4481
Enrique A. Goytizolo, Email: goytizoloe@hss.edu, Department of Anaesthesiology, Hospital for Special Surgery, Hospital for Special Surgery, 535 East 70th Street, New York, NY 10021
Douglas E. Padgett, Email: padgettd@hss.edu, Department of Orthopaedic Surgery, Hospital for Special Surgery, Hospital for Special Surgery, 535 East 70th Street, New York, NY 10021
Spencer S. Liu, Email: liuss@u.washington.edu, Department of Anaesthesiology, Hospital for Special Surgery (current affiliation: Department of Anaesthesiology & Pain Medicine, University of Washington), University of Washington, Box 356540, Seattle, WA 98195
David J. Mayman, Email: maymand@hss.edu, Department of Orthopaedic Surgery, Hospital for Special Surgery, Hospital for Special Surgery, 535 East 70th Street, New York, NY 10021
Amar S. Ranawat, Email: ranawatamar@hss.edu, Department of Orthopaedic Surgery, Hospital for Special Surgery, Hospital for Special Surgery, 535 East 70th Street, New York, NY 10021
Matthew C. Rade, Email: mrade@buffalo.edu, Department of Anaesthesiology, Hospital for Special Surgery (current affiliation: University at Buffalo School of Medicine and Biomedical Sciences), Office of Medical Education Biomedical Education Building, Rm. 40, 3435 Main St. Bldg. 22 Buffalo, New York 14214
Geoffrey H. Westrich, Email: westrichg@hss.edu, Department of Orthopaedic Surgery, Hospital for Special Surgery, Hospital for Special Surgery, 535 East 70th Street, New York, NY 10021
References
- 1.Block BM, Liu SS, Rowlingson AJ, et al. Efficacy of postoperative epidural analgesia: a meta-analysis. JAMA. 2003;290:2455–2463. doi: 10.1001/jama.290.18.2455. [DOI] [PubMed] [Google Scholar]
- 2.Raeder JC. Local infiltration analgesia for pain after total knee replacement surgery: a winner or just a strong runner-up? Anesth Analg. 2011;113:684–686. doi: 10.1213/ANE.0b013e3182288e14. [DOI] [PubMed] [Google Scholar]
- 3.McCartney CJ, McLeod GA. Local infiltration analgesia for total knee arthroplasty. Br J Anaesth. 2011;107:487–489. doi: 10.1093/bja/aer255. [DOI] [PubMed] [Google Scholar]
- 4.YaDeau JT, Cahill JB, Zawadsky MW, et al. The effects of femoral nerve blockade in conjunction with epidural analgesia after total knee arthroplasty. Anesth Analg. 2005;101:891–895. doi: 10.1213/01.ANE.0000159150.79908.21. [DOI] [PubMed] [Google Scholar]
- 5.Ranawat AS, Ranawat CS. Pain management and accelerated rehabilitation for total hip and total knee arthroplasty. J Arthroplasty. 2007;22:12–15. doi: 10.1016/j.arth.2007.05.040. [DOI] [PubMed] [Google Scholar]
- 6.Parvataneni HK, Shah VP, Howard H, et al. Controlling pain after total hip and knee arthroplasty using a multimodal protocol with local periarticular injections: a prospective randomized study. J Arthroplasty. 2007;22:33–38. doi: 10.1016/j.arth.2007.03.034. [DOI] [PubMed] [Google Scholar]
- 7.Toftdahl K, Nikolajsen L, Haraldsted V, et al. Comparison of peri- and intraarticular analgesia with femoral nerve block after total knee arthroplasty: a randomized clinical trial. Acta Orthop. 2007;78:172–179. doi: 10.1080/17453670710013645. [DOI] [PubMed] [Google Scholar]
- 8.Zwarenstein M, Treweek S, Gagnier JJ, et al. Improving the reporting of pragmatic trials: an extension of the CONSORT statement. BMJ. 2008;337:2390. doi: 10.1136/bmj.a2390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buvanendran A, Kroin JS, Della Valle CJ, et al. Perioperative oral pregabalin reduces chronic pain after total knee arthroplasty: a prospective, randomized, controlled trial. Anesth Analg. 2010;110:199–207. doi: 10.1213/ANE.0b013e3181c4273a. [DOI] [PubMed] [Google Scholar]
- 10.Dalury DF, Lieberman JR, MacDonald SJ. Current and innovative pain management techniques in total knee arthroplasty. J Bone Joint Surg Am. 2011;(93-A):1938–1943. doi: 10.2106/JBJS.9320icl. [DOI] [PubMed] [Google Scholar]
- 11.Cullen DJ, Apolone G, Greenfield S, Guadagnoli E, Cleary P. ASA physical status and age predict morbidity after three surgical procedures. Ann Surg. 1994;220:3–9. doi: 10.1097/00000658-199407000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gilron I, Jensen MP. Clinical trial methodology of pain treatment studies: selection and measurement of self-report primary outcomes for efficacy. Reg Anes Pain Med. 2011;36:374–381. doi: 10.1097/AAP.0b013e318217a635. [DOI] [PubMed] [Google Scholar]
- 13.Bost JE, Williams BA, Bottegal MT, Dang Q, Rubio DM. The 8-item Short-Form Health Survey and the physical comfort composite score of the quality of recovery 40-item scale provide the most responsive assessments of pain, physical function, and mental function during the first 4 days after ambulatory knee surgery with regional anesthesia. Anesth Analg. 2007;105:1693–1700. doi: 10.1213/01.ane.0000287659.14893.65. [DOI] [PubMed] [Google Scholar]
- 14.Bennett MI, Smith BH, Torrance N, Potter J. The S-LANSS score for identifying pain of predominantly neuropathic origin: validation for use in clinical and postal research. J Pain. 2005;6:149–158. doi: 10.1016/j.jpain.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 15.Kluivers KB, Riphagen I, Vierhout ME, Brolmann HA, de Vet HC. Systematic review on recovery specific quality-of-life instruments. Surgery. 2008;143:206–215. doi: 10.1016/j.surg.2007.08.017. [DOI] [PubMed] [Google Scholar]
- 16.Herrera FJ, Wong J, Chung F. A systematic review of postoperative recovery outcomes measurements after ambulatory surgery. Anesth Analg. 2007;105:63–69. doi: 10.1213/01.ane.0000265534.73169.95. [DOI] [PubMed] [Google Scholar]
- 17.Apfelbaum JL, Gan TJ, Zhao S, Hanna DB, Chen C. Reliability and validity of the perioperative opioid-related symptom distress scale. Anesth Analg. 2004;99:699–709. doi: 10.1213/01.ANE.0000133143.60584.38. [DOI] [PubMed] [Google Scholar]
- 18.YaDeau JT, Liu SS, Rade MC, Marcello D, Liguori GA. Performance characteristics and validation of the opioid-related symptom distress scale for evaluation of analgesic side effects after orthopedic surgery. Anesth Analg. 2011;113:369–377. doi: 10.1213/ANE.0b013e31821ae3f7. [DOI] [PubMed] [Google Scholar]
- 19.Ma Y, Mazumdar M, Memtsoudis SG. Beyond repeated-measures analysis of variance: advanced statistical methods for the analysis of longitudinal data in anesthesia research. Reg Anesth Pain Med. 2012;37:99–105. doi: 10.1097/AAP.0b013e31823ebc74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kehlet H, Andersen LO. Local infiltration analgesia in joint replacement: the evidence and recommendations for clinical practice. Acta Anaesthesiol Scand. 2011;55:778–784. doi: 10.1111/j.1399-6576.2011.02429.x. [DOI] [PubMed] [Google Scholar]
- 21.Essving P, Axelsson K, Aberg E, et al. Local infiltration analgesia versus intrathecal morphine for postoperative pain management after total knee arthroplasty: a randomized controlled trial. Anesth Analg. 2011;113:926–933. doi: 10.1213/ANE.0b013e3182288deb. [DOI] [PubMed] [Google Scholar]
- 22.Affas F, Nygards EB, Stiller CO, Wretenberg P, Olofsson C. Pain control after total knee arthroplasty: a randomized trial comparing local infiltration anesthesia and continuous femoral block. Acta Orthop. 2011;82:441–447. doi: 10.3109/17453674.2011.581264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Busch CA, Shore BJ, Bhandari R, et al. Efficacy of periarticular multimodal drug injection in total knee arthroplasty: a randomized trial. J Bone Joint Surg Am. 2006;88-A:959–963. doi: 10.2106/JBJS.E.00344. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Numerical Rating Scale (NRS) pain scores (PCEA+FNB, patient-controlled epidural analgesia plus femoral nerve block; POD, post-operative day)