Abstract
Background
Preterm infants are at risk for postnatal growth failure (PGF). Identification of biomarkers that are associated with neonatal growth may help reduce PGF and associated long-term morbidity.
Objective
To investigate the associations between cord blood vascular endothelial growth factor (VEGF) and its soluble receptor (sFlt-1) with birth weight (BW) and postnatal growth in premature infants.
Study Design and Methods
From an ongoing birth cohort, 123 premature infants from 23 to 36 weeks gestational age (GA) were studied. Cord blood plasma VEGF and sFlt-1 were measured via enzyme-linked immunoassay. Growth parameters and nutritional information were evaluated. Multivariate logistic regression models were constructed to evaluate the associations of VEGF and sFlt-1 on PGF, defined as weight < 10th percentile at 36 weeks corrected age or discharge.
Results
VEGF was positively correlated, and sFlt-1 was negatively correlated with BW and BW-for-GA percentiles. Higher cord blood VEGF levels were associated with reduced risk of PGF (OR=0.7; 95% CI=0.5–0.9), while higher sFlt-1 levels appeared to increase the risk of PGF (OR=1.6; 95% CI=1.1–2.4). The above biomarker associations were attenuated after adjustment for maternal preeclampsia, fetal growth restriction and related neonatal characteristics, and when taking into account placental vascular pathologies. Longitudinal growth patterns by mean weight and length percentiles were consistently lower among infants with low VEGF/sFlt-1 ratios.
Conclusions
Our data support that intrauterine regulation of angiogenesis is an important mechanism of fetal and postnatal growth. Cord blood VEGF and sFlt-1 are useful in elucidating how intrauterine processes may have long-standing effects on developing premature infants.
Keywords: Birth weight, cord blood, postnatal growth, preterm infants, vascular endothelial growth factor (VEGF), fetal growth restriction, fetal origins
Introduction
Preterm infants are at considerable risk for postnatal growth failure (PGF), which has been defined as body weight < 10th percentile at 36 weeks corrected gestational age (GA) [1,2]. Preterm infants who are small-for-gestational age (SGA) at birth are at greatest risk for poor postnatal growth [3]. Failure to gain weight during the neonatal period may have a significant negative effect on both short- and long-term health. In SGA infants, the outcome of intellectual performance was found to be worse among those who do not catch-up in height, weight, and head circumference, compared to those with catch-up growth [4,5]. In addition, epidemiological studies have linked poor neonatal growth to obesity, insulin resistance, and cardiovascular disease [6,7].
Although fetal growth restriction and resultant SGA birth weight (< 10th percentile) is strongly associated with poor postnatal growth, even appropriate for GA (AGA) premature infants are at risk. The mechanisms for PGF are poorly understood, but angiogenesis, the formation of new blood vessels from preexisting ones, appears to be a critical process for intra- and extra-uterine growth [8]. Pro-angiogenic vascular endothelial growth factor (VEGF) and its soluble antagonist, fms-like tyrosine kinase 1 (sFlt-1), are promising biomarkers for understanding and predicting PGF, since they function as a regulatory system for angiogenesis. Excess sFlt-1 and decreased VEGF in the placenta, maternal serum, and umbilical cord blood may have a pathological role in preeclampsia, which is an important risk factor for fetal growth and perhaps early postnatal growth [9–14].
In this study, we evaluated the relationship between cord blood VEGF and sFlt-1, birth weight (BW), postnatal growth patterns and placental histopathology in preterm infants enrolled in an ongoing birth cohort study. We hypothesized that cord blood VEGF and sFlt-1 are associated with PGF, independent of BW status and other factors related to preterm birth. These findings will enhance our understanding of the pathophysiology of neonatal growth in preterm infants who are at risk for PGF.
Methods
Study Design and Patients
Study patients (mothers and their infants) were part of an ongoing longitudinal prospective cohort study being conducted at Northwestern Prentice Women’s Hospital in Chicago, IL. Inclusion criteria for this larger cohort are all infants live-born at < 37 weeks GA with available cord blood at delivery. Infants with a prenatal diagnosis of congenital anomalies or syndromes, or those for whom GA cannot be reliably assessed were excluded. For this present study, a subset of mother-infant pairs was selected from the larger cohort to include the following BW status groups among preterm infants: 1) ≤ 1000 g; 2) 1001–1500 g; 3) 1501–2000 g; 4) > 2000 g. Parental consent was obtained prior to enrollment. The study was approved by the institutional review board of Northwestern University.
Maternal and Infant Covariates
Maternal and infant clinical information were recorded using a standardized abstraction form that included data on prenatal care, intrapartum management, pregnancy complications and birth outcomes. Standardized definitions included the following: 1) GA was determined based on last normal menstrual period (LNMP) confirmed by ultrasounds or averaged ultrasound parameters obtained prior to 20 weeks gestation [15]. LNMP estimate was used whenever the estimated date of confinement correlated with first trimester ultrasound within 1 week or second trimester ultrasound within 2 weeks. Otherwise, ultrasound estimate was used. Only births that could be accurately dated by this algorithm were included in the study; 2) Maternal preeclampsia was defined according to American College of Obstetrics and Gynecology Committee criteria for clinical practice diagnosis that included gestational hypertension (new onset after 20 weeks’ gestation) with documented proteinuria, and included eclampsia and hemolysis, elevated liver enzymes, and low platelet count (HELLP) syndrome [16]; 3) Placental weight and histopathology information were recorded via standardized pathology review by the study’s perinatal pathologist. Placental vascular pathology included evidence of maternal or fetal vascular lesions according to the criteria by Redline, et al. [17,18]; 4) Neonatal complications were identified according to the widely used benchmarks: bronchopulmonary dysplasia (BPD) [19]; intraventricular hemorrhage (IVH) [20]; necrotizing enterocolitis (NEC) [21]; and diagnoses of retinopathy of prematurity (ROP) were obtained from NICU records for each infant.
Parameters of Growth
Longitudinal growth parameters of weight (g), length (cm), and head circumference (cm) were measured at birth and at weekly intervals up to hospital discharge. Continuous variable weight, length, and head circumference percentiles were determined using the most recent Fenton growth curves for premature infants [22]. Values were calculated using the formula provided by this reference, in which growth parameters were entered for the completed weeks of gestation for each infant. Postnatal growth failure (PGF) was defined as weight-for-corrected GA <10th percentile at 36 weeks or NICU discharge, whichever came first.
Cord Blood VEGF and sFlt-1
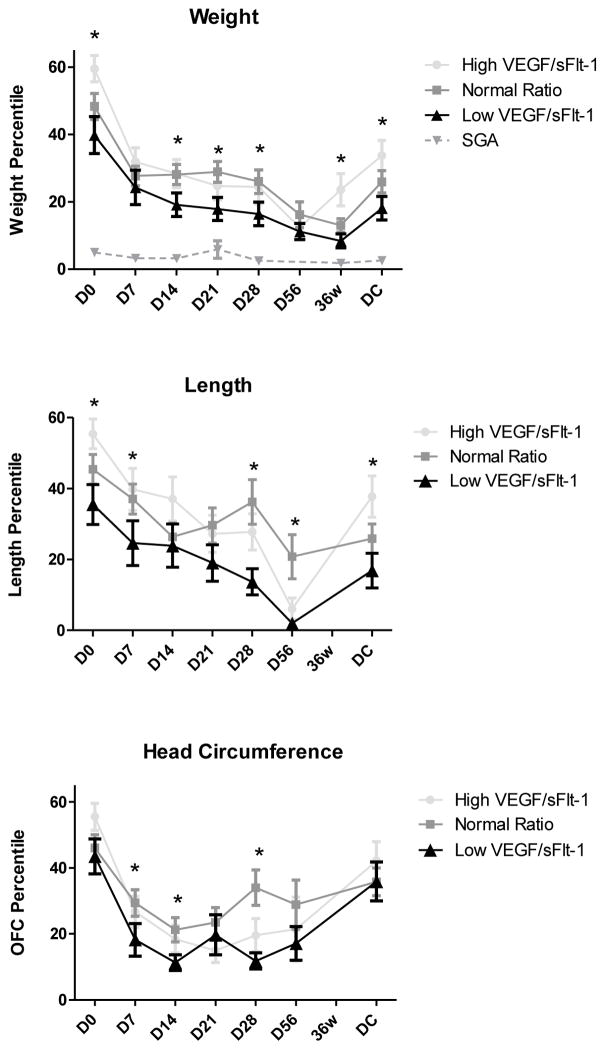
Mixed arterial-venous cord blood was collected at delivery into EDTA tubes, stored temporarily on ice, and spun at 2500 rpm for 10 minutes in a refrigerated tabletop centrifuge. Plasma was separated into aliquots and stored at −80°C until assay. Plasma VEGF and sFlt-1 were simultaneously measured in duplicate using commercially available EIA kits (R&D Systems, Minneapolis, MN). EIA results were read using a Bio-Rad iMark (Hercules, CA) automated plate reader at 450 nm with background correction at 540 nm. For VEGF, the limit of detection (LOD) was non-detectable, and intra- and interassay coefficients of variation (CV) were 6.7% and 8.8%, respectively. For sFlt-1, LOD was 1.5 pg/ml, and intra- and interassay CV were 3.8% and 9.8%, respectively. The ratio of VEGF to sFlt-1 level (VEGF/sFlt-1) for each patient was calculated to indicate relative amount of circulating VEGF to its soluble receptor [23]. For purposes of plotting longitudinal growth (Figure 1), low VEGF/sFlt-1 was defined as a ratio in the 1st quartile (< 0.03). High VEGF/sFlt-1 was defined as a ratio in the 4th quartile (> 0.5).
Figure 1.
Postnatal growth percentiles of weight, length, and head circumference (occipital-frontal circumference, OFC) according to cord blood VEGF/sFlt-1 ratio. Low VEGF/sFlt-1 (1st quartile), normal ratio VEGF/sFlt-1 (2nd–3rd quartile), and high VEGF/sFlt-1 (4th quartile) shown.
*P<0.05, low ratio vs. normal to high ratio percentile
Statistical Analysis
The chi-square or Fisher’s exact tests and Student’s t-tests were used to compare categorical and continuous variables, respectively. Continuous biomarker data were reported in pg/ml and median levels compared using non-parametric tests. Multivariate logistic regression models were constructed to evaluate the associations of log-transformed biomarkers on PGF, adjusting for relevant maternal and infant demographics and clinical covariates. P <0.05 was considered statistically significant with a power of 0.9 using 2-sided testing. All analyses were conducted using STATA software (StataCorp, College Station, TX).
Results
Study Patients
Clinical and biomarker data were studied on 123 mother-infant pairs enrolled in the cohort. As shown in Table 1, roughly one-half of the patients were identified as having PGF at 36 weeks or NICU discharge. As expected, BW and BW-for-GA percentiles were lower in the PGF group. In fact, all infants born SGA (BW < 10th percentile) had PGF. Infants with PGF were slightly more likely to be born from mothers with preeclampsia, be of multiple gestation, have retinopathy of prematurity and necrotizing enterocolitis, and a longer median length of hospitalization. PGF infants were also more likely to have evidence of maternal vascular pathology on placental histology.
Table 1.
Maternal and infant demographics and clinical characteristics
| PGF n=65 | No PGF n=58 | P value | |
|---|---|---|---|
|
| |||
| Gestational age, weeks (mean±sd) | 30.8±3.8 | 31.9±3.4 | 0.09 |
|
| |||
| Birth weight, grams | 1388.1±716.0 | 2016.1±541.4 | <0.001 |
|
| |||
| Birth weight for gestational age percentile | 31.1±23.4 | 68.9±18.5 | <0.001 |
|
| |||
| Male gender, n(%) | 36(49) | 38(51) | 0.25 |
|
| |||
| Multiple gestation | 29(45) | 17(30) | 0.08 |
|
| |||
| Apgar score, median (IQR) | |||
| 1-minute | 6 (3,8) | 7.5 (5,8) | 0.07 |
| 5-minute | 8 (7,9) | 8.5 (8,9) | 0.29 |
|
| |||
| Maternal age, years (mean ± sd) | 31.1±6.4 | 31.7±6.4 | 0.53 |
|
| |||
| Maternal race, n(%) | |||
| Black | 12(10) | 7(6) | |
| White | 30(24) | 34(28) | 0.35 |
| Other | 21(17) | 19(15) | |
|
| |||
| Chorioamnionitis | 4(44) | 5(56) | 0.60 |
|
| |||
| Vaginal delivery | 27(46) | 32(54) | 0.13 |
|
| |||
| Antenatal steroids | 25(53) | 22(47) | 0.95 |
|
| |||
| Preeclampsia | 24(67) | 12(33) | 0.05 |
|
| |||
| Maternal Diabetes | 6(50) | 6(50) | 0.84 |
|
| |||
| Placental characteristics:** | |||
|
| |||
| Placental weight, grams (mean±sd) | 395.1±228.5 | 423.3±181.4 | 0.51 |
|
| |||
| Maternal vascular pathology | 35(61) | 12 (30) | 0.004 |
|
| |||
| Fetal vascular pathology | 11(19) | 7(17) | 0.78 |
|
| |||
| Patent ductus arteriosus | 17(55) | 14(45) | 0.79 |
|
| |||
| Moderate-severe bronchopulmonary dysplasia | 17(26) | 9(16) | 0.14 |
|
| |||
| Necrotizing enterocolitis | 12(75) | 4(25) | 0.06 |
|
| |||
| Grade 3–4 IVH | 6(9) | 1(2) | 0.12 |
|
| |||
| Retinopathy of prematurity | 20(31) | 8(14) | 0.03 |
|
| |||
| SGA (<10% percentile) | 15(100) | 0(0) | <0.001 |
|
| |||
| Hospital stay, median days (IQR) | 44(16,89) | 26(5,50) | 0.02 |
|
| |||
| Daily caloric intake, kcal/kg/day (mean±se): | |||
|
| |||
| Day of life 7 | 89.8±3.3 | 92.7±2.0 | 0.24 |
|
| |||
| 14 | 104.4±3.1 | 107.3±2.2 | 0.24 |
|
| |||
| 21 | 110.0±3.3 | 113.3±2.6 | 0.22 |
|
| |||
| 28 | 108.7±3.4 | 112.7±3.9 | 0.22 |
|
| |||
| 56 | 114.0±4.8 | 111.4±4.3 | 0.63 |
|
| |||
| Protein intake, gm/kg/day: | |||
|
| |||
| Day of life 7 | 3.0±0.1 | 2.6±0.2 | 1.00 |
|
| |||
| 14 | 3.3±0.1 | 3.0±0.1 | 1.00 |
|
| |||
| 21 | 3.2±0.1 | 3.0±0.1 | 0.78 |
|
| |||
| 28 | 3.1±0.1 | 2.9±0.2 | 0.79 |
|
| |||
| 56 | 3.4±0.1 | 3.1±0.2 | 0.87 |
P-values calculated using student’s t-test for continuous variables and X2 for categorical variables.
Data available on 57 PGF and 41 non-PGF births.
Correlations between cord blood VEGF, sFlt-1, and birth weight
Table 2 shows median biomarker levels according to BW and BW percentile groups. VEGF levels did not differ significantly across the 4 BW groups (P-trend=0.88), but for sFlt-1 there was a significant trend towards decreasing levels with increasing BW (P-trend=0.01). For continuous BW percentile and its subgroups (< 25th, 25–49th, 50–74th, and ≥ 75th) there was a significant direct correlation with VEGF and an indirect correlation with sFlt-1 with increasing percentiles.
Table 2.
Correlations between cord blood VEGF and sFlt-1 with birth weight
| N | VEGF median(IQR) | P | sFlt-1 median(IQR) | P | |
|---|---|---|---|---|---|
| BW group: | |||||
| ≤1000g | 25 | 50.3 (35.8, 105.7) | 0.88 | 1000 (371.8, 1627.2) | 0.01 |
| 1001–1500g | 28 | 57.9 (39.3, 174.3) | 663.1 (333.6, 1283.7) | ||
| 1500–2000g | 34 | 54.2 (36.1, 149.0) | 632.4 (341.5, 1046.0) | ||
| >2000g | 36 | 85.0 (23.5, 272.5) | 399.0 (192.8, 940.5) | ||
| BW percentiles: | |||||
| <25th | 32 | 41.2 (29.3, 62.4) | 0.003 | 856.1 (419.8, 2123.9) | 0.01 |
| 25–49th | 24 | 48.4 (34.1, 89.8) | 879.4 (333.6, 1258.0) | ||
| 50–74th | 42 | 108.4 (39.6, 355.0) | 402.2 (260.9, 1072.0) | ||
| ≥75th | 25 | 58.0 (40.2, 344.5) | 530.5 (274.8, 724.2) | ||
P-trend calculated using Wilcoxon rank-sum non-parametric tests across ordered groups (nptrend).
Biomarker associations with longitudinal growth
Figure 1 shows the patterns of longitudinal growth according to percentiles for weight, length and head circumference among infants with low (1st quartile), normal range (2nd–3rd quartile), and high (4th quartile) VEGF/sFlt-1 ratios. Infants with low VEGF to sFlt-1 ratios had overall lower birth weight and length percentiles, and their growth persistently tracked along the lower growth percentiles for weight and length. These patterns persisted even when observations were limited to non-SGA infants and infants of more mature gestational age of > 28 weeks (data not shown). As compared with infants with normal to high ratios, infants with low ratios had largely negative change in weight and length percentiles, with means that fell below the 20th percentile by day 21, with little catch-up growth towards discharge.
Biomarker associations with postnatal growth failure (PGF)
As shown in Figure 1, weight and length percentiles were overall lower at NICU discharge among infants with low VEGF/sFlt-1 ratios. The associations between cord blood VEGF, sFlt-1 and PGF are shown in Table 3. Median VEGF was lower among infants with PGF as compared with infants without PGF. An inverse pattern was seen with sFlt-1. In the logistic regression models, the adjusted odds ratio for each biomarker (log-transformed) was determined using the absence of PGF as the reference group (Table 3). The associations remained significant after adjustment for maternal race/ethnicity, infant gender, multiple gestation and GA, but for sFlt-1 was attenuated after further adjustment for maternal preeclampsia and SGA birth weight. The association with VEGF was also not modified after adjustment for neonatal complications that might prolong hospitalization or lead to delayed growth in the neonatal period (e.g., bronchopulmonary dysplasia, necrotizing enterocolitis, intraventricular hemorrhage, and retinopathy of prematurity). Of note, the nutritional intake profiles during hospitalization (e.g., daily caloric and protein intakes) did not differ by PGF status (Table 1) or VEGF/sFlt-1 ratio (data not shown).
Table 3.
Biomarker levels across PGF status and logistic regression models for the association of cord blood VEGF and sFlt-1 on the development of PGF.
| Biomarker pg/ml median (IQR) | OR (95% CI) | ||||
|---|---|---|---|---|---|
| Non-PGF | PGF | Model 1 | Model 2 | Model 3 | |
| VEGF | 89.7 (37.8, 221.9) | 49.0 (32.3, 104.3) | 0.7 (0.5, 0.9)* | 0.6 (0.4, 0.9)* | 0.6 (0.4, 0.9)* |
| sFlt-1 | 451.3 (269.1, 862.0) | 798.7 (327.5, 1384.1) | 1.6 (1.1, 2.4)* | 1.3 (0.8, 2.1) | 1.4 (0.8, 2.2) |
| Stratified by placental vascular pathology (none versus any)** | |||||
| VEGF | |||||
| No vascular pathology | 64.9 (34.9, 349.3) | 58.6 (29.3, 214.0) | 0.8 (0.5, 1.4) | ||
| Any vascular pathology | 95.4 (58.0, 175.8) | 48.5 ** (35.8, 87.1) | 0.5 (0.3, 1.1) | ||
| sFlt-1 | |||||
| No vascular pathology | 398.6 (205.2, 738.8) | 515.0 (296.0, 809.9) | 1.3 (0.6, 2.8) | ||
| Any vascular pathology | 615.0 (330.9, 1121) | 1028 (417.9, 1829.3) | 1.5 (0.8, 2.7) | ||
P<0.05. Odds ratios (OR) and 95% confidence intervals (CI) calculated using logistic regression. Model 1: adjusted for maternal race, infant gender, multiple gestation, and gestational age at birth. Model 2: further adjusted for maternal preeclampsia and small-for-gestational age birth weight (<10th percentile). Model 3: further adjusted for bronchopulmonary dysplasia, necrotizing enterocolitis, intraventricular hemorrhage, and retinopathy of prematurity.
Stratified models adjusted according to Model 1, and include patients with complete placental histopathology data (N=98). P<0.05 for PGF vs. Non-PGF among infants with placental vascular pathology.
The role of placental vascular disease
Placental vascular pathologies (maternal or fetal) were more prominent with PGF (Table 1) and elevated with sFlt-1 (P=.001), but not associated with VEGF (P=0.62). Since cord blood levels could reflect not only fetal but also placental growth and angiogenesis, we investigated how the presence of placental vascular lesions might affect the biomarker-PGF associations. Stratification of the logistic regression models by the presence versus absence of any vascular pathology resulted in modifications within each strata such that the biomarker associations were no longer significant (Table 3). However, median VEGF was significantly lower in PGF infants with placental vascular disease. Among infants with both low VEGF/sFlt-1 ratio and placental vascular disease, 30 out of 39 had PGF (78%). When considered together, the presence of either a low VEGF/sFlt-1 ratio or any placental vascular lesion identified 49 of 56 cases of PGF (88%).
Discussion
In this cohort of preterm infants of a wide gestational age range, cord blood VEGF increases with BW and BW-for-GA percentile, while its soluble receptor, sFlt-1 is decreased disproportionately but consistently at birth. In addition, infants with relatively low circulating VEGF to sFlt-1 at birth continue to have delayed growth postnatally. Lastly, we found that infants with low VEGF and elevated sFlt-1 were more likely to have PGF at 36 weeks corrected GA or discharge. These biomarker associations are influenced by factors associated with placental dysfunction, such as maternal preeclampsia and fetal growth restriction. These findings have important implications for our understanding of the role of vascular endothelial growth factors in fetal and neonatal growth in the premature infant.
To our knowledge, this is the first study to comprehensively examine the relationship between cord blood VEGF, sFlt-1 and BW status in a large sample of preterm infants followed for their growth outcomes. Our findings support previous studies that report a strong correlation between cord blood VEGF and fetal growth restriction [24,25]. Our finding that VEGF increases and sFlt-1 decreases with advancing BW and GA is consistent with previous reports [26,27].
Elevated maternal sFlt-1 has been shown to be a predictor of adverse pregnancy outcomes related to preeclampsia. Coupled with low placental growth factor (PIGF), elevated sFlt-1 is a marker of abnormal placental vascular development leading to chronic fetal hypoxia [27]. This “angiogenic imbalance” also appears to be related to intrauterine inflammation, which we have previously described in association with PGF [28]. Whether inflammatory processes potentiate abnormal angiogenesis or vice versa remains to be determined. Regardless, these studies provide ongoing evidence of the potential role of early fetal programming that may impact postnatal growth and subsequent early childhood development.
Fetal and neonatal levels of VEGF are perhaps better described than sFlt-1, although, the impact of VEGF on the developing infant remains unclear. Investigators of the Extremely Low Gestational Age Newborns (ELGAN) study group have shown that VEGF and its receptors are increased during the first postnatal weeks of life in extremely low GA infants [29], and that low levels may be associated with the development of neonatal lung disease [30]. In animal studies, the development and maintenance of adiposity is dependent upon angiogenesis, and VEGF and its receptors have been shown to play an important role [31]. Therefore, we speculate that infants with low circulating VEGF at birth may suffer delayed postnatal growth due to their lack of capacity for normal adiposity essential for weight gain and linear growth. In a recent study by Olmos and colleagues, cord blood VEGF and sFlt-1 along with insulin-like growth factor I (IGF-1), an important factor for somatic growth, were associated with preeclampsia [14]. Further evaluation of human umbilical vein endothelial cells in this study suggested that aberrant IGF-1 stimulation of sFlt-1 accompanies preeclampsia. Therefore, IGF-1 may play an important role in the development of PGF and this interaction warrants further investigation.
In our patient sample, we found that although BW and low BW percentile remain the most important predictors of PGF, infants who are not growth-restricted at birth may suffer from poor postnatal growth. Such infants with low VEGF to sFlt-1 ratios were found to be at risk (Figure 1), and at NICU discharge had significantly lower growth percentiles despite optimal nutrition in the NICU. We took into consideration several covariates that might modify the growth associations with VEGF and sFlt-1. After adjustment for maternal preeclampsia and SGA status, two central risk factors shown to accompany low cord blood VEGF, the association between VEGF and PGF remained significant. Similar patterns were seen when taking into account GA and factors associated with prematurity that might negatively impact postnatal growth.
Cord blood VEGF and sFlt-1 were also indicators of placental dysfunction. In stratified analyses, placental vascular pathology appeared to be an important modifier between VEGF, sFlt-1, and PGF. Neither cord blood nor placental markers appeared to act independently on PGF. However, infants with abnormalities in both cord blood VEGF/sFlt-1 and placental vascular histology were more likely to have PGF than either marker alone. While it is possible that growth factors are up-regulated by placental dysfunction [32], further studies are needed to understand this complex interplay and whether these factors are responsible for fetal growth, or merely markers of intrauterine pathology leading to growth problems.
There are advantages and disadvantages to use a wide GA range. We were able to characterize the patterns of VEGF and sFlt-1 along the spectrum of GA and BW, both categorically and continuously, which has not been previously described. It is possible that the findings with PGF could be confounded by lower GA and BW. We took these factors into consideration by adjustment and restriction of observations to non-SGA and > 28 week infants, and found that the associations with longitudinal growth and PGF remained unchanged. Other limitations of this study include that the relatively small sample size did not allow us to test for potentially important interactions with preeclampsia and fetal growth restriction, and to investigate other closely related markers and their longitudinal trends. Further evaluation is warranted in a larger sample to address these next questions. Lastly, the single center study limits generalizability but allowed us to follow a homogeneous cohort of NICU patients with respect to their nutritional management.
In conclusion, our findings demonstrate the associations of cord blood VEGF and sFlt-1 on fetal growth and subsequent postnatal growth in the premature infant. These biomarkers are useful in understanding how intrauterine processes have long-standing effect on the premature infant. Poor postnatal growth during a critical period of development can lead to adult diseases including obesity, insulin resistance, and cardiovascular disease. Therefore, our findings have important clinical and public health implications. Further studies are needed, but it is possible that consideration of these promising biomarkers may help guide nutritional NICU management and prevent future morbidity.
Acknowledgments
Financial support: This project was supported by NIH HL109478 (PI: Farrow), the Northwestern Memorial Foundation Friends of Prentice Grant and NIH K23 HL093302 (PI: Mestan).
Footnotes
Conflict of interest statement:
The authors have no conflict of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lemons JA, Bauer CR, Oh W, Korones SB, Papile L, Stoll BJ, et al. Very low birth weight outcomes of the National Institute of Child Health and Human Development Neonatal Research Network, January 1995 through December 1996. Pediatrics. 2001;107(1) doi: 10.1542/peds.107.1.e1. Available at: www.pediatrics.org/cgi/content/full/107/1/e1. [DOI] [PubMed] [Google Scholar]
- 2.Ehrenkranz RA, Younes N, Lemons JA, Fanaroff AA, Donovan EF, Wright LL, et al. Longitudinal growth of hospitalized very low birth weight infants. Pediatrics. 1999;104(2):280–289. doi: 10.1542/peds.104.2.280. [DOI] [PubMed] [Google Scholar]
- 3.Kamoji VM, Dorling JS, Manktelow BN, Draper ES, Field DJ. Extremely growth-retarded infants: is there a viability centile? Pediatrics. 2006;118:758–763. doi: 10.1542/peds.2005-2399. [DOI] [PubMed] [Google Scholar]
- 4.Lundgren EM, Cnattingius S, Jonsson B, Tuvemo T, et al. Intellectual and psychological performance in males born small for gestational age with and without catch-up growth. Pediatr Res. 2001;50:91–96. doi: 10.1203/00006450-200107000-00017. [DOI] [PubMed] [Google Scholar]
- 5.Leviton A, Fichorova RN, O’Shea M, Kuban K, Paneth N, Dammann O, Allred E. Two-hit model of brain damage in the very preterm newborn: small for gestational age and postnatal systemic inflammation. Pediatric Research. 2013;73(3):362–370. doi: 10.1038/pr.2012.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lal MK, Manktelow BN, Draper ES, Field DJ. Chronic lung disease of prematurity and intrauterine growth retardation: a population-based study. Pediatrics. 2003;111:483–487. doi: 10.1542/peds.111.3.483. [DOI] [PubMed] [Google Scholar]
- 7.Thureen PJ. The neonatologist’s dilemma: catch-up growth or beneficial undernutrition in very low birth weight infants: what are optimal growth rates? J Pediatr Gastroenterol Nutr. 2008;45(suppl 3):152–154. doi: 10.1097/01.mpg.0000302962.08794.62. [DOI] [PubMed] [Google Scholar]
- 8.Liekens S, DeClercq E, Neyts J. Angiogenesis: regulators and clinical applications. Biochemical Pharmacology. 2001;61:253–70. doi: 10.1016/s0006-2952(00)00529-3. [DOI] [PubMed] [Google Scholar]
- 9.Ahmad S, Ahmad A. Elevated placental soluble vascular endothelial growth factor receptor-1 inhibits angiogenesis in preeclampsia. Circ Res. 2004;95:884–891. doi: 10.1161/01.RES.0000147365.86159.f5. [DOI] [PubMed] [Google Scholar]
- 10.Levine RJ, Maynard SE, Qian C, Lim KH, England LJ, Yu KF, et al. Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med. 2003;350:672–683. doi: 10.1056/NEJMoa031884. [DOI] [PubMed] [Google Scholar]
- 11.Thadhani R, Mutter WP, Wolf M, Levine RJ, Taylor RN, Sukhatme VP, et al. First trimester placental growth factor and soluble fms-like tyrosine kinase 1 and risk for preeclampsia. J Clin Endocrinol Metab. 2004;89:770–775. doi: 10.1210/jc.2003-031244. [DOI] [PubMed] [Google Scholar]
- 12.Lyall F, Greer IA, Boswell F, Fleming R. Suppression of serum vascular endothelial growth factor immunoreactivity in normal pregnancy and in pre-eclampsia. Br J Obstet Gynaecol. 1997;104:223–228. doi: 10.1111/j.1471-0528.1997.tb11050.x. [DOI] [PubMed] [Google Scholar]
- 13.Polliotti BM, Fry AG, Saller DN, Mooney RA, Cox C, Miller RK. Second-trimester maternal serum placental growth factor and vascular endothelial growth factor for predicting severe, early-onset preeclampsia. Obstet Gynecol. 2003;101:1266–1274. doi: 10.1016/s0029-7844(03)00338-7. [DOI] [PubMed] [Google Scholar]
- 14.Olmos A, Diaz L, Avila E, Barrera D, Lopez-Marure R, Biruete B, Larrea F, Halhali A. Associations between insulin-like growth factor I, vascular endothelial growth factor and its soluble receptor 1 in umbilical serum and endothelial cells obtained from normotensive and preeclamptic pregnancies. Growth Factors. 2013;31(4):123–29. doi: 10.3109/08977194.2013.802692. [DOI] [PubMed] [Google Scholar]
- 15.American College of Obstetrics and Gynecologists. ACOG Practice Bulletin No 101: ultrasonography in pregnancy. Obstet Gynecol. 2009;113(2 pt 1):451–461. doi: 10.1097/AOG.0b013e31819930b0. [DOI] [PubMed] [Google Scholar]
- 16.ACOG Committee on Obstetric Practice ACOG practice bulletin. Diagnosis and management of preeclampsia and eclampsia. Number 33, January 2002. American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet. 2002;77(1):67–75. [PubMed] [Google Scholar]
- 17.Redline RW, Boyd T, Campbell V, Hyde S, Kaplan C, Khong TY, Prashner HR, Waters BL Society for Pediatric Pathology, Perinatal Section, Maternal Vascular Perfusion Nosology Committee. Maternal vascular underperfusion: nosology and reproducibility of placental reaction patterns. Pediatr Dev Pathol. 2004;7(3):237–49. doi: 10.1007/s10024-003-8083-2. [DOI] [PubMed] [Google Scholar]
- 18.Redline RW, Ariel I, Baergen RN, Desa DJ, Kraus FT, Roberts DJ, Sander CM. Fetal vascular obstructive lesions: noslogy and reproducibility of placental reaction patterns. Peduatr Dev Pathol. 2004;7(5):443–52. doi: 10.1007/s10024-004-2020-x. [DOI] [PubMed] [Google Scholar]
- 19.Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005;116(6):1353–1360. doi: 10.1542/peds.2005-0249. [DOI] [PubMed] [Google Scholar]
- 20.Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1500 gm. J Pediatr. 1978;92(4):529–534. doi: 10.1016/s0022-3476(78)80282-0. [DOI] [PubMed] [Google Scholar]
- 21.Walsh MC, Kliegman RM. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am. 1986;33(1):179–201. doi: 10.1016/S0031-3955(16)34975-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fenton TR. Anew growth chart for preterm babies: Babson and Benda’s chart updated with recent data and a new format. BMC Pediatr. 2003;3:13. doi: 10.1186/1471-2431-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Toi M, Bando H, Ogawa T, Muta M, Hornig C, Weich HA. Significance of vascular endothelial growth factor (VEGF)/soluble VEGF receptor-1 relationship in breast cancer. Int J Cancer. 2002;98(1):14–18. doi: 10.1002/ijc.10121. [DOI] [PubMed] [Google Scholar]
- 24.Boutsikou T, Malamitsi-Puchner A, Economou E, Boutskiou M, Puchner K-P, Hassiakos D. Soluble vascular endothelial growth factor receptor-1 in intrauterine growth restricted fetuses and neonates. Early Human Development. 2006;82:235–239. doi: 10.1016/j.earlhumdev.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 25.Wallner W, Sengenberger R, Strick R, Strissel RL, Meurer B, Beckmann MW, Schlembach D. Angiogenic growth factors in maternal and fetal serum in pregnancies complicated by intrauterine growth restriction. Clinical Science. 2007;112:51–57. doi: 10.1042/CS20060161. [DOI] [PubMed] [Google Scholar]
- 26.Tsao PN, Wei SC, Su YN, Chou HC, Chen CY, Hsieh WS. Excess soluble fms-like trosine kinase 1 and low platelet counts in premature neonates of preeclamptic mothers. Pediatrics. 2005;116:468–72. doi: 10.1542/peds.2004-2240. [DOI] [PubMed] [Google Scholar]
- 27.Rana S, Hacker MR, Modest AM, Salahuddin S, Lim KH, Verlohren S, et al. Circulating angiogenic factors and risk of adverse maternal and perinatal outcomes in twin pregnancies with suspected preeclampsia. Hypertension. 2012;60(2):451–458. doi: 10.1161/HYPERTENSIONAHA.112.195065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mestan K, Yu Y, Matoba N, Cerda S, Demmin B, Pearson C, Ortiz K, Wang X. Placental inflammatory response is associated with poor neonatal growth: preterm birth cohort study. Pediatrics. 2010;125(4):e891–898. doi: 10.1542/peds.2009-0313. [DOI] [PubMed] [Google Scholar]
- 29.Leviton A, Allred EN, Yamamoto H, Fichorova RN. Relationships among the concentrations of 25 inflammation-associated proteins during the first postnatal weeks in the blood of infants born before the 28th week of gestation. Cytokine. 2012;57(1):182–90. doi: 10.1016/j.cyto.2011.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Laughon M, Bose C, Allred EN, O’Shea TM, Ehrenkranz RA, Van Marter LJ, et al. Patterns of blood protein concentrations of ELGANs classified by three patterns of respiratory disease in the first 2 postnatal weeks. Pediatr Res. 2011;70(3):292–6. doi: 10.1203/PDR.0b013e3182274f35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lijnen RH, Scroyen I. Effect of Vascular Endothelial Growth Factor-Receptor 2 antagonism on adiposity in obese mice. J Mol Endocrinol. 2013;50(3):319–24. doi: 10.1530/JME-12-0244. [DOI] [PubMed] [Google Scholar]
- 32.Semczuk M, Borczynska A, Bialas M, Rozwadowska N, Semczuk-Sikora A, Malcher A, Kurpisz M. Expression of genes coding for proangiogenic factors and their receptors in human placenta and intrauterine growth restriction. Reprod Biol. 2013;13(2):133–8. doi: 10.1016/j.repbio.2013.03.004. [DOI] [PubMed] [Google Scholar]