Abstract
Nasopharyngeal carcinoma is rare in western countries, accounting for less than 1% of all malignancies. Despite prognosis is satisfactory for newly diagnosed, non-metastatic disease, management of recurrent disease is challenging, with a survival expectancy of approximately 6 mo with the use of chemotherapy as the sole salvage treatment. We report a case of recurrent nasopharyngeal carcinoma treated with a combination of chemotherapy, radiotherapy and surgery in the context of a multidisciplinary approach. A durable complete response was achieved.
Keywords: Cetuximab, Nasopharyngeal carcinoma, Re-irradiation, Surgery of metastases, Undifferentiated
Core tip: Recurrent nasopharyngeal carcinoma requires multi-modality therapy based on radiotherapy, surgery and chemotherapy, with a careful evaluation of expected toxicity and patient's quality of life.
INTRODUCTION
Nasopharyngeal carcinoma (NPC) accounts for less than 1% of all malignancies and is rare in western countries[1]. NPC is usually poorly differentiated and is diagnosed in young patients. The prognosis of loco-regional disease is satisfactory, with a 5-year overall survival exceeding 80%. Radiation alone is employed for stage I-II disease, while for locally advanced NPC the combination of chemotherapy and radiotherapy is the standard approach[1]. The advent of new radiotherapy techniques, like intensity modulated radiotherapy (IMRT), has further improved prognosis of newly diagnosed NPC patients and contributed to allow re-irradiation of recurrent disease. On the other hand, management of recurrent/metastatic disease remains challenging for medical and radiation oncologists. In addition to cisplatin-based chemotherapy, which is the standard systemic treatment for NPC[2], cetuximab may be in patients with NPC and squamous histology according to guidelines. Importantly, in undifferentiated NPC, epithelial growth factor receptor is often overexpressed and k-RAS is never mutated, so cetuximab may provide benefit also in these patients[3]. We here report how multidisciplinary management coupled with recent advances in the field allowed us the obtain a durable complete response in a patient with relapsing undifferentiated nasopharyngeal carcinoma.
CASE REPORT
In September 2009, a 59-year-old male patient was referred to our office for undifferentiated nasopharyngeal carcinoma. Histological diagnosis was made on fiberoscopy-guided biopsy. A computed tomography (CT) scan showed a large lesion arising from the posterior wall of the nasopharynx and extending into the paranasal sinuses. The lesion infiltrated the clivus and the oropharynx, and bilateral laterocervical lymphnode metastases were detected. Magnetic resonance imaging (MRI) confirmed CT findings (clinical stage, T4N3M0, IVa AJCC).
A therapeutic strategy based on 3 cycles of neoadjuvant docetaxel, cisplatin and 5-fluorouracil followed by radiotherapy was pursed after written informed consent was obtained. Docetaxel and cisplatin were given at doses of 75 mg/m2 on day one and 5-Fluorouracil was administered at 750 mg/m2 daily via continuous infusion for four consecutive days every three weeks. In November 2009, CT scan (Figure 1) showed partial response according to RECIST criteria 1.1 (reduction greater than 50% in the sum of the longest diameters of target lesions). From December 2009 until February 2010, a combined cetuximab-RT treatment was delivered. Cetuximab was given at standard doses. A total dose of 70 Gy (2 Gy dose fractions) on clinical target volume was delivered via 3D conformational radiotherapy. Toxicity mainly consisted of grade 2 cutaneous rash and grade 2 xerostomia, and did not lead to treatment interruption. Forty-five days after completion of chemo-radiotherapy, a complete response was shown on CT scan (Figure 2) and on PET scan after 60 d.
Figure 1.
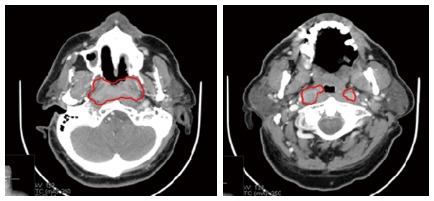
A large lesion arising from the posterior wall of the nasopharynx and bilateral lymphnode metastasis were detected in the parapharyngeal space (October 2009).
Figure 2.
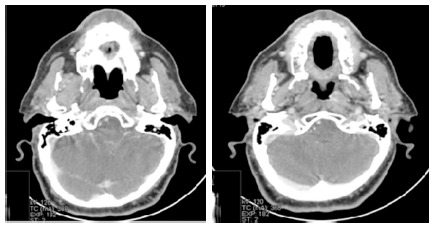
After neoadjuvant TPF followed by cetuximab-radiotherapy, a complete response was obtained (March 2010).
The patient remained free of disease recurrence until May 2012, when CT scan showed loco-regional recurrence involving the nasopharynx, the left orbitary cavity and intraparotid lymph nodes on the left side of the head. Patient presented with visual disturbances and moderate pain. PET scan and cytology confirmed the nature and extension of the recurrence. After multidisciplinary consultation involving the medical oncologist, the radiation oncologist, the pathologist and the surgeon, we decided to use a combined strategy based on an neoadjuvant chemotherapy, followed by re-irradiation and a surgical evaluation of residual disease.
Given the prolonged time to relapse, we deemed the disease to have preserved its sensitivity to taxanes and platinum compounds, so we delivered carboplatin (CBDCA) AUC 5 (area under curve) on day one every 3 wk, paclitaxel at the dose of 175 mg/m2 on day one every three weeks and standard doses of weekly cetuximab. Radiological and symptomatic improvement was obtained after three cycles. A CT scan showed disappearance of the nasopharyngeal lesion, shrinkage of the lymphnode mass but no change of the orbital lesion. Toxicity was low, with grade 1 skin rash the most relevant side effect. Re-irradiation was performed from the end of August to the beginning of October 2012 via helical IMRT, 18 FDG PET/CT based planning. A total dose of 66 Gy, delivered in 30 daily fractions of 2.2 Gy, were administered to the site of disease, with the exclusion of the lymphnode mass in the neck, with disappearance (Figure 3) of both the orbital lesion and the nasopharynx. After subsequent chemotherapy (three cycles of CBDCA-Pac and cetuximab) CT scan showed that the only site of persistent disease was the lymph node mass in the neck (Figure 4). Patient was scheduled for surgical removal of parothyd and laterocervical II, III and IV neck levels. In June 2013, CT scan showed no sign of residual disease. As of January 2014, the patient is free of disease. He complains of grade 2 chronic xerostomia due to radiotherapy, and a facial nerve paralysis due to the surgical intervention.
Figure 3.
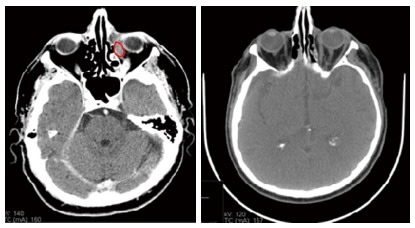
Computed tomography scan showed an intraorbital lesion (May 2012).
Figure 4.
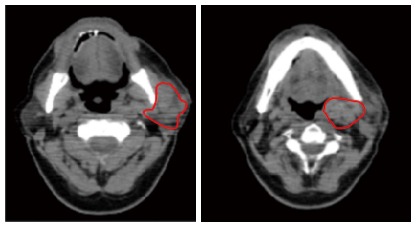
Computed tomography scan showed that the only site of persistent disease was the lymph node mass in the neck (December 2012).
DISCUSSION
Locally advanced nasopharyngeal carcinoma can be successfully managed by combination platinum-based chemotherapy and radiotherapy[4]. Neo-adjuvant chemotherapy is also a valuable option and is especially indicated in patients with large lesions and locally advance disease, in order to decrease the gross tumor volume[5]. Comibination of taxanes and platinum compounds is highly active, not only in nasopharyngeal carcinomas but also in other clinical situations, such as head-neck carcinomas of unknown primary[6].
On the other hand, current management of recurrent/metastatic disease is far from yielding satisfactory results, and the prognosis is grim. In addition to cisplatin-based chemotherapy, cetuximab may also be employed in patients with NPC, as shown in some preliminary experiences[7]. Our case appears of great interest not only because cetuximab appeared to improve the outcome at first presentation, but it appeared to have preserved its effectiveness at disease relapse. Cetuximab was well tolerated both at initial presentation and at recurrence. Randomized controlled trials are required to assess efficacy of cetuximab in nasopharyngeal carcinoma before it can be recommended in this setting.
Our case also highlights the importance of a multidisciplinary approach in all patients and especially in those with recurrent disease. The multidisciplinary approach is able to balance toxicity and efficacy associated to combined use of diversified treatments. In recurrent patients, the use of chemotherapy as the sole salvage treatment is associated to a 6-mo prognosis[8-10]. With a multidisciplinary approach, we obtained a complete response, and our patient is free of disease recurrence after more than 6 mo and has an acceptable quality of life. Doctor-doctor and patient-doctor communication was of utmost importance for the management of this case, which should set an example of optimal integrated strategy of recurrent nasopharyngeal carcinoma.
COMMENTS
Case characteristics
Patient presented with recurrent nasopharyngeal carcinoma treated with chemotherapy, biological therapy, radiation therapy and surgery.
Clinical diagnosis
Patient was affected by a locally advanced nasopharyngeal tumor, which was shown to be undifferentiated carcinoma on biopsy
Differential diagnosis
Differential diagnosis included lymphoma and squamous carcinoma.
Laboratory diagnosis
Patient had normal liver, bone marrow and kidney function at diagnosis and throughout treatment.
Imaging diagnosis
Patient had locally advanced disease at diagnosis, with a large lesion arising from the posterior wall of the nasopharynx and infiltrating the clivus and bilateral laterocervical lymphnode metastases.
Pathological diagnosis
Patient was affected by undifferentiated nasopharyngeal carcinoma.
Treatment
After patient underwent treatment with docetaxel, cisplatin and 5-Fluorouracil and combined cetuximab-radiotherapy, he was treated with carboplatin, paclitaxel and cetuximab, followed by re-irradiation and surgery.
Term explanation
Clinical target volume.
Experiences and lessons
Irradiation with cetuximab is advantageous when chemotherapy cannot be delivered.
Peer review
This paper is a useful clinical case in head and neck diseas.
Footnotes
P- Reviewers: Ao R, Li YZ S- Editor: Song XX L- Editor: A E- Editor: Wu HL
References
- 1.Caponigro F, Longo F, Ionna F, Perri F. Treatment approaches to nasopharyngeal carcinoma: a review. Anticancer Drugs. 2010;21:471–477. doi: 10.1097/CAD.0b013e328337160e. [DOI] [PubMed] [Google Scholar]
- 2.Boussen H, Cvitkovic E, Wendling JL, Azli N, Bachouchi M, Mahjoubi R, Kalifa C, Wibault P, Schwaab G, Armand JP. Chemotherapy of metastatic and/or recurrent undifferentiated nasopharyngeal carcinoma with cisplatin, bleomycin, and fluorouracil. J Clin Oncol. 1991;9:1675–1681. doi: 10.1200/JCO.1991.9.9.1675. [DOI] [PubMed] [Google Scholar]
- 3.Chan AT, Hsu MM, Goh BC, Hui EP, Liu TW, Millward MJ, Hong RL, Whang-Peng J, Ma BB, To KF, et al. Multicenter, phase II study of cetuximab in combination with carboplatin in patients with recurrent or metastatic nasopharyngeal carcinoma. J Clin Oncol. 2005;23:3568–3576. doi: 10.1200/JCO.2005.02.147. [DOI] [PubMed] [Google Scholar]
- 4.Ma J, Mai HQ, Hong MH, Min HQ, Mao ZD, Cui NJ, Lu TX, Mo HY. Results of a prospective randomized trial comparing neoadjuvant chemotherapy plus radiotherapy with radiotherapy alone in patients with locoregionally advanced nasopharyngeal carcinoma. J Clin Oncol. 2001;19:1350–1357. doi: 10.1200/JCO.2001.19.5.1350. [DOI] [PubMed] [Google Scholar]
- 5.Perri F, Bosso D, Buonerba C, Lorenzo GD, Scarpati GD. Locally advanced nasopharyngeal carcinoma: Current and emerging treatment strategies. World J Clin Oncol. 2011;2:377–383. doi: 10.5306/wjco.v2.i12.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perri F, Ionna F, Muto P, Buonerba C, Della Vittoria Scarpati G, Bosso D, Fulciniti F, Daponte A, Argenone A, Sandomenico F, et al. Induction docetaxel-cisplatin followed by extended-field radiotherapy in patients with cervical metastases from unknown primary carcinoma. Anticancer Res. 2013;33:1135–1139. [PubMed] [Google Scholar]
- 7.Smee RI, Meagher NS, Broadley K, Ho T, Williams JR, Bridger GP. Recurrent nasopharyngeal carcinoma: current management approaches. Am J Clin Oncol. 2010;33:469–473. doi: 10.1097/COC.0b013e3181b4b037. [DOI] [PubMed] [Google Scholar]
- 8.Roeder F, Zwicker F, Saleh-Ebrahimi L, Timke C, Thieke C, Bischof M, Debus J, Huber PE. Intensity modulated or fractionated stereotactic reirradiation in patients with recurrent nasopharyngeal cancer. Radiat Oncol. 2011;6:22. doi: 10.1186/1748-717X-6-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Teo PM, Kwan WH, Chan AT, Lee WY, King WW, Mok CO. How successful is high-dose (& gt; or = 60 Gy) reirradiation using mainly external beams in salvaging local failures of nasopharyngeal carcinoma? Int J Radiat Oncol Biol Phys. 1998;40:897–913. doi: 10.1016/s0360-3016(97)00854-7. [DOI] [PubMed] [Google Scholar]
- 10.Perri F, Muto P, Aversa C, Daponte A, Della Vittoria G, Pepe S, Caponigro F. Integrated therapeutic approaches in head and neck cancer: the importance of multidisciplinary team management. Anticancer Agents Med Chem. 2013;13:834–843. doi: 10.2174/18715206113139990110. [DOI] [PubMed] [Google Scholar]


