Abstract
Myelolipomas are rare tumors consisting of both adipose and hematopoietic tissue and are typically found within the adrenal gland. Extra-adrenal involvement is rare, especially those tumors involving the perirenal space and collecting system. We report a case of a patient with an incidentally discovered perirenal mass that was initially concerning for a retroperitoneal liposarcoma. Following surgical resection and pathological analysis, the lesion was found to be an extra-adrenal myelolipoma. This case report and review of the literature demonstrates the importance of the proper work-up and management of perirenal lipoma variants while addressing the issues of tissue biopsy, surgical intervention, and pre- and post-operative surveillance.
Keywords: Myelolipoma, Lipoma, Perirenal mass, Nephrectomy, Oncology
Core tip: We report a case of a patient with an incidentally discovered perirenal mass that was initially concerning for a retroperitoneal liposarcoma. Following surgical resection and pathological analysis, the lesion was found to be an extra-adrenal myelolipoma. This case report and review of the literature demonstrates the importance of the proper work-up and management of perirenal lipoma variants while addressing the issues of tissue biopsy, surgical intervention, and pre- and post-operative surveillance.
INTRODUCTION
Myelolipomas are mesenchymal tumors which consist of a mixture of mature adipose tissue with hematopoietic cells. This intriguing tumor most commonly occurs within the adrenal gland; however, it has been occasionally found within the pelvis, thorax, retroperitoneal space, and various other sites throughout the body[1-7]. There have been less than 60 reported cases of extra-adrenal myelolipomas to this date, with the majority of the literature describing neoplasms found within the pre-sacral space[2,8-10]. Perirenal extra-adrenal myelolipomas are especially rare, with only 9 cases previously reported[11]. We present a case of a patient with an incidentally discovered perirenal mass which, after having shown interval growth on longitudinal surveillance imaging studies, was surgically resected along with a left nephrectomy for presumed retroperitoneal liposarcoma. On final pathological analysis the lesion was found to be an extra-adrenal myelolipoma.
CASE REPORT
A 78-year-old gentleman presented to the surgical oncology clinic to be evaluated for a left-sided retroperitoneal mass that was incidentally discovered on a computed tomography (CT) scan for a suspected case of acute pancreatitis. His prior medical history included hypertension, hyperlipidemia, acalculous cholecystitis, atrial fibrillation, and coronary artery disease. Initial radiographic findings revealed a non-enhancing heterogeneous mass measuring approximately 3.8 cm × 2.3 cm in longitudinal and anterior-posterior (AP) dimensions, just inferior to the left renal vein and medial to the left kidney (Figure 1). As the lesion appeared to contain mostly adipose with a small amount of soft tissue density, a well differentiated liposarcoma was suspected. The patient was initially offered surgical resection of the lesion, which he refused. Given the small size of the mass and patient’s age and health status, the decision was made to closely monitor the lesion with routine cross-sectional surveillance imaging and regular follow-up at 4 to 6 mo.
Figure 1.
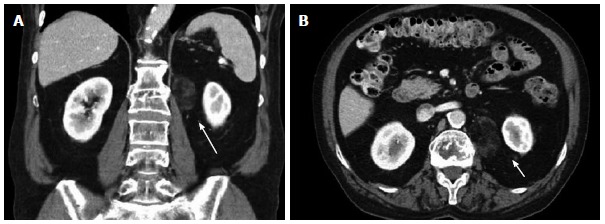
Initial computed tomography scan. Shows incidentally found non-enhancing heterogeneous mass measuring approximately 3.8 cm × 2.3 cm in longitudinal (A) and anterior-posterior dimensions (B), just inferior to the left renal vein (long arrow) and medial to the left kidney (arrow).
Throughout the surveillance period, the patient did not complain of any new symptoms. Physical examination repeatedly revealed a soft, non-tender abdomen with no palpable masses or hernias. Repeat cross-sectional imaging studies, however, did reveal a slowly enlarging left-sided heterogeneous perirenal mass. A magnetic resonance imaging (MRI) obtained 17 mo after initial diagnosis showed that the mass had increased in size to 5.0 cm × 3.4 cm (Figure 2). Four months prior the tumor had remained unchanged. The concern for a progressing malignant lesion prompted the decision to proceed with surgical intervention. Due to its proximity to the renal vessels, as well as the fact that the preoperative diagnosis was liposarcoma, the mass was excised en bloc with the left kidney in an attempt to gain wide surgical margins. The patient tolerated the procedure well and his post-operative course was uneventful. He was discharged home in stable condition on the ninth day following the procedure.
Figure 2.
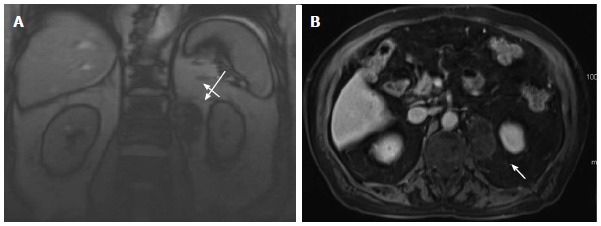
Surveillance magnetic resonance imaging. Imaging obtained 17 mo after the initial diagnostic computed tomography scan shows that the mass, located just inferior to the left renal vein (long arrow) and medial to the left kidney (arrow), increased in size to 5.0 cm × 3.4 cm in longitudinal (A) and anterior-posterior dimensions (B).
Gross pathology revealed an encapsulated, well-defined, focally hemorrhagic mass measuring 7.2 cm × 4.1 cm × 3.3 cm in size. The tumor did not extend into the renal capsule or adrenal gland. Histology revealed that the mass was composed of mostly mature adipocytes mixed with islands of hematopoietic cells. Trilineage hematopoiesis was present, including nucleated red blood cells and megakaryocytes (Figure 3). Tumor resection margins were free. The above mentioned morphological features were consistent with the diagnosis of “perirenal (extra-adrenal) myelolipoma”.
Figure 3.
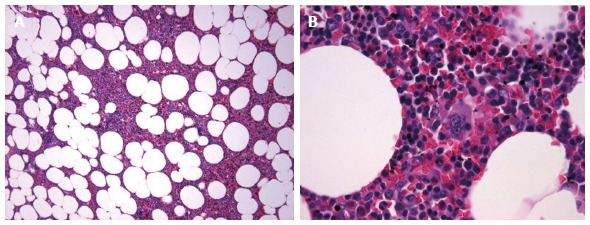
Hematoxylin and eosin stain at 10 × (A) and 60 × (B) magnification. Shows mature adipose cells with hematopoietic cells including erythroid precursors, granulocytic precursors, and megakaryocytes.
DISCUSSION
Myelolipoma is a unique mesenchymal tumor that is composed of a mixture of adipose and hematopoietic cells. The first case of an adrenal lesion containing both fat and myeloid elements was described by Gierke[12] in 1905. The reported incidence of myelolipoma on autopsy ranges from 0.08% to 0.4%[13]. This type of tumor is most commonly localized to the adrenal gland; however, there are rare but well-documented cases of extra-adrenal involvement[1]. To our knowledge, less than 60 cases of extra-adrenal myelolipomas have been reported[2,8-10], most of them involving the pre-sacral space. Tumors involving the mediastinum, lung, spleen, mandible, and nasal cavity have also been described[2-7]. Perirenal extra-adrenal myelolipomas are especially rare, with only 9 cases described so far[11].
A review of the literature shows that extra-adrenal myelolipomas exhibit a slight female predominance and are typically discovered between the ages of 50 to 70 years old[4,7,11]. Most tumors are unilateral and have been found to range from 2 to 26 cm in size at the time of diagnosis[14,15]. The etiology of extra-adrenal myelolipomas is still to be established. Several theories exist regarding their embryologic origin and pathogenesis. Amin et al[16] suggest that there may be a relationship between the re-activation of primitive peritoneal foci of extramedullary hematopoiesis under pathological stresses (i.e., severe anemia, sepsis, myeloproliferative disease) and the origin and progression of extra-adrenal myelolipomas. Another theory postulates that myelolipomas originate from metaplasia of previously uncommitted adrenal cortical mesenchymal cells or hematopoietic stem cells that normally migrate to the adrenal gland during intrauterine development[16].
The widespread application of modern imaging techniques has led to a dramatic increase in the detection of extra-adrenal myelolipomas. The majority of patients are asymptomatic at the time of diagnosis, and lesions are discovered incidentally on imaging for alternative medical problems. Typically, physical examination and routine blood tests fail to yield any conclusive diagnostic findings. Depending on the size and location of the lesion, some patients may present with vague flank or abdominal pain due to hemorrhage, mechanical compression, or tumor infarction[17]. CT and MRI have been used to diagnose extra-adrenal myelolipomas. When a myelolipoma is contained within the adrenal gland, the diagnosis is straightforward because it is the only known entity composed of adipose tissue occurring in this location[18]. A fatty mass within the retroperitoneal space represents a diagnostic challenge because the differential diagnosis includes an angiomyolipoma, a retroperitoneal teratoma, or a well-differentiated liposarcoma. A study that reviewed the MRI results of 126 consecutively imaged grossly fatty masses found that the sensitivity of MRI in diagnosing well-differentiated liposarcomas is 100%; however, its specificity is merely 83% due to the inability to differentiate between liposarcomas and other lipoma variants[19].
Fine needle biopsy under ultrasound or CT guidance may be useful for the diagnosis of extra-adrenal myelolipoma. Well-differentiated liposarcoma differs from myelolipoma in that the former contains atypical stromal cells, variable-sized adipocytes, some of them with nuclear atypia, and lipoblast which, however, are not diagnostic, being absent in some cases. By contrast, extra-adrenal myelolipomas are composed of mature adipocytes with scattered hematopoietic cells, including megakaryocytes[20]. Although these histological differences between the two tumors, in many cases the final diagnosis is difficult, if not impossible, based on tissue biopsy[11]. Furthermore, the risks of hemorrhage, rupture, or infection that are associated with biopsy must factor into a clinician’s decision to proceed with this invasive diagnostic procedure[11]. In our patient, tissue biopsy was deferred due to the patient’s preference to forego the procedure.
There is currently no standard treatment for patients with this disease. Daneshmand et al[21] suggest that small asymptomatic tumors (< 4 cm) should be monitored with routine cross-sectional surveillance imaging, while large symptomatic tumors (> 7 cm) should be surgically removed. Extra-adrenal myelolipomas have been removed using a thoracoabdominal incision, but recently a laparoscopic approach has proven to be just as effective[10]. Early detection and proper management of myelolipomas is important due to the potential for tumor growth and hemorrhage. A study of 86 myelolipomas found that hemorrhage is more common in larger lesions with a diameter measuring greater than 10 cm[22].
A review of 9 reported cases perirenal extra-adrenal myelolipomas, shows that the average age at diagnosis is 62 years of age (Table 1). Perirenal lesions exhibited a male-to-female ratio of 7:2. At the time of diagnosis, patients were either asymptomatic or complained of various symptoms including flank pain, dysuria, frequency, urgency, weight loss, hematuria, or abdominal distention. CT and ultrasound were the imaging modalities used to characterize the masses. Biopsy was used in only 2 of the 9 cases prior to surgical intervention. The average size on imaging is 8.7 cm × 7.4 cm, while the size of the resected masses on gross pathological evaluation is 11.8 cm × 8.0 cm × 5.9 cm. Treatment included open and laparoscopic mass excision with or without nephrectomy or partial nephrectomy depending on concern for adequate surgical margins. Upon reviewing the literature, we felt it was reasonable to monitor the lesion with routine surveillance imaging until the tumor increased in size and to perform a mass resection with a nephrectomy to ensure adequate surgical margins.
Table 1.
Review of reported cases of perirenal extra-adrenal myelolipomas
| Age at time of diagnosis (yr) | Sex | Presentation | Diagnostic imaging | Biopsy | Gross pathology | Treatment |
| 45 | Male | Asymptomatic | CT (5 cm × 5 cm) | No | 6.0 cm × 3.5 cm × 2.5 cm | Partial nephrectomy |
| 45 | Female | Flank pain Dysuria Frequency Urgency | CT (10 cm × 7 cm) | Yes | 9.0 cm × 6.4 cm × 5.5 cm | Laparoscopic mass resection |
| 60 | Male | Abdominal pain | CT (4.2 cm × 3.7 cm) | No | Not reported | Radical nephrectomy |
| 63 | Male | Asymptomatic | CT (6.5 cm × 5.5 cm) | No | Not reported | Open mass resection |
| 65 | Male | Flank pain, Weight loss Hematuria | CT (5.5 cm × 4.5 cm) | No | 7.0 cm × 5.0 cm × 1.5 cm | Radical nephrectomy |
| 66 | Female | Abdominal distention | CT (20 cm × 20 cm) | No | 20 cm × 15 cm × 15 cm | Open mass resection |
| 67 | Male | Asymptomatic | CT (7 cm × 5 cm) | No | Not reported | Radical nephrectomy |
| 70 | Male | Flank pain Fever | Ultrasound (12 cm × 8.5 cm) | No | 17.0 cm × 10.0 cm × 5.0 cm | Open mass resection |
| 77 | Male | Abdominal distension Hypertension | CT (Bilateral fat-containing masses) | Yes | Not reported | Follow-up CT 3 mo showed no change |
CT: Computed tomography.
Since an extra-adrenal myelolipoma is such a rare entity, a retroperitoneal mass that has imaging characteristics of a well-differentiated liposarcoma should ultimately end up being approached and treated as such. However, this report demonstrates that extra-adrenal myelolipoma should be considered as part of the list of differential diagnoses. In cases in which surgical extirpation of an extra-adrenal myelolipoma is performed, there are no clear recommendations for post-operative surveillance. Our review did not reveal a case of local recurrence of a retroperitoneal myelolipoma, however, routine radiographic surveillance would certainly be helpful to detect potential locally recurrent disease.
In summary, perirenal extra-adrenal myelolipoma is extremely rare. This neoplasm is typically discovered incidentally on cross-sectional imaging and commonly thought to be a liposarcoma. It can be managed conservatively or surgically depending on the patient’s symptoms or level of concern for a malignant lesion. Early detection and proper management of myelolipomas are important due to the potential for tumor growth and hemorrhage.
COMMENTS
Case characteristics
This case features a left-sided retroperitoneal mass that was incidentally discovered on a computed tomography (CT) scan for a suspected case of acute pancreatitis.
Clinical diagnosis
Imaging revealed a non-enhancing heterogeneous mass measuring approximately 3.8 cm x 2.3 cm in longitudinal and anterior-posterior dimensions, just inferior to the left renal vein and medial to the left kidney, and histological evaluation revealed that the mass was composed of mostly mature adipocytes mixed with islands of hematopoietic cells.
Differential diagnosis
Differential diagnosis was most concerning for liposarcoma, lipoma, malignant fibrous histiocytoma, or a fibrosarcoma.
Laboratory diagnosis
Laboratory findings were non-contributory to arriving at the final diagnosis.
Imaging diagnosis
CT and MRI were used to initially detect and follow the progression of the mass.
Pathological diagnosis
Hematoxylin and eosin (H and E) stain at 10 x and 60 x magnification revealed mature adipose cells with hematopoietic cells including erythroid precursors, granulocytic precursors, and megakaryocytes.
Treatment
The mass was excised en bloc with the left kidney in an attempt to gain wide surgical margins.
Related reports
The list of references to this article contains several related reports to aid readers to further understand this topic.
Term explanation
Myelolipoma is a unique mesenchymal tumor that is composed of a mixture of adipose and hematopoietic cells.
Experiences and lessons
Perirenal extra-adrenal myelolipomas are neoplasms that are typically discovered incidentally on cross-sectional imaging, they can be managed conservatively or surgically depending on the patient’s symptoms or level of concern for a malignant lesion, and early detection and proper management of myelolipomas are critical due to the potential for tumor growth and hemorrhage.
Peer review
This study describes a lesion which is not a unique phenomenon. Nevertheless, it is well writen with a good review of the literature.
Footnotes
P- Reviewers: Fernandez-Pello S, Magro G, Tsamis D S- Editor: Ma YJ L- Editor: A E- Editor: Wu HL
References
- 1.Meaglia JP, Schmidt JD. Natural history of an adrenal myelolipoma. J Urol. 1992;147:1089–1090. doi: 10.1016/s0022-5347(17)37482-7. [DOI] [PubMed] [Google Scholar]
- 2.Baker KS, Lee D, Huang M, Gould ES. Presacral myelolipoma: a case report and review of imaging findings. J Radiol Case Rep. 2012;6:1–9. doi: 10.3941/jrcr.v6i6.1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Geng C, Liu N, Yang G, Qi M, Chen W. Primary mediastinal myelolipoma: A case report and review of the literature. Oncol Lett. 2013;5:862–864. doi: 10.3892/ol.2012.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang WT, Zhao SJ, Lin DM. Pulmonary-bronchus myelolipoma and review on extra-adrenal myelolipomas in Chinese literature. Chin Med J (Engl) 2012;125:3188–3190. [PubMed] [Google Scholar]
- 5.Cina SJ, Gordon BM, Curry NS. Ectopic adrenal myelolipoma presenting as a splenic mass. Arch Pathol Lab Med. 1995;119:561–563. [PubMed] [Google Scholar]
- 6.Chiarini L, Bertoldi C, Criscuolo M, Ferronato G. [Myelolipomatosis. A report of a case located in the mandible] Minerva Stomatol. 1992;41:165–172. [PubMed] [Google Scholar]
- 7.George SA, Manipadam MT, Thomas R. Primary myelolipoma presenting as a nasal cavity polyp: a case report and review of the literature. J Med Case Rep. 2012;6:127. doi: 10.1186/1752-1947-6-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bandurski R, Zaręba K, Kędra B. Rare case of multifocal (adrenal and extra - adrenal ) myelolipoma. Pol Przegl Chir. 2013;85:348–350. doi: 10.2478/pjs-2013-0052. [DOI] [PubMed] [Google Scholar]
- 9.Talwalkar SS, Shaheen SP. Extra-adrenal myelolipoma in the renal hilum: a case report and review of the literature. Arch Pathol Lab Med. 2006;130:1049–1052. doi: 10.5858/2006-130-1049-EMITRH. [DOI] [PubMed] [Google Scholar]
- 10.Beiko D, Roldan H, Sengupta SK, George RL. Laparoscopic excision of a large extra-adrenal perirenal myelolipoma. Can Urol Assoc J. 2010;4:E39–E41. doi: 10.5489/cuaj.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghaouti M, Znati K, Jahid A, Zouaidia F, Bernoussi Z, Mahassini N. Renal myelolipoma: a rare extra-adrenal tumor in a rare site: a case report and review of the literature. J Med Case Rep. 2013;7:92. doi: 10.1186/1752-1947-7-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gierke E. Unusual myeloid tissue in the adrenal gland. Beitr Pathol Anat. 1905:3: 11–25. [Google Scholar]
- 13.Doddi S, Singhal T, Leake T, Sinha P. Management of an incidentally found large adrenal myelolipoma: a case report. Cases J. 2009;2:8414. doi: 10.4076/1757-1626-2-8414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kammen BF, Elder DE, Fraker DL, Siegelman ES. Extraadrenal myelolipoma: MR imaging findings. AJR Am J Roentgenol. 1998;171:721–723. doi: 10.2214/ajr.171.3.9725304. [DOI] [PubMed] [Google Scholar]
- 15.Dan D, Bahadursingh S, Hariharan S, Ramjit C, Naraynsingh V, Maharaj R. Extra-adrenal perirenal myelolipoma. A case report and review of literature. G Chir. 2012;33:62–65. [PubMed] [Google Scholar]
- 16.Amin MB, Tickoo SK, Schultz D. Myelolipoma of the renal sinus. An unusual site for a rare extra- adrenal lesion. Arch Pathol Lab Med. 1999;123:631–634. doi: 10.5858/1999-123-0631-MOTRS. [DOI] [PubMed] [Google Scholar]
- 17.Olobatuyi FA, Maclennan GT. Myelolipoma. J Urol. 2006;176:1188. doi: 10.1016/j.juro.2006.06.095. [DOI] [PubMed] [Google Scholar]
- 18.Butori N, Guy F, Collin F, Benet C, Causeret S, Isambert N. Retroperitoneal extra-adrenal myelolipoma: appearance in CT and MRI. Diagn Interv Imaging. 2012;93:e204–e207. doi: 10.1016/j.diii.2011.12.010. [DOI] [PubMed] [Google Scholar]
- 19.Gaskin CM, Helms CA. Lipomas, lipoma variants, and well-differentiated liposarcomas (atypical lipomas): results of MRI evaluations of 126 consecutive fatty masses. AJR Am J Roentgenol. 2004;182:733–739. doi: 10.2214/ajr.182.3.1820733. [DOI] [PubMed] [Google Scholar]
- 20.Temizoz O, Genchellac H, Demir MK, Unlu E, Ozdemir H. Bilateral extra-adrenal perirenal myelolipomas: CT features. Br J Radiol. 2010;83:e198–e199. doi: 10.1259/bjr/28801968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Daneshmand S, Quek ML. Adrenal myelolipoma: diagnosis and management. Urol J. 2006;3:71–74. [PubMed] [Google Scholar]
- 22.Kenney PJ, Wagner BJ, Rao P, Heffess CS. Myelolipoma: CT and pathologic features. Radiology. 1998;208:87–95. doi: 10.1148/radiology.208.1.9646797. [DOI] [PubMed] [Google Scholar]
- 23.Wagner JR, Kleiner DE, Walther MM, Linehan WM. Perirenal myelolipoma. Urology. 1997;49:128–130. doi: 10.1016/S0090-4295(97)00368-3. [DOI] [PubMed] [Google Scholar]
- 24.Pascual García X, Bujons Tur A, Rodríguez Faba O, Gómez Ruiz JJ, Palou Redorta J, Villavicencio Mavrich H. Extraadrenal perirenal myelolipoma: report of a case and review of the literature. Actas Urol Esp. 2007;31:932–934. doi: 10.1016/s0210-4806(07)73751-8. [DOI] [PubMed] [Google Scholar]
- 25.Brietta LK, Watkins D. Giant extra-adrenal myelolipoma. Arch Pathol Lab Med. 1994;118:188–190. [PubMed] [Google Scholar]
- 26.Sneiders A, Zhang G, Gordon BE. Extra-adrenal perirenal myelolipoma. J Urol. 1993;150:1496–1497. doi: 10.1016/s0022-5347(17)35823-8. [DOI] [PubMed] [Google Scholar]
- 27.Kilinc N. Extra-adrenal myelolipoma: A case report and review of the literature. Pak J Med Sci. 2007;23:779–781. [Google Scholar]


