To the Editor,
Musculoskeletal disorders (MSDs) are among the most common and costly health problems among working populations, and constitute a major cause of disability.(1) Occupational health practitioners must manage, prevent, and assess the work-relatedness of this large and diverse set of disorders, which affect different body parts and have different risk factors, treatments, and prognoses. The relationships of workplace exposures to MSDs are often difficult for practitioners to assess, due to the multifactorial nature of these disorders, differing findings in the medical literature on associations between personal and work-related factors, and the difficulties of applying existing literature to an individual patient. However, assessment of work related factors is often central to decisions regarding treatment, work ability, and compensation.
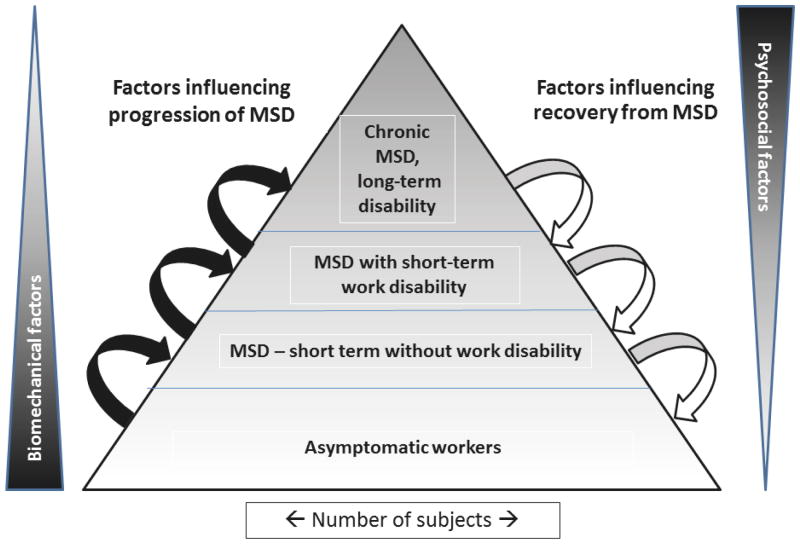
The multi factorial nature of MSDs has been well described: personal, psychosocial, and workplace physical exposures are all associated with higher rates of MSDs in working populations.(2–7) Assessment of etiology is made more complex because MSDs at any body part comprise a diverse set of outcomes, ranging from symptoms of discomfort to long-term work disability. Discussions of work-related risk factors for MSD often fail to consider that different risk factors may affect different stages of disease severity. For instance, risk factors assessed among workers presenting for surgery or among those with long-term disability may be different from risk factors assessed among newly symptomatic workers. While integrated models of impairment and disability describe this spectrum of severity,(8) these models do not explicitly address differences in work-related etiological or prognostic factors among workers with different outcomes.(9–11) We present a diagram of a simple conceptual model (figure 1) that may clarify this issue for researchers and practitioners.
Figure 1. Diagram on a conceptual model suggested the “pyramid of disability”.
Figure 1 shows a pyramid of disability, with the base comprising workers without symptoms of MSD. Some workers subsequently experience symptoms of MSD but do not seek treatment, while others seek treatment but experience no work disability. A smaller number of them progress to short-term or chronic functional impairment and work disability. As risk changes, recovery of function and alleviation of symptoms occurs, and workers move back down to lower levels of the pyramid. Therapeutic interventions, work related and non-work related exposures to physical and psychosocial stressors, medical co-morbidities, workplace policies, and a variety of other personal and social factors can mediate transitions between levels of this pyramid. The risk factors that play a predominant role in the initial transition from asymptomatic to symptomatic may differ from factors that most strongly affect prognosis and disability among symptomatic workers. There are suggestions in the existing literature that work-related biomechanical factors are probably more strongly associated with initial incidence of MSD and transitions between states at the bottom of the pyramid,(4,12–14) while psychosocial and psychological factors may be more strongly associated with outcome and prognosis.(15) These differences in contribution are likely relative, not absolute - psychosocial factors may play a role in early presentation of some disorders,(5,16) and changes in workplace ergonomics have been associated with faster return-to-work among those with long-term work absence.(17)
Few studies have examined separately the risk factors for transitions between different stages of symptoms and disability, nor have most reviews considered separately the risk factors for different outcomes such as MSD without time loss and MSD with prolonged time loss. If the risk factors for these outcomes differ, this may explain some of the lack of clarity in the current literature on work-related risk factors and MSDs. It may also explain to some extent the different views of the work-relatedness of MSDs held by different practitioners. Musculoskeletal specialists such as rheumatologists, rehabilitation specialists, and hand or back surgeons typically see workers referred because of prolonged symptoms or work disability, while primary care physicians or occupational health practitioners may be the first to see a newly symptomatic worker; different practitioners may form different conceptions of association between work and MSD that are relevant to their typical patient population. However, research findings or clinical experience related to particular MSD outcomes may not be generalizable to outcomes with greater or lesser severity.
We suggest that clinical practice and future research consider that factors influencing the onset, progression, and recovery from different stages of MSD severity are probably different, and assessments of work related factors should take into account different stages of MSD severity and progression toward impairment and disability. Limitations came from the variability of the context and the prevalence,(18) the multifactorial nature of MSD and the complex relationships between biomechanical and psychological,(19) with the possibility of highly exposed workers who might not develop any disability.(20) The model we have presented is simplistic and requires empiric validation, but may be useful in explaining differences in views and research findings on work-related risk factors and MSDs. It might encourage further discussions and practical studies in area of etiology, prevention, and treatment.
Acknowledgments
This study was supported by ANSES (French agency for Food, Environmental and Occupational Health Safety, APR EST 2011 TeMIS, CDC/NIOSH (grant # R01OH008017-01) and by the National Center for Research Resources (NCRR) (grant # UL1 RR024992), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of ANSES, NIOSH, NCRR, or NIH
Footnotes
No conflict of interest
References
- 1.McDonald M, DiBonaventura M daCosta, Ullman S. Musculoskeletal pain in the workforce: the effects of back, arthritis, and fibromyalgia pain on quality of life and work productivity. J Occup Environ Med. 2011;53(7):765–770. doi: 10.1097/JOM.0b013e318222af81. [DOI] [PubMed] [Google Scholar]
- 2.Bongers PM, de Winter CR, Kompier MA, Hildebrandt VH. Psychosocial factors at work and musculoskeletal disease. Scand J Work Environ Health. 1993;19(5):297–312. doi: 10.5271/sjweh.1470. [DOI] [PubMed] [Google Scholar]
- 3.Hagberg M, Silverstein BA, Wells R, Smith MJ, Herbert R, Hendrick HW, et al. Work related musculoskeletal disorders (WMSDs). A reference book for prevention. Bristol: Taylor and Francis; 1995. [Google Scholar]
- 4.Sluiter BJ, Rest KM, Frings-Dresen MH. Criteria document for evaluating the work-relatedness of upper-extremity musculoskeletal disorders. Scand J Work Environ Health. 2001;27(Suppl 1):1–102. [PubMed] [Google Scholar]
- 5.Andersen JH, Kaergaard A, Frost P, Thomsen JF, Bonde JP, Fallentin N, et al. Physical, psychosocial, and individual risk factors for neck/shoulder pain with pressure tenderness in the muscles among workers performing monotonous, repetitive work. Spine. 2002;27(6):660–667. doi: 10.1097/00007632-200203150-00017. [DOI] [PubMed] [Google Scholar]
- 6.Jansen JP, Morgenstern H, Burdorf A. Dose-response relations between occupational exposures to physical and psychosocial factors and the risk of low back pain. Occup Environ Med. 2004;61(12):972–979. doi: 10.1136/oem.2003.012245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Macdonald LA, Härenstam A, Warren ND, Punnett L. Incorporating work organisation into occupational health research: an invitation for dialogue. Occup Environ Med. 2008;65(1):1–3. doi: 10.1136/oem.2007.033860. [DOI] [PubMed] [Google Scholar]
- 8.Finger ME, Glässel A, Erhart P, Gradinger F, Klipstein A, Rivier G, et al. Identification of relevant ICF categories in vocational rehabilitation: a cross sectional study evaluating the clinical perspective. J Occup Rehabil. 2011;21(2):156–166. doi: 10.1007/s10926-011-9308-2. [DOI] [PubMed] [Google Scholar]
- 9.Armstrong TJ, Buckle P, Fine LJ, Hagberg M, Jonsson B, Kilbom A, et al. A conceptual model for work-related neck and upper-limb musculoskeletal disorders. Scand J Work Environ Health. 1993;19(2):73–84. doi: 10.5271/sjweh.1494. [DOI] [PubMed] [Google Scholar]
- 10.Marras WS. State-of-the-art research perspectives on musculoskeletal disorder causation and control: the need for an intergraded understanding of risk. J Electromyogr Kinesiol. 2004;14(1):1–5. doi: 10.1016/j.jelekin.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 11.Hagberg M, Violante F, Bonfiglioli R, Descatha A, Gold J, Evanoff B, et al. Prevention of musculoskeletal disorders in workers: classification and health surveillance - statements of the Scientific Committee on Musculoskeletal Disorders of the International Commission on Occupational Health. BMC musculoskeletal disorders. 2012;13(1):109. doi: 10.1186/1471-2474-13-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miranda H, Viikari-Juntura E, Heistaro S, Heliovaara M, Riihimaki H. A population study on differences in the determinants of a specific shoulder disorder versus nonspecific shoulder pain without clinical findings. Am J Epidemiol. 2005;161(9):847–855. doi: 10.1093/aje/kwi112. [DOI] [PubMed] [Google Scholar]
- 13.Van Tulder M, Koes B, Bombardier C. Low back pain. Best Pract Res Clin Rheumatol. 2002;16(5):761–775. doi: 10.1053/berh.2002.0267. [DOI] [PubMed] [Google Scholar]
- 14.Neupane S, Virtanen P, Leino-Arjas P, Miranda H, Siukola A, Nygård CH. Multi-site pain and working conditions as predictors of work ability in a 4-year follow-up among food industry employees. Eur J Pain. 2013 Mar;17(3):444–51. doi: 10.1002/j.1532-2149.2012.00198.x. [DOI] [PubMed] [Google Scholar]
- 15.Fransen M, Woodward M, Norton R, Coggan C, Dawe M, Sheridan N. Risk factors associated with the transition from acute to chronic occupational back pain. Spine. 2002;27(1):92–98. doi: 10.1097/00007632-200201010-00022. [DOI] [PubMed] [Google Scholar]
- 16.Cote P, van der, Cassidy JD, Carroll LJ, Hogg-Johnson S, Holm LW, et al. The burden and determinants of neck pain in workers: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine (Phila Pa 1976) 2008;33(4 Suppl):S60–S74. doi: 10.1097/BRS.0b013e3181643ee4. [DOI] [PubMed] [Google Scholar]
- 17.Loisel P, Abenhaim L, Durand P, Esdaile JM, Suissa S, Gosselin L, et al. A population-based, randomized clinical trial on back pain management. Spine. 1997;22(24):2911–2918. doi: 10.1097/00007632-199712150-00014. [DOI] [PubMed] [Google Scholar]
- 18.Coggon D, Ntani G, Vargas-Prada S, Martinez JM, Serra C, Benavides FG, et al. International variation in absence from work attributed to musculoskeletal illness: findings from the CUPID study. Occup Environ Med. 2013;70(8):575–584. doi: 10.1136/oemed-2012-101316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nguyen V, Teysseyre D, Herquelot E, Cyr D, Imbernon E, Goldberg M, et al. Effets à long terme des facteurs biomécaniques et psychosociaux professionnels sur les douleurs importantes de l'épaule dans la cohorte Gazel. Arch Mal Prof Environ. 2013;74(5):499–508. [Google Scholar]
- 20.Karjalainen K, Malmivaara A, van Tulder M, Roine R, Jauhiainen M, Hurri H, et al. Multidisciplinary biopsychosocial rehabilitation for neck and shoulder pain among working age adults. Cochrane Database Syst Rev. 2003;2:CD002194. doi: 10.1002/14651858.CD002194. [DOI] [PubMed] [Google Scholar]