Abstract
Pediatric loss of control (LOC) eating heightens risk for excessive weight gain and further disordered eating. Assessment of LOC typically involves self-report interview or laboratory test meal, although no study has concurrently examined data from both methods. We gathered eating episode data via interview (Child Eating Disorder Examination; ChEDE) and a laboratory test meal, among 22 overweight girls (aged 7-12 years) reporting LOC eating. Children consumed more energy during ChEDE episodes, although ChEDE and test meal episodes did not differ in macronutrient content. Episodes' correlation for amount consumed (grams) did not reach significance, p=.076. In exploratory analyses among the 7 children reporting LOC during the test meal, episodes were significantly correlated for grams consumed. Findings provide preliminary data to suggest that semi-structured interviews accurately capture children's LOC episode quantity. Episodes did not qualitatively differ, although children reported consuming more energy during self-reported episodes. Replication is warranted in larger studies.
Introduction and Aims
Loss of control (LOC) eating episodes are commonly reported by overweight children (Tanofsky-Kraff, 2009). LOC eating is associated with deficits in psychosocial functioning (Goldschmidt & Wilfley, 2009; Morgan et al., 2002). Children who report LOC eating are at risk for excessive weight and fat gain over time (Field et al., 2012; Tanofsky-Kraff et al., 2006; Tanofsky-Kraff, Yanovski, et al., 2009) and the development of partial and full-syndrome binge eating disorder (Tanofsky-Kraff et al., 2011).
Assessing LOC eating among children poses various challenges. Assessment often involves gathering data on a small number of eating episodes recently experienced by the child (e.g., self-reported recall), which may or may not be representative of their typical eating patterns. Semi-structured interviews, such as the Eating Disorder Examination adapted for Children (ChEDE) (Bryant-Waugh, Cooper, Taylor, & Lask, 1996), provide an opportunity to explicate constructs to youth to enhance comprehension, but self-report measures are susceptible to errors such as recall bias and social desirability. In particular, children may have difficulty reporting the content or features of LOC eating episodes accurately. For example, children may have difficulty understanding complex constructs such as LOC. Children also may have difficulty recalling the types and amounts of foods eaten; one study has demonstrated that children with LOC may underreport intake of dessert-type foods even immediately following a meal (Wolkoff et al., 2011). This difficulty may be due in part to the commonly-reported experience of feeling “numb” or “zoning out” during an LOC eating episode (Tanofsky-Kraff, Goossens, et al., 2007).
A controlled laboratory test meal setting provides the opportunity to measure a child's food intake directly. However, the laboratory setting has its own limitations, including its relative unfamiliarity to the child, the limited types and amounts of foods that can be made available, and the high cost (both financial and regarding the time and effort involved in executing laboratory test meals), often enabling only one or two test meals to be administered per child within a research study.
The limitations of self-report interviews and laboratory test meals may impact the ability of results to generalize to a child's naturalistic, day-to-day dietary intake. Comparing data across measures may help clarify the relation between dietary intake as reported by children and as directly observed in the laboratory. Concordance between episodes gathered from each method may indicate that data obtained in a controlled research setting reflects a child's actual overall dietary intake. In particular, across studies using both retrospective self-report (Theim et al., 2007) and laboratory test meals (Tanofsky-Kraff, McDuffie, et al., 2009), children with LOC consume a lower proportion of energy from protein, and a greater proportion of intake from carbohydrates and from dessert and snack-type foods. These relatively more energy-dense episodes may be indicative of an overall diet that promotes excess weight gain over time. However, no study has concurrently examined the reported and observed eating episodes of children with LOC within the same study.
Within a sample of overweight girls reporting LOC eating, the present study gathered initial pilot data comparing two eating episodes per child: a LOC episode as reported on the ChEDE and a meal consumed during a laboratory test meal paradigm. The total energy (kcal) consumed, macronutrient content, and types of foods (e.g., snacks, desserts) were compared between episodes. It was hypothesized that total energy, macronutrients, and food types would be concordant between eating episode measurements.
Methods
Data were drawn from a study comparing the impact of a negative mood versus a neutral mood induction prior to a laboratory test meal (Goldschmidt, Tanofsky-Kraff, & Wilfley, 2011). For the purposes of the present study, only data from the initial screening visit and the neutral meal were used.
Participants
Overweight and obese girls (N = 22) aged 6 to 12 years) were recruited as part of an investigation of pediatric eating behaviors. Girls' mean age was 10.6 ± 1.8 (range 7.5 – 12.9 years). Overweight was defined as a body mass index (BMI, kg/m2) ≥ 85th percentile for age and sex, according to CDC growth charts (Kuczmarski et al., 2000). Children's mean z-BMI score was 2.3 ± 0.40, and the racial/ethnic breakdown of the sample was 59% African-American, 23% White, 5% American Indian/Alaskan Native. The remaining 14% self-identified as “Other.”
Children were included if they reported having experienced at least one episode of LOC eating in the past three months. Exclusion criteria included medications known to affect weight/appetite, and conditions affecting diet/appetite (e.g., thyroid disease) or ability to sustain attention during a pre-test meal mood induction (e.g., attention deficit/hyperactivity disorder). Participants were recruited from the community through multiple outlets (e.g., local schools, children's hospitals, pediatrician referrals, advertisements at local organizations, participants from previous studies who had agreed to be contacted). All eligible participants received a $25 gift card for participation at each study visit ($75 total) and were offered a free group behavioral weight loss treatment (Epstein, Myers, Raynor, & Saelens, 1998) at a later date.
Procedure
Each child was required to attend three study visits with a parent or caregiver. At the first visit, study procedures were explained and each child and parent provided written informed assent and consent, respectively. Participants completed questionnaire and interview assessments, and eligible families were then scheduled to return for two test meal visits on separate days. One of the test meals was conducted following a negative mood induction; these data are not included in the present analyses. Data for the present study was collected during the neutral mood induction (control) meal, which involved watching a neutral film clip (i.e., a series of scenes from the movie “Winged Migration” [Sony Pictures Classics, 2003]) prior to consuming the test meal). For additional details regarding study recruitment and procedure, please see the main outcome report (Goldschmidt et al., 2011).
Measures
Anthropometrics
Children's weight and height were measured in the clinic using a calibrated electronic scale and stadiometer, respectively, and used to calculate children's z-BMI (Kuczmarski et al., 2000).
Pubertal stage
Figured drawings of Tanner sexual stages were used to assess pubertal status. This less-invasive method for assessing pubertal stage has been well-validated in pre-adolescent children (Duke, Litt, & Gross, 1980; Neinstein, 1982; Schlossberger, Turner, & Irwin, 1992). Only pubic hair ratings were obtained in the current study, considering prior validation data for this population (Bonat, Pathomvanich, Keil, Field, & Yanovski, 2002).
Self-reported eating episode
The ChEDE (Bryant-Waugh et al., 1996), a child-adapted version of the adult Eating Disorder Examination (EDE) (Fairburn & Cooper, 2000), was administered to all children. The ChEDE assesses episodes of LOC eating in the past three months. For the purposes of the present study, the LOC eating episode that was deemed most pathological was selected, in keeping with previously used metholodology (Tanofsky-Kraff, Goossens, et al., 2007; Tanofsky-Kraff et al., 2004; Theim et al., 2007): an objective binge episode (OBE; an unambiguously large LOC episode), if one was present, or a subjective binge episode (SBE; a not unambiguously large LOC episode) if the child reported no OBEs. If multiple episodes of the same type were recorded (i.e., multiple OBEs, or multiple SBEs if no OBEs), the first one recorded by the interviewer was selected. All foods and amounts reported as consumed during the episode were recorded by the interviewer for analysis, as described below. The ChEDE has demonstrated good psychometric properties with children of this age group (Bryant-Waugh et al., 1996; Hilbert et al., 2013; Watkins, Frampton, Lask, & Bryant-Waugh, 2005).
Laboratory test meal eating episode
Children were provided with a test meal in the clinic designed to elicit LOC eating (Goldschmidt et al., 2011; Mirch et al., 2006; Tanofsky-Kraff, Haynos, Kotler, Yanovski, & Yanovski, 2007). Three hours prior to arriving at the clinic, participants were asked to consume a standard breakfast that was previously provided to them (a Kellogg's Nutri-grain® bar [140 kilocalories, 3 g fat] and a Nestle Juicy Juice® apple juice box [100 kilocalories, 0 g fat]). In a separate room from the test meal, children were asked to rate their hunger, fullness, and desire to eat, and then watched the neutral film. Children were then instructed to “let yourself go and eat as much as you like,” and then ate ad libitum from a multi-item, 10,000 kilocalorie buffet meal (56% carbohydrate, 33% fat, 11% protein) consisting of a range of common foods (e.g., sandwich components, fruit/vegetables, cookies, chips). Children were not monitored while eating (i.e., they were left alone in the room), and they were not told explicitly that their intake subsequently would be measured. Food items were weighed before and after the test meal using an XP-3000 Series Compact Balance Scale (Denver Instruments, Gottingen, Germany) to determine amounts consumed of each food type. For further procedural details, see Goldschmidt et al., 2011.
For each ChEDE episode and test meal, energy content (in kilocalories), weight (in grams), and macronutrient content (kilocalories from carbohydrate, fat, and protein) of foods consumed was determined using Nutritionist Pro Diet Analysis software (Axxya Systems, 2007). Additionally, energy consumed specifically from desserts and snacks was calculated, based on prior literature suggesting that this category of food is the type most likely to differ between eating episodes with and without LOC (Tanofsky-Kraff, McDuffie, et al., 2009; Theim et al., 2007). Beverages typically are not included when considering the size of an eating episode during administration of the ChEDE. Therefore, to ensure a parallel comparison between ChEDE and test meal episodes, energy and weight consumed from beverages was omitted from analyses.
Statistical analyses
All analyses were performed with IBM SPSS v19.0. The directional differences between the ChEDE and test meal episodes were calculated as the self-reported intake minus the actual intake consumed during the test meal (using the log-transformation of total grams and energy consumed, as well as the arcsine of the square root of percent energy from each macronutrient group and food category). Bland-Altman comparisons (Bland & Altman, 1986) confirmed that zBMI, age, and pubertal stage were not significantly related to differences in intake between the two measures, ps > .08; thus, these variables were not included as covariates in analyses. Further, total energy intake (log-transformed grams and kcal consumed during each episode) were not significantly correlated with differences in macronutrient or food category intake, ps >.06, and thus were not included as covariates in analyses.
Paired t-tests were conducted to compare each child's episode quantity (i.e., log-transformed kcal and grams consumed) and quality (i.e., arcsine of the square root of percentage energy from carbohydrates, fat, and protein, as well as from desserts/snacks).
Pearson correlations were conducted to examine the strength of relations between ChEDE episode intake and test meal episode intake, for total amount (grams) and energy (kcal) consumed, as well as arcsine of the square root of percentage intake from carbohydrates, protein, fat, and desserts and snacks.
Results
Differences in quantity were found between children's ChEDE and test meal episodes, in that total energy intake reported for children's ChEDE episodes (1151 ± 616 kcal) was significantly higher than their energy ingested during the test meal (808 ± 246 kcal), p = .012. However, children's ChEDE and test meal episodes did not significantly qualitatively differ (i.e., in macronutrient or food type content), ps > .07 (see Table 1).
Table 1. Size, Macronutrient Content, and Food Types Consumed during Test Meal Episodes and Self-reported Episodes on the Child Eating Disorder Examination (ChEDE).
| Test meal episode | ChEDE episode | t statistic | p-value | |
|---|---|---|---|---|
| Kilocalories (kcal) | 808 ± 246 | 1151 ± 616 | -2.270 | .034 |
| Grams | 357 ± 140 | 230 ± 127 | 4.348 | <.001 |
| % Kcal from Carbohydrates | 43% | 45% | -.676 | .506 |
| % Kcal from Fat | 43% | 39% | 1.758 | .093 |
| % Kcal from Protein | 14% | 17% | -1.863 | .076 |
| % Kcal from Desserts/snacks | 18% | 17% | 1.159 | .260 |
Note: Raw data (i.e., kcal, grams, and percentages) are presented here, although as noted above, statistical analyses were conducted on transformed variables (log-transformed kcal and grams consumed, and the arcsine of the square root of all percentages).
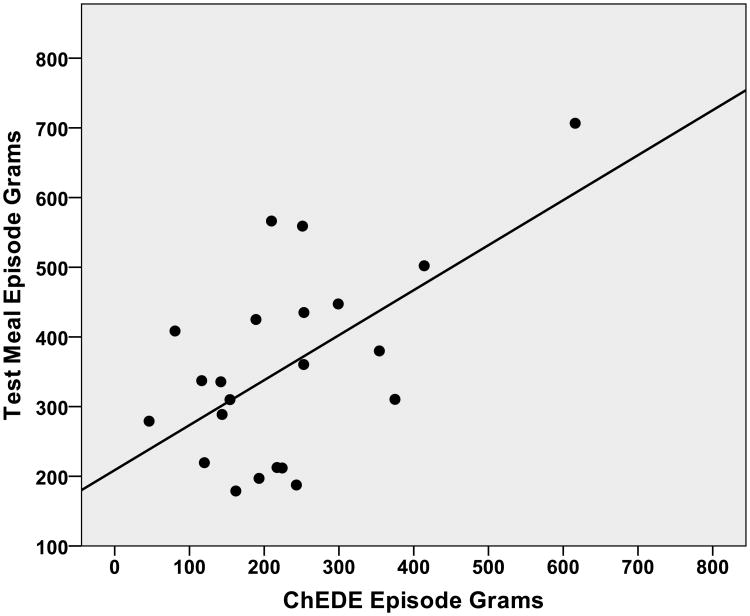
The correlation between children's ChEDE and test meal episodes' quantity with regard to grams of food consumed did not reach statistical significance, r = .386, p = .076 (see Figure 1). No other significant correlations were found between children's episodes, for: total energy intake, r = .273, p = .219, percent energy from carbohydrates, r = -.128, p = .570, fat, r = -.217, p = .332, or protein, r = .052, p = .819, or from desserts/snacks, r = .131, p = .561.
Figure 1.
Association between Grams of Food Consumed during Test Meal Episodes and Self-reported Episodes on the Child Eating Disorder Examination (ChEDE). Note: Raw data are presented here, although as noted above, statistical analyses were conducted on transformed variables (log-transformed kcal and grams consumed). r = .386, p = .076
Exploratory analyses were conducted only among the subset of children who reported experiencing LOC during the test meal (n = 7). When the above correlations were conducted only among these 7 children, children's ChEDE and test meal episodes were significantly correlated for grams consumed, r = .797, p = .034, and were correlated for total energy intake at r = .735, although this latter correlation did not reach statistical significance, p = .060. No other significant correlations were found between children's episodes, for: percent energy from carbohydrates, r = -.140, p = .765, fat, r = -.462, p = .296, or protein, r = .169, p = .717, or from desserts/snacks, r = -.076, p = .872.
Discussion
Children's dietary intake according to self-report (i.e., ChEDE) and observed during a laboratory test meal were overall not significantly associated, although when examining data only from children who specifically reported feeling a sense of LOC during the test meal, episodes' size (i.e., food consumed in grams) and energy consumed were correlated. These preliminary data suggest that semi-structured interviews seem to accurately capture the quantity of children's LOC episodes. Additionally, LOC eating episodes assessed via self-report and in a test meal did not qualitatively differ (i.e., macronutrient content or proportion of energy from desserts/snacks), indicating that children may select similar categories of foods when experiencing LOC, whether these eating episodes are in a laboratory or naturalistic setting.
Of note, however, episodes appeared to differ quantitatively in that test meal episodes contained a larger amount of food (in grams) whereas ChEDE episodes contained more energy (kcal). Despite apparently selecting a similar proportion of foods from the desserts and snacks category during each meal, one possibility is that children may consume more total energy when they have their preferred high-energy dense “binge foods” available in a naturalistic setting. As such, it may be important to offer these foods when assessing a child's eating within a laboratory test meal setting. That is, having these personalized food selections available to a child may yield meal data that are more representative of a child's typical LOC eating episode, as opposed to focusing on providing a wide range of foods. Additionally, children may underestimate the amount of food (i.e., grams of food) that they consumed when retrospectively reporting an eating episode, as compared to intake objectively measured in the lab, and this pattern may be even more pronounced among overweight children (Livingstone & Robson, 2000). Although all children in the present study reported LOC eating, one study has suggested that children with LOC (as compared to children without LOC) may be less accurate in reporting energy intake from carbohydrates and desserts, in particular (Wolkoff et al., 2011).
Interestingly, children consumed less energy when in the controlled laboratory setting, as compared to the naturalistic environment. Although results may have been impacted by measurement error inherent in self-reported eating episodes, the excess energy being ingested by children at LOC eating episodes (i.e., an estimated approximately 980 kcal in one meal, when averaging between assessment methods) predisposes overweight children to further excess weight gain. Of note, it also is possible that children felt more inhibited in their eating when in a controlled laboratory setting (despite instructions to “let themselves go”); for example, some children may have been concerned that their eating was being monitored and consequently felt more self-conscious than if they were eating alone in a real-life setting. Although interventions geared towards reducing or eliminating LOC eating among youth are likely to help ameliorate excess weight gain, the content and size of children's LOC reported eating episodes suggests that modifying children's environments to include few energy-dense foods may foster an overall lower caloric intake, despite the presence of LOC.
Overall, the present study provided preliminary evidence that among overweight girls who report LOC eating, assessment of LOC episodes via interview methods and using laboratory observation may be capturing similar patterns of eating. Of note, participants only included overweight pre-adolescent girls, recruited specifically for a study of eating behaviors; thus, children in the study (or their parents) may have had greater concerns about eating or weight as compared to the general population. Future replication of these results is needed to determine if findings replicate in larger samples and among boys and normal weight and/or non-treatment seeking children.
Acknowledgments
This work was made possible by NHLBI grant T32 HL007456 and the Academy for Eating Disorders Student Research Award (Dr. Goldschmidt), NIMH grant K24 MH070446 (Dr. Wilfley), and grant UL1 RR024992 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. The study authors had complete control of the protocol's execution, data collection, and analysis. Portions of this manuscript were presented at the 16th annual meeting of the Eating Disorders Research Society, Cambridge, MA.
Footnotes
Address where work was completed: Washington University School of Medicine, Department of Psychiatry, 660 S. Euclid Ave, St. Louis, MO, 63110
References
- Axxya Systems. Nutritionist Pro Diet Analysis. Stafford, TX: 2007. computer software. [Google Scholar]
- Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- Bonat S, Pathomvanich A, Keil MF, Field AE, Yanovski JA. Self-assessment of pubertal stage in overweight children. Pediatrics. 2002;110(4):743–747. doi: 10.1542/peds.110.4.743. [DOI] [PubMed] [Google Scholar]
- Bryant-Waugh RJ, Cooper PJ, Taylor CL, Lask BD. The use of the eating disorder examination with children: A pilot study. International Journal of Eating Disorders. 1996;19(4):391–397. doi: 10.1002/(SICI)1098-108X(199605)19:4<391∷AIDEAT6>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- Duke PM, Litt IF, Gross RT. Adolescents' self-assessment of sexual maturation. Pediatrics. 1980;66(6):918–920. [PubMed] [Google Scholar]
- Epstein LH, Myers MD, Raynor HA, Saelens BE. Treatment of pediatric obesity. Pediatrics. 1998;101(3 Pt 2):554–570. [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. (14th) 2000 doi: 10.1192/bjp.154.6.807. [DOI] [PubMed] [Google Scholar]
- Field AE, Sonneville KR, Micali N, Crosby RD, Swanson SA, Laird NM, et al. Horton NJ. Prospective association of common eating disorders and adverse outcomes. Pediatrics. 2012;130(2):e289–295. doi: 10.1542/peds.2011-3663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt AB, Tanofsky-Kraff M, Wilfley DE. A laboratory-based study of mood and binge eating behavior in overweight children. Eating Behaviors. 2011;12(1):37–43. doi: 10.1016/j.eatbeh.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt AB, Wilfley DE. Binge eating in children and adolescents. In: Chambers N, editor. Binge eating: Psychological factors, symptoms and treatment. Nova Publishers; New York: 2009. pp. 165–183. [Google Scholar]
- Hilbert A, Buerger A, Hartmann AS, Spenner K, Czaja J, Warschburger P. Psychometric evaluation of the eating disorder examination adapted for children. European Eating Disorders Review. 2013;21(4):330–339. doi: 10.1002/erv.2221. [DOI] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. Johnson CL. CDC growth charts: United States. Advance Data. 2000;(314):1–27. [PubMed] [Google Scholar]
- Livingstone MB, Robson PJ. Measurement of dietary intake in children. Proc Nutr Soc. 2000;59(2):279–293. doi: 10.1017/s0029665100000318. Review. [DOI] [PubMed] [Google Scholar]
- Mirch MC, McDuffie JR, Yanovski SZ, Schollnberger M, Tanofsky-Kraff M, Theim KR, et al. Yanovski JA. Effects of binge eating on satiation, satiety, and energy intake of overweight children. American Journal of Clinical Nutrition. 2006;84(4):732–738. doi: 10.1093/ajcn/84.4.732. doi: 84/4/732 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan CM, Yanovski SZ, Nguyen TT, McDuffie J, Sebring NG, Jorge MR, et al. Yanovski JA. Loss of control over eating, adiposity, and psychopathology in overweight children. International Journal of Eating Disorders. 2002;31(4):430–441. doi: 10.1002/eat.10038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neinstein LS. Adolescent self-assessment of sexual maturation: Reassessment and evaluation in a mixed ethnic urban population. Clinical Pediatrics. 1982;21(8):482–484. doi: 10.1177/000992288202100806. [DOI] [PubMed] [Google Scholar]
- Schlossberger NM, Turner RA, Irwin CE., Jr Validity of self-report of pubertal maturation in early adolescents. Journal of Adolescent Health. 1992;13(2):109–113. doi: 10.1016/1054-139x(92)90075-m. [DOI] [PubMed] [Google Scholar]
- Tanofsky-Kraff M. Binge eating among children and adolescents. In: Jelalian E, Steele R, editors. Handbook of Child and Adolescent Obesity. Springer Publishers; New York: [Google Scholar]
- Tanofsky-Kraff M, Cohen ML, Yanovski SZ, Cox C, Theim KR, Keil M, et al. Yanovski JA. A prospective study of psychological predictors of body fat gain among children at high risk for adult obesity. Pediatrics. 2006;117(4):1203–1209. doi: 10.1542/peds.2005-1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Goossens L, Eddy KT, Ringham R, Goldschmidt A, Yanovski SZ, et al. Yanovski JA. A multisite investigation of binge eating behaviors in children and adolescents. Journal of Consulting and Clinical Psychology. 2007;75(6):901–913. doi: 10.1037/0022-006X.75.6.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Haynos AF, Kotler LA, Yanovski SZ, Yanovski JA. Laboratory-based studies of eating among children and adolescents. Current Nutrition and Food Science. 2007;3(1):55–74. doi: 10.2174/1573401310703010055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, McDuffie JR, Yanovski SZ, Kozlosky M, Schvey NA, Shomaker LB, et al. Yanovski JA. Laboratory assessment of the food intake of children and adolescents with loss of control eating. American Journal of Clinical Nutrition. 2009;89(3):738–745. doi: 10.3945/ajcn.2008.26886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Shomaker LB, Olsen C, Roza CA, Wolkoff LE, Columbo KM, et al. Yanovski JA. A prospective study of pediatric loss of control eating and psychological outcomes. J Abnorm Psychol. 2011;120(1):108–118. doi: 10.1037/a0021406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Yanovski SZ, Schvey NA, Olsen CH, Gustafson J, Yanovski JA. A prospective study of loss of control eating for body weight gain in children at high risk for adult obesity. International Journal of Eating Disorders. 2009;42(1):26–30. doi: 10.1002/eat.20580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Yanovski SZ, Wilfley DE, Marmarosh C, Morgan CM, Yanovski JA. Eating-disordered behaviors, body fat, and psychopathology in overweight and normal-weight children. Journal of Consulting and Clinical Psychology. 2004;72(1):53–61. doi: 10.1037/0022-006X.72.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theim KR, Tanofsky-Kraff M, Salaita CG, Haynos AF, Mirch MC, Ranzenhofer LM, et al. Yanovski JA. Children's descriptions of the foods consumed during loss of control eating episodes. Eating Behaviors. 2007;8(2):258–265. doi: 10.1016/j.eatbeh.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins B, Frampton I, Lask B, Bryant-Waugh R. Reliability and validity of the child version of the Eating Disorder Examination: A preliminary investigation. International Journal of Eating Disorders. 2005;38(2):183–187. doi: 10.1002/eat.20165. [DOI] [PubMed] [Google Scholar]
- Wolkoff LE, Tanofsky-Kraff M, Shomaker LB, Kozlosky M, Columbo KM, Elliott CA, et al. Yanovski JA. Self-reported vs. actual energy intake in youth with and without loss of control eating. Eating Behaviors. 2011;12(1):15–20. doi: 10.1016/j.eatbeh.2010.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]