The pituitary and placental glycoprotein hormone receptors belong to the G-protein-coupled receptor (GPCR) superfamily that contains seven transmembrane helices [1, 2]. Of these, the human luteinizing hormone/chorionic gonadotropin receptor (LHCGR) binds two structurally related hormones: luteinizing hormone (LH) and human chorionic gonadotropin (hCG), derived respectively from pituitary gonadotropes and placental syncytial trophoblasts [1, 2]. In the male LHCGRs are expressed primarily on Leydig cells, although their expression in prostate/prostate cell lines has also been reported [1–6]. In the female, LHCGRs are expressed on ovarian granulosa and thecal cells and regulate ovulation, corpus luteum function, and maintenance of pregnancy [1, 2, 7, 8]. Several studies indicate that LHCGRs are also expressed on various non-gonadal human tissues including the female reproductive tract [1, 2, 7–11]. Stimulation of LHCGRs by LH/hCG ligands results in cAMP production and steroidogenesis depending on cell type, ovary developmental stage and physiological context [7, 8, 12]. Various other intracellular signaling pathways are also affected, although much less is clear regarding their in vivo significance [7, 8]. In the adult female, signaling via LHCGRs is primarily required for ovulation. LHCGRs are under a tightly regulated ligand-mediated desensitization pathway that involves an LH receptor binding protein whose molecular identity, mechanism of action and regulation have been extensively studied in recent years [13–15].
A single gene designated LHCGR encodes the LHCGR that is essential for normal gonadal and reproductive function in both sexes [8, 13, 16, 17]. Although initially considered rare, in the past two decades, various mutations and polymorphisms have been identified in the human LHCGR (located on chromosome 2) that consists of 11 exons and 10 introns [18–23]. These include unique SNPs, or deletions, or point mutations identified throughout the LHCGR resulting in a spectrum of fertility/infertility phenotypes including sex reversal [18–23]. In this issue of JARG, Mitri et al., report a novel compound heterozygous mutation in the LHCGR and present interesting clinical phenotypes that manifest in the affected female patient (Mitri et al., A novel compound heterozygous mutation of the luteinizing hormone receptor: implications for fertility, doi:10.1007/s10815-014-0249-5).
A novel compound heterozygous mutation in the LHCGR
Clinical phenotypes and hormone profiles
The patient that Mitri et al. studied was a 33-year-old woman without any pediatric medical problems. She attained normal puberty, and was identified with primary amenorrhea during her adolescent years. She underwent progesterone treatment for several days and was maintained on monthly oral contraceptive pills for several years to curtail hot flashes. She was trying to conceive for 5 years. Her actual diagnosis was uncertain; she was suspected to have polycystic ovarian syndrome. Physical examination and ultrasound imaging confirmed she had normal reproductive tract development and accessory reproductive organs and displayed normal size uterus and ovaries containing several follicles. Laparoscopic ovarian drilling, intrauterine artificial inseminations, GnRH agonist, recombinant FSH, and hCG stimulation therapy were all performed without any success. Histological evaluation of ovarian biopsy revealed only early stage (primordial, primary, and intermediary) but not secondary, preantral, and antral (late stage mature) follicles. Interestingly, she became pregnant following transplantation of donor eggs and delivered a full-term baby girl without any complications during gestation.
The Authors next quantified baseline hormone levels (gonadotropins, androstenedione, free and total testosterone, and 17-hydroxy progesterone) using immunoassays. They did not find any significant differences and all hormones tested were within normal range. The patient exhibited poor or no response to stimulation by hCG and did not elicit an increased testosterone production.
Artificial Reproductive Technology (ART) protocols
After achieving pregnancy with donor eggs, the patient desired to conceive with her own eggs. Having identified that the patient had impaired ovarian folliculogenesis, the Authors sought ovarian stimulation protocol, in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI). They have initiated the IVF cycle with recombinant FSH stimulation, GnRH antagonist treatment, followed by multiple daily injections of recombinant FSH and finally GnRH agonist stimulation to induce ovulation. Because these protocols resulted in immature oocyte retrieval from smaller follicles, additional treatments were performed to obtain oocytes from larger follicles and mucify the cumulus–oocyte complexes. Ultimately, 7 oocytes were retrieved in 2 days, of which one was mature in MII stage and 6 were at germinal vesicle stage. In vitro maturation was then attempted in presence of amphiregulin (epidermal growth factor analogue) and this resulted in two additional oocytes that reached MII stage. Three embryos resulted upon ICSI but they did not reach the blastocyst stage and were arrested on day 5. Hence, embryo transfer was not performed.
DNA sequencing
As is the case with analysis of many mutations, the next logical step was to sequence the DNA of the patient, siblings and parents. The patient’s poor response to hCG, ovarian folliculogenesis defects, low E2 levels, and her older sister’s clinical history of inguinal gonads all pointed that LHCGR could be a likely suspect. The entire LHCGR was bi-directionally sequenced. The DNA sequencing analysis revealed interesting characteristics. First, both sisters and the patient’s mother showed a 27 bp deletion in exon 1 in one allele at position 34–60. This deletion is within the signal peptide encoding sequence and thus should produce a soluble or an ER-trapped receptor. Second, both sisters and the patient’s father showed an additional 2 bp (TC) heterozygous deletion in exon 11 resulting in a frame shift mutation, emergence of a premature stop codon and presumably truncated receptor. Finally, a missense mutation (Asn Δ Ser) in exon 10 at position 312 was also identified in both sisters and father. Thus, the patient separately inherited both the mutant alleles in heterozygous condition (and hence is compound heterozygous) from parents who are heterozygous for a single mutation (and hence are normal) that would likely result in production of abnormal LHCGRs and rendering the patient completely LH/hCG hormone-insensitive.
Final remarks and future directions
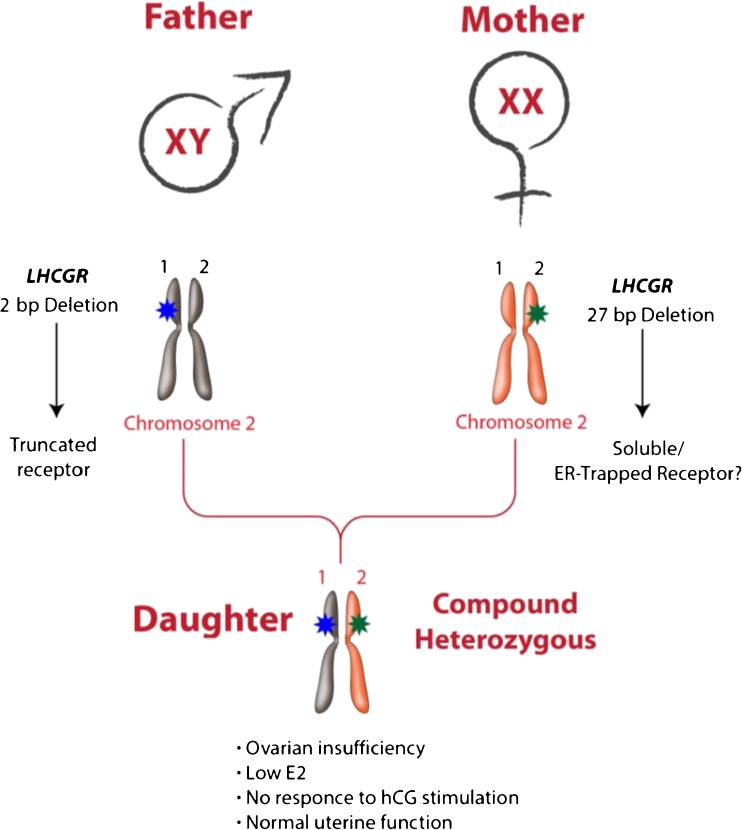
The report by Mitri et al. typifies the classical clinical phenotype–genotype analysis. This ultimately led to identifying the molecular basis of the infertility phenotype as a result of a novel compound heterozygous mutation in the LHCGR (Fig. 1). The Authors have also persistently and systematically followed the single patient, and received consent from family members. Although mutations in gonadotropins/gonadotropin receptors are considered rare [19, 20, 24, 25], the Authors have gone on to demonstrate that both the LHCGR alleles are “hit” with two different mutations in heterozygous condition, an event considered even more rare. Moreover, in the present study they also identified a novel mutation in exon I in the signal peptide encoding sequence that had never previously been reported. The report by Mitri et al. constitutes a series of emerging novel compound heterozygous mutations in a single gene [26–28]. A compound heterozygous mutation was reported nearly 2 years ago in luteinizing hormone beta subunit encoding gene (LHB) in a man [29]. His parents who carried individual heterozygous mutations of the gene were phenotypically normal and did not demonstrate any fertility defects [29].
Fig. 1.
LHCGR is located on short arm of human chromosome 2. In the report by Mitri et al., a female patient likely inherited each of the two heterozygous mutations in LHCGR from her parents. The paternal mutation is a 2 bp deletion predicted to result in a premature stop codon and truncated receptor. The maternal mutation is a 27 bp deletion in exon I encoding the signal peptide and results presumably in soluble or misrouted receptor that could get ER-retained. The parents were heterozygous carriers of a single mutation and did not display any fertility defects. The patient (daughter) carrying the compound heterozygous LHCGR exhibited severe fertility defects. She was able to achieve normal pregnancy when in vitro fertilized donor eggs were transplanted indicating normal uterine function. Colored stars indicate mutation on each of the alleles designated numerically 1 and 2
Mitri et al. also performed a variety of ART protocols, and succeeded in a patient achieving donor egg-derived pregnancy without any gestational complications. Although controversy exists on functional relevance of uterine LHCGRs with the existing Lhcgr mutant mouse models [30, 31], the present results by Mitri et al. establish that uterine LHCGRs are not indispensible for implantation and pregnancy maintenance in a single patient.
What remains to be studied with this interesting mutation reported by Mitri et al.? First, biochemical characterization of the individual and compound heterozygous mutant receptors expressed in vitro using cell lines and their intracellular distribution and trafficking could be studied [32]. Second, cases of sex reversal resulting in Leydig cell defects that could have been misdiagnosed as androgen-insensitivity could be re-visited and genetic screening of these patients for any potential mutations in LHCGR could be undertaken [33]. Third, di-genic and oligo-genic mutations in several genes that act in concert are known to cause a variety of human reproductive disorders [33–37]. It is likely that some forms of idiopathic infertility cases could result from heterozygous mutations in one allele of LHCGR and another yet unidentified gene (s). One could begin to analyze DNA samples from such patients using the emerging high-throughput sequencing approaches [33–37]. Finally, if indeed the 27 bp mutation in LHCGR exon I results in mis-routing and ER trapping of the mutant LHCGRs, attempts to rescue these misfolded/ER-trapped receptors in vitro [38] and eventually in patients using a pharmacoperone-based therapeutic approach should be feasible [25, 39, 40].
Acknowledgments
I thank Huizhen Wang and Stan Fernald for helping me with graphics design.
Footnotes
CAPSULE Discovery of a novel mutation in the LHCGR will prompt new strategies for the detection of human reproductive diseases based on gonadotropin insensitivity and their clinical management for infertile patients.
References
- 1.Bousfield GR, Jia L, Ward DN. Gonadotropins: chemistry and biosynthesis. Knobil and Neill's Physiology of Reproduction. 3 Vol 1. Elsevier Press, New York: ed Neill JD; 2006. pp. 1581–1634. [Google Scholar]
- 2.Pierce JG, Parsons TF. Glycoprotein hormones: structure and function. Annu Rev Biochem. 1981;50:465–495. doi: 10.1146/annurev.bi.50.070181.002341. [DOI] [PubMed] [Google Scholar]
- 3.Bodek G, Kowalczyk A, Waclawik A, Huhtaniemi I, Ziecik AJ. Targeted ablation of prostate carcinoma cells through LH receptor using Hecate-CGbeta conjugate: functional characteristic and molecular mechanism of cell death pathway. Exp Biol Med (Maywood) 2005;230(6):421–428. doi: 10.1177/15353702-0323006-10. [DOI] [PubMed] [Google Scholar]
- 4.Ingles SA, Liu SV, Pinski J. LHRH and LHR genotypes and prostate cancer incidence and survival. Int J Mol Epidemiol Genet. 2013;4(4):228–234. [PMC free article] [PubMed] [Google Scholar]
- 5.Liu SV, Liu S, Pinski J. Luteinizing hormone-releasing hormone receptor targeted agents for prostate cancer. Expert Opin Investig Drugs. 2011;20(6):769–778. doi: 10.1517/13543784.2011.574611. [DOI] [PubMed] [Google Scholar]
- 6.Pinski J, et al. Effect of luteinizing hormone on the steroidogenic pathway in prostate cancer. Prostate. 2011;71(8):892–898. doi: 10.1002/pros.21305. [DOI] [PubMed] [Google Scholar]
- 7.Richards JS. Hormonal control of gene expression in the ovary. Endocr Rev. 1994;15(6):725–751. doi: 10.1210/edrv-15-6-725. [DOI] [PubMed] [Google Scholar]
- 8.Richards JS, Pangas SA. The ovary: basic biology and clinical implications. J Clin Invest. 2010;120(4):963–972. doi: 10.1172/JCI41350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rao CV. Potential novel roles of luteinizing hormone and human chorionic gonadotropin during early pregnancy in women. Early Pregnancy : Biol Med : Off J Soc Investig Early Pregnancy. 1997;3(1):1–9. [PubMed] [Google Scholar]
- 10.Rao CV, Alsip NL. Use of the rat model to study hCG/LH effects on uterine blood flow. Semin Reprod Med. 2001;19(1):75–85. doi: 10.1055/s-2001-13914. [DOI] [PubMed] [Google Scholar]
- 11.Rao CV, Lei ZM. Consequences of targeted inactivation of LH receptors. Mol Cell Endocrinol. 2002;187(1–2):57–67. doi: 10.1016/S0303-7207(01)00694-3. [DOI] [PubMed] [Google Scholar]
- 12.Fan HY, Liu Z, Mullany LK, Richards JS. Consequences of RAS and MAPK activation in the ovary: the good, the bad and the ugly. Mol Cell Endocrinol. 2012;356(1–2):74–79. doi: 10.1016/j.mce.2011.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Menon KM, Menon B. Structure, function and regulation of gonadotropin receptors - a perspective. Mol Cell Endocrinol. 2012;356(1–2):88–97. doi: 10.1016/j.mce.2012.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Menon KM, Menon B, Wang L, Gulappa T, Harada M. Molecular regulation of gonadotropin receptor expression: relationship to sterol metabolism. Mol Cell Endocrinol. 2010;329(1–2):26–32. doi: 10.1016/j.mce.2010.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Menon KM, Munshi UM, Clouser CL, Nair AK. Regulation of luteinizing hormone/human chorionic gonadotropin receptor expression: a perspective. Biol Reprod. 2004;70(4):861–866. doi: 10.1095/biolreprod.103.024471. [DOI] [PubMed] [Google Scholar]
- 16.Ascoli M. Molecular basis of the regulation of the lutropin/choriogonadotropin receptor. Biochem Soc Trans. 1997;25(3):1021–1026. doi: 10.1042/bst0251021. [DOI] [PubMed] [Google Scholar]
- 17.Ascoli M, Fanelli F, Segaloff DL. The lutropin/choriogonadotropin receptor, a 2002 perspective. Endocr Rev. 2002;23(2):141–174. doi: 10.1210/edrv.23.2.0462. [DOI] [PubMed] [Google Scholar]
- 18.Huhtaniemi I. Mutations affecting gonadotropin secretion and action. Horm Res. 2003;60(Suppl 3):21–30. doi: 10.1159/000074496. [DOI] [PubMed] [Google Scholar]
- 19.Huhtaniemi IT, Themmen AP. Mutations in human gonadotropin and gonadotropin-receptor genes. Endocrine. 2005;26(3):207–217. doi: 10.1385/ENDO:26:3:207. [DOI] [PubMed] [Google Scholar]
- 20.Themmen AP. An update of the pathophysiology of human gonadotrophin subunit and receptor gene mutations and polymorphisms. Reproduction. 2005;130(3):263–274. doi: 10.1530/rep.1.00663. [DOI] [PubMed] [Google Scholar]
- 21.Themmen AP, Martens JW, Brunner HG. Activating and inactivating mutations in LH receptors. Mol Cell Endocrinol. 1998;145(1–2):137–142. doi: 10.1016/S0303-7207(98)00180-4. [DOI] [PubMed] [Google Scholar]
- 22.Themmen AP, Verhoef-Post M. LH receptor defects. Semin Reprod Med. 2002;20(3):199–204. doi: 10.1055/s-2002-35384. [DOI] [PubMed] [Google Scholar]
- 23.Themmen APN, Huhtaniemi IT. Mutations of gonadotropins and gonadotropin receptors: elucidating the physiology and pathophysiology of pituitary-gonadal function. Endocr Rev. 2000;21(5):551–583. doi: 10.1210/edrv.21.5.0409. [DOI] [PubMed] [Google Scholar]
- 24.Hotaling JM. Genetics of male infertility. Urol clin North Am. 2014;41(1):1–17. doi: 10.1016/j.ucl.2013.08.009. [DOI] [PubMed] [Google Scholar]
- 25.Ulloa-Aguirre A, Zarinan T, Dias JA, Conn PM. Mutations in G protein-coupled receptors that impact receptor trafficking and reproductive function. Mol Cell Endocrinol. 2014;382(1):411–423. doi: 10.1016/j.mce.2013.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brioude F, et al. Two families with normosmic congenital hypogonadotropic hypogonadism and biallelic mutations in KISS1R (KISS1 receptor): clinical evaluation and molecular characterization of a novel mutation. PLoS One. 2013;8(1):e53896. doi: 10.1371/journal.pone.0053896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Leanos-Miranda A, Ulloa-Aguirre A, Janovick JA, Conn PM. In vitro coexpression and pharmacological rescue of mutant gonadotropin-releasing hormone receptors causing hypogonadotropic hypogonadism in humans expressing compound heterozygous alleles. J Clin Endocrinol Metab. 2005;90(5):3001–3008. doi: 10.1210/jc.2004-2071. [DOI] [PubMed] [Google Scholar]
- 28.Tello JA, et al. Congenital hypogonadotropic hypogonadism due to GnRH receptor mutations in three brothers reveal sites affecting conformation and coupling. PLoS One. 2012;7(6):e38456. doi: 10.1371/journal.pone.0038456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Basciani S, et al. Hypogonadism in a patient with two novel mutations of the luteinizing hormone beta-subunit gene expressed in a compound heterozygous form. J Clin Endoc Metab. 2012;97(9):3031–3038. doi: 10.1210/jc.2012-1986. [DOI] [PubMed] [Google Scholar]
- 30.Lei ZM, et al. Targeted disruption of luteinizing hormone/human chorionic gonadotropin receptor gene. Mol Endocrinol. 2001;15(1):184–200. doi: 10.1210/mend.15.1.0586. [DOI] [PubMed] [Google Scholar]
- 31.Pakarainen T, Zhang FP, Poutanen M, Huhtaniemi I. Fertility in luteinizing hormone receptor-knockout mice after wild-type ovary transplantation demonstrates redundancy of extragonadal luteinizing hormone action. J Clin Invest. 2005;115(7):1862–1868. doi: 10.1172/JCI24562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Segaloff DL. Regulatory processes governing the cell surface expression of LH and FSH receptors. Sub-Cell Biochem. 2012;63:113–129. doi: 10.1007/978-94-007-4765-4_7. [DOI] [PubMed] [Google Scholar]
- 33.Crowley WF, Jr, Pitteloud N, Seminara S. New genes controlling human reproduction and how you find them. Trans Am Clin Climatol Assoc. 2008;119:29–37. [PMC free article] [PubMed] [Google Scholar]
- 34.Balasubramanian R, Crowley WF., Jr Isolated GnRH deficiency: a disease model serving as a unique prism into the systems biology of the GnRH neuronal network. Mol Cell Endocrinol. 2011;346(1–2):4–12. doi: 10.1016/j.mce.2011.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pitteloud N, et al. Digenic mutations account for variable phenotypes in idiopathic hypogonadotropic hypogonadism. J Clin Invest. 2007;117(2):457–463. doi: 10.1172/JCI29884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Seminara SB, Crowley WF., Jr Genetic approaches to unraveling reproductive disorders: examples of bedside to bench research in the genomic era. Endocr Rev. 2002;23(3):382–392. doi: 10.1210/edrv.23.3.0469. [DOI] [PubMed] [Google Scholar]
- 37.Seminara SB, Oliveira LM, Beranova M, Hayes FJ, Crowley WF., Jr Genetics of hypogonadotropic hypogonadism. J Endocrinol Investig. 2000;23(9):560–565. doi: 10.1007/BF03343776. [DOI] [PubMed] [Google Scholar]
- 38.Stewart MD, et al. Mice harboring Gnrhr E90K, a mutation that causes protein misfolding and hypogonadotropic hypogonadism in humans, exhibit testis size reduction and ovulation failure. Mol Endocrinol. 2012;26(11):1847–1856. doi: 10.1210/me.2012-1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Conn PM, et al. Transitioning pharmacoperones to therapeutic use: In vivo proof-of-principle and design of high throughput screens. Pharmacol Res : Off J Ital Pharmacol Soc. 2014;83C:38–51. doi: 10.1016/j.phrs.2013.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tao YX & Conn PM (2014) Chaperoning G Protein-coupled Receptors: From Cell Biology to Therapeutics. Endocrine reviews:er20131121. [DOI] [PMC free article] [PubMed]