Abstract
Prevalence of posttraumatic stress disorder (PTSD) defined according to the American Psychiatric Association’s Diagnostic and Statistical Manual fifth edition (DSM-5; 2013) and fourth edition (DSM-IV; 1994) was compared in a national sample of U.S. adults (N = 2,953) recruited from an online panel. Exposure to traumatic events, PTSD symptoms, and functional impairment were assessed online using a highly structured, self-administered survey. Traumatic event exposure using DSM-5 criteria was high (89.7%), and exposure to multiple traumatic event types was the norm. PTSD caseness was determined using Same Event (i.e., all symptom criteria met to the same event type) and Composite Event (i.e., symptom criteria met to a combination of event types) definitions. Lifetime, past-12-month, and past 6-month PTSD prevalence using the Same Event definition for DSM-5 was 8.3%, 4.7%, and 3.8% respectively. All 6 DSM-5 prevalence estimates were slightly lower than their DSM-IV counterparts, although only 2 of these differences were statistically significant. DSM-5 PTSD prevalence was higher among women than among men, and prevalence increased with greater traumatic event exposure. Major reasons individuals met DSM-IV criteria, but not DSM-5 criteria were the exclusion of nonaccidental, nonviolent deaths from Criterion A, and the new requirement of at least 1 active avoidance symptom.
The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association [APA], 2013) includes several changes to the criteria for a post-traumatic stress disorder (PTSD) diagnosis including (a) modification of the A1 stressor criterion; (b) elimination of Criterion A2, which required that the A1 stressor event produce fear, helplessness, or horror; (c) four symptom clusters (e.g., Criteria B–E) as opposed to the three symptom clusters (B–D) as required in DSM-IV (APA, 1994) and DSM-IV-TR (APA, 2000); (d) minor changes in Criterion B, the reexperiencing criterion; and (e) expanding the scope of B–E symptoms (Friedman, Resick, Bryan, & Brewin, 2011). Another change acknowledges that more than one traumatic event can be involved (APA, 2013). Kilpatrick, Resnick, and Acierno (2009) described composite PTSD, referring to PTSD symptoms arising from multiple types of traumatic events or multiple incidents within a given type (e.g., combat exposure), so with the explicit acknowledgment in the DSM-5 that more than one traumatic event can contribute to the development of PTSD, understanding how this impacts PTSD prevalence becomes an important question.
Modifications to Criterion A include exclusion of some stressor events defined as Criterion A1 events in the DSM-IV (e.g., unexpected deaths from natural causes). Specific changes to symptom clusters include (a) a new Criterion C composed of active avoidance symptoms that were previously part of a broader Criterion C in the DSM-IV; (b) a new Criterion D (negative alterations in cognition and mood associated with the traumatic event/s) that contains some symptoms from the DSM-IV Criterion C, as well as some substantially modified and new symptoms; and (c) a new Criterion E (marked alterations in arousal and reactivity associated with the traumatic event/s) that includes one new symptom (reckless or self-destructive behavior) and subtle modifications to other symptoms.
How these changes will affect PTSD prevalence is unclear. Some argue that there will be little or no impact (e.g., Frueh, Elhai, & Acierno, 2010). Conversely, McFarlane (2011) suggested that DSM-5 PTSD prevalence may be reduced by the new requirement for at least one active avoidance symptom. To our knowledge, only two published studies have examined these issues. Elhai and colleagues (2012) used a convenience sample of college students who completed a web survey of exposure to the DSM-IV Criterion A1 and DSM-5 Criterion A traumatic events and ratings of PTSD symptom intensity during the past month to their only event, or most distressing event, using a modified form of the PTSD Symptom Scale (PSS-SR; Foa, Riggs, Dancu, & Rothbaum, 1993). Past-month PTSD prevalence was higher, although not significantly so, using the DSM-5 versus the DSM-IV criteria. Limitations of this study included use of a convenience sample of college students and a self-report checklist measuring PTSD.
A second study compared past-month PTSD prevalence based on DSM-IV and DSM-5 criteria using a nonprobability sample of 185 volunteers for studies on trauma and health recruited from an academic medical center and Veterans Affairs (VA) medical center (Calhoun et al., 2012). The Clinician-Administered PTSD Scale (CAPS) was used to assess PTSD using DSM-IV criteria, and four new items were constructed to measure new or substantially modified DSM-5 PTSD symptoms (i.e., D2, D3, D4, and E2). Using DSM-IV criteria, 98% had a Criterion A1 event, 95% met the criteria for A1 and A2, and 89% met DSM-5 Criterion A. Using DSM-IV criteria, 50% met criteria for PTSD. The estimated prevalence of PTSD using DSM-5 criteria was 52%. The authors provided a series of estimates for the projected DSM-5 prevalence across a range of base-rate estimates for the DSM-IV and predicted that DSM-5 prevalence would be substantially higher than DSM-IV prevalence if true DSM-IV prevalence was at lower levels of between 5% and 11%. As noted by the authors, limitations in the sample (e.g., overrepresentation of racial minorities, a nonprobability method of sample selection, high PTSD prevalence) limit the ability to generalize findings to adults in the general population, but strengths included using the CAPS to measure PTSD. In summary, although there are different predictions about the impact of changes in the DSM-5 on PTSD prevalence, research has produced conflicting results and has not addressed the issue within samples that would permit generalization to adults in the general population.
Therefore, the major objectives of this study were to determine: (a) national estimates of exposure to DSM-IV and DSM-5 Criterion A events; (b) national estimates of DSM-IV and DSM-5 PTSD prevalence based on meeting symptom criteria included in the DSM-5 to a single Criterion A event type (Same Event) or to multiple Criterion A event types (Composite Event); (c) reasons for differences in meeting criteria as defined in the DSM-IV and the DSM-5; (d) sex differences in PTSD prevalence; and (e) the conditional probability of PTSD as a function of specific Criterion A event types and numbers of types of event exposure.
Method
Study Overview
The National Stressful Events Survey (Kilpatrick, Resnick, Baber, Guille, & Gros, 2011) was conducted with a large sample recruited from an online panel of U.S. adults, and participants were assessed for exposure to DSM-IV and DSM-5 Criterion A events, as well as for PTSD symptoms and distress or functional impairment associated with PTSD symptoms. The National Stressful Events Survey assessment measure was a self-administered, highly structured survey completed online that mirrored the format of an interactive structured clinical interview by using a conditional branching format that included follow-up questions contingent on prior responses. Also, questions measuring exposure to Criterion A events and PTSD symptoms were developed with input from and review by the DSM-5 Sub-work Group to ensure that the wording captured the content of events and symptoms as intended.
Participants
The sample was recruited from an active panel of adults who were participating in Survey Sampling International (Shelton, CT), a research sampling company that provides potential survey sample participants for university-based and other types of survey research. Survey Sampling International maintains web panels of potential research participants matched to U.S. Census demographics from all geographic regions of the United States who are invited to participate in web surveys. Eligible panel participants for this study were stratified based on sex and age categories within the U.S. Census breakdown of the population. Potential participants received a general invitation from Survey Sampling International stating that they were eligible to participate in a survey. Those interested clicked on a link that took them to a website at the Medical University of South Carolina that contained the National Stressful Events Survey. This web survey, which was programmed using the Research Electronic Data Capture system (Harris, Thielke, Taylor, Gonzalez, & Conde, 2009), contained an introduction and checkbox for the participant to indicate that he or she was 18 years old or older and that they agreed to participate in the survey. The introduction stated that the survey concerned the extent to which people had experienced stressful life events and how being exposed to those events affected them. They were told that it was important for people to participate whether or not they had experienced stressful events and whether or not the events had affected them. The survey was anonymous, and study procedures were approved by the Medical University of South Carolina Institutional Review Board. Participants who completed the survey received points worth approximately $3 and were entered into a raffle with a prize equivalent to $25,000 held every 3 months for which participants completing all types of Survey Sampling International surveys were eligible. According to the 2010 U.S. Census, 19.8% of U.S. households currently lack home-Internet access, but some individuals from these households have Internet access through smartphones. Therefore, although this sampling method does not yield a true national probability sample, it provides a diverse nonconvenience sample that is generally demographically and geographically representative of U.S. adults. The field period for data collection was September 21–29, 2010, so a large number of invitations were sent out. Because the survey was terminated when the allotted number of interviews was completed, we cannot ascertain how many individuals received invitations or the proportion of those receiving invitations that accessed the website; however, 3,756 adults accessed the website containing the National Stressful Events Survey description and survey, and 3,457 (92% cooperation rate) agreed to participate. Of those, 2,953 completed the survey (85.4% completion rate for those who agreed to participate and 78.6% completion rate for those who accessed the website). Survey data were weighted by age, sex, and race/ethnicity based on the 2010 U.S. Census. Sex, age, and race/ethnicity characteristics of the sample are included in Table 1.
Table 1.
Demographic Characteristics of Participants (Weighted)
| Variable | n | % | SE |
|---|---|---|---|
| Sex | |||
| Male | 1,415 | 47.9 | 1.4 |
| Female | 1,538 | 52.1 | 1.4 |
| Age (years) | |||
| 18–24 | 332 | 11.3 | 0.9 |
| 25–34 | 563 | 19.1 | 1.0 |
| 35–44 | 508 | 17.2 | 1.3 |
| 45–54 | 571 | 19.3 | 1.0 |
| 55–64 | 488 | 16.5 | 0.9 |
| 65 or older | 490 | 16.6 | 0.8 |
| Race/ethnicity | |||
| White | 2,214 | 75.0 | 1.5 |
| Black | 363 | 12.3 | 1.0 |
| Native American | 46 | 1.6 | 0.4 |
| Asian/Pacific Islander | 145 | 4.9 | 0.6 |
| Some other race | 50 | 1.7 | 0.8 |
| Two or more races | 135 | 4.6 | 1.0 |
| Hispanic ethnicity | |||
| Hispanic | 495 | 16.8 | 1.5 |
| Non-Hispanic | 2,458 | 83.2 | 1.5 |
Measures
Assessment of exposure to stressful events
Twenty-five close-ended questions measured exposure to DSM-IV or DSM-5 Criterion A events. Questions were prefaced by introductory remarks that provided an overview and definition of the types of events that were asked about and encouraged disclosure. For example, the introduction to questions measuring personal experiences of interpersonal violence included the following statement:
Many people tell us they have been victims of interpersonal violence. When we say interpersonal violence, we mean that someone was physically attacked or sexually violated by another person. These situations can be difficult to talk about, and they can happen at any time during your life, even when you are a child. The person committing the violence isn’t always a stranger but can be a parent or other relative, friend, romantic partner, someone else you know well, or even a spouse. These experiences can be extremely stressful and are not always reported to authorities or discussed with others. These things can happen to men as well as women.
Three questions were asked about other events (i.e., other than those they had been asked about in the close-ended questions) that produced physical injuries, fear of being seriously injured or killed, or a potential “other” event defined as “any extraordinarily stressful situation or event other than the ones that I have asked about.” Those who had experienced any of the three other stressful events were asked to provide a written description of that experience. Those responding affirmatively to one or more of the 28 screening questions were asked a series of follow-up questions to determine (a) how many times they had experienced stressful events; (b) which event they experienced first; and (c) if they had experienced multiple events, which one was the worst. For the purpose of these follow-up questions and for subsequent questions regarding PTSD symptom attribution to events, participants were presented with an abbreviated list of 14 event-type categories (representing a summary of major event types assessed using the initial 28-item screen). This included nine event types that would meet Criterion A1 as described in the DSM-IV and Criterion A as defined in the DSM-5 (i.e., accident/fire, disaster, exposure to hazardous chemicals, combat or presence in a warzone, physical or sexual assault, witnessing physical or sexual assault, harm to a family member or close friend due to violence or accident, death of a family member or close friend due to accident or violence, witnessing a dead body or body parts), a 10th event type that would only meet DSM-5 Criterion A (i.e., repeated or extreme exposure to aversive details of a traumatic event(s) not including exposure through electronic media, television, movies, or pictures unless this exposure is work-related); an 11th event type that would only meet DSM-IV Criterion A (death of a family member or close friend that was not violent or accidental), and the three other types of stressful events (other events resulting in injury, perceived as potentially life threatening, or perceived as extraordinarily stressful). We combined physical or sexual assault for the purpose of symptom attribution as “direct interpersonal violence,” which has been consistently identified as a class of events most likely to result in PTSD (e.g., Ozer, Best, Lipsey, & Weiss, 2003; Resnick, Kilpatrick, Dansky, Saunders, & Best, 1993).
Descriptive information was collected about the first event as well as the worst event (if applicable) including age at time of event and whether the participant thought they might be seriously injured or killed, experienced a panic attack during or shortly after the event, and/or experienced emotions of fear, anger, sadness, horror, violation of trust or embarrassment/shame during the event. Endorsement of fear of death or serious injury, experience of panic or other emotions was used to determine whether DSM-IV A2 criterion was met. In summary, the strategy used for assessment of exposure to stressful events was considerably more comprehensive than that typically used in many epidemiological studies, which often use checklists of events with limited introductions or follow-up probes. Therefore, it is likely that the approach used in the National Stressful Events Survey resulted in greater disclosure of traumatic events than would have occurred had a simple checklist of events been used.
Assessment of PTSD symptoms and functional impairment
For each of the 20 DSM-5 PTSD symptoms endorsed, a series of follow-up questions was presented. These obtained information about symptom recency; for symptoms present during the past month, participants were asked how much they had been bothered by the symptom during that month based on a 5-point scale (1 = Not at all, 5 = Extremely). For symptoms that referenced traumatic events (i.e., symptoms B1, 2, 3, 4, and 5; C1 and 2; D1 and D3), the first follow-up question determined which event type(s) were incorporated in the symptom content (e.g., what event or events were involved in the content of nightmares). For remaining PTSD symptoms not referencing specific events, the first follow-up question asked if the symptom began or got worse following an event or events. If they responded yes, they were asked which event type(s) occurred before the symptom began or got worse. Participants endorsing symptoms with content related to and/or onset or worsening following a stressor event were then presented with the abbreviated list of 14 event types described above, and asked to indicate which event type(s), if any, were related to symptoms. Selection of more than one event type was allowed.
Functional impairment as defined by the DSM-IV and the DSM-5 was assessed by five questions measuring how distressing it was when they had PTSD symptoms on a 5-point scale (1 = Not at all, 5 = Extremely), and whether PTSD symptoms produced problems with employment and in their personal life, relationships, or school. Functional impairment was positive if PTSD symptoms were quite a bit or extremely distressing for them, or they reported problems in one or more of the four areas of functioning.
Procedure
Cases in which other events were reported in the event-screening section were reviewed only if they were identified as an event that led to development/worsening or were related in content to all necessary symptom criteria to meet PTSD at the diagnostic level according to the DSM-IV or the DSM-5 using the Same Event PTSD definition described below. Narrative responses were reviewed by four doctoral-level PTSD experts after familiarizing themselves with the DSM-IV and DSM-5 Criterion A definitions and the interview question content assessing DSM-IV and DSM-5 Criterion A events. Reviewers determined whether each open-ended event met Criterion A definitions in the DSM-IV, the DSM-5, or both. In cases of rater disagreements, events were coded using a consensus process.
For events that met the definition for DSM-IV Criterion A1, descriptive information about the first and worst event was examined to determine if the A1 event also met the DSM-IV definition for Criterion A2.
Two methods were used to determine PTSD. The first method required that symptom thresholds for DSM-5 Criteria B (n = 1), C (n = 1), D (n = 2), and E (n = 2) be met to a combination of DSM-5 Criterion A event types. Thus, all symptom criteria thresholds must be met, but they could be met in response to any combination of Criterion A event types. This was designated the Composite Event PTSD definition. The second method required Criteria B, C, D, and E symptom thresholds to be met to the same Criterion A event type. Both Composite Event and Same Event PTSD definitions also required the functional impairment criterion to be met, indicating that the PTSD symptoms produced significant distress and/or impairment in functioning. Similar methods were used to determine Composite Event and Same Event PTSD based on the DSM-IV.
PTSD prevalence was determined for three periods: (a) lifetime (i.e., met criteria at any time), (b) past year (i.e., met criteria during the past 12 months), and (c) past 6 months (i.e., met criteria during the past 6 months). Lifetime, past-year, and past-6-month prevalence was calculated using Composite Event and Same Event definitions based on both the DSM-IV and the DSM-5.
Data Analysis
The Research Electronic Data Capture platform (Harris et al., 2009) was used to program the National Stressful Events Survey questionnaire and to record all survey data. All prevalence algorithms were computed as defined above using syntax programmed in SPSS 20. Taylor-series linearization was used for all standard error estimation given the weighted design of the study. The SAS-Callable SUDAAN software (Version 11.0; Research Triangle Institute, 2012) was used to generate weighted survey data, prevalence estimates, and χ2 tests. The z-score comparisons with other prevalence data were estimated with weighted prevalence estimates and survey-adjusted standard errors to compare whether PTSD prevalence was significantly different between the DSM-IV and the DSM-5. Difference scores were created and discordant pairs (e.g., diagnosis positive based on the DSM-IV, diagnosis negative based on the DSM-5) were analyzed using a dependent sample t test in Stata 12.
Results
Traumatic Event Exposure
Most respondents (89.7%) reported exposure to at least one DSM-5 Criterion A event (see Table 2). For comparison with other studies, we report the separate prevalence of direct sexual or physical assault by sex. The prevalence of either type of direct interpersonal violence victimization was 53.1% (58.6% of women and 47.1% of men), which included childhood physical abuse, aggravated assault (physical assault with a weapon, or with intent to kill or seriously harm perceived by the victim), rape, and other sexual assault (see Table 2). Prevalence of sexual assault victimization was 29.7% overall (42.4% among women and 15.8% among men). Physical assault victimization was 43.7% overall (44.9% of women and 42.4% of men).
Table 2.
Prevalence of Exposure to Events (Weighted)
| Event type | n | % | SE |
|---|---|---|---|
| DSM-5 Criterion A | |||
| Disaster | 1,491 | 50.5 | 1.3 |
| Accident/fire | 1,427 | 48.3 | 1.3 |
| Exposure to hazardous chemicals | 493 | 16.7 | 1.1 |
| Combat or warzone exposure | 231 | 7.8 | 0.7 |
| Physical or sexual assault | 1,568 | 53.1 | 1.3 |
| Witnessed physical/sexual assault | 982 | 33.2 | 1.3 |
| Witnessed dead bodies/parts unexpectedly | 667 | 22.6 | 1.1 |
| Threat or injury to family or close friend due to violence/accident/disaster | 956 | 32.4 | 1.2 |
| Death of family/close friend due to violence/accident/disaster | 1,529 | 51.8 | 1.3 |
| Work exposure | 340 | 11.5 | 0.9 |
| Other DSM-5 Criterion A event | 53 | 1.8 | 0.3 |
| Any DSM-5 event | 2,647 | 89.7 | 0.7 |
| DSM-IV Criterion A excluded from the DSM-5 | |||
| Threat or injury to family or close friend (nonviolent) | 93 | 3.2 | 0.6 |
| Sudden unexpected death (nonviolent) | 1,668 | 56.5 | 1.3 |
| Serious illness of self or close friend or family member | 5 | 0.2 | 0.1 |
| Other injury/life threat/other extremely stressful event | 1,245 | 42.2 | 1.3 |
| Any event | 2,766 | 93.7 | 0.5 |
Note. DSM-5 = Diagnostic and Statistical Manual of Mental Disorders (5th ed.; American Psychiatric Association [APA], 2013); DSM-IV = Diagnostic and Statistical Manual of Mental Disorders (4th ed.; APA, 1994).
Six DSM-5 Criterion A event types were experienced by 30% or more of the sample (see Table 2). Many participants had been exposed to more than one type of DSM-5 Criterion A event. The modal number of DSM-5 Criterion A event types within the full sample was 3 (M = 3.30, SD = 2.32).
Estimated Prevalence of PTSD
Lifetime, past-12-month, and past-6-month prevalence estimates of PTSD using the DSM-5 and current DSM-IV criteria are included in Table 3. Separate prevalence estimates based on Same Event and Composite Event PTSD definitions are included. Only two prevalence comparisons were statistically significant. The prevalence of the DSM-5 lifetime Composite Event PTSD and the prevalence of the DSM-5 past-12-month Same Event PTSD each was significantly lower than the corresponding prevalence according to the DSM-IV. In all other instances, the DSM-5 prevalence estimates were slightly lower, but differences were not statistically significant. Our study’s past-12-month DSM-IV prevalence of 6.3% was also compared with the past-12-month DSM-IV PTSD prevalence of 3.6% reported by Kessler, Chiu, Demler, Merikangas, and Walters (2005). Results indicated that the prevalence of past-12-month DSM-IV PTSD in the present study was significantly higher than the 12-month DSM-IV PTSD prevalence found by Kessler, Chiu, and colleagues (2005; z = −5.79, p < .001).
Table 3.
Prevalence of PTSD Based on Caseness Definitions (Weighted)
| Definition | DSM-IV (%) | SE | DSM-5 (%) | SE | t (df = 2952) |
|---|---|---|---|---|---|
| Composite event PTSD | |||||
| Lifetime | 10.6 | 0.8 | 9.4 | 0.8 | 30.87* |
| Past 12 months | 6.9 | 0.7 | 5.3 | 0.6 | 5.46 |
| Past 6 months | 5.1 | 0.6 | 4.2 | 0.6 | 4.55 |
| Same event PTSD | |||||
| Lifetime | 9.8 | 0.8 | 8.3 | 0.7 | 6.95 |
| Past 12 months | 6.3 | 0.7 | 4.7 | 0.6 | 46.96* |
| Past 6 months | 4.7 | 0.6 | 3.8 | 0.6 | 3.05 |
Note. DSM-IV = Diagnostic and Statistical Manual of Mental Disorders (4th ed.; American Psychiatric Association [APA], 1994); DSM-5 = Diagnostic and Statistical Manual of Mental Disorders (5th ed.; APA, 2013); PTSD = posttraumatic stress disorder. Dependent sample t tests with Taylor series linearization conducted to estimate standard errors.
p < .05.
Reasons for the Discrepancies Between the DSM-IV and the DSM-5
Using the Same Event definition for lifetime PTSD, 7.3% of the sample met diagnostic criteria according to the DSM-5 and the DSM-IV; 2.5% according to the DSM-IV, but not the DSM-5; and 1.0% according to the DSM-5, but not the DSM-IV. Thus, among the 9.8% meeting Same Event DSM-IV criteria, 75% also met the DSM-5 criteria, and 25% did not meet DSM-5 criteria. Of the 8.3% meeting Same Event DSM-5 criteria, 88% also met the DSM-IV criteria, and 12% did not meet DSM-IV criteria. Why did cases meet the DSM-IV, but not the DSM-5 criteria? Our analysis indicated that 60% of such cases occurred solely because of the revised Criterion A definition in the DSM-5 that now excludes indirect exposure due to nonviolent deaths (53% of cases discrepant with the DSM-IV and 90% of all cases that were discrepant only based on Criterion A). The remaining cases discrepant solely based on Criterion A met the DSM-5 PTSD criteria related to certain types of illness (10%). Apart from the 60% failing to meet DSM-5 criteria solely due to Criterion A, another 37% of the DSM-IV positive-only cases did not meet the DSM-5 criteria due to failure to have at least one active avoidance symptom. Another 2% of positive cases based on DSM-IV criteria did not meet the DSM-5 criteria because they met neither Criterion A nor Criterion C. Only 1% of the DSM-IV positive-only cases did not meet the DSM-5 criteria because they failed to meet Criterion D of the DSM-5.
Of the 12.2% of cases positive for DSM-5, but not DSM-IV criteria, none resulted from failure to meet Criterion A1, but 2% were due to not meeting Criterion A2 of the DSM-IV. Most cases meeting the DSM-5, but not the DSM-IV criteria were due to either not meeting the DSM-IV Criterion C (avoidance/numbing) or Criterion D (arousal). Specifically, 55% did not meet the DSM-IV Criterion C, 38% did not meet the DSM-IV Criterion D, and 5% met neither the DSM-IV C nor D criteria.
Prevalence of PTSD by Sex
Prevalence of PTSD was higher among women than men for all lifetime and current PTSD definitions (see Table 4). Past-12-month Same Event DSM-IV and DSM-5 PTSD prevalence for women and men was compared to past-12-month DSM-IV PTSD-prevalence data reported by Kessler, Chiu, and colleagues (2005), which were 5.2% among women and 1.8% among men, respectively. Results indicated that prevalence of past-12-month DSM-IV PTSD in the present study was significantly higher (z = −5.36 and −7.18, ps < .001) for women and men, respectively.
Table 4.
Prevalence of PTSD by Sex (Weighted)
| Definition |
DSM-IV (%)
|
DSM-5 (%)
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| % Male | SE | % Female | SE | χ2 | % Male | SE | % Female | SE | χ2 | |
| Composite event PTSD | ||||||||||
| Lifetime | 6.5 | 1.1 | 14.4 | 1.2 | 24.69*** | 5.7 | 1.0 | 12.8 | 1.1 | 22.02*** |
| Past 12 months | 4.7 | 1.0 | 8.8 | 1.0 | 8.14** | 3.2 | 0.9 | 7.3 | 0.9 | 10.39** |
| Past 6 months | 3.6 | 0.9 | 6.5 | 0.8 | 5.76* | 3.1 | 0.9 | 5.3 | 0.8 | 3.87* |
| Same event PTSD | ||||||||||
| Lifetime | 6.1 | 1.1 | 13.2 | 1.2 | 20.25*** | 5.4 | 1.0 | 11.0 | 1.1 | 14.15*** |
| Past 12 months | 4.4 | 1.0 | 8.1 | 1.0 | 6.76* | 3.0 | 0.8 | 6.2 | 0.9 | 6.60* |
| Past 6 months | 3.4 | 0.9 | 6.0 | 0.8 | 4.82* | 3.0 | 0.8 | 4.6 | 0.7 | 1.92 |
Note. DSM-IV = Diagnostic and Statistical Manual of Mental Disorders (4th ed.; American Psychiatric Association [APA], 1994); DSM-5 = Diagnostic and Statistical Manual of Mental Disorders (5th ed.; APA, 2013); PTSD = posttraumatic stress disorder. The Taylor series linearization method was used to obtain standard errors utilizing the SUDAAN software system.
p < .05.
p < .01.
p < .001.
Conditional Probability of Lifetime PTSD as a Function of Criterion A Event Type and Number of Events per the DSM-5
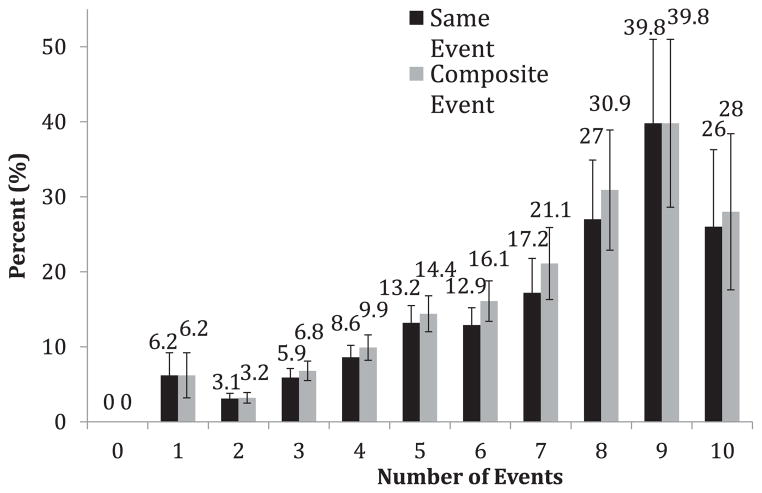
Lifetime DSM-5 PTSD prevalence varied as a function of the type of Criterion A event (see Table 5). Consistent with prior research, prevalence was highest among victims of interpersonal violence and combat. Prevalence of Same Event PTSD according to the DSM-5 among those reporting exposure to any DSM-5 Criterion A event was 9.3%. Same Event and Composite Event PTSD prevalence increased as a function of numbers of DSM-5 Criterion A event types experienced (see Figure 1).
Table 5.
Lifetime DSM-5 Prevalence as a Function of DSM-5 Criterion A Event Exposure (Weighted)
| DSM-5 Criterion A event | n | Composite event (%) | SE | Same event (%) | SE |
|---|---|---|---|---|---|
| Disaster | 1,491 | 10.1 | 1.0 | 0.4 | 0.1 |
| Accident/fire | 1,427 | 11.7 | 1.0 | 0.9 | 0.2 |
| Hazardous chemicals | 493 | 14.9 | 1.9 | 1.0 | 0.7 |
| Combat/war zone | 231 | 10.6 | 2.1 | 3.8 | 1.1 |
| Sexual/physical assault | 1,568 | 15.3 | 1.2 | 7.3 | 0.9 |
| Witnessed sexual or physical assault | 982 | 16.6 | 1.6 | 1.8 | 0.6 |
| Witnessed dead bodies | 667 | 15.9 | 2.0 | 1.4 | 0.5 |
| Family/close friend threat/injury | 956 | 16.7 | 1.6 | 2.5 | 0.9 |
| Death due to violence/accident/disaster | 1,529 | 13.5 | 1.3 | 4.3 | 1.0 |
| Work/secondary exposure | 340 | 17.7 | 3.2 | 0.2 | 0.2 |
| Any DSM-5 Criterion A event | 2,647 | 10.5 | 0.9 | 9.3 | 0.8 |
Note. DSM-5 = Diagnostic and Statistical Manual of Mental Disorders (5th ed.; American Psychiatric Association, 2013).
Figure 1.
Percentage with lifetime Same Event and Composite Event DSM-5 PTSD as a function of number of Criterion A event types.
Lifetime Same Event DSM-5 PTSD Specific to Single- or Multiple-Event Types
As noted, Figure 1 depicts prevalence of lifetime Same Event PTSD as a function of number of DSM-5 Criterion A event types. It does not, however, provide information on the number of event types to which all necessary symptom criteria were met. Within the full sample (N = 2,953), 91.7% did not meet Same Event PTSD criteria, 6.8% met Same Event criteria to only one event type, 0.9% met Same Event criteria to two event types, 0.4% met Same Event criteria to three event types, and 0.2% met Same Event criteria to four event types. For descriptive purposes, the distribution within the subgroup of the sample that met lifetime Same Event DSM-5 PTSD criteria to one or more event types (8.3% of the full sample), 81.5% met criteria to one event type; 10.5% met criteria to two event types; 5.4% met criteria to three events; and 2.6% met criteria to four event types.
Discussion
The study yielded several important findings examining, comparing, and identifying potential reasons for differences in national estimates of lifetime, past-year, and current PTSD prevalence using the DSM-IV and the DSM-5 criteria. First, consistent with other reports (Kessler, Sonnega, Bromet, Hughes, & Nelson 1995), the vast majority (89.7%) of the sample had experienced one or more DSM-5 Criterion A events. Similarly, the prevalence of sexual or physical assault was comparable to one of the most-cited national studies of U.S. adult men and women, which found prevalence of direct physical or sexual assault victimization to be 55% among women and 66.8% among men (Tjaden & Thoennes, 1998). Prevalence of accidental or violent deaths among close friends or family members was slightly higher than in some other national studies (e.g., Pietrzak, Goldstein, Southwick, & Grant, 2011). However, the present study included a more in-depth assessment of violent or accidental deaths using multiple questions assessing homicide, drunk-driving, suicide, drug-overdose, disaster, and accident-related deaths of close friends or family members that may provide a more sensitive and valid assessment of the range of violent deaths included in the DSM-5 Criterion A. The modal number of DSM-5 Criterion A event types experienced within the sample was 3, and the complex history of traumatic events raises questions about how to best assess PTSD symptoms when most individuals have experienced multiple traumatic events.
Second, the estimated U.S.-based population prevalence of DSM-5 PTSD was statistically significantly lower than the estimated DSM-IV PTSD population prevalence under both the broadest lifetime Composite Event definition and the narrowest past–12 month Same Event PTSD definition. PTSD prevalence according to the DSM-5 criteria was lower than the PTSD prevalence according to the DSM-IV criteria under the other four definitions although not significantly so. Thus, the changes made in the DSM-5 did not result in increased PTSD prevalence counter to the Calhoun et al. (2012) prediction that prevalence according to the DSM-5 criteria would be substantially higher under conditions in which true population prevalence according to the DSM-IV criteria was comparable to that found in the present study.
Third, the vast majority of individuals meeting lifetime criteria for Same Event PTSD met criteria for PTSD according to both the DSM-IV and the DSM-V. For those who met DSM-IV, but not DSM-5 PTSD criteria, the biggest factor was the exclusion of sudden, unexpected death not due to violence as a Criterion A event in DSM-5. This factor accounted for over 50% of all such discrepant cases. This finding is consistent with the results of Breslau and colleagues (1998) who observed that sudden, unexpected death was related to a high percentage of DSM-IV PTSD cases within a representative Detroit area sample. However, that study did not clearly distinguish between sudden unexpected deaths resulting from violence/accidents versus nonviolent causes. Additional research is needed to evaluate whether some types of nonviolent/accidental, but sudden unexpected deaths lead to similar patterns of PTSD symptoms and what key elements may be identified in such cases.
In the present study, the second major factor in discrepancy of cases meeting the DSM-IV but not DSM-5 criteria was failure to have at least one active avoidance symptom as required to meet DSM-5 Criterion C. As noted, concern has been raised about cases that might be missed due to this requirement. However, some argue that presence of active avoidance may increase distinctiveness of PTSD from some other disorders such as major depression (Forbes et al., 2011). The separation of active avoidance from other DSM-IV Criterion C items is also consistent with results of multiple-factor-analytic studies and role of avoidance in conceptualizations of PTSD (Friedman et al., 2011). In short, most would agree that avoidance is a key part of the PTSD construct and clinical picture, and most would agree that PTSD without active avoidance is not PTSD as we know it.
With respect to cases that were positive for lifetime same-event PTSD according to the DSM-5 criteria but not the DSM-IV criteria, most were due to failure to meet the old Criterion C (avoidance/numbing) or the old Criterion D (arousal). Failure to meet the DSM-IV Criterion C could occur, for example, if a participant met the DSM-5 Criterion D (negative alterations in cognitions and mood associated with the traumatic event/s) based solely on newly included symptoms (e.g., distorted blame, persistent negative emotional state), or endorsed only one numbing symptom consistent with the DSM-IV criteria and had endorsed only one DSM-5 Criterion C (active avoidance) symptom. Finally, some individuals met the DSM-5 Criterion E (marked alterations in arousal and reactivity associated with the traumatic event/s), but not the DSM-IV Criterion D (arousal) by virtue of endorsing the newly included DSM-5 symptom describing reckless and self-destructive behavior as one of only two arousal criterion symptoms endorsed.
Fourth, the National Stressful Events Survey prevalence estimates of past year PTSD using the DSM-IV criteria were higher than those obtained in the National Comorbidity Survey-Replication (NCS-R; Kessler, Chiu, et al., 2005). Generally, patterns across sex were consistent with findings from the original NCS (Kessler et al., 1995) indicating similar magnitudes of elevated lifetime (Kessler, Berglund, et al., 2005) and past 12-month PTSD (Kessler, Chiu, et al., 2005) among women as compared to men. There are several potential reasons for the small DSM-IV PTSD prevalence difference across the two studies. The NCS-R is exemplary and used a sample drawn and weighted to be representative of the U.S. adult population in 2000. The NCS-R used an in-person assessment strategy with a highly structured interview to measure PTSD. The present National Stressful Events Survey sample was recruited from an online web panel, and our data were weighted to 2010 Census estimates of the U.S. adult population, which has different demographic characteristics than the 2000 Census (e.g., a higher proportion of Hispanics). These demographic changes in the U.S. population could account for some of the difference. The National Stressful Events Survey used a self-administered, highly structured survey approach. Fewer people were skipped out of the PTSD-symptom module in the National Stressful Events Survey than in the NCS-R because we included people who reported exposure to other stressful events as well as Criterion A events. Another unique feature of the National Stressful Events Survey was the approach to assessment of PTSD in reference to any reported Criterion A event types as opposed to a select subset of events. This approach entailed asking about symptoms without a priori determining selected events. As described, those reporting symptoms then were asked to identify all types of events related to specific symptoms. Finally, a recent study by Wolford and colleagues (2008) found similar response rates and criterion validity for assessment of PTSD based on in-person interviews or assessments conducted by computer. In any case, the prevalence estimates based on DSM-IV criteria from the National Stressful Events Survey and the NCS-R are not so strikingly different as to call our major findings into question.
Fifth, findings related to lifetime prevalence of PTSD among those exposed to different types of traumatic events were important for two reasons. Findings were consistent with previous reports that the highest conditional probabilities of PTSD are associated with events involving interpersonal violence or military combat (e.g., Breslau et al., 1998; Kessler et al., 2005; Resnick et al., 1993). Although the conditional probabilities of PTSD to interpersonal violence and combat/war related events were relatively lower than those observed in studies noted above, this may partially relate to the breadth of events assessed (e.g., broad range of physical and sexual assault), the lack of selection of index events based on symptom endorsement that is included in the methodology of some studies, and the inclusion of all event types as opposed to worst or other selected index event as the method of PTSD assessment. Similarly, the event-specific PTSD prevalence of symptoms to a given event type is narrower than the conditional risk of Same Event PTSD (to any specific event) among those with a given history of the event type (e.g., sexual or physical assault). Conditional probabilities of PTSD using Composite Event and event-specific PTSD to an individual event type (depicted in Table 5) differed substantially for some stressor events. For example, the conditional probability of PTSD given disaster exposure was 10.1% using the Composite Event definition, but only 0.4% using the more rigorous event-specific definition. Thus, a hurricane survivor may have re-experiencing symptoms related to natural disaster, but may experience other PTSD symptoms to another experienced traumatic event such as a physical or sexual assault. Similar patterns occurred for other stressor-event types. This indicates that some events may appear to have higher conditional probability of producing PTSD than is actually the case unless the assessment strategy determines whether PTSD symptomatology is attributable to the index event versus the combination of several traumatic events.
Findings regarding the extent of exposure to multiple-event types and the extent to which multiple exposure resulted in higher risk of lifetime PTSD have implications for both how PTSD is conceptualized and for how it should be assessed. With respect to PTSD conceptualization, the field must move beyond a narrow focus on PTSD responses to a single event because it is clear from this and previous studies that exposure to multiple events is the norm and that the probability of PTSD increases with greater event exposure. These findings are consistent with previous reports indicating that prior- and/or multiple-traumatic-event exposure increases risk of PTSD (e.g., Ozer et al., 2003; Walsh et al., 2012). This pattern was also seen with the Same Event definition, suggesting a cumulative effect of exposure to prior-/multiple-event type(s) even when assessing PTSD in reference to a single-event type. Potential bidirectional associations between PTSD and traumatic-event exposure are also important to study and understand (e.g., Cougle, Resnick, & Kilpatrick, 2009).
Further research is needed to study implications of these findings with regard to risk factors for PTSD and implications for treatment. Understanding whether PTSD symptoms to one event may exacerbate the reaction to a subsequent event and/or conversely, the experience of a new event may reactivate or worsen symptoms to a previously experienced event(s) could add to knowledge regarding the impact of cumulative exposure to events. Such information might also be relevant to explore within treatment approaches that may need to more clearly address symptoms that relate to more than one traumatic event. Further study of potential underlying mechanisms (biological, psychological, behavioral, environmental) should be conducted to gain greater understanding of observed patterns.
Findings should be weighed in light of the study’s limitations. Findings were based on an Internet survey. The fact that the study did not include a true national probability sample of U.S. adults is a limitation, as is the fact that approximately 20% of U.S. adults without Internet access were excluded from the sampling frame. However, the use of a sample drawn from a geographically and demographically diverse national online panel and the application of weighting to the U.S. adult population based on age, sex, race, and ethnicity does offset this limitation and provides some ability to generalize findings to the population of U.S. adults. Also, the comparisons of PTSD prevalence based on the DSM-IV criteria versus the DSM-5 criteria were not affected by any discrepancies between our sample and a true national probability sample. The study did not include a clinician-administered assessment of PTSD, which many view as the gold standard for PTSD assessment, but clinician interviews are impractical and not the norm for large-scale epidemiologic studies. The use of a highly structured self-administered survey measuring traumatic event exposure and PTSD symptoms mitigates this limitation, but future research is needed that examines the concordance between diagnoses according to the DSM-5 criteria using the National Stressful Events Survey assessment procedure and approach with those obtained by clinicians using semistructured clinical interviews.
It is also clear that our strategy for assessing PTSD differed from that used in other studies comparing PTSD diagnoses using the DSM-IV and the DSM-5 criteria (e.g., Calhoun et al., 2012; Elhai et al., 2012). This includes the fact that methods in the current study allowed for assessment of PTSD to any qualifying traumatic event rather than to a single index event (and/or subset of worst or randomly selected event as in other epidemiological reports). Also, it is reasonable to assume that differences in how the new and modified DSM-5 Criterion A events and symptoms were worded and measured may have accounted for some of the differences in PTSD prevalence found. Also, differences in samples and patterns of exposure to traumatic events across studies are likely to have contributed to PTSD-prevalence differences based on the DSM-5 criteria. However, the current sample was more representative of the general population than samples used in these previous studies, and Criterion A events and symptoms were measured using language reviewed by the DSM-5 Sub-work Group to operationalize the PTSD diagnosis. We also compared the draft PTSD criteria and text language of the DSM-5 with that used in the published DSM-5 (APA, 2013). Although there are some relatively minor changes in wording in the symptoms, the questions used in the National Stressful Events Survey are consistent with the finalized symptom descriptions. Therefore, we believe that findings from this study can be used to provide a reasonable preliminary estimate of PTSD prevalence within the U.S. adult population based on the DSM-5 criteria.
Finally, we believe that the National Stressful Events Survey findings, along with other recent reports, may assuage concerns that changes in PTSD would be problematic. Revisions had minimal effect on PTSD prevalence among the general population of U.S. adults. A previous publication using symptom data from the National Stressful Events Survey and a convenience sample of veterans conducted confirmatory factor and item-response-theory analyses and found support for the new DSM-5 symptom clusters (Miller et al., 2012). Further support for the reliability of the PTSD construct as revised in the DSM-5 was provided by DSM-5 field trial results, which found PTSD to have one of the highest test-retest reliabilities of any diagnosis (κ = .67) based on clinician interviews (Freedman et al., 2013). Based on these results, the authors concluded that “ … PTSD is now a reliable diagnosis … ” (p. 3). Therefore, evidence is consistent with a DSM-5 PTSD diagnosis that is reliable, has evidence of construct validity, is not substantially different in terms of prevalence based on the DSM-IV criteria, but that includes changes in Criterion A, in PTSD symptoms, and in PTSD symptom clusters. From clinical and research perspectives, the challenge is to develop and evaluate new assessment tools that can measure exposure to DSM-5 traumatic events and DSM-5 PTSD symptoms. We believe that the National Stressful Events Survey assessment measure could be modified to accomplish this task. Specifically, a self-administered assessment tool that can measure exposure to DSM-5 traumatic events, PTSD symptoms, and functional impairment and that can capture the complexity of multiple traumatic event exposure on PTSD symptomatology could prove useful to clinicians as well as researchers.
Acknowledgments
This research was funded by an American Psychiatric Association DSM grant to Dean Kilpatrick and by funding from the U.S. Department of Veterans Affairs Mental Health Services. This work was supported in part by the South Carolina Clinical & Translational Research Institute, with an academic home at the Medical University of South Carolina, National Institute of Health Grant numbers UL1 RR029882 and UL1 TR000062. Manuscript preparation was supported by NIMH grant T32 MH018869 (Principal Investigator: Dean G. Kilpatrick), National Institute on Drug Abuse grant R01 DA023099 (Principal Investigator: Heidi Resnick), and Veterans Affairs Merit Review Award 5I01CX000431-02 (Principal Investigator: Mark W. Miller). We acknowledge Brittany Baber’s significant role in interview programming, and colleagues Drs. Kirstin Gros, Constance Guille, Kate Walsh, and Dawne Vogt for reviews of interview questions and/or classification of open ended stressor event descriptions.
Footnotes
Contents are solely the responsibility of the authors and views expressed do not necessarily represent those of the APA or other agencies supporting this research.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text rev. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: Author; 2013. [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community. Archives of General Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Calhoun PS, Hertzberg JS, Kirby AC, Dennis MF, Hair LP, Dedert EA, Beckham JC. The effect of draft DSM-V criteria on posttraumatic stress disorder prevalence. Depression and Anxiety. 2012;29:1032–1042. doi: 10.1002/da.22012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cougle JR, Resnick H, Kilpatrick DG. A prospective examination of PTSD symptoms as risk factors for subsequent exposure to potentially traumatic events among women. Journal of Abnormal Psychology. 2009;118:405–411. doi: 10.1037/a0015370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhai JD, Miller ME, Ford JD, Biehn TL, Palmieri PA, Frueh BC. Posttraumatic stress disorder in DSM-5: Estimates of prevalence and symptom structure in a nonclinical sample of college students. Journal of Anxiety Disorders. 2012;26:58–64. doi: 10.1016/j.janxdis.2011.08.013. [DOI] [PubMed] [Google Scholar]
- Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress. 1993;6:459–473. doi: 10.1002/jts.2490060405. [DOI] [Google Scholar]
- Forbes D, Fletcher S, Lockwood E, O’Donnell M, Creamer M, Bryant RA, Silove D. Requiring both avoidance and emotional numbing in DSM-V PTSD: Will it help? Journal of Affective Disorders. 2011;130:483–486. doi: 10.1016/j.jad.2010.10.032. [DOI] [PubMed] [Google Scholar]
- Freedman R, Lewis DA, Michaels R, Pine DS, Schultz SK, Tamminga CA, Yager J. The initial field trials of DSM-5: New blooms and old thorns. American Journal of Psychiatry. 2013;170:1–5. doi: 10.1176/appi.ajp.2012.12091189. [DOI] [PubMed] [Google Scholar]
- Friedman MJ, Resick PA, Bryant RA, Brewin CR. Considering PTSD for DSM-5. Depression and Anxiety. 2011;28:750–769. doi: 10.1002/da.20767. [DOI] [PubMed] [Google Scholar]
- Frueh BC, Elhai JD, Acierno R. The future of posttraumatic stress disorder in the DSM. Psychological Injury and Law. 2010;3:260–270. doi: 10.1007/s12207-010-9088-6. [DOI] [Google Scholar]
- Harris PA, Thielke R, Taylor R, Gonzalez N, Conde JG. Research Electronic Data Capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R) Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. Retrieved from http://www.hcp.med.harvard.edu/ncs/publications.php. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of twelvemonth DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R) Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. Retrieved from http://www.hcp.med.harvard.edu/ncs/publications.php. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Co-morbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.100210.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Acierno R. Should PTSD Criterion A be retained? Journal of Traumatic Stress. 2009;22:374–383. doi: 10.1002/jts.20436. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Baber B, Guille C, Gros K. The National Stressful Events Web Survey (NSES-W) Charleston, SC: Medical University of South Carolina; 2011. [Google Scholar]
- McFarlane AC. Redefining PTSD in DSM-5: Conundrums and potentially unintended consequences. In: Stein DJ, Friedman MJ, Blanco C, editors. Post-traumatic stress disorder. West Sussex, UK: Wiley-Blackwell; 2011. pp. 42–47. [Google Scholar]
- Miller MW, Wolf EJ, Kilpatrick D, Resnick H, Marx BP, Holowka DW, Friedman MJ. The prevalence and latent structure of proposed DSM-5 posttraumatic stress disorder symptoms in US national and veteran samples. Psychological Trauma: Theory, Research, Practice and Policy. 2012 doi: 10.1037/a0029730. advance online publication. [DOI] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, Weiss DW. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: Results from Wave 2 of the National Epidemiologic survey on alcohol and related conditions. Journal of Anxiety Disorders. 2011;25:456–465. doi: 10.1016/j.janxdis.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Research Triangle Institute. SUDAAN (Release 11.0.0) [Computer software] Research Triangle Park, NC: Author; 2012. [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology. 1993;61:984–991. doi: 10.1037/0022-006X.61.6.984. [DOI] [PubMed] [Google Scholar]
- Tjaden P, Thoennes N. Prevalence, incidence, and consequences of violence against women. Research in Brief (NCJ172837) Washington, DC: U.S. Department of Justice, National Institute of Justice; 1998. [Google Scholar]
- United States Census Bureau. Census. 2010 Accessed at: http://www.census.gov/2010census/
- Walsh K, Danielson CK, McCauley JL, Saunders BE, Kilpatrick DG, Resnick HS. National prevalence of posttraumatic stress disorder among sexually revictimized adolescent, college, and adult household-residing women. Archives of General Psychiatry. 2012;69:935–942. doi: 10.1001/archgenpsychiatry.2012.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolford G, Rosenberg SD, Rosenberg HJ, Swartz MS, Butterfield MI, Swanson JW, Jankowski MK. A clinical trial comparing interviewer with computer-assisted assessment among clients with severe mental illness. Psychiatric Services. 2008;59:769–775. doi: 10.1176/ps.2008.59.7.769. [DOI] [PubMed] [Google Scholar]