Abstract
We describe here the isolation and identification of a Shiga toxin 1 (Stx1)-producing Enterobacter cloacae strain, M12X01451, from a human clinical specimen. The bacterial isolate was identified as E. cloacae using a polyphasic approach that included phenotypic, genetic, and proteomic analyses. The M12X01451 stx1 was sequenced, and the holotoxin was found to share only 87% amino acid sequence identity with the nearest Stx1 subtype reference sequence. Sequence analysis of the regions immediately flanking stx1 displayed similarities with bacteriophage-related sequences, suggesting a prophage origin. The stx1 gene was a stable element within the M12X01451 genome, as demonstrated by real-time PCR detection following successive subculturing of the bacterial isolate. Culture supernatant from M12X01451 was cytotoxic to Vero cells but was not neutralized by an anti-Stx1 monoclonal antibody. In addition, Stx1 from M12X01451 demonstrated limited antigenicity with two commercially available lateral flow immunoassays. The M12X01451 Stx represents a new Stx1 subtype based on the degree of sequence dissimilarity with Stx1 subtype reference sequences and its limited reactivity with anti-Stx1 antibodies.
INTRODUCTION
Escherichia coli and other bacteria gain significant pathogenic potential through transduction by Stx-converting phages. The acquisition of Stx genes has been mainly attributed to lysogeny by short-tailed lambdoid phages belonging to the family Podoviridae (1). These phages have a broad host range facilitated, in part, through the recognition of BamA, an outer membrane protein that is highly conserved among Gram-negative bacteria (2). Following entry into the host bacteria, the phage genome may integrate at any one of several recognition sites within the host genome. For O157 E. coli, Stx-converting phages integrate into a limited number of locations within the bacteria genome (3). In contrast, the Stx-converting phage integration sites for non-O157 E. coli have been found to be much more diverse (4). The availability of multiple integration sites may facilitate the acquisition of several Stx-converting phages within a single host and confer the ability to produce different types or subtypes of Stx.
Shiga toxins are produced during lytic replication and assembly of Stx-converting phages within the bacterial host and are essential determinants of pathogenesis in human infections with Stx-producing E. coli (STEC). Structurally, Shiga toxins are A-B toxins, with the holotoxin consisting of five B subunits and a single A subunit. The B subunits direct binding of the holotoxin by interacting with the glycolipid globotriaosylceramide (Gb3), selectively expressed on the surface of eukaryotic cells. The A subunit is released from the B subunits upon entry into the cell and acts by inhibiting protein synthesis through N-glycosidase activity targeting adenine 4324 of the 28S rRNA component of the eukaryotic ribosome. Two types of Shiga toxins, Stx1 and Stx2, are distinguished based on the inability of antisera to provide cross-neutralization (5). The two toxin types share 56% amino acid sequence similarity (6). Several subtypes for each toxin type have been described. A recent effort to standardize Stx nomenclature proposed three Stx1 subtypes (Stx/Stx1, Stx1c, and Stx1d) and seven Stx2 subtypes (Stx2a through -g), based on phylogenetic analysis of holotoxin sequences (7). Shiga toxin subtypes have been found to differ in receptor preference and toxin potency. Notably, Stx2a and Stx2d are 100 times more potent than Stx1 and other Stx2 subtypes and are more likely to be associated with severe disease outcomes such as hemorrhagic colitis and hemolytic uremic syndrome (HUS) (8–11).
The acquisition of Stx-converting phages is largely associated with E. coli strains. However, other Stx-producing microorganisms have been infrequently reported and include Acinetobacter haemolyticus, Aeromonas sp., Citrobacter freundii, Enterobacter cloacae, and Escherichia albertii (12–16). The Shiga toxins expressed by these microorganisms have been found to be highly similar in amino acid sequences to those produced by E. coli strains. However, transduction of these microorganisms by Stx-converting phages appears to be relatively unstable, with reports of loss of Stx expression following a single subculture (13, 17). Here, we describe the characterization of an E. cloacae strain that produces a novel subtype of Stx1, the gene of which was stable with repeated subculture.
MATERIALS AND METHODS
Screening and isolation of STEC.
As a public health reference laboratory, the Microbial Diseases Laboratory (MDL) of the California Department of Public Health accepts Stx-positive enrichment broths for STEC isolation and confirmatory testing. Upon receipt, enrichment broths are plated onto MacConkey agar (MAC) and cefixime tellurite-sorbitol MacConkey agar (CT-SMAC) for colony isolation. Isolated colonies are subcultured to triple-sugar iron agar, lysine iron agar, and motility-ornithine-indole agar, and the resulting biochemical profiles are used to select cultures for further testing. Cultured isolates and the original enrichment broths are initially screened using real-time PCR for the detection of stx1 and stx2 (18). In a situation where stx is detected by real-time PCR for the enrichment broth but not the corresponding bacterial isolates, the original enrichment broth is subcultured to Luria-Bertani (LB) broth and the process of colony isolation and real-time PCR testing is repeated once more in an effort to isolate STEC. Additional testing using the Vero cell cytotoxicity assay may be implemented to confirm Stx expression and type (19). For Stx type determination, the monoclonal antibodies 13C4 and 11F11 (American Type Culture Collection, Manassas, VA) are used to demonstrate neutralization of Stx1 and Stx2, respectively, in the Vero cell cytotoxicity assay. Additionally, isolates may also be tested for the presence of the virulence genes eaeA and hlyA by PCR (20). Following this algorithm, a Gram-negative (GN) broth yielded a bacterial isolate, M12X01451, which produced Stx1.
Bacterial identification.
To determine species level identification, the bacterial isolate was subjected to conventional phenotypic and biochemical testing and partial 16S rRNA gene analysis as previously described (21, 22). The Ribosome Database Project (RDP) version 10 and the National Center for Biotechnology Information (NCBI) nr/nt database were searched for related 16S rRNA gene sequences, and the reference sequence having the highest score was considered the best match. Matrix-assisted laser desorption ionization–time of flight (MALDI-TOF) mass spectroscopy was also performed on extracted bacterial cells to assist with the identification of the bacterial isolate (23). The sample was analyzed using the Microflex LT instrument and Biotyper software version 3.0 (Bruker Daltonics, Billerica, MA).
Partial stx1 sequence analysis.
Two PCRs were used to generate partial stx1 sequences. The primer set of stx1–5′-F1/stx1-seq-R1 and the primer set of stx1-seq-F1/stx1–3′-R1 (Table 1) were used to amplify the 5′ end and the 3′ end of stx1, respectively. Nucleic acids were extracted by heating a suspension of M12X01451 in 10 mM Tris (pH 8.5) for 10 min at 95°C, subjecting it to mechanical disruption for 3 min using the Mini-Beadbeater-8 (Biospec Products, Bartlesville, OK), and removing the cell debris by centrifugation at 13,000 × g for 5 min. The PCRs consisted of the M12X01451 nucleic acid extract (each primer at 200 nM) and 1× Qiagen Multiplex PCR master mix (Qiagen Inc., Valencia, CA). Amplification was performed with the GeneAmp PCR system 9700 (Life Technologies, Grand Islands, NY) using the following parameters for stx1–5′-F1/stx1-seq-R1: 94°C for 15 min, 40 cycles of 94°C for 30 s, 52°C for 90 s, and 72°C for 90 s, followed by a final extension step of 72°C for 10 min. Similar amplification parameters were used for stx1-seq-F1/stx1–3′-R1, with the exception that the annealing temperature was lowered to 46°C. PCR products were separated by agarose gel electrophoresis and purified using the QIAquick gel extraction kit (Qiagen, Inc.). Purified PCR products were subjected to cycle sequencing, which was performed on the GeneAmp PCR system 9700 using the Dye Terminator cycle sequencing (DTCS) Quick Start kit (Beckman Coulter, Brea, CA) according to the manufacturer's recommendations. The cycle sequencing products were purified using Performa DTR gel filtration cartridges (Edge Biosystems, Gaithersburg, MD) and separated by capillary electrophoresis on the CEQ 8000 genetic analysis system (Beckman Coulter). Sequence assembly and analysis were performed using BioNumerics version 5.2 (Applied Maths, Austin, TX).
TABLE 1.
Oligonucleotides used in this study
| Oligonucleotide | Sequence (5′ to 3′) | Use(s) |
|---|---|---|
| stx1-seq-F1a | ATGTCATTCGCTCTGCAATAGGTAC | Amplification and partial sequencing |
| stx1–3′-R1 | TATTTAACATTGATGAACCYCC | Amplification and partial sequencing |
| stx1–5′-F1 | ATGGTGCTCAAGGAGTATTG | Amplification and partial sequencing |
| stx1-seq-R1a | GAAGAAGAGACTGAAGATTCCATCTG | Amplification and partial sequencing |
| stx1InvF1 | GGCATTCAGCGAATCCACATAC | Inverse nested PCR |
| stx1InvR1 | ACCAGATGGAATCTTCAGTCACTTC | Inverse nested PCR |
| stx1InvF2 | GCTGTGGAGAAATCGACTGTAAAATC | Inverse nested PCR |
| stx1InvR2 | CAAATTACGGGGATGACGATAACC | Inverse nested PCR |
| stx1e-seq-F1 | GCAACCATGCTCTGGAATAC | Amplification of stx1e holotoxin |
| stx1e-seq-R1 | GTGTTGAAACAGAAACGCCT | Amplification of stx1e holotoxin |
| stx1e-seq-F2 | CTAATGCAGTCGCCCAGGAT | stx1e sequencing |
| stx1e-seq-F3 | TTTGTTACGGTGACAGCCGA | stx1e sequencing |
| stx1e-seq-F4 | GTGTTGGCAGCACCTGATTG | stx1e sequencing |
| stx1e-seq-R2 | CCTCACTGAACCCCTCTCCA | stx1e sequencing |
| stx1e-seq-R3 | CTCAGCCTTCCCCAGTTCAG | stx1e sequencing |
| stx1e-seq-R4 | AAAATCCTGGGCGACTGCAT | stx1e sequencing |
| EcloacStx1F | GGAAGGCTGAGCAGTGTTCTG | stx1e real-time PCR |
| EcloacStx1R | GGATTGCATTAACCCCTCCAAAAG | stx1e real-time PCR |
| EcloacStx1TMP | FAM-CCCAACACGAACAGAGTCTTGCCCA-BHQ1b | stx1e real-time PCR |
Previously described oligonucleotide (7).
FAM, 6-carboxyfluorescein; BHQ1, Black Hole quencher.
Inverse nested PCR and DNA sequencing.
Genomic DNA was extracted and purified from M12X01451 using the DNeasy tissue kit (Qiagen, Inc.) according to the manufacturer's recommendations for Gram-negative bacteria. Five micrograms of DNA was restricted with BspHI (New England BioLabs, Ipswich, MA) for 1 h at 37°C and the DNA fragments were purified using the QIAamp PCR purification kit (Qiagen, Inc.). The purified DNA was diluted 1:100, and DNA ligation was performed for 30 min at 16°C with T4 DNA ligase (New England BioLabs). The initial round of inverse PCR was performed using the Q5 High-Fidelity PCR kit (New England BioLabs) and the external primer set of stx1InvF1 and stx1InvR1 (Table 1) at a final concentration of 500 nM each. The PCR was diluted 1:10, and 1 μl of this dilution was subjected to a second round of PCR using the Q5 High-Fidelity PCR kit and the internal primer set stx1InvF2 and stx1InvR2 (Table 1) at a final concentration of 500 nM each. For both PCRs, the reaction volumes were 25 μl and the amplification parameters were as follows: 98°C for 30 s, 35 cycles of 98°C for 10 s, 67°C for 30 s, and 72°C for 3 min, and then a single final extension step of 72°C for 2 min. The nested PCR product was purified using the QIAamp PCR purification kit, and the flanking regions were sequenced using the primers stx1InvF2 and stx1InvR2. Based on this sequence, primers stx1e-seq-F1 and stx1e-seq-R1 (Table 1) were designed to amplify a 2,259-bp segment encompassing the complete coding region of stx1. Amplification was performed using the conditions described above for the Q5 High-Fidelity PCR kit. Bidirectional sequencing of the amplified product was performed as described earlier using the primers listed in Table 1.
stx1 stability.
A fresh culture of M12X01451 was prepared from a frozen stock by inoculating 5 ml of tryptone broth, incubating for 4 h at 35°C, followed by a subculture to motility agar. After a 24-h incubation at 35°C, a loopful of growth was used to inoculate 2 ml of LB broth and the culture incubated at 35°C for another 24 h. A 10 μl loopful of bacterial growth was then transferred to a fresh 2 ml tube of LB broth and the culture incubated for 24 h at 35°C. Subcultures were prepared in this way for 10 consecutive days. Following each 24-h incubation, a 200-μl aliquot of the culture was removed and stored at −20°C for testing by real-time PCR. For preparation of nucleic acids, the aliquots were centrifuged at 13,000 × g for 5 min and the cell pellets were resuspended in 200 μl of molecular grade water and heated at 95°C for 10 min. The cellular debris was removed by centrifugation at 13,000 × g for 5 min and the supernatant used as the template for real-time PCR. A primer and probe set targeting stx1 (Table 1) from M12X01451 was designed using Beacon Designer software (Premier BioSoft, Palo Alto, CA) for the development of a fluorogenic 5′ exonuclease assay. Nucleic acid extracts from the consecutive subcultures of M12X01451 were tested at a 1:100 dilution using the QuantiFast Probe PCR kit (Qiagen Inc.) and the ABI 7500 FAST real-time PCR system according to the manufacturer's recommendation.
Lateral flow immunoassays.
The ability of two lateral flow immunoassays, the Shiga Toxin Quik Chek (Alere, Waltham, MA) and the Immunocard STAT! EHEC (Meridian Bioscience, Cincinnati, OH) were evaluated for the ability to detect Shiga toxin produced by M12X01451. Both immunoassays were performed following the package inserts for the agar plate method. Kit controls were tested in parallel with M12X01451 and performed as expected.
Nucleotide sequence accession number.
The M12X01451 stx1 sequence was submitted to GenBank and assigned the accession number KF926684.
RESULTS
Isolation and identification of a Stx1-producing E. cloacae.
The case patient sought medical attention for nonbloody diarrhea and abdominal cramping that persisted for 5 days. Neither vomiting nor fever was noted. With the exception of colonic cleansing every 2 weeks for the 2 months preceding illness onset, the case patient's medical and food exposure history was unremarkable. A stool specimen was collected from the case patient and submitted to a commercial laboratory, where an enrichment broth of the stool sample tested positive for Stx by immunoassay. In accordance with recommendations from the Centers for Disease Control and Prevention, the commercial laboratory forwarded the Stx-positive broth to its local public health laboratory for STEC isolation (24). The local public health laboratory, in turn, submitted the broth and three suspected STEC isolates to the MDL for STEC confirmation and Stx typing. The suspected STEC isolates were negative for stx1 and stx2, whereas the broth tested positive for stx1 by real-time PCR. Testing of the broth by the Vero cell assay demonstrated typical Stx cytotoxicity. However, the cytotoxicity was not neutralized by the monoclonal antibody 13C4, which recognizes the B subunit of Stx1. Direct plating of the broth onto MAC and CT-SMAC plates failed to yield an STEC isolate. The submitted broth was also subcultured to LB broth for enrichment and subsequently plated onto MAC and CT-SMAC plates. Colony screening by real-time PCR detected stx1 from 1 of 10 suspect isolates tested, whereas stx2 was undetected for all isolates. To ensure purity, the colony was streaked onto an MAC plate, and a bacterial isolate was picked for testing by real-time PCR and Vero cell cytotoxicity. The bacterial isolate was designated M12X01451. Real-time PCR testing of M12X01451 consistently produced late cycle threshold (CT) values (∼32 cycles) for stx1. The culture supernatant from M12X01451 produced typical Stx cytotoxicity, and the endpoint of cytotoxicity was titrated at a 1:10,000 dilution. As was demonstrated for the broth sample, the monoclonal antibody, 13C4, failed to neutralize cytotoxicity even at the lowest cytotoxic dose of the M12X01451 culture supernatant (data not shown). Additional characterization of M12X01451 failed to demonstrate the presence of the STEC virulence genes eaeA and hlyA.
Identification of the Stx-producing isolate, M12X01451, was accomplished using a polyphasic testing approach that consequently identified it as E. cloacae. Phenotypic characteristics that distinguished this isolate from E. coli (as well as other members of the Enterobacter and Pantoea agglomerans) included positive reactions for Voges-Proskauer, ornithine decarboxylase, arginine dihydrolase, citrate, and malonate; negative reactions for indole and lysine decarboxylase; and hydrolysis of urea and esculin. Acid fermentation was also present in l-rhamnose, cellobiose, alpha-methyl d-glucoside, sucrose, d-sorbitol, and melibiose. MALDI-TOF mass spectroscopy was performed and provided a best match with E. cloacae (identification score of 2.233) but did not rule out other members of the E. cloacae complex, including Enterobacter kobei (identification score of 2.078) and Enterobacter ludwigii (identification score of 2.017), using the 10% score differential for species identification (25). Partial 16S rRNA sequencing provided 1,419 nucleotides (nt) that matched an E. cloacae strain with 100% sequence identity following a search of the NCBI database and produced a score of 1.000 using the RDP Seqmatch. A search of RDP type strain 16S rRNA sequences provided a best score of 0.989 with E. cloacae type strain ATCC 13047. The next best species level match was the E. ludwigii type strain EN-119 with a score of 0.945. Taken together, the laboratory data supported the identification of this Shiga toxin-producing isolate as E. cloacae.
Sequence analysis of M12X01451 stx1.
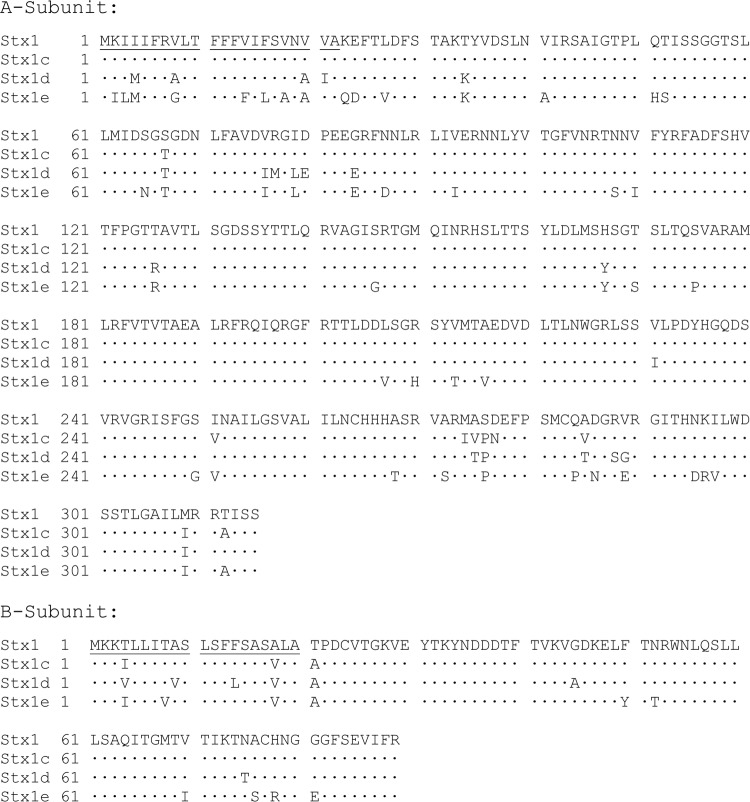
The consistently late CT values obtained for M12X01451 by real-time PCR suggested stx1 sequence polymorphisms. Attempts to amplify the entire coding region of stx1 using primers designed to match regions immediately flanking stx1 were unsuccessful. PCR amplifications using highly conserved internal stx1 primer sequences were successful at low annealing temperatures and yielded a partial sequence for stx1 of M12X01451. Based on this partial sequence, inverse nested PCR was performed to obtain sequence information flanking stx1. Primers designed from the flanking sequences were used to amplify and sequence a 2,259-bp fragment encompassing the entire stx1 coding region of M12X01451 as well as the immediate 5′ and 3′ nucleotide sequences flanking stx1. The M12X01451 holotoxin gene sequence is 1,227 bp in length and contains a 9-bp intervening sequence between stxA1 and stxB1. Comparison of the M12X01451 holotoxin gene sequence with other stx1 sequences in the NCBI nr/nt database indicated a best match at 87% nucleotide sequence identity. An NCBI BLASTp search with the M12X01451 StxA1 indicated a best match of 87% amino acid sequence identity with several StxA1 sequences and 86% sequence identity with the archetypal Stx/StxA1 sequence. A similar search using the subunit B amino sequence for M12X01451 yielded a best match of 92% with several StxB1 sequences and 60% sequence identity with the archetypal Stx/StxB1 sequence. An amino acid comparison of the M12X01451 Stx1 with Stx1 subtype reference sequences is shown in Fig. 1. Relative to Stx/Stx1, amino acid substitutions are biased toward the amino- and carboxy-terminal ends of the A and B subunits of Stx1 from M12X01451, with several substitutions localized to the putative signal peptide sequences. Among the Stx1 subtype reference sequences, the M12X01451 Stx1 sequence is most closely related to Stx1c, sharing 87.4% sequence identity for the holotoxin.
FIG 1.
Amino acid comparison of M12X01451 Stx1e with Stx1 subtype reference sequences. Stx1 subtype reference strains (and corresponding GenBank sequences) are Stx1 (strain EDL933) (M19473), Stx1c (strain DG131/3) (Z36901), and Stx1d (strain MHI813) (AY170851). Amino acids conserved with the Stx1 sequence are indicated with a dot. Amino acid substitutions are indicated by a single-letter amino acid designation. Signal peptide regions are underlined.
The NCBI nr/nt database was queried for sequences similar to the 5′ and 3′ flanking regions of M12X01451 stx1. An NCBI megablast search of the 859 nt immediately upstream of M12X01451 stx1 yielded two results, 93% sequence identity to a region of the E. cloacae NCTC 9394 draft genome (GenBank accession number FP929040) and 90% sequence identity to a region of enterotoxigenic E. coli UHNK88 complete genome (GenBank accession number CP002729). Both of these regions contain a partial coding sequence for a putative antiterminator protein and appear to be phage associated based on the annotation of the surrounding genes. An NCBI BLASTn search for sequences related to the 173 bp flanking the 3′ end of M12X01451 stx1 provided a best score (79% sequence similarity; 97 of 123 nt) with a region of the Escherichia phage 1720a-02 complete genome (GenBank accession number KF030455). These results suggest that the nucleotide sequence flanking M12X01451 stx1 is likely phage derived.
Stability of M12X01451 stx1.
To assess the stability of stx1, M12X01451 was subcultured daily for 10 days and a sample of the overnight growth was tested by a real-time PCR assay targeting M12X01451 stx1. The CT value for each sample remained consistent over the course of the study, indicating that stx1 is a relatively stable element within the M12X01451 genome (data not shown).
Lateral flow immunoassay detection of M12X01451 Stx1.
Two lateral flow immunoassays, the Shiga Toxin Quik Chek and Immunocard STAT! EHEC, were evaluated for detection of M12X01451 Stx1. A negative test result was obtained with the Immunocard STAT! EHEC immunoassay, whereas a weak-positive Stx1 result was achieved with the Shiga Toxin Quik Chek immunoassay.
DISCUSSION
We have described the isolation and identification of an E. cloacae strain producing a novel Stx1 subtype from a patient with a mild diarrheal illness. The genus Enterobacter is classified within the family Enterobacteriaceae and its members have a widespread environmental distribution, including occupying ecologic niches such as soil, plants, and animals. Members of the E. cloacae complex are being increasingly recognized as significant pathogens with regard to health care-associated infections and emerging antimicrobial resistance. A Stx-producing E. cloacae strain has been previously described (15). This strain was isolated along with an STEC strain from the feces of an infant patient with HUS. Both the E. cloacae and STEC isolates possessed closely related stx2. The E. cloacae stx2 coding region was fully sequenced and was recently classified as an Stx2a variant (7). A subsequent report on this E. cloacae strain indicated that stx2 was unstable and that the gene was no longer detectable upon subculture of frozen stocks (26). Instability of stx has been noted in STEC strains and appears to be a fairly common characteristic of other Stx-producing microorganisms (12–14, 17). In contrast to the Stx2-producing E. cloacae strain, the M12X01451 stx1 was detected following repeated subculture, indicating that the gene is relatively stable. DNA sequencing of the regions immediately flanking M12X01451 stx1 provided evidence that the gene is likely maintained by a prophage within the M12X01451 genome. Confirmation of this awaits whole-genome sequencing of M12X01451 and transduction studies demonstrating M12X01451 Stx1 conversion of a naive bacterial strain.
In general, Stx2 displays greater sequence heterogeneity than Stx1. Seven subtypes of Stx2 and three subtypes of Stx1 have recently been proposed based on phylogenetic comparison of holotoxin amino acid sequences (7). Amino acid sequence similarities of 96% and 83% were used to define cutoff values for Stx1 and Stx2 subtype determinations, respectively. Stx subtypes can be further refined into Stx variants, which may represent as little as a single amino acid substitution. The Stx1 amino acid sequence for M12X01451 was found to share only 87% sequence identity with the nearest Stx1 subtype reference sequence, which would be considered well below the cutoff value for Stx1 subtype identification. Given the sequence dissimilarity of the M12X01451 Stx1 with known Stx1 subtypes, and conforming to recent nomenclature recommendations, we propose that the M12X01451 Stx1 holotoxin be designated Stx1e.
Relative to Stx/Stx1, amino acid substitutions in Stx1e were located throughout the A and B subunits but were more prevalent in the amino- and carboxy-terminal regions of both subunits. Amino acid residues considered to be essential to the catalytic activity of the A subunit were conserved in Stx1e. Notably, amino acids Y77, Y114, E167, R170, and W203 (amino acid numbering based on the sequence for the mature protein), which are critical to the active site of StxA1 (27), are conserved within the Stx1e sequence. In contrast, the B subunit of Stx1e has several amino acid substitutions that are located within regions predicted to interact with Gb3. The crystal structure of the Stx1 B pentamer complexed with a Gb3 analogue has been resolved and revealed three receptor-binding sites, referred to as binding sites 1 to 3 (28, 29). Binding site 2 is considered to be the primary high-affinity binding site for Gb3. StxB1e has two substitutions in critical amino acids, F30Y and A56S (amino acid numbering based on the sequence for the mature protein), within binding site 2. A third substitution, N32T, is located in binding site 1. The F30Y and the N32T substitutions represent conservative changes in amino acids, whereas the A56S constitutes a change from a nonpolar to a polar amino acid. Further characterization of Stx1e is needed to determine if these amino acid substitutions have an influence on receptor binding affinity, specificity, and toxin potency, as has been demonstrated for the subunit B variant, Stx2d, and through mutagenesis studies for other Stx subtypes (30–32). The amino acid substitutions in binding sites 1 and 2 of Stx1e may also explain its lack of recognition by the Stx1-neutralizing monoclonal antibody 13C4. The epitope recognized by 13C4 has been mapped to a nonlinear region overlapping binding sites 1 and 2 of StxB1 (33). An asparagine at position 55 of StxB1 was found to be essential for 13C4 recognition. Stx1d, which has an N55T substitution in the B subunit, is refractory to detection by 13C4 (34). Similarly, the substitution noted in the adjacent amino acid (A56S) of Stx1e may also play a critical role in 13C4 recognition.
The lack of recognition by 13C4 and the significant amino acid sequence divergence indicate that Stx1e may differ antigenically from other Stx1 subtypes. Lateral flow immunoassays are convenient methods for detecting Stx and can be used to distinguish between Stx1 and Stx2. While initially detected by an undisclosed enzyme-linked immunoassay at a commercial laboratory, Stx1e was not detected by the Immunocard STAT! EHEC immunoassay and was only weakly detected by the Shiga Toxin Quik Chek immunoassay—both lateral flow immunoassays approved by the Food and Drug Administration for Stx detection. The limited ability of the lateral flow immunoassays to detect Stx1e likely reflects antigenic differences, as the amount of antigen tested was well within the analytical sensitivity of the assays. These results suggest that Stx1e may prove to be a diagnostic challenge for some antigen detection systems and that better diagnostic tools may be needed to assess the prevalence, distribution, and clinical relevance of Stx1e.
ACKNOWLEDGMENT
We thank Akiko Kimura of the Infectious Diseases Branch of CDPH for providing epidemiologic support for this investigation.
Footnotes
Published ahead of print 23 April 2014
REFERENCES
- 1. Smith DL, Wareing BM, Fogg PC, Riley LM, Spencer M, Cox MJ, Saunders JR, McCarthy AJ, Allison HE. 2007. Multilocus characterization scheme for shiga toxin-encoding bacteriophages. Appl. Environ. Microbiol. 73:8032–8040. 10.1128/AEM.01278-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Smith DL, James CE, Sergeant MJ, Yaxian Y, Saunders JR, McCarthy AJ, Allison HE. 2007. Short-tailed stx phages exploit the conserved YaeT protein to disseminate Shiga toxin genes among enterobacteria. J. Bacteriol. 189:7223–7233. 10.1128/JB.00824-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ogura Y, Ooka T, Asadulghani Terajima J, Nougayrède JP, Kurokawa K, Tashiro K, Tobe T, Nakayama K, Kuhara S, Oswald E, Watanabe H, Hayashi T. 2007. Extensive genomic diversity and selective conservation of virulence-determinants in enterohemorrhagic Escherichia coli strains of O157 and non-O157 serotypes. Genome Biol. 8:R138. 10.1186/gb-2007-8-7-r138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Steyert SR, Sahl JW, Fraser CM, Teel LD, Scheutz F, Rasko DA. 2012. Comparative genomics and stx phage characterization of LEE-negative Shiga toxin-producing Escherichia coli. Front. Cell. Infect. Microbiol. 2:133. 10.3389/fcimb.2012.00133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Strockbine NA, Marques LR, Newland JW, Smith HW, Holmes RK, O'Brien AD. 1986. Two toxin-converting phages from Escherichia coli O157:H7 strain 933 encode antigenically distinct toxins with similar biologic activities. Infect. Immun. 53:135–140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jackson MP, Neill RJ, O'Brien AD, Holmes RK, Newland JW. 1987. Nucleotide sequence analysis and comparison of the structural genes for Shiga-like toxin I and Shiga-like toxin II encoded by bacteriophages from Escherichia coli 933. FEM Microbiol. Lett. 44:109–114. 10.1111/j.1574-6968.1987.tb02252.x [DOI] [PubMed] [Google Scholar]
- 7. Scheutz F, Teel LD, Beutin L, Piérard D, Buvens G, Karch H, Mellmann A, Caprioli A, Tozzoli R, Morabito S, Strockbine NA, Melton-Celsa AR, Sanchez M, Persson S, O'Brien AD. 2012. Multicenter evaluation of a sequence-based protocol for subtyping Shiga toxins and standardizing Stx nomenclature. J. Clin. Microbiol. 50(9):2951–2963. 10.1128/JCM.00860-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fuller CA, Pellino CA, Flagler MJ, Strasser JE, Weiss AA. 2011. Shiga toxin subtypes display dramatic differences in potency. Infect. Immun. 79:1329–1337. 10.1128/IAI.01182-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bielaszewska M, Friedrich AW, Aldick T, Schürk-Bulgrin R, Karch H. 2006. Shiga toxin activatable by intestinal mucus in Escherichia coli isolated from humans: predictor for a severe clinical outcome. Clin. Infect. Dis. 43:1160–1167. 10.1086/508195 [DOI] [PubMed] [Google Scholar]
- 10. Friedrich AW, Bielaszewska M, Zhang WL, Pulz M, Kuczius T, Ammon A, Karch H. 2002. Escherichia coli harboring Shiga toxin 2 gene variants: frequency and association with clinical symptoms. J. Infect. Dis. 185:74–84. 10.1086/338115 [DOI] [PubMed] [Google Scholar]
- 11. Persson S, Olsen KE, Ethelberg S, Scheutz F. 2007. Subtyping method for Escherichia coli Shiga toxin (verocytotoxin) 2 variants and correlations to clinical manifestations. J. Clin. Microbiol. 2007 45:2020–2024. 10.1128/JCM.02591-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Grotiuz G, Sirok A, Gadea P, Varela G, Schelotto F. 2006. Shiga toxin 2-producing Acinetobacter haemolyticus associated with a case of bloody diarrhea. J. Clin. Microbiol. 44:3838–3841. 10.1128/JCM.00407-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Alperi A, Figueras MJ. 2010. Human isolates of Aeromonas possess Shiga toxin genes (stx1 and stx2) highly similar to the most virulent gene variants of Escherichia coli. Clin. Microbiol. Infect. 16:1563–1567. 10.1111/j.1469-0691.2010.03203.x [DOI] [PubMed] [Google Scholar]
- 14. Schmidt H, Montag M, Bockemühl J, Heesemann J, Karch H. 1993. Shiga-like toxin II-related cytotoxins in Citrobacter freundii strains from humans and beef samples. Infect. Immun. 1993 61:534–543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Paton AW, Paton JC. 1996. Enterobacter cloacae producing a Shiga-like toxin II-related cytotoxin associated with a case of hemolytic-uremic syndrome. J. Clin. Microbiol. 1996 34:463–465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ooka T, Seto K, Kawano K, Kobayashi H, Etoh Y, Ichihara S, Kaneko A, Isobe J, Yamaguchi K, Horikawa K, Gomes TA, Linden A, Bardiau M, Mainil JG, Beutin L, Ogura Y, Hayashi T. 2012. Clinical significance of Escherichia albertii. Emerg. Infect. Dis. 18:488–492. 10.3201/eid1803.111401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bielaszewska M, Prager R, Köck R, Mellmann A, Zhang W, Tschäpe H, Tarr PI, Karch H. 2007. Shiga toxin gene loss and transfer in vitro and in vivo during enterohemorrhagic Escherichia coli O26 infection in humans. Appl. Environ. Microbiol. 73:3144–3150. 10.1128/AEM.02937-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jinneman KC, Yoshitomi KJ, Weagant SD. 2003. Multiplex real-time PCR method to identify Shiga toxin genes stx1 and stx2 and Escherichia coli O157:H7/H-serotype. Appl. Environ. Microbiol. 69:6327–6333. 10.1128/AEM.69.10.6327-6333.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Crandall C, Abbott SL, Zhao YQ, Probert W, Janda JM. 2006. Isolation of toxigenic Hafnia alvei from a probable case of hemolytic uremic syndrome. Infection. 34:227–229. 10.1007/s15010-006-5088-6 [DOI] [PubMed] [Google Scholar]
- 20. Wang G, Clark CG, Rodgers FG. 2002. Detection in Escherichia coli of the genes encoding the major virulence factors, the genes defining the O157:H7 serotype, and components of the type 2 Shiga toxin family by multiplex PCR. J. Clin. Microbiol. 40:3613–3619. 10.1128/JCM.40.10.3613-3619.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Janda JM, Abbott SL, Khashe S, Probert W. 2002. Phenotypic and genotypic properties of the genus Hafnia. J. Med. Microbiol. 51:575–580 [DOI] [PubMed] [Google Scholar]
- 22. Schuurman T, de Boer RF, Kooistra-Smid AM, van Zwet AA. 2004. Prospective study of use of PCR amplification and sequencing of 16S ribosomal DNA from cerebrospinal fluid for diagnosis of bacterial meningitis in a clinical setting. J. Clin. Microbiol. 42:734–740. 10.1128/JCM.42.2.734-740.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mellmann A, Cloud J, Maier T, Keckevoet U, Ramminger I, Iwen P, Dunn J, Hall G, Wilson D, Lasala P, Kostrzewa M, Harmsen D. 2008. Evaluation of matrix-assisted laser desorption ionization-time-of-flight mass spectrometry in comparison to 16S rRNA gene sequencing for species identification of nonfermenting bacteria. J. Clin. Microbiol. 46:1946–1954. 10.1128/JCM.00157-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gould LH, Bopp C, Strockbine N, Atkinson R, Baselski V, Body B, Carey R, Crandall C, Hurd S, Kaplan R, Neill M, Shea S, Somsel P, Tobin-D'Angelo M, Griffin PM, Gerner-Smidt PCenters for Disease Control and Prevention (CDC). 2009. Recommendations for diagnosis of Shiga toxin–producing Escherichia coli infections by clinical laboratories. MMWR Recomm. Rep. 58:1–14 [PubMed] [Google Scholar]
- 25. Degand N, Carbonnelle E, Dauphin B, Beretti JL, Le Bourgeois M, Sermet-Gaudelus I, Segonds C, Berche P, Nassif X, Ferroni A. 2008. Matrix-assisted laser desorption ionization–time of flight mass spectrometry for identification of nonfermenting Gram-negative bacilli isolated from cystic fibrosis patients. J. Clin. Microbiol. 46:3361–3367. 10.1128/JCM.00569-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Paton JC, Paton AW. 1997. Instability of a Shiga toxin type 2 gene in Enterobacter cloacae. J. Clin. Microbiol. 35:1917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Deresiewicz RL, Calderwood SB, Robertus JD, Collier RJ. 1992. Mutations affecting the activity of the Shiga-like toxin I A-chain. Biochemistry 31:3272–3280. 10.1021/bi00127a032 [DOI] [PubMed] [Google Scholar]
- 28. Ling H, Boodhoo A, Hazes B, Cummings MD, Armstrong GD, Brunton JL, Read RJ. 1998. Structure of the Shiga-like toxin I B-pentamer complexed with an analogue of its receptor Gb3. Biochemistry 37:1777–1788. 10.1021/bi971806n [DOI] [PubMed] [Google Scholar]
- 29. Bast DJ, Banerjee L, Clark C, Read RJ, Brunton JL. 1999. The identification of three biologically relevant globotriaosyl ceramide receptor binding sites on the Verotoxin 1 B subunit. Mol. Microbiol. 32:953–960. 10.1046/j.1365-2958.1999.01405.x [DOI] [PubMed] [Google Scholar]
- 30. Ling H, Pannu NS, Boodhoo A, Armstrong GD, Clark CG, Brunton JL, Read RJ. 2000. A mutant Shiga-like toxin IIe bound to its receptor Gb(3): structure of a group II Shiga-like toxin with altered binding specificity. Structure. 8:253–264. 10.1016/S0969-2126(00)00103-9 [DOI] [PubMed] [Google Scholar]
- 31. Samuel JE, Perera LP, Ward S, O'Brien AD, Ginsburg V, Krivan HC. 1990. Comparison of the glycolipid receptor specificities of Shiga-like toxin type II and Shiga-like toxin type II variants. Infect. Immun. 58:611–618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Cummings MD, Ling H, Armstrong GD, Brunton JL, Read RJ. 1998. Modeling the carbohydrate-binding specificity of pig edema toxin. Biochemistry 37:1789–1799. 10.1021/bi971807f [DOI] [PubMed] [Google Scholar]
- 33. Smith MJ, Carvalho HM, Melton-Celsa AR, O'Brien AD. 2006. The 13C4 monoclonal antibody that neutralizes Shiga toxin type 1 (Stx1) recognizes three regions on the Stx1 B subunit and prevents Stx1 from binding to its eukaryotic receptor globotriaosylceramide. Infect. Immun. 74:6992–6998. 10.1128/IAI.01247-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bürk C, Dietrich R, Açar G, Moravek M, Bülte M, Märtlbauer E. 2003. Identification and characterization of a new variant of Shiga toxin 1 in Escherichia coli ONT:H19 of bovine origin. J. Clin. Microbiol. 41:2106–2112. 10.1128/JCM.41.5.2106-2112.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]