ABSTRACT
Live attenuated cold-adapted (ca) H5N1, H7N3, H6N1, and H9N2 influenza vaccine viruses replicated in the respiratory tract of mice and ferrets, and 2 doses of vaccines were immunogenic and protected these animals from challenge infection with homologous and heterologous wild-type (wt) viruses of the corresponding subtypes. However, when these vaccine candidates were evaluated in phase I clinical trials, there were inconsistencies between the observations in animal models and in humans. The vaccine viruses did not replicate well and immune responses were variable in humans, even though the study subjects were seronegative with respect to the vaccine viruses before vaccination. Therefore, we sought a model that would better reflect the findings in humans and evaluated African green monkeys (AGMs) as a nonhuman primate model. The distribution of sialic acid (SA) receptors in the respiratory tract of AGMs was similar to that in humans. We evaluated the replication of wt and ca viruses of avian influenza (AI) virus subtypes H5N1, H6N1, H7N3, and H9N2 in the respiratory tract of AGMs. All of the wt viruses replicated efficiently, while replication of the ca vaccine viruses was restricted to the upper respiratory tract. Interestingly, the patterns and sites of virus replication differed among the different subtypes. We also evaluated the immunogenicity and protective efficacy of H5N1, H6N1, H7N3, and H9N2 ca vaccines. Protection from wt virus challenge correlated well with the level of serum neutralizing antibodies. Immune responses were slightly better when vaccine was delivered by both intranasal and intratracheal delivery than when it was delivered intranasally by sprayer. We conclude that live attenuated pandemic influenza virus vaccines replicate similarly in AGMs and human subjects and that AGMs may be a useful model to evaluate the replication of ca vaccine candidates.
IMPORTANCE Ferrets and mice are commonly used for preclinical evaluation of influenza vaccines. However, we observed significant inconsistencies between observations in humans and in these animal models. We used African green monkeys (AGMs) as a nonhuman primate (NHP) model for a comprehensive and comparative evaluation of pairs of wild-type and pandemic live attenuated influenza virus vaccines (pLAIV) representing four subtypes of avian influenza viruses and found that pLAIVs replicate similarly in AGMs and humans and that AGMs can be useful for evaluation of the protective efficacy of pLAIV.
INTRODUCTION
Ahighly pathogenic (HP) H5N1 avian influenza (AI) virus has caused numerous outbreaks in wild and domestic birds and has infected several mammalian species, including humans, since it emerged in Hong Kong in 1997 (1) and reemerged in China (2, 3) in 2003 and in Vietnam (4) and Thailand (5) in 2004. From 2003 through 2013, there have been more than 600 laboratory-confirmed human H5N1 cases and more than 300 deaths in 15 countries (6). In addition to H5N1 virus infections, outbreaks of H7 AI in poultry have been associated with sporadic transmission to humans (7, 8) and H9N2 subtype AI viruses have also crossed the species barrier and transmitted to humans (9–11). In 2009, a swine-origin H1N1 virus emerged in humans and caused the first influenza pandemic in 40 years. In response to the threat of a pandemic caused by animal influenza viruses, several pandemic vaccines have been developed and evaluated in humans (12–18).
The two types of seasonal influenza vaccines that are licensed and widely distributed in the United States are inactivated and live attenuated virus vaccines; both of these platforms have been used to develop vaccines against pandemic influenza (19, 20). Clinical studies with inactivated split-virion or whole-virion H5N1 vaccines indicate that multiple doses, a large antigen dose, or an oil-in-water adjuvant is necessary to elicit the level of immunity required to meet the serologic criteria for vaccine licensure (13, 14, 21–23), and in the absence of adjuvant, whole-virus vaccines induced more robust immune responses than split-virion vaccines (18).
There are several features of live attenuated influenza virus vaccines (LAIV) that may be advantageous in the event of a pandemic. First, LAIV induce broad cross protection against heterologous strains in naive individuals (24, 25). Because the identity of a pandemic strain cannot be predicted, a vaccine that induces a broadly cross-reactive immune response is desirable. Second, intranasally (i.n.) delivered LAIV elicit mucosal antibodies (Abs) and cellular immune responses as well as serum antibodies (26). Third, the yield of LAIV doses in embryonated eggs is greater than that of inactivated influenza virus vaccines, making it possible to manufacture vaccine for larger numbers of people. Two LAIV backbones are licensed for seasonal influenza in different parts of the world. The influenza A virus strains contained in the LAIV licensed in the United States are composed of 6 internal protein genes of the influenza A/Ann Arbor/6/60 (H2N2) cold-adapted (ca) (AA ca) virus and the two surface glycoprotein genes, hemagglutinin (HA) and neuraminidase (NA), of the circulating strain of interest. The LAIV licensed in Russia uses the A/Leningrad/137/17/57 ca virus as a backbone (27, 28). Both platforms were used to develop pandemic influenza virus vaccines (20), and several AA ca-virus-based vaccine candidates, including the H5N1, H6N1, H7N3, and H9N2 subtypes, have been tested in preclinical studies in mice and ferrets and in phase I clinical trials in humans (12, 15, 29–34). Although the vaccine viruses replicated well in the upper respiratory tract tissues of mice and ferrets, they were restricted in the lower respiratory tract as was anticipated based on their temperature-sensitive phenotype. The immune responses induced by two doses of the AA ca virus pandemic vaccines were sufficient to protect animals against lethal infection and/or viral replication in the lower respiratory tract upon challenge with wild-type (wt) viruses (31–34). However, the replication of and immune responses to these vaccines were variable in humans (12, 15, 29, 30). Therefore, we sought an animal model that would better reflect the findings in humans and considered nonhuman primates (NHPs) because of their genetic and physiological similarity to humans. Several species of NHPs have previously been used to study AI virus infection and vaccine efficacy (35–38). African green monkeys (AGMs) have been successfully used as NHP models for other respiratory viruses, including parainfluenza viruses (39, 40), respiratory syncytial virus (41), and severe acute respiratory syndrome (SARS) coronavirus (42). Therefore, we undertook an evaluation of several different subtypes of influenza A viruses in AGMs.
MATERIALS AND METHODS
Viruses and cells.
A/Vietnam/1203/2004 (H5N1) wt (H5N1 wt), A/teal/Hong Kong/W312/97 (H6N1) wt (H6N1 wt), A/chicken/British Columbia/CN-7/2004 (H7N3) wt (H7N3 wt), and A/chicken/Hong Kong/G9/97 (H9N2) wt (H9N2 wt) virus strains were kindly provided by Alexander Klimov and Nancy Cox of the Centers for Disease Control and Prevention, John Pasick, Canadian Food Inspection Agency, National Centre for Foreign Animal Disease, Winnipeg, Canada, and Robert G. Webster, St. Jude Children's Research Hospital, Memphis, TN. The reassortant A/Vietnam/1203/2004 (H5N1) ca virus strain in which the multibasic amino acid site in the HA was deleted (H5N1 ca) and the A/teal/Hong Kong/W312/97 (H6N1) ca (H6N1 ca) and A/chicken/British Columbia/CN-6/2004 (H7N3) ca (H7N3 ca) virus strains were generated by reverse genetics as described previously (32). The A/chicken/Hong Kong/G9/97 (H9N2) ca (H9N2 ca) virus strain was generated by genetic reassortment (33). Viruses were propagated in 10-to-11-day-old embryonated hen's eggs.
Madin-Darby canine kidney (MDCK) cells were maintained in modified Eagle's medium with 10% fetal calf serum and l-glutamine.
Animals.
Adult male or female African green monkeys (AGMs [Chlorocebus aethiops]) were used. All experiments, including animal studies with HPAI viruses H5N1 and H7N3, were conducted in enhanced biosafety level 3 (BSL-3) containment laboratories approved for use by the U.S. Department of Agriculture and Centers for Disease Control and Prevention. Animal experiments were done at Bioqual, Inc. (Rockville, MD) and at the NIH in compliance with the guidelines of the respective Institutional Animal Care and Use Committees.
Virus inoculation and sample collection.
Groups of AGMs were inoculated with 2 × 106 50% tissue culture infectious doses (TCID50) (1.0 ml of 1 × 106 intranasal [i.n.] doses plus 1.0 ml of 1 × 106 intratracheal [i.t.] doses) of each virus. The FluMist seasonal vaccine approved for humans is administered intranasally using prefilled sprayers containing 106.5 to 107.5 fluorescent focus units (FFU) in 0.2 ml. Blood samples and nasal/pharyngeal swabs were collected daily, and tracheal lavage fluid was collected every other day and on the day of necropsy. In each experiment, at least two AGMs were sacrificed 2 and 4 days postinfection (pi) and in some studies on day 7 pi. Tissue samples, including nasal turbinates, trachea, and lungs, were collected at necropsy. Samples from two areas (distal and proximal) of each upper and lower lobe were collected from each lung. Tissues were frozen immediately after harvest and stored at −80°C until they were processed for virus titration. Sample collection was modified as results of earlier experiments became available. For example, nasal washes were collected daily from animals inoculated with H6N1, H7N3, and H9N2 (wt and ca) viruses and samples from nasal and pharyngeal swabs were analyzed separately for H6N1 and H9N2 studies. Data on replication of the HPAI H5N1 wt virus were obtained from two separate experiments. The data for the shared time points from the two experiments were pooled for analysis. Brain and spleen samples were collected at necropsy from AGMs that received the H5N1 virus.
Viral titration.
Harvested tissues were homogenized in Leibovitz L-15 medium at 10% (wt/vol). The swabs were immersed in 1 ml of L-15 medium at room temperature for 5 min, and after the swab was removed, the samples were clarified by centrifugation at 2,500 rpm for 10 min. The nasal washes were collected by flushing each nostril with 1 ml of phosphate-buffered saline (PBS), and tracheal lavage fluid was obtained through intratracheal intubation/washes with 2 to 3 ml of PBS; these samples were also clarified by centrifugation. Clarified homogenates or secretion samples (swabs, nasal washes, or tracheal lavage fluid) were titrated on MDCK cell monolayers, and titers were expressed as TCID50 per gram or per ml, respectively, as previously described (32).
Immune responses and protective efficacy.
AGMs were immunized with one or two doses of 2 × 106 TCID50 ca vaccine virus 28 days apart. AGMs immunized with the H7N3 ca vaccine virus received only one dose. The monkeys were challenged with H5N1 wt or with H7N3 wt virus on day 59 or day 63 after the first inoculation, respectively. The challenge infection with H6N1 and H9N2 wt viruses was done on day 56 after the first vaccine dose. Tissues were harvested for virus titration when peak replication of the wt virus was anticipated, which was 2 days after challenge as indicated above. Sera were collected weekly and tested for hemagglutination inhibition (HAI) antibodies (Abs) and neutralizing Abs as previously described (32). Two-fold dilutions of heat-inactivated serum were tested in a microneutralization (MN) assay for the presence of antibodies that neutralized the replication of 100 TCID50 of wt viruses in MDCK cells, with four wells per dilution on a 96-well plate. The presence of viral cytopathic effect was read on days 3 and 4. The dilution of serum that completely prevented cytopathic effect in 50% of the wells was calculated by the Reed-Muench formula (43).
ELISA for IgA in nasal wash.
Enzyme-linked immunosorbent assays (ELISA) were performed as previously described (44). Briefly, plates were coated with baculovirus-expressed recombinant HA protein from the A/Vietnam/1203/04 (H5N1) virus (NR10510), A/teal/Hong Kong/W312/97 (H6N1) virus (NR-653), or A/chicken/G9/97 (H9N2) virus (NR-659) obtained through the National Institutes of Health Biodefense and Emerging Infectious Diseases Repository and used at 1 μg/ml (50 μl per well). Nasal wash samples in 2-fold serial dilutions were incubated on the plates at 4°C overnight. Bound antibodies were detected with biotinylated goat anti-monkey IgA (α-chain) and horseradish peroxidase (HRP)-conjugated streptavidin (Dako, Carpinteria, CA). Wells with an optical density (OD) of >0.2 after subtraction of background OD at 450 nm were considered to represent positive results.
Lectin histochemistry.
Lectin histochemistry using linkage-specific lectins was carried out essentially as described by Kuchipudi et al. (45) with some modifications. Lectins used in the current study included Sambucus nigra agglutinin (SNA) and Maackia amurensis I (MALI), MALII, or MAH agglutinins (all provided by Vector Laboratories, Burlingame, CA). Briefly, sections from formalin-fixed paraffin-embedded tissues from an uninfected AGM were cut at 5 μm thickness, deparaffinized in xylenes, and rehydrated through graded concentrations of ethanol. Tissue sections were microwave pretreated for 20 min using a citrate-based antigen unmasking solution (Vector Laboratories, Burlingame, CA), followed by a 1-h incubation at room temperature (RT) with fluorescein isothiocyanate (FITC)-labeled SNA or FITC-labeled MALI and biotinylated MALII lectin, each at a dilution of 1:100. Sections were washed in PBS containing 2% fish skin gelatin (FSG; Sigma) (PBS/FSG) and then incubated with streptavidin-Alexa Fluor 594 conjugate (Invitrogen, Grand Island, NY) for 30 min at RT. Nuclei were stained with DAPI (4′,6-diamidino-2-phenylindole) (Vector Laboratories, Burlingame, CA), and sections were mounted with ProLong Gold antifade reagent (Invitrogen, Grand Island, NY). Negative controls were performed by omitting primary reagents. To rule out nonspecific binding of the lectins, selected tissue sections were treated prior to microwaving and lectin staining with sialidase A (neuraminidase; New England BioLabs, Ipswich, MA) at 12.5 U/μl for 24 h at 37°C.
For double-label lectin and immunofluorescence studies, sections were processed as described above and incubated with FITC-labeled SNA for 1 h at RT. Sections were washed in PBS/FSG and then incubated with a primary Ab, either cytokeratin (AE1/AE3) or Von Willebrand factor (VWF), both provided by Abcam (Cambridge, MA), for 1 h at RT. Bound Ab was detected using a biotinylated anti-mouse secondary Ab for cytokeratin or an anti-rabbit secondary Ab for VWF (both supplied by Vector Laboratories, Burlingame, CA), followed by streptavidin-Alexa Fluor 594 conjugate (Invitrogen, Grand Island, NY). Nuclei were stained with DAPI, and sections were mounted with ProLong Gold antifade mounting medium (Invitrogen, Grand Island, NY). Images were captured using an Olympus BX51 microscope outfitted with an Olympus DP70 camera. Composite images were generated using Adobe Photoshop software.
Statistical analysis.
Virus titers in tissues and secretions in animals inoculated with wt and ca viruses as well as in animals inoculated with a sprayer and by the intranasal and intratracheal (i.n. plus i.t.) routes were compared using the Mann-Whitney U test. Comparisons were excluded from statistical analysis if the number of samples in the groups was ≤3 because of the small sample size.
RESULTS
Distribution of α2,3- and α2,6-linked sialic acid (SA) receptors in the respiratory tract of AGMs.
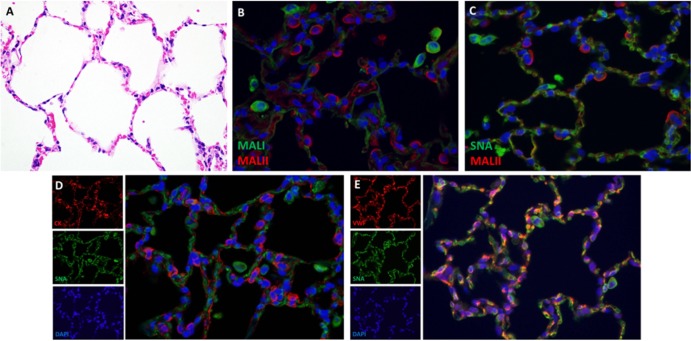
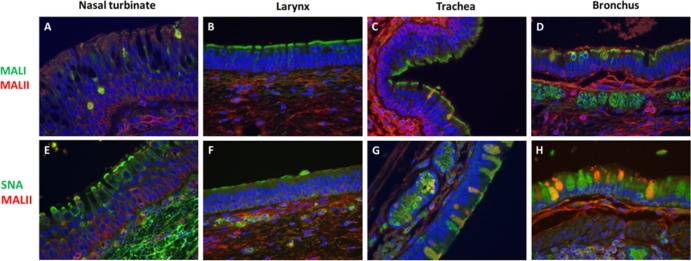
To evaluate the distribution of sialic acid receptors along the respiratory tract of AGMs, lectin histochemistry using Sambucus nigra agglutinin (SNA) and Maackia amurensis I (MALI) and Maackia amurensis II (MALII) agglutinins was carried out on formalin-fixed paraffin-embedded sections of nasal turbinates, larynx, trachea, and lung. SNA binds SAα2,6-Gal glycans. MALI and MALII lectins, which are widely used to identify SAα2,3-glycans, preferentially bind sulfated sugars (46).
MALI and MALII lectins.
In the nasal turbinates, patchy MALI staining was observed in the ciliated cells of the epithelium (Fig. 1A). In addition, there was strong staining of macrophages and blood vessels. Patchy MALI staining of ciliated epithelial cells continued into the larynx, trachea, and bronchi, though a majority of areas gave results that were completely negative. Representative areas of positive staining are shown in Fig. 1B to D. In the bronchi, MALI staining was also seen on macrophages and goblet cells. In the lung, MALI staining was present only on alveolar macrophages (Fig. 2B). In contrast to the binding of MALI to ciliated epithelial cells of the upper respiratory tract, binding of MALII was restricted to the submucosal connective tissue and goblet cells of submucosal glands and was not present along the surface of the ciliated epithelium (Fig. 1A and E). This pattern of lectin binding continued into the larynx and trachea, whereas in the bronchi, MALII binding was also present on ciliated epithelial cells (Fig. 1B to D and F to H). In the lungs, MALII binding was seen primarily on type II pneumocytes (Fig. 2B and C).
FIG 1.
Distribution of α2,3- and α2,6-linked sialic acid receptors in the respiratory tract of AGMs. Double-label lectin histochemistry demonstrates SNA binding to ciliated respiratory epithelial cells in the nasal turbinates, whereas MALI binding was most prominent on lining epithelial cells of the larynx, trachea, and bronchus. Original magnification, ×400.
FIG 2.
Distribution of α2,3- and α2,6-linked sialic acid receptors in the lungs of AGMs. (A) Hematoxylin and eosin (H&E) staining on lung showing normal alveolar architecture. (B) Double-label lectin histochemistry on lung shows MALII binding to type II pneumocytes in the alveoli. MALI binding was restricted to alveolar macrophages. (C) Double-label lectin histochemistry on lung showing SNA binding to alveolar macrophages and cells resembling vascular endothelial cells. (D and E) Lectin histochemistry combined with immunofluorescence shows that SNA-expressing cells in the alveoli are VWF-positive endothelial cells and not epithelial cells. Original magnification, ×400.
SNA lectin.
In the upper respiratory tract (nasal turbinates), SNA, which binds the SA α2,6-Gal glycans, was the prominent signal and was expressed along the apical surface of ciliated epithelial cells and in goblet cells of the submucosal glands (Fig. 1E). SA α2,6-Gal receptor expression was less prominent in the larynx and trachea, where patchy staining of epithelial cells and macrophages was present (Fig. 1F and G). In the lung, SNA binding was seen primarily in goblet cells of the main-stem bronchi, in alveolar macrophages, and in cells within the alveolar walls that were morphologically compatible with vascular endothelial cells (Fig. 2C). To further characterize the phenotype of these SA α2,6-Gal receptor-expressing cells in the alveolar walls and to discriminate between lectin binding of endothelial cells and of type I pneumocytes, lung sections were doubly labeled with SNA and either cytokeratin (type I pneumocytes) or Von Willebrand factor (VWF:endothelial cells). SNA colocalized exclusively with VWF, indicating that endothelial cells, and not type I pneumocytes, are the SA α2,6-Gal receptor-expressing cells in the alveolar walls (Fig. 2D and E).
Clinical signs in AGMs infected with avian influenza viruses.
Animals were observed and body weight and temperature were monitored daily. No signs of illness were observed in any of the animals that received any of the viruses, wild type (wt) or cold adapted (ca), and no significant change in weight or temperature was recorded (data not shown). However, the study design would preclude detection of late symptoms of disease.
Virus replication was assessed in secretion samples collected daily and tissue samples collected at necropsy. The data are presented for wt virus followed by ca virus in the text and in tables organized by type of sample.
Replication of H5N1 viruses.
The H5N1 wt virus replicated efficiently in the upper and lower respiratory tract of AGMs (Tables 1 and 2). Virus titers in the nasal turbinates and trachea peaked on day 2, though the titers in individual animals ranged from 102.0 to 106.5 TCID50/g. The titer of virus in nasal/pharyngeal swabs and tracheal lavage fluid was highest on day 1 (103.5 TCID50/ml in nasal/pharyngeal swab samples and 103.6 TCID50/ml in tracheal lavage fluid) (Table 2) and gradually decreased, but the titer was detectable until day 7 postinfection (pi; data not shown). High titers of virus were detected in the lungs, with average titers of 105.2, 104.3, and 102.2 TCID50/g on days 2, 4 and 7, respectively (Table 1). Virus was not detected in the spleen or brain of any AGM infected with the H5N1 wt virus (data not shown).
TABLE 1.
Replication of H5N1 and H7N3 wt and ca viruses in the respiratory tissues of African green monkeysa
| Virus | Day pi | Nasal turbinates |
Trachea |
Lung |
|||
|---|---|---|---|---|---|---|---|
| No. of culture-positive AGMs/total no. of AGMsb | Individual or mean titer(s) ± SEc | No. of culture-positive AGMs/total no. of AGMsb | Individual or mean titer(s) ± SEc | No. of culture-positive AGMs/total no. of AGMsb | Individual or mean titer(s) ± SEc | ||
| H5N1 wt | 2 | 4/4 | 5.2 ± 0.4 | 4/4 | 3.7 ± 0.6 | 4/4 | 5.2 ± 0.4 |
| 4 | 1/4 | 2.5 | 4/4 | 3.5 ± 0.8 | 4/4 | 4.3 ± 0.5 | |
| 7 | 1/2 | 3.0 | 2/2 | 2.2, 1.7 | 2/2 | 2.0, 2.3 | |
| H5N1 ca | 2 | 2/2 | 3.7, 4.4 | 0/2 | ≤1.5 | 2/2 | 1.6, 1.6 |
| 4 | 1/2 | 5.9 | 0/2 | ≤1.5 | 0/2 | ≤1.5 | |
| 7 | 0/2 | ≤1.5 | 0/2 | ≤1.5 | 0/2 | ≤1.5 | |
| H7N3 wt | 2 | 2/2 | 2.7, 4.4 | 2/2 | 5.2, 5.4 | 2/2 | 5.5, 6.6 |
| 4 | 2/2 | 3.0, 3.4 | 2/2 | 5.3, 6.7 | 2/2 | 3.7, 5.3 | |
| H7N3 ca (expt 1) | 2 | 0/2 | ≤1.5 | 0/2 | ≤1.5 | 0/2 | ≤1.5 |
| 4 | 0/2 | ≤1.5 | 0/2 | ≤1.5 | 0/2 | ≤1.5 | |
| H7N3 ca (expt 2) | 2 | 4/4 | 4.3 ± 0.6 | 1/4 | 2.0 | NDd | ND |
wt, wild type; ca, cold adapted.
Data represent numbers of AGMs with detectable virus titer (>1.5 log10 TCID50/g).
Titers are expressed as log10 TCID50/g; individual titers are presented in italics if only one or two AGMs were culture positive; mean titers are presented if more than three animals were culture positive. SE, standard error.
ND, not done.
TABLE 2.
Recovery of H5N1 and H7N3 wt and ca viruses from nasal and pharyngeal swabs and respiratory tract secretionsa
| Virus | Day pi | Nasal and pharyngeal swab |
Tracheal lavage fluid |
Nasal wash |
|||
|---|---|---|---|---|---|---|---|
| No. of culture-positive AGMs/total no. of AGMsb | Individual or mean titer(s) ± SEc | No. of culture-positive AGMs/total no. of AGMsb | Individual or mean titer(s) ± SEc | No. of culture-positive AGMs/total no. of AGMsb | Individual or mean titer(s) ± SEc | ||
| H5N1 wt | 1 | 10/10 | 3.5 ± 0.5 | 10/10 | 3.6 ± 0.5 | NDd | ND |
| 2 | 8/10 | 3.5 ± 0.5 | 10/10 | 2.9 ± 0.4 | |||
| 3 | 3/6 | 2.5 ± 0.5 | 5/6 | 2.9 ± 0.3 | |||
| 4 | 6/6 | 2.1 ± 0.5 | 6/6 | 3.5 ± 0.3 | |||
| H5N1 ca | 1 | 0/6 | ≤0.5 | 0/6 | ≤0.5 | ND | ND |
| 2 | 0/6 | ≤0.5 | 0/6 | ≤0.5 | |||
| 3 | 0/4 | ≤0.5 | 0/4 | ≤0.5 | |||
| 4 | 0/4 | ≤0.5 | 0/4 | ≤0.5 | |||
| H7N3 wt | 1 | 4/4 | 4.6 ± 0.3 | ND | ND | 2/4 | 1.0, 1.5 |
| 2 | 4/4 | 4.6 ± 0.3 | 2/2 | 3.2, 4.4 | 4/4 | 2.9 ± 0.6 | |
| 3 | 2/2 | 4.4, 4.4 | ND | ND | 1/2 | 4.4 | |
| 4 | 2/2 | 3.4, 3.7 | 1/2 | 1.0 | 1/2 | 1.5 | |
| H7N3 ca | 1 | 2/4 | 3.0, 3.0 | ND | ND | 1/4 | 1.5 |
| 2 | 4/4 | 3.9 ± 0.3 | 0/2 | ≤0.5 | 4/4 | 1.7 ± 0.2 | |
| 3 | 2/2 | 2.7, 4.0 | ND | ND | 2/2 | 2.7, 3.2 | |
| 4 | 1/2 | 1.5 | 0/2 | ≤0.5 | 1/2 | 3.0 | |
wt, wild type; ca, cold adapted.
Data represent numbers of AGMs with detectable virus titer (>0.5 log10 TCID50/ml).
Titers are expressed as log10 TCID50/g; individual titers are presented in italics if only one or two AGMs were culture positive; mean titers are presented if more than three animals were culture positive. SE, standard error.
ND, not done.
Among animals infected with the H5N1 ca virus, a relatively high titer of virus (∼103.7 to ∼105.9 TCID50/g) was detected in nasal turbinate tissues on day 2 pi and in one of two animals on day 4 pi (Table 1). Virus was not detected in nasal/pharyngeal swabs. There was no detectable virus in the trachea and a low titer of virus (101.6 TCID50/g) was detected in the lungs on day 2 pi (Table 1). Thus, the H5N1 wt virus replicated well in the upper and lower respiratory tract, while the H5N1 ca virus replicated efficiently only in the nasal turbinates. Interestingly, although the H5N1 ca virus was detected in nasal turbinate tissue, it was not detected in nasal/pharyngeal swabs (Table 2). The difference in virus titers in nasal/pharyngeal swabs and tracheal lavage fluid between H5N1 wt virus- and H5N1 ca virus-infected animals was statistically significant (P < 0.05).
Replication of H7N3 viruses.
The H7N3 wt virus was detected in both upper and lower respiratory tissues collected from all AGMs (Tables 1 and 2). The mean virus titers were 103.5 TCID50/g and 103.2 TCID50/g in nasal turbinates and 105.3 TCID50/g and 106.0 TCID50/g in the trachea on days 2 and 4 pi, respectively. Virus was also detected in secretions, including nasal/pharyngeal swabs, nasal washes, and tracheal lavage fluid (Table 2). The mean titers in the lungs were 106.1 TCID50/g and 104.5 TCID50/g on days 2 and 4, respectively (Table 1).
In contrast, the H7N3 ca virus was initially not detected in any of the respiratory tract tissue samples (Table 1). However, the virus was detected in nasal/pharyngeal swabs and nasal wash of all animals at titers of ∼102.7 to ∼103.9 TCID50/ml and ∼101.7 to ∼102.7 TCID50/ml, respectively, on days 2 and 3 postinfection (Table 2). Due to the small number of animals we tested, the possibility of sampling problems could not be excluded. Therefore, we repeated the study of the H7N3 ca virus in 4 additional AGMs. In addition to nasal turbinates and trachea, additional respiratory tissues, including those of nasal passages, conjunctiva, nasopharynx, lingual tonsil, oropharynx, laryngopharynx, larynx, and esophagus, were collected. Lung tissue was not collected in this study. H7N3 ca virus was detected in nasal turbinates of all four AGMs in this study with a range of ∼102 to ∼105.2 TCID50/g. Virus was also detected in other tissues, but a higher titer of virus and a more frequent presence of virus was noted in upper respiratory tract tissues, including conjunctiva (2 of 4 [2/4] AGMs), nasopharynx (3/4), lingual tonsil (3/4), oropharynx (3/4), laryngopharynx (2/4), larynx (1/4), esophagus (1/4), upper trachea (1/4), middle trachea (1/4), and lower trachea (1/4) (data not shown).
In summary, the H7N3 wt virus replicated well in upper and lower respiratory tract tissues and was present in respiratory secretions. The H7N3 ca virus was detected only in the upper respiratory tract, including nasal turbinates as well as nasal/pharyngeal swabs and nasal washes, but not in the lungs or tracheal lavage fluid.
Replication of H6N1 viruses.
As in the second experiment with the H7N3 ca virus, in the study of H6N1 AI virus replication, we collected samples from the pharynx and larynx for virus titration and processed the pharyngeal and nasal swabs separately instead of combining them. The H6N1 wt virus showed the most efficient replication among the AI viruses we had tested. High titers of virus ranging from 104.0 to 105.5 TCID50/g were recovered from the upper and lower respiratory tract tissues from all AGMs on days 2 and 4 (Table 3). Virus was also found in respiratory secretions, with peak titers on day 2 of 102.9 (nasal wash) to 103.8 (tracheal lavage fluid) TCID50/ml and recovery rates of 87.5% to 100% (Table 4).
TABLE 3.
Replication of H6N1and H9N2 wt and ca viruses in respiratory tissues of African green monkeysa
| Virus | Day pi | Nasal turbinates |
Pharynx |
Larynx |
Trachea |
Lung |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of culture-positive AGMs/total no. of AGMsb | Individual or mean titer(s) ± SEc | No. of culture-positive AGMs/total no. of AGMsb | Individual or mean titer(s) ± SEc | No. of culture-positive AGMs/total no. of AGMsb | Individual or mean titer(s) ± SEc | No. of culture-positive AGMs/total no. of AGMsb | Individual or mean titer(s) ± SEc | No. of culture-positive AGMs/total no. of AGMsb | Individual or mean titer(s) ± SEc | ||
| H6N1 wt | 2 | 4/4 | 5.6 ± 0.3 | 4/4 | 5.4 ± 0.9 | 4/4 | 5.0 ± 0.6 | 4/4 | 5.2 ± 0.5 | 4/4 | 4.5 ± 0.4 |
| 4 | 4/4 | 5.5 ± 0.7 | 4/4 | 5.7 ± 0.8 | 4/4 | 5.0 ± 0.5 | 4/4 | 5.1 ± 0.5 | 4/4 | 4.0 ± 0.3 | |
| H6N1 ca | 2 | 2/4 | 2, 4.3 | 0/4 | ≤1.5 | 0/4 | ≤1.5 | 0/4 | ≤1.5 | 0/4 | ≤1.5 |
| 4 | 1/4 | 2.0 | 0/4 | ≤1.5 | 0/4 | ≤1.5 | 0/4 | ≤1.5 | 0/4 | ≤1.5 | |
| H9N2 wt | 2 | 1/4 | 2.5 | 2/4 | 3.7, 5.5 | 2/4 | 2.5, 4.2 | 2/4 | 4.4, 3.7 | 4/4 | 2.9 ± 0.1 |
| 4 | 1/4 | 3.4 | 1/4 | 4.2 | 2/4 | 4.2, 3.2 | 2/4 | 3.7, 2.0 | 4/4 | 2.9 ± 0.4 | |
| H9N2 ca | 2 | 0/4 | ≤1.5 | 0/4 | ≤1.5 | 0/4 | ≤1.5 | 0/4 | ≤1.5 | 0/4 | ≤1.5 |
| 4 | 1/4 | 4.2 | 0/4 | ≤1.5 | 0/4 | ≤1.5 | 0/4 | ≤1.5 | 0/4 | ≤1.5 | |
wt, wild type; ca, cold adapted.
Data represent numbers of AGMs with detectable virus titer (>1.5 log10 TCID50/g).
Titers are expressed as log10 TCID50/g; individual titers are presented in italics if only one or two AGMs were culture positive; mean titers are presented if more than three animals were culture positive. SE, standard error.
TABLE 4.
Recovery of H6N1 and H9N2 wt and ca viruses from swabs and respiratory tract secretionsa
| Virus | Day pi | Nasal swab |
Pharyngeal swab |
Tracheal lavage fluid |
Nasal wash |
||||
|---|---|---|---|---|---|---|---|---|---|
| No. of culture-positive AGMs/total no. of AGMsb | Individual or mean titer(s) ± SEc | No. of culture-positive AGMs/total no. of AGMsb | Individual or mean titer(s) ± SEc | No. of culture-positive AGMs/total no. of AGMsb | Individual or mean titer(s) ± SEc | No. of culture-positive AGMs/total no. of AGMsb | Individual or mean titer(s) ± SEc | ||
| H6N1 wt | 1 | 1/8 | 1.0 | 7/8 | 2.5 ± 1.3 | 8/8 | 3.8 ± 1.2 | 4/8 | 2.0 ± 0.9 |
| 2 | 7/8 | 3.5 ± 1.5 | 7/8 | 3.6 ± 0.8 | 8/8 | 3.8 ± 1.3 | 7/8 | 2.9 ± 1.6 | |
| 3 | 3/4 | 3.0 ± 2.0 | 3/4 | 3.6 ± 1.1 | 3/4 | 3.5 ± 1.7 | 3/4 | 3.9 ± 0.7 | |
| 4 | 3/4 | 4.1 ± 0.8 | 2/4 | 5.0 ± 0.4 | 3/4 | 4.8 ± 0.6 | 3/4 | 2.6 ± 1.1 | |
| H6N1 ca | 1 | 0/8 | ≤0.5 | 0/8 | ≤0.5 | 0/8 | ≤0.5 | 0/8 | ≤0.5 |
| 2 | 0/8 | ≤0.5 | 0/8 | ≤0.5 | 0/8 | ≤0.5 | 0/8 | ≤0.5 | |
| 3 | 0/4 | ≤0.5 | 0/4 | ≤0.5 | 0/4 | ≤0.5 | 0/4 | ≤0.5 | |
| 4 | 0/4 | ≤0.5 | 0/4 | ≤0.5 | 0/4 | ≤0.5 | 0/4 | ≤0.5 | |
| H9N2 wt | 1 | 0/8 | ≤0.5 | 1/8 | 4.2 | 6/8 | 3.9 ± 0.4 | 0/8 | ≤0.5 |
| 2 | 0/8 | ≤0.5 | 1/8 | 4.7 | 3/8 | 4.0 ± 0.3 | 0/8 | ≤0.5 | |
| 3 | 0/4 | ≤0.5 | 0/4 | ≤0.5 | 2/4 | 4.5, 4.4 | 1/4 | 4.2 | |
| 4 | 2/4 | 4.7, 3.4 | 2/4 | 4.7, 4.7 | 2/4 | 1.0, 5.0 | 1/4 | 5.2 | |
| H9N2 ca | 1 | 0/8 | ≤0.5 | 0/8 | ≤0.5 | 0/8 | ≤0.5 | 0/8 | ≤0.5 |
| 2 | 0/8 | ≤0.5 | 0/8 | ≤0.5 | 0/8 | ≤0.5 | 0/8 | ≤0.5 | |
| 3 | 0/4 | ≤0.5 | 0/4 | ≤0.5 | 0/4 | ≤0.5 | 0/4 | ≤0.5 | |
| 4 | 0/4 | ≤0.5 | 0/4 | ≤0.5 | 0/4 | ≤0.5 | 0/4 | ≤0.5 | |
wt, wild type; ca, cold adapted.
Data represent numbers of AGMs with detectable virus titer (>0.5 log10 TCID50/ml).
Titers are expressed as log10TCID5/g; individual titers are presented in italics if only one or two AGMs were culture positive; mean titers are presented if more than three animals were culture positive. SE, standard error.
The H6N1 ca virus was detected in the nasal turbinates of only 50% (day 2) and 25% (day 4) of AGMs at titers of 102.0 to 104.0 TCID50/g (Table 3). Virus was not recovered from any other tissues or respiratory secretions (Table 4). Thus, the replication pattern of the H6N1 ca virus was similar to that of the H5N1 ca virus. The difference in virus titers in all tissues and secretions between H6N1 wt virus- and H6N1 ca virus-infected animals was statistically significant (P < 0.05).
Replication of H9N2 viruses.
The H9N2 wt virus replicated poorly in the upper respiratory tract tissue samples compared to the other AI viruses we had tested. Virus was recovered from nasal turbinates, pharynx, larynx, and trachea at titers ranging 102.5 to 104.4 TCID50/g from only 25% to 50% of the animals (Table 3). The detection of virus in respiratory secretions was sporadic (Table 4). Virus was detected in 2 of 4 AGMs on day 4 in nasal swabs and in only 1 of 4 AGMs on days 3 and 4 (in the same animal) in nasal wash, while virus was recovered from the tracheal lavage fluid of 37.5% to 75% of animals that received the virus. Virus was detected in the lungs of all AGMs, with an average virus titer of 102.9 TCID50/g (Table 3).
The H9N2 ca virus was detected in the nasal turbinates of only 1 of 4 AGMs on day 2 at a titer of 104.2 TCID50/g (Table 3). Virus was not recovered from any other tissues or respiratory secretions (Table 4). With the exception of the lung samples, the difference in virus titers between H9N2 wt virus- and H9N2 ca virus-infected animals was not statistically significant (P > 0.05).
In summary, most of the wt AI viruses tested replicated efficiently in the respiratory tract of AGMs. The H9N2 wt virus replicated less efficiently than the other AI viruses in respiratory tract tissues other than the lung. On the other hand, replication of the ca vaccine viruses was limited to the upper respiratory tract and was moderately to highly restricted in titer. In this regard, the findings in AGMs were consistent with the clinical experience with these vaccine candidates. Although the immunogenicity of the vaccine viruses has been evaluated in humans, the efficacy of pandemic influenza virus vaccines cannot be assessed in humans. Therefore, we were particularly interested in determining whether the low level of vaccine virus replication was sufficient to immunize and protect AGMs from challenge with the wt viruses.
Immunogenicity and protective efficacy of the H5N1, H6N1, H7N3, and H9N2 ca vaccine viruses in AGMs.
In order to assess the immunogenicity and efficacy of one or two doses of the H5N1 ca vaccine, two groups of three AGMs were inoculated with 2 × 106 TCID50 H5N1 ca virus delivered in 1 ml each intratracheally and intranasally (i.n. plus i.t.). This dose is consistent with doses used in other studies of viral replication in NHPs (47, 48). One group of AGMs received a second dose of vaccine 28 days after the first dose. A single dose of H5N1 ca vaccine did not elicit a serum HAI Ab or neutralizing Ab response by day 59. However, all three AGMs that received two doses of H5N1 ca vaccine developed HAI Abs (at titers of 80, 160, and 320) and neutralizing Abs (403, 508, and 640) 1 week after the second dose of vaccine (day 35; data not shown). The Ab titers peaked on day 42 (Table 5) and decreased somewhat by the day of challenge (day 59). H5 HA-specific IgA antibody was detected in nasal washes at dilutions of between 1:2 and 1:16 of three of four or all four AGMs that received one dose or two doses of H5N1 ca vaccine, respectively (data not shown). The protective efficacy of the H5N1 ca vaccine virus against H5N1 wt virus challenge was evaluated at necropsy 2 days after challenge. High titers of challenge virus (∼104.2 to ∼106.7 TCID50/g) were detected in the trachea and lungs of the mock-immunized AGMs (Table 5). Virus was not detected in any respiratory tissues or secretion samples from the AGMs that received two doses of the H5N1 ca vaccine virus. In contrast, one dose of vaccine did not prevent challenge virus replication in respiratory tissues; a high titer of challenge virus was detected in the lungs of all three animals, with titers of 104.3, 104.4, and 107.1 TCID50/g, respectively. Challenge virus was also detected in nasal/pharyngeal swabs and/or tracheal lavage samples of the AGMs that were subjected to mock immunization or received a single dose of H5N1 ca vaccine.
TABLE 5.
Immunogenicity and protective efficacy of H5N1 and H7N3 ca vaccines in AGMsa
| Vaccine/no. of doses | Challenge virus | AGM no.b | Serum Ab response |
Titer of challenge virus in respiratory tissues(log10 TCID50/g) |
Titer of challenge virus in swabs and lavage fluid(log10 TCID50/ml) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| HAI |
MN |
||||||||||
| Day 42c | Day of challenged | Day 42e | Day of challenge | Nasal turbinates | Trachea | Lung | Nasal/pharyngeal swab | Tracheal lavage fluid | |||
| Mock/1 | H5N1 wt | H5-M 1 | <20 | <20 | <20 | <20 | ≤1.5 | 4.2 | 6.6 | ≤1.5 | ≤1.5 |
| H5-M 2 | <20 | <20 | <20 | <20 | 4.4 | 5.4 | 5.5 | 2.7 | 3.2 | ||
| H5-M 3 | <20 | <20 | <20 | <20 | 3.4 | 6.7 | 5.8 | 4.2 | ≤1.5 | ||
| H5N1 ca/1 | H5N1 wt | H5-1D 1 | <20 | <20 | <20 | <20 | ≤1.5 | ≤1.5 | 4.4 | ≤0.5 | 1.5 |
| H5-1D 2 | <20 | <20 | <20 | <20 | ≤1.5 | 3.7 | 7.1 | 3.5 | 3.7 | ||
| H5-1D 3 | <20 | <20 | <20 | <20 | 2.5 | 4.2 | 4.3 | ≤0.5 | 3.0 | ||
| H5N1 ca/2 | H5N1 wt | H5-2D 1 | 1280 | 320 | 1810 | 905 | ≤1.5 | ≤1.5 | ≤1.5 | ≤0.5 | ≤0.5 |
| H5-2D 2 | 80 | 20 | 254 | 113 | ≤1.5 | ≤1.5 | ≤1.5 | ≤0.5 | ≤0.5 | ||
| H5-2D 3 | 640 | 160 | 1613 | 226 | ≤1.5 | ≤1.5 | ≤1.5 | ≤0.5 | ≤0.5 | ||
| Mock/1 | H7N3 wt | H7-M | <20 | <20 | <20 | <20 | ≤1.5 | 5.7 | 4.2 | 4.0 | 4.4 |
| H7N3 ca/1 | H7N3 wt | H7-1D 1 | 40 | 40 | 81 | 256 | ≤1.5 | ≤1.5 | ≤1.5 | ≤0.5 | ≤0.5 |
| H7-1D 2 | 20 | 20 | 102 | 128 | ≤1.5 | ≤1.5 | ≤1.5 | 3.37 | 4.0 | ||
| H7-1D 3 | 80 | 80 | 162 | 362 | <1.5 | ≤1.5 | ≤1.5 | ≤0.5 | ≤0.5 | ||
ca, cold adapted.
AGM numbers are expressed as follows: subtype of vaccine (H5, H5N1 ca vaccine; H7, H7N3 ca vaccine)-number of doses (1D, one dose; 2D, two doses; M, mock [L15 medium]) followed by animal identification number.
The HAI assay was performed using 1% horse red blood cells, and titers are expressed as the highest dilution of serum that inhibited agglutination of 8 hemagglutination units (HAU) of virus. The lower limit of detection was 20. Antibody titers from individual animals are listed.
AGMs were challenged on day 59 with H5N1 wt virus and on day 63 with H7N3 wt virus. Serum samples from AGMs were collected before challenge infection. The lower limit of detection of virus in tissues was 1.5 log10 TCID50/g and in swabs and lavage fluid was 0.5 log10 TCID50/ml.
MN titers are expressed as the serum dilution that inhibited infectivity of 100 TCID50 of virus in a microneutralization assay using MDCK cells. The lower limit of detection was 20. Antibody titers from individual animals are listed.
On the basis of the results from the H5N1 ca vaccine efficacy study, we expected that two doses of H7N3 ca vaccine would also provide complete protection against challenge infection with H7N3 wt virus. Therefore, we investigated the correlation between the level of HAI or neutralizing Abs and the level of protection by evaluating the effect of only one dose of the H7N3 ca vaccine. All three AGMs immunized with a H7N3 ca virus developed HAI Abs and neutralizing Abs; the neutralizing Ab titers increased between day 42 and the day of challenge. The HAI Ab titers were lower than the neutralizing Ab titers and did not rise between day 42 and the day of challenge. The challenge virus replicated efficiently in the respiratory tissues and nasal swabs, washes, and tracheal lavage fluid of the mock-immunized animal. The AGMs with prechallenge neutralizing Ab titers of 256 and 362 and HAI Ab titers of 40 and 80 were completely protected from wt virus infection (Table 5). Challenge virus was detected in tracheal lavage fluid and nasal/pharyngeal swabs but not in tissue homogenates of the AGM with a prechallenge neutralizing Ab titer of 128 and an HAI Ab titer of 20. Thus, the level of protection correlated with the level of neutralizing Abs and HAI Abs.
AGMs were immunized with 1 or 2 doses of H6N1 and H9N2 ca vaccine viruses. Similarly to the AGMs that received 2 doses of H5N1 ca vaccine, all AGMs that received 2 doses of H6N1 or H9N2 ca vaccines developed high levels of HAI Abs (∼160 to ∼1,280 or ∼80 to ∼640, respectively) and neutralizing Abs (∼254 to ∼1,280 or ∼101 to ∼1,016, respectively) on day 58. The vaccinated AGMs were completely protected from challenge virus replication in the respiratory tract except for a small amount of virus (102 TCID50/g) detected in the trachea of one AGM that received the H6N1 ca vaccine, and the difference in virus titer between animals that received 1 or 2 doses of H6N1 or H9N2 ca vaccine and mock-vaccinated animals was statistically significant (Table 6).
TABLE 6.
Immunogenicity and protective efficacy of H6N1 and H9N2 ca vaccines in AGMsa
| Vaccine/no. of doses | Challenge virus | AGM no.b | Serum Ab response |
Titer of challenge virus in respiratory tissues(log10 TCID50/g) |
Titer of challenge virus in swabs and lavage fluid(log10 TCID50/ml) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HAIc |
MNd |
Nasal turbinates | Trachea | Lung | Nasal swab | Pharyngeal swab | Tracheal lavage fluid | |||||
| Day 42 | Day 58e | Day 42 | Day 58e | |||||||||
| Mock/1 | H6N1 wt | H6-M 1 | <20 | <20 | <10 | <10 | ≤1.5 | 2.5 | 2.8 | ≤0.5 | ≤0.5 | 1.0 |
| H6-M 2 | <20 | <20 | <10 | <10 | 5.2 | 4.7 | 3.7 | 4.0 | ≤0.5 | 1.0 | ||
| H6-M 3 | <20 | <20 | <10 | <10 | 5.4 | 6.7 | 3.6 | 4.2 | 2.7 | 3.2 | ||
| H6-M 4 | <20 | <20 | <10 | <10 | 3.7 | 3.6 | 3.6 | 3.4 | ≤0.5 | 3.0 | ||
| H6N1 ca/1 | H6N1 wt | H6-1D 1 | 40 | 20 | 50 | 50 | ≤1.5 | ≤1.5 | ≤1.5 | 3.2 | ≤0.5 | ≤0.5 |
| H6-1D 2 | 80 | 40 | 50 | 226 | ≤1.5 | ≤1.5 | ≤1.5 | ≤0.5 | ≤0.5 | ≤0.5 | ||
| H6-1D 3 | <20 | <20 | 28 | <10 | ≤1.5 | ≤1.5 | ≤1.5 | ≤0.5 | ≤0.5 | ≤0.5 | ||
| H6-1D 4 | <20 | <20 | 32 | 25 | ≤1.5 | ≤1.5 | ≤1.5 | ≤0.5 | ≤0.5 | ≤0.5 | ||
| H6N1 ca/2 | H6N1 wt | H6-2D 1 | 1280 | 1280 | 2560 | 1016 | ≤1.5 | ≤1.5 | ≤1.5 | ≤0.5 | ≤0.5 | ≤0.5 |
| H6-2D 2 | 160 | 160 | 453 | 254 | ≤1.5 | ≤1.5 | ≤1.5 | ≤0.5 | ≤0.5 | ≤0.5 | ||
| H6-2D 3 | 320 | 160 | 905 | 453 | ≤1.5 | ≤1.5 | ≤1.5 | ≤0.5 | ≤0.5 | ≤0.5 | ||
| H6-2D 4 | 1280 | 640 | 2560 | 1280 | ≤1.5 | 2 | ≤1.5 | ≤0.5 | ≤0.5 | ≤0.5 | ||
| Mock/1 | H9N2 wt | H9-M 1 | <20 | <20 | <10 | <10 | ≤1.5 | 5.2 | 2.4 | 1.0 | 1.0 | 2.7 |
| H9-M 2 | <20 | <20 | <10 | <10 | ≤1.5 | 2.5 | 3.0 | ≤0.5 | ≤0.5 | 1.0 | ||
| H9-M 3 | <20 | <20 | <10 | <10 | 6.0 | 2.0 | 3.6 | 3.2 | 1.0 | 3.4 | ||
| H9-M 4 | <20 | <20 | <10 | <10 | ≤1.5 | 4.0 | 3.4 | ≤0.5 | 2.4 | 4.0 | ||
| H9N2 ca/1 | H9N2 wt | H9-1D 1 | <20 | <20 | 50 | 32 | ≤1.5 | ≤1.5 | 1.6 | ≤0.5 | ≤0.5 | ≤0.5 |
| H9-1D 2 | <20 | <20 | 25 | 28 | ≤1.5 | ≤1.5 | 2.3 | ≤0.5 | ≤0.5 | ≤0.5 | ||
| H9-1D 3 | 80 | 40 | 403 | 80 | ≤1.5 | ≤1.5 | ≤1.5 | ≤0.5 | ≤0.5 | ≤0.5 | ||
| H9-1D 4 | 80 | 40 | 113 | 113 | ≤1.5 | ≤1.5 | ≤1.5 | ≤0.5 | ≤0.5 | ≤0.5 | ||
| H9N2 ca/2 | H9N2 wt | H9-2D 1 | 640 | 640 | 403 | 1016 | ≤1.5 | ≤1.5 | ≤1.5 | ≤0.5 | ≤0.5 | ≤0.5 |
| H9-2D 2 | 160 | 80 | 320 | 101 | ≤1.5 | ≤1.5 | ≤1.5 | ≤0.5 | ≤0.5 | ≤0.5 | ||
| H9-2D 3 | 320 | 160 | 901 | 160 | ≤1.5 | ≤1.5 | ≤1.5 | ≤0.5 | ≤0.5 | ≤0.5 | ||
| H9-2D 4 | 160 | 80 | 453 | 113 | ≤1.5 | ≤1.5 | ≤1.5 | ≤0.5 | ≤0.5 | ≤0.5 | ||
ca, cold adapted.
AGM numbers are expressed as follows: subtype of vaccine (H6, H6N1 ca vaccine; H9, H9N2 ca vaccine)-number of doses (1D, one dose; 2D, two doses; M, mock [L15 medium]) followed by animal identification number.
The HAI assay was performed using 1% horse red blood cells for H6N1 virus and 0.5% turkey blood cells for H9N2 virus, and titers are expressed as the highest dilution of serum that inhibited agglutination of 8 HAU of virus. The lower limit of detection was 20. Antibody titers from individual animals are listed.
MN titers are expressed as the serum dilution that inhibited infectivity of 100 TCID50 of virus in a microneutralization assay using MDCK cells. The lower limit of detection was 10. Antibody titers from individual animals are listed.
AGMs were challenged on day 56 with wt viruses, and tissues and secretions were collected from AGMs 2 days after the challenge infection (day 58). The lower limit of detection of virus in tissues was 1.5 log10 TCID50/g and in swab and lavage fluid was 0.5 log10 TCID50/ml.
AGMs that received 1 dose of H6N1 ca vaccine developed undetectable to moderate levels (∼<10 to ∼226) of serum MN Abs, and 50% of the AGMs developed HAI Abs (∼20 to ∼40) on day 58. Challenge virus was not detected in the respiratory tissues of AGMs that received 1 dose of H6N1 ca virus vaccine though virus was recovered from the nasal swab of one AGM. H6 HA-specific IgA antibodies were not detected in nasal washes of H6N1 ca virus-vaccinated AGMs (data not shown).
All AGMs that received 1 dose of H9N2 ca virus vaccine developed moderate levels of neutralizing Abs (∼28 to ∼113) and 50% had low HAI Abs (40) on day 58. Challenge virus was isolated from the lungs of two AGMs that had received 1 dose of the H9N2 ca virus vaccine and developed low neutralizing Abs and no detectable HAI Ab titers. Thus, low or undetectable serum Ab levels of H9N2 Ab correlated with the lack of protection against challenge infection. IgA was also detectable in nasal wash in both groups that received 1 or 2 doses of vaccine, starting from day 28 postvaccination. H9 HA-specific IgA antibody was detected in nasal washes at dilutions of between 1:2 and 1:16 of all four AGMs that received one or two doses of H9N2 ca virus vaccine (data not shown).
Effect of different immunization routes on virus replication and immune responses.
A combination of intranasal and intratracheal (i.n. plus i.t.) administration of influenza viruses is commonly used in NHP models (35, 48, 49). However, seasonal and pandemic LAIVs are administered to humans as a nasal spray using a prefilled sprayer (12). In order to investigate this method of vaccine delivery, we anesthetized AGMs and immunized them with 0.2 ml H5N1 ca virus vaccine using a prefilled sprayer as is used in humans or with 1 ml each by i.n.-plus-i.t. administration. Two of three AGMs immunized by either method developed serum HAI Abs and neutralizing Abs after 2 doses of vaccine (Table 7). The Ab titers were slightly higher following i.n.-plus-i.t. administration than following the nasal spray administration. When AGMs immunized by the i.n.-plus-i.t. route were challenged with H5N1 wt virus, all three AGMs were protected from replication of wt virus in the upper respiratory tract and two of the three were protected from virus replication in the lungs. In contrast, two of three and one of three AGMs immunized with a sprayer were protected from challenge virus replication in the upper respiratory tract and in the lungs, respectively. However, the difference in virus titers in tissues or in antibody levels between animals that received vaccine administered by sprayer or i.n. plus i.t. was not statistically significant.
TABLE 7.
Immunogenicity and protective efficacy of H5N1 ca vaccine administered by sprayer or by intranasal and intratracheal routesa
| Vaccine/route | AGM no.b | Serum Ab response |
Titer of challenge virus in respiratory tissues(log10 TCID50/g) |
Titer of challenge virus in swab and lavage fluid (log10 TCID50/ml) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HAIc |
MNd |
Nasal turbinates | Trachea | Lung | Nasal swab | Pharyngeal swab | Nasal wash | Tracheal lavage fluid | ||||
| Day 42 | Day 49 | Day 42 | Day 49 | |||||||||
| Mock/sprayer | M1 | <20 | <20 | <20 | <20 | 6.0 | 7.4 | 7.0 | 4.7 | 3.4 | ≤0.5 | ≤0.5 |
| M2 | <20 | <20 | <20 | <20 | 6.4 | 6.2 | 6.0 | 5.0 | 4.2 | ≤0.5 | ≤0.5 | |
| Mock/intranasal + intratracheal | M3 | <20 | <20 | <20 | <20 | 5.4 | 7.2 | 7.6 | 4.2 | 4.2 | ≤0.5 | ≤0.5 |
| M4 | <20 | <20 | <20 | <20 | 5.7 | 6.0 | 6.5 | 3.2 | 4.2 | ≤0.5 | ≤0.5 | |
| H5N1ca/sprayer | S1 | 40 | 40 | 202 | 202 | ≤1.5 | ≤1.5 | ≤1.5 | 1.0 | 1.0 | ≤0.5 | ≤0.5 |
| S2 | <20 | <20 | 16 | <20 | ≤1.5 | ≤1.5 | 5.0 | 3.2 | 1.0 | ≤0.5 | ≤0.5 | |
| S3 | <20 | <20 | <20 | <20 | 2.0 | 6.2 | 5.6 | 1.0 | 3.37 | ≤0.5 | ≤0.5 | |
| H5N1 ca/intranasal + intratracheal | i.n.+i.t.1 | 160 | 160 | 905 | 508 | ≤1.5 | ≤1.5 | 1.6 | ≤0.5 | 3.2 | ≤0.5 | ≤0.5 |
| i.n.+i.t.2 | <20 | <20 | <20 | <20 | ≤1.5 | ≤1.5 | ≤1.5 | ≤0.5 | 4.2 | ≤0.5 | ≤0.5 | |
| i.n.+i.t.3 | 160 | 160 | 202 | 254 | ≤1.5 | ≤1.5 | ≤1.5 | ≤0.5 | 4.2 | ≤0.5 | ≤0.5 | |
ca, cold adapted.
M, mock; S, sprayer; i.n.+i.t., intranasal and intratracheal.
The HAI assay was performed using 0.5 % turkey red blood cells, and titers are expressed as the highest dilution of serum that inhibited agglutination of 8 HAU of virus. The lower limit of detection was 20. Antibody titers from individual animals are listed.
Neutralizing Ab titers are expressed as the serum dilution that inhibited infectivity of 100 TCID50 of virus in a microneutralization assay using MDCK cells. The lower limit of detection was 20. Antibody titers from individual animals are listed.
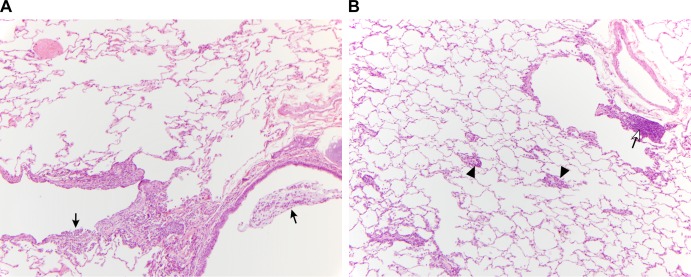
Although there was no gross pathological change detected in any animals, including the mock-immunized ones, mild pneumonia was observed in animals in all groups at a microscopic level following challenge infection. The pattern of pneumonia is a multifocal bronchointerstitial pneumonia centered primarily on terminal bronchioles with extension into the immediately adjacent alveoli. The pneumonia was generally milder in the i.n.-plus-i.t.-vaccinated group than in the sprayer-vaccinated and mock-immunized groups. In addition, there was more prominent and consistent lymphocytic perivascular cuffing noted in the i.n.-plus-i.t. group than in the sprayer group, in which the inflammatory response was predominantly neutrophilic (Fig. 3).
FIG 3.
Comparison of lung pathology results 2 days postchallenge with H5N1 wt virus in AGMs immunized i.n. with a sprayer versus i.n.-plus-i.t. immunization. (A) Section of lung from an intranasally (sprayer) vaccinated monkey (AGM7). There are low to moderate numbers of neutrophils and macrophages visible adjacent to a bronchus (lower right) and bronchiole (lower left). Black arrows indicate neutrophils within the lumen of these airways. Perivascular lymphocyte cuffing is absent. (B) Section of lung from an i.n.-plus-i.t.-vaccinated monkey (AGM8). Arrowheads indicate small-caliber blood vessels surrounded by low to moderate numbers of lymphocytes (perivascular lymphocyte cuffing). The open arrow indicates aggregated lymphocytes adjacent to a bronchiole (lymphocyte hyperplasia).
DISCUSSION
Mice and ferrets are the most commonly used animal models for influenza research, including the evaluation of influenza virus vaccines. However, in our experience of evaluating pandemic LAIVs generated against various subtypes of AI viruses, we found inconsistencies in the findings in preclinical studies in mice and ferrets and in studies in humans (12, 15, 29–34). Therefore, we sought an alternative animal model that would better mimic the findings in humans and in which we could explore the efficacy against wt virus challenge.
We made three important observations in AGMs related to infection with wt AI virus and the corresponding ca vaccine viruses representing 4 different subtypes. First, although infection was not associated with clinical illness in the 7 days of observation, the wt AI viruses replicated efficiently in the upper and lower respiratory tracts. Reports of clinical illness associated with influenza virus infection in NHPs vary from asymptomatic infection (viral replication without clinical illness) in cebus and owl monkeys (50), squirrel monkeys (51), and rhesus macaques (36) to clinical illness seen in pig-tailed macaques (48) and cynomolgus macaques (35, 47). Several clades of H5N1 wt viruses have been shown to replicate in the respiratory tract and induce respiratory disease in cynomolgus macaques (35, 47, 52). On the other hand, only mild symptoms, although to different degrees depending upon the virus strains, were reported in rhesus macaques (36, 53). In contrast, we did not see any signs of illness in AGMs infected with the A/Vietnam/1203/04 (VN04) clade 1 H5N1 virus although the virus replicated efficiently in the respiratory tract.
Second, while the replication of the ca LAIV vaccines was restricted to the upper respiratory tract, likely as a consequence of the temperature-sensitive phenotype of the vaccine viruses, the levels of recovery of the H5N1, H6N1, H7N3, and H9N2 ca viruses in tissue homogenates and secretions, including nasal and pharyngeal swabs, nasal washes, and tracheal lavage fluid, differed significantly. The H5N1, H6N1, and H9N2 ca viruses were isolated from nasal turbinate tissues but not from nasal and pharyngeal swabs or tracheal lavage fluid. In contrast, the H7N3 ca virus was recovered from nasal turbinate tissue but high titers of viruses were also detected in nasal/pharyngeal swabs and nasal washes. As reported previously, the H7N7 ca virus was also recovered from nasal/pharyngeal swabs (54).
The clinical trial subjects had daily nasal washes for a week after intranasal administration of each dose of vaccine. The H5N1 ca vaccine virus was not detected after the first dose of vaccine and was isolated from nasal washes from 2 of 19 subjects on a single day following the second dose of vaccine (12). The H6N1 ca virus was not detected in any subject, and the H9N2 ca virus was recovered by culture from only 2 of 39 subjects who received one dose of vaccine (29, 30). The H7N3 ca virus was recovered by culture from nasal washes of 24% of vaccine recipients, with peak titers ranging from 100.75 to 102.25 TCID50/ml (15). Although it is difficult to compare these data directly, the higher recovery rate of the H7N3 ca virus in human nasal wash samples correlates well with the high titer of virus in respiratory secretions of AGMs. With a few exceptions, tissue samples were generally more sensitive than secretion samples for detection of virus in AGMs. However, nasal wash or nasal swab samples are used to evaluate the replication of LAIVs in humans since it is not feasible to collect tissue samples.
The third interesting observation was that the low level of replication of the H5N1 ca virus in AGMs was sufficient to induce serum neutralizing Abs after two doses of vaccine and that the animals were fully protected from replication of the wt challenge virus. Although the level of neutralizing Abs prior to challenge ranged from 40 to 640, the AGMs were well protected, with no detectable virus in tissues or secretions regardless of Ab titer. In humans, the H5N1 ca vaccine virus was poorly immunogenic and only 1 (5%) of 21 subjects developed detectable neutralizing Abs after two doses of vaccine (12). When we compared the efficacies of the H5N1 ca virus vaccine delivered by different routes to anesthetized AGMs, higher immune responses were observed in AGMs that received vaccine by i.n.-plus-i.t. administration than in the group that received vaccine by nasal spray. However, nasal spray vaccine was more immunogenic in AGMs than in humans, though it is important to note that the AGMs were anesthetized for vaccination and that this may alter the delivery of the nasal spray. Interestingly, the characteristics of the inflammatory responses after challenge infection were slightly different between the animals vaccinated by sprayer and those vaccinated by i.n.-plus-i.t. administration. The lymphocytic and macrophage response noted in the lungs of i.n.-plus-i.t.-vaccinated animals was more prominent than that noted in the lungs of animals vaccinated by sprayer. On the other hand, neutrophils were predominantly present in the lungs of animals immunized with the sprayer. Thus, the route of immunization affected the outcome of vaccination. Overall, the data from our studies in AGMs indicate that a neutralizing Ab response was protective. A live attenuated vaccine against the A/Anhui/2/05 (clade 2.3) H5N1 virus was generated on the AA ca (AH/AAca) virus background and tested in Chinese-origin rhesus macaques (36). Macaques vaccinated with the AH/AAca virus developed both HAI Abs and neutralizing Abs 4 weeks after one dose of vaccine, and following two doses of vaccine, the monkeys were protected from replication of homologous and heterologous H5N1 wt challenge viruses. In contrast, we did not detect HAI Abs or neutralizing Abs in AGMs after 1 dose of the VN04 ca virus vaccine; only AGMs that received two doses of vaccine developed antibodies and were protected from challenge infection with wt virus. These differences may due to the virus strains used (clade 1 versus clade 2.3) or the susceptibilities of the two primate species to these viruses. Although the replication kinetics of the AH/AAca virus in rhesus macaques was not reported, it is possible that AH/AAca virus replicated more efficiently in rhesus macaques than the VN04 ca virus did in AGMs.
An important finding from this study is that the other subtypes of AI ca viruses tested also elicited protective immunity to wt challenge virus replication in AGMs. One dose of the H7N3 ca virus vaccine was sufficient to induce a robust neutralizing Ab response in AGMs, and prechallenge Ab titers correlated with the level of protective efficacy. Virus was not detected in any samples from AGMs with serum neutralizing Ab titers of 256 and 362, while 103 to 104 TCID50/ml of challenge virus was detected in the nasal swab and tracheal lavage fluid of the monkey with a neutralizing Ab titer of 128 (Table 5). AGMs immunized with H6N1 ca virus vaccine developed high titers of neutralizing Abs and HAI Abs after two doses of vaccine. On the other hand, despite rather poor replication of H9N2 ca virus compared to other subtypes of ca viruses, immune responses, including development of serum neutralizing Abs and HAI Abs, were comparable to those seen with H6N1 ca virus. The serum neutralizing Ab titers prior to the challenge infection were significantly lower with 1-dose vaccination with H6N1 ca virus (undetectable to 226) and H9N2 ca virus (28 to 113) vaccines than the titers seen with 1-dose vaccination with H7N3 ca virus vaccine. However, despite the relatively low serum Ab titer, challenge virus replication was not detected in AGMs that received 1 dose of H6N1 ca virus vaccine. On the other hand, despite similar Ab titers, challenge virus was detected in the lungs of two AGMs that received 1 dose of H9N2 ca virus vaccine (Table 6). Thus, the titers of neutralizing Ab that conferred protection from challenge with wt virus differed among the different subtypes, and there was a great variability in the immune responses elicited by the different subtypes of AI ca virus vaccines although they had similarly restricted replication profiles.
In humans, the H7N3 ca virus vaccine was moderately immunogenic and 48% of vaccine recipients developed a 4-fold rise in neutralizing Ab, 71% had serum IgA responses, and 33% had nasal wash IgA responses (15). None of the human subjects that received the H6N1 ca virus vaccine had a ≥4-fold response in neutralizing Abs or HAI Abs, but a ≥4-fold rise of serum IgG, serum IgA, or nasal wash IgA was seen in 29%, 24%, or 5% of vaccines, respectively (30). Interestingly, despite the poor replication, all of the human subjects who received the H9N2 ca virus vaccine developed immune responses measured by one or more methods (HAI, MN, or ELISA) (29). In previously seronegative subjects, 50% and 21% of the vaccinees exhibited a ≥4-fold rise of in the level of serum IgG and nasal wash IgA, respectively. Thus, the immune response to pandemic LAIVs was generally more robust in AGMs than in humans.
We found that the distribution of the types of SA receptors in the respiratory tract of AGMs was similar to that of humans. In humans, SAα2,6-Gal predominates in the upper respiratory tract epithelium, whereas SAα2,3-Gal or sulfated glycans are restricted to the lower respiratory tract, mainly in nonciliated cuboidal bronchiolar cells and type II pneumocytes; SAα2,6-Gal is also expressed in type I pneumocytes (55, 56). In AGMs, we found that the epithelium of the nasal turbinates exclusively expressed SAα2,6-Gal. Therefore, the ability of the AI viruses to replicate efficiently in the upper respiratory tract of AGMs was unexpected. The larynx and tracheal epithelial cells were stained by MALI (preferential binding to SAα2,3-Galβ1–4GlcNAc and 3-sulfoGalβ1–4GlcNAc) but not by MALII (which binds to SAα2,3-Galβ1–3GlcNAc as well as to SAα2,3-Galβ1–4GlcNAc). It has been suggested that different isoforms of SAα2,3-Gal receptors may be involved in binding of AI viruses (56–58) and that this may even vary among subtypes. In general, it was reported in previous studies that the pattern of SA receptor distribution correlated with the differential binding of avian and human viruses in different parts of the respiratory tree (55, 59). However, all the wt AI viruses tested in our study except the H9N2 virus replicated efficiently in the upper respiratory tract. Additional immunohistochemical analyses are needed to identify the specific cell types in which different subtypes of wt and ca AI viruses replicate. Interestingly, in the lower respiratory tract, SAα2,6-Gal receptors were mostly expressed in endothelial cells, whereas SAα2,3-Gal receptors were found in pneumocytes. SAα2,3-Gal receptor expression was seen on type II pneumocytes that were identified by their characteristic morphology. SAα2,6-Gal receptors have been identified on type I pneumocytes in humans (55, 57); however, identification of cells in these studies was based on cellular morphology and the distinction between endothelial cells and type I pneumocytes was not clearly demonstrated. The expression of SAα2,6-Gal receptors on endothelial cells was reported in other animal species, including dogs, cats, tigers, pigs, ferrets, chickens, and ducks (60). Although the expression of SAα2,6-Gal receptors on endothelial cells in alveoli could be unique to animals, it is possible that the SNA-positive cells that were identified as type I pneumocytes in humans could have included endothelial cells. Although we were not able to perform dual staining with MALII and endothelial or epithelial cell markers, elongated alveolar lining cells stained with MALII could be type I pneumocytes and/or endothelial cells. Glycan microarray analysis has been used to study the species specificity of influenza viruses (61–63). A recent study identified a wide diversity of glycans present in the human respiratory tract which can be used by influenza viruses and found that currently available glycan arrays do not represent the full spectrum of glycans that exist in the human respiratory tract (64).
In summary, the distribution of SAα2,3-Gal and SAα2,6-Gal receptors in the respiratory tract of AGMs was similar to that seen with humans. The wt AI viruses replicated efficiently in the respiratory tract of AGMs, while replication of the ca vaccine viruses was highly restricted and limited to the upper respiratory tract. The patterns and sites of ca virus replication differed among the different subtypes and mimicked the replication of the pandemic LAIVs that we observed in humans. However, the H5N1, H7N3, H6N1, H9N2, and H7N7 (54) pandemic LAIV vaccines were immunogenic in AGMs and a neutralizing Ab response was associated with protective efficacy in this model. In addition, we found that the immune responses and protective efficacy observed with i.n.-plus-i.t. inoculation of vaccine were comparable to those observed when the vaccine was administered intranasally with a sprayer as in humans. This model can be used to evaluate the efficacy of candidate LAIVs in the future.
ACKNOWLEDGMENTS
This research was performed as part of a Cooperative Research and Development Agreement (CRADA) between the Laboratory of Infectious Diseases, NIAID, and MedImmune and was supported in part by the Intramural Research Program of the NIH, NIAID.
We thank Anthony Cook and Brad Finneyfrock at Bioqual Inc., the staff of the NIH animal center at Poolesville, MD, and the Comprehensive Medicine Branch, and W. L. Shupert and the staff of the Rocky Mountain Veterinary Branch of NIAID, NIH, for excellent technical support in the animal studies. We also thank Rebecca Rosenke, Histopathology Laboratory of RML, NIAID, NIH, for her work on IHC staining.
Footnotes
Published ahead of print 7 May 2014
REFERENCES
- 1.Subbarao K, Klimov A, Katz J, Regnery H, Lim W, Hall H, Perdue M, Swayne D, Bender C, Huang J, Hemphill M, Rowe T, Shaw M, Xu X, Fukuda K, Cox N. 1998. Characterization of an avian influenza A (H5N1) virus isolated from a child with a fatal respiratory illness. Science 279:393–396. 10.1126/science.279.5349.393 [DOI] [PubMed] [Google Scholar]
- 2.Peiris JS, Yu WC, Leung CW, Cheung CY, Ng WF, Nicholls JM, Ng TK, Chan KH, Lai ST, Lim WL, Yuen KY, Guan Y. 2004. Re-emergence of fatal human influenza A subtype H5N1 disease. Lancet 363:617–619. 10.1016/S0140-6736(04)15595-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO. 19 February 2003, posting date Influenza A (H5N1) in Hong Kong Special Administrative Region of China. WHO, Geneva, Switzerland: http://www.who.int/csr/don/2003_2_19/en/ [Google Scholar]
- 4.WHO. 14 January 2004, posting date Avian influenza A(H5N1) in humans in Viet Nam and poultry in Asia - update. WHO, Geneva, Switzerland: http://www.who.int/csr/don/2004_01_14/en/ [Google Scholar]
- 5.WHO. 23 January 2004, posting date Avian influenza A (H5N1) in humans in Thailand - update 6. WHO, Geneva, Switzerland: http://www.who.int/csr/don/2004_01_23/en/ [Google Scholar]
- 6.WHO. 2013. Cumulative number of confirmed human cases for avian influenza A(H5N1) reported to WHO, 2003–2013. WHO, Geneva, Switzerland [Google Scholar]
- 7.Fouchier RA, Schneeberger PM, Rozendaal FW, Broekman JM, Kemink SA, Munster V, Kuiken T, Rimmelzwaan GF, Schutten M, Van Doornum GJ, Koch G, Bosman A, Koopmans M, Osterhaus AD. 2004. Avian influenza A virus (H7N7) associated with human conjunctivitis and a fatal case of acute respiratory distress syndrome. Proc. Natl. Acad. Sci. U. S. A. 101:1356–1361. 10.1073/pnas.0308352100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koopmans M, Wilbrink B, Conyn M, Natrop G, van der Nat Vennema HH, Meijer A, van Steenbergen J, Fouchier R, Osterhaus A, Bosman A. 2004. Transmission of H7N7 avian influenza A virus to human beings during a large outbreak in commercial poultry farms in the Netherlands. Lancet 363:587–593. 10.1016/S0140-6736(04)15589-X [DOI] [PubMed] [Google Scholar]
- 9.Butt KM, Smith GJ, Chen H, Zhang LJ, Leung YH, Xu KM, Lim W, Webster RG, Yuen KY, Peiris JS, Guan Y. 2005. Human infection with an avian H9N2 influenza A virus in Hong Kong in 2003. J. Clin. Microbiol. 43:5760–5767. 10.1128/JCM.43.11.5760-5767.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guo Y, Li J, Cheng X. 1999. Discovery of men infected by avian influenza A (H9N2) virus. Zhonghua Shi Yan He Lin Chuang Bing Du Xue Za Zhi 13:105–108 (In Chinese.) [PubMed] [Google Scholar]
- 11.Peiris M, Yuen KY, Leung CW, Chan KH, Ip PL, Lai RW, Orr WK, Shortridge KF. 1999. Human infection with influenza H9N2. Lancet 354:916–917. 10.1016/S0140-6736(99)03311-5 [DOI] [PubMed] [Google Scholar]
- 12.Karron RA, Talaat K, Luke C, Callahan K, Thumar B, Dilorenzo S, McAuliffe J, Schappell E, Suguitan A, Mills K, Chen G, Lamirande E, Coelingh K, Jin H, Murphy BR, Kemble G, Subbarao K. 2009. Evaluation of two live attenuated cold-adapted H5N1 influenza virus vaccines in healthy adults. Vaccine 27:4953–4960. 10.1016/j.vaccine.2009.05.099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bresson JL, Perronne C, Launay O, Gerdil C, Saville M, Wood J, Hoschler K, Zambon MC. 2006. Safety and immunogenicity of an inactivated split-virion influenza A/Vietnam/1194/2004 (H5N1) vaccine: phase I randomised trial. Lancet 367:1657–1664. 10.1016/S0140-6736(06)68656-X [DOI] [PubMed] [Google Scholar]
- 14.Treanor JJ, Campbell JD, Zangwill KM, Rowe T, Wolff M. 2006. Safety and immunogenicity of an inactivated subvirion influenza A (H5N1) vaccine. N. Engl. J. Med. 354:1343–1351. 10.1056/NEJMoa055778 [DOI] [PubMed] [Google Scholar]
- 15.Talaat KR, Karron RA, Callahan KA, Luke CJ, DiLorenzo SC, Chen GL, Lamirande EW, Jin H, Coelingh KL, Murphy BR, Kemble G, Subbarao K. 2009. A live attenuated H7N3 influenza virus vaccine is well tolerated and immunogenic in a Phase I trial in healthy adults. Vaccine 27:3744–3753. 10.1016/j.vaccine.2009.03.082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Couch RB, Patel SM, Wade-Bowers CL, Nino D. 2012. A randomized clinical trial of an inactivated avian influenza A (H7N7) vaccine. PLoS One 7:e49704. 10.1371/journal.pone.0049704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Atmar RL, Keitel WA, Patel SM, Katz JM, She D, El Sahly H, Pompey J, Cate TR, Couch RB. 2006. Safety and immunogenicity of nonadjuvanted and MF59-adjuvanted influenza A/H9N2 vaccine preparations. Clin. Infect. Dis. 43:1135–1142. 10.1086/508174 [DOI] [PubMed] [Google Scholar]
- 18.Lin J, Zhang J, Dong X, Fang H, Chen J, Su N, Gao Q, Zhang Z, Liu Y, Wang Z, Yang M, Sun R, Li C, Lin S, Ji M, Wang X, Wood J, Feng Z, Wang Y, Yin W. 2006. Safety and immunogenicity of an inactivated adjuvanted whole-virion influenza A (H5N1) vaccine: a phase I randomised controlled trial. Lancet 368:991–997. 10.1016/S0140-6736(06)69294-5 [DOI] [PubMed] [Google Scholar]
- 19.Leroux-Roels I, Leroux-Roels G. 2009. Current status and progress of prepandemic and pandemic influenza vaccine development. Expert Rev. Vaccines 8:401–423. 10.1586/erv.09.15 [DOI] [PubMed] [Google Scholar]
- 20.Chen GL, Subbarao K. 2009. Live attenuated vaccines for pandemic influenza. Curr. Top. Microbiol. Immunol. 333:109–132. 10.1007/978-3-540-92165-3_5 [DOI] [PubMed] [Google Scholar]
- 21.Nolan TM, Richmond PC, Skeljo MV, Pearce G, Hartel G, Formica NT, Hoschler K, Bennet J, Ryan D, Papanaoum K, Basser RL, Zambon MC. 2008. Phase I and II randomised trials of the safety and immunogenicity of a prototype adjuvanted inactivated split-virus influenza A (H5N1) vaccine in healthy adults. Vaccine 26:4160–4167. 10.1016/j.vaccine.2008.05.077 [DOI] [PubMed] [Google Scholar]
- 22.Levie K, Leroux-Roels I, Hoppenbrouwers K, Kervyn AD, Vandermeulen C, Forgus S, Leroux-Roels G, Pichon S, Kusters I. 2008. An adjuvanted, low-dose, pandemic influenza A (H5N1) vaccine candidate is safe, immunogenic, and induces cross-reactive immune responses in healthy adults. J. Infect. Dis. 198:642–649. 10.1086/590913 [DOI] [PubMed] [Google Scholar]
- 23.Leroux-Roels I, Borkowski A, Vanwolleghem T, Drame M, Clement F, Hons E, Devaster JM, Leroux-Roels G. 2007. Antigen sparing and cross-reactive immunity with an adjuvanted rH5N1 prototype pandemic influenza vaccine: a randomised controlled trial. Lancet 370:580–589. 10.1016/S0140-6736(07)61297-5 [DOI] [PubMed] [Google Scholar]
- 24.Belshe RB, Gruber WC, Mendelman PM, Cho I, Reisinger K, Block SL, Wittes J, Iacuzio D, Piedra P, Treanor J, King J, Kotloff K, Bernstein DI, Hayden FG, Zangwill K, Yan L, Wolff M. 2000. Efficacy of vaccination with live attenuated, cold-adapted, trivalent, intranasal influenza virus vaccine against a variant (A/Sydney) not contained in the vaccine. J. Pediatr. 136:168–175. 10.1016/S0022-3476(00)70097-7 [DOI] [PubMed] [Google Scholar]
- 25.Mendelman PM, Rappaport R, Cho I, Block S, Gruber W, August M, Dawson D, Cordova J, Kemble G, Mahmood K, Palladino G, Lee MS, Razmpour A, Stoddard J, Forrest BD. 2004. Live attenuated influenza vaccine induces cross-reactive antibody responses in children against an a/Fujian/411/2002-like H3N2 antigenic variant strain. Pediatr. Infect. Dis. J. 23:1053–1055. 10.1097/01.inf.0000143643.44463.b1 [DOI] [PubMed] [Google Scholar]
- 26.Clements ML, Betts RF, Tierney EL, Murphy BR. 1986. Serum and nasal wash antibodies associated with resistance to experimental challenge with influenza A wild-type virus. J. Clin. Microbiol. 24:157–160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kendal AP. 1997. Cold-adapted live attenuated influenza vaccines developed in Russia: can they contribute to meeting the needs for influenza control in other countries? Eur. J. Epidemiol. 13:591–609. 10.1023/A:1007327505862 [DOI] [PubMed] [Google Scholar]
- 28.Rudenko LG, Slepushkin AN, Monto AS, Kendal AP, Grigorieva EP, Burtseva EP, Rekstin AR, Beljaev AL, Bragina VE, Cox N, et al. 1993. Efficacy of live attenuated and inactivated influenza vaccines in schoolchildren and their unvaccinated contacts in Novgorod, Russia. J. Infect. Dis. 168:881–887. 10.1093/infdis/168.4.881 [DOI] [PubMed] [Google Scholar]
- 29.Karron RA, Callahan K, Luke C, Thumar B, McAuliffe J, Schappell E, Joseph T, Coelingh K, Jin H, Kemble G, Murphy BR, Subbarao K. 2009. A live attenuated H9N2 influenza vaccine is well tolerated and immunogenic in healthy adults. J. Infect. Dis. 199:711–716. 10.1086/596558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Talaat KR, Karron RA, Luke CJ, Thumar B, McMahon BA, Chen GL, Lamirande EW, Jin H, Coelingh KL, Kemble G, Subbarao K. 2011. An open label Phase I trial of a live attenuated H6N1 influenza virus vaccine in healthy adults. Vaccine 29:3144–3148. 10.1016/j.vaccine.2011.02.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Joseph T, McAuliffe J, Lu B, Vogel L, Swayne D, Jin H, Kemble G, Subbarao K. 2008. A live attenuated cold-adapted influenza A H7N3 virus vaccine provides protection against homologous and heterologous H7 viruses in mice and ferrets. Virology 378:123–132. 10.1016/j.virol.2008.05.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Suguitan AL, Jr, McAuliffe J, Mills KL, Jin H, Duke G, Lu B, Luke CJ, Murphy B, Swayne DE, Kemble G, Subbarao K. 2006. Live, attenuated influenza A H5N1 candidate vaccines provide broad cross-protection in mice and ferrets. PLoS Med. 3:e360. 10.1371/journal.pmed.0030360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen H, Matsuoka Y, Swayne D, Chen Q, Cox NJ, Murphy BR, Subbarao K. 2003. Generation and characterization of a cold-adapted influenza A H9N2 reassortant as a live pandemic influenza virus vaccine candidate. Vaccine 21:4430–4436. 10.1016/S0264-410X(03)00430-4 [DOI] [PubMed] [Google Scholar]
- 34.Chen Z, Santos C, Aspelund A, Gillim-Ross L, Jin H, Kemble G, Subbarao K. 2009. Evaluation of live attenuated influenza a virus h6 vaccines in mice and ferrets. J. Virol. 83:65–72. 10.1128/JVI.01775-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rimmelzwaan GF, Kuiken T, van Amerongen G, Bestebroer TM, Fouchier RA, Osterhaus AD. 2001. Pathogenesis of influenza A (H5N1) virus infection in a primate model. J. Virol. 75:6687–6691. 10.1128/JVI.75.14.6687-6691.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fan S, Gao Y, Shinya K, Li CK, Li Y, Shi J, Jiang Y, Suo Y, Tong T, Zhong G, Song J, Zhang Y, Tian G, Guan Y, Xu XN, Bu Z, Kawaoka Y, Chen H. 2009. Immunogenicity and protective efficacy of a live attenuated H5N1 vaccine in nonhuman primates. PLoS Pathog. 5:e1000409. 10.1371/journal.ppat.1000409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tolnay AE, Baskin CR, Tumpey TM, Sabourin PJ, Sabourin CL, Long JP, Pyles JA, Albrecht RA, Garcia-Sastre A, Katze MG, Bielefeldt-Ohmann H. 2010. Extrapulmonary tissue responses in cynomolgus macaques (Macaca fascicularis) infected with highly pathogenic avian influenza A (H5N1) virus. Arch. Virol. 155:905–914. 10.1007/s00705-010-0662-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kuiken T, Rimmelzwaan GF, Van Amerongen G, Osterhaus AD. 2003. Pathology of human influenza A (H5N1) virus infection in cynomolgus macaques (Macaca fascicularis). Vet. Pathol. 40:304–310. 10.1354/vp.40-3-304 [DOI] [PubMed] [Google Scholar]
- 39.Schaap-Nutt A, Higgins C, Amaro-Carambot E, Nolan SM, D'Angelo C, Murphy BR, Collins PL, Schmidt AC. 2011. Identification of human parainfluenza virus type 2 (HPIV-2) V protein amino acid residues that reduce binding of V to MDA5 and attenuate HPIV-2 replication in nonhuman primates. J. Virol. 85:4007–4019. 10.1128/JVI.02542-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bartlett EJ, Amaro-Carambot E, Surman SR, Newman JT, Collins PL, Murphy BR, Skiadopoulos MH. 2005. Human parainfluenza virus type I (HPIV1) vaccine candidates designed by reverse genetics are attenuated and efficacious in African green monkeys. Vaccine 23:4631–4646. 10.1016/j.vaccine.2005.04.035 [DOI] [PubMed] [Google Scholar]
- 41.Jin H, Cheng X, Traina-Dorge VL, Park HJ, Zhou H, Soike K, Kemble G. 2003. Evaluation of recombinant respiratory syncytial virus gene deletion mutants in African green monkeys for their potential as live attenuated vaccine candidates. Vaccine 21:3647–3652. 10.1016/S0264-410X(03)00426-2 [DOI] [PubMed] [Google Scholar]
- 42.McAuliffe J, Vogel L, Roberts A, Fahle G, Fischer S, Shieh WJ, Butler E, Zaki S, St Claire M, Murphy B, Subbarao K. 2004. Replication of SARS coronavirus administered into the respiratory tract of African Green, rhesus and cynomolgus monkeys. Virology 330:8–15. 10.1016/j.virol.2004.09.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Reed LJ, Muench H. 1938. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 27:493–497 [Google Scholar]
- 44.Chen GL, Lau YF, Lamirande EW, McCall AW, Subbarao K. 2011. Seasonal influenza infection and live vaccine prime for a response to the 2009 pandemic H1N1 vaccine. Proc. Natl. Acad. Sci. U. S. A. 108:1140–1145. 10.1073/pnas.1009908108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kuchipudi SV, Nelli R, White GA, Bain M, Chang KC, Dunham S. 2009. Differences in influenza virus receptors in chickens and ducks: implications for interspecies transmission. J. Mol. Genet. Med. 3:143–151. 10.4172/1747-0862.1000026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Geisler C, Jarvis DL. 2011. Effective glycoanalysis with Maackia amurensis lectins requires a clear understanding of their binding specificities. Glycobiology 21:988–993. 10.1093/glycob/cwr080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rimmelzwaan GF, Kuiken T, van Amerongen G, Bestebroer TM, Fouchier RA, Osterhaus AD. 2003. A primate model to study the pathogenesis of influenza A (H5N1) virus infection. Avian Dis. 47:931–933. 10.1637/0005-2086-47.s3.931 [DOI] [PubMed] [Google Scholar]
- 48.Baskin CR, García-Sastre A, Tumpey TM, Bielefeldt-Ohmann H, Carter VS, Nistal-Villán E, Katze MG. 2004. Integration of clinical data, pathology, and cDNA microarrays in influenza virus-infected pigtailed macaques (Macaca nemestrina). J. Virol. 78:10420–10432. 10.1128/JVI.78.19.10420-10432.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Itoh Y, Shinya K, Kiso M, Watanabe T, Sakoda Y, Hatta M, Muramoto Y, Tamura D, Sakai-Tagawa Y, Noda T, Sakabe S, Imai M, Hatta Y, Watanabe S, Li C, Yamada S, Fujii K, Murakami S, Imai H, Kakugawa S, Ito M, Takano R, Iwatsuki-Horimoto K, Shimojima M, Horimoto T, Goto H, Takahashi K, Makino A, Ishigaki H, Nakayama M, Okamatsu M, Warshauer D, Shult PA, Saito R, Suzuki H, Furuta Y, Yamashita M, Mitamura K, Nakano K, Nakamura M, Brockman-Schneider R, Mitamura H, Yamazaki M, Sugaya N, Suresh M, Ozawa M, Neumann G, Gern J, Kida H, Ogasawara K, Kawaoka Y. 2009. In vitro and in vivo characterization of new swine-origin H1N1 influenza viruses. Nature 460:1021–1025. 10.1038/nature08260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Murphy BR, Sly DL, Tierney EL, Hosier NT, Massicot JG, London WT, Chanock RM, Webster RG, Hinshaw VS. 1982. Reassortant virus derived from avian and human influenza A viruses is attenuated and immunogenic in monkeys. Science 218:1330–1332. 10.1126/science.6183749 [DOI] [PubMed] [Google Scholar]
- 51.Murphy BR, Hinshaw VS, Sly DL, London WT, Hosier NT, Wood FT, Webster RG, Chanock RM. 1982. Virulence of avian influenza A viruses for squirrel monkeys. Infect. Immun. 37:1119–1126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bielefeldt-Ohmann H, Tumpey TM, Sabourin PJ, Long JP, García-Sastre A, Tolnay AE, Albrecht R, Pyles JA, Olson PH, Aicher LD, Rosenzweig ER, Murali-Krishna K, Clark EA, Kotur MS, Fornek JL, Proll S, Palermo RE, Sabourin CL, Katze MG. 2009. Early and sustained innate immune response defines pathology and death in nonhuman primates infected by highly pathogenic influenza virus. Proc. Natl. Acad. Sci. U. S. A. 106:3455–3460. 10.1073/pnas.0813234106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shinya K, Gao Y, Cilloniz C, Suzuki Y, Fujie M, Deng G, Zhu Q, Fan S, Makino A, Muramoto Y, Fukuyama S, Tamura D, Noda T, Eisfeld AJ, Katze MG, Chen H, Kawaoka Y. 2012. Integrated clinical, pathologic, virologic, and transcriptomic analysis of H5N1 influenza virus-induced viral pneumonia in the rhesus macaque. J. Virol. 86:6055–6066. 10.1128/JVI.00365-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Min JY, Vogel L, Matsuoka Y, Lu B, Swayne D, Jin H, Kemble G, Subbarao K. 2010. A live attenuated H7N7 candidate vaccine virus induces neutralizing antibody that confers protection from challenge in mice, ferrets, and monkeys. J. Virol. 84:11950–11960. 10.1128/JVI.01305-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shinya K, Ebina M, Yamada S, Ono M, Kasai N, Kawaoka Y. 2006. Avian flu: influenza virus receptors in the human airway. Nature 440:435–436. 10.1038/440435a [DOI] [PubMed] [Google Scholar]
- 56.Nicholls JM, Chan MC, Chan WY, Wong HK, Cheung CY, Kwong DL, Wong MP, Chui WH, Poon LL, Tsao SW, Guan Y, Peiris JS. 2007. Tropism of avian influenza A (H5N1) in the upper and lower respiratory tract. Nat. Med. 13:147–149. 10.1038/nm1529 [DOI] [PubMed] [Google Scholar]
- 57.Nicholls JM, Bourne AJ, Chen H, Guan Y, Peiris JS. 2007. Sialic acid receptor detection in the human respiratory tract: evidence for widespread distribution of potential binding sites for human and avian influenza viruses. Respir. Res. 8:73. 10.1186/1465-9921-8-73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nicholls JM, Chan RW, Russell RJ, Air GM, Peiris JS. 2008. Evolving complexities of influenza virus and its receptors. Trends Microbiol. 16:149–157. 10.1016/j.tim.2008.01.008 [DOI] [PubMed] [Google Scholar]
- 59.van Riel D, Munster VJ, de Wit E, Rimmelzwaan GF, Fouchier RA, Osterhaus AD, Kuiken T. 2007. Human and avian influenza viruses target different cells in the lower respiratory tract of humans and other mammals. Am. J. Pathol. 171:1215–1223. 10.2353/ajpath.2007.070248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Thongratsakul S, Suzuki Y, Hiramatsu H, Sakpuaram T, Sirinarumitr T, Poolkhet C, Moonjit P, Yodsheewan R, Songserm T. 2010. Avian and human influenza A virus receptors in trachea and lung of animals. Asian Pac. J. Allergy Immunol. 28:294–301 http://apjai.digitaljournals.org/index.php/apjai/article/viewFile/353/340 [PubMed] [Google Scholar]
- 61.Stevens J, Blixt O, Chen LM, Donis RO, Paulson JC, Wilson IA. 2008. Recent avian H5N1 viruses exhibit increased propensity for acquiring human receptor specificity. J. Mol. Biol. 381:1382–1394. 10.1016/j.jmb.2008.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Stevens J, Blixt O, Glaser L, Taubenberger JK, Palese P, Paulson JC, Wilson IA. 2006. Glycan microarray analysis of the hemagglutinins from modern and pandemic influenza viruses reveals different receptor specificities. J. Mol. Biol. 355:1143–1155. 10.1016/j.jmb.2005.11.002 [DOI] [PubMed] [Google Scholar]
- 63.Stevens J, Blixt O, Tumpey TM, Taubenberger JK, Paulson JC, Wilson IA. 2006. Structure and receptor specificity of the hemagglutinin from an H5N1 influenza virus. Science 312:404–410. 10.1126/science.1124513 [DOI] [PubMed] [Google Scholar]
- 64.Walther T, Karamanska R, Chan RW, Chan MC, Jia N, Air G, Hopton C, Wong MP, Dell A, Malik Peiris JS, Haslam SM, Nicholls JM. 2013. Glycomic analysis of human respiratory tract tissues and correlation with influenza virus infection. PLoS Pathog. 9:e1003223. 10.1371/journal.ppat.1003223 [DOI] [PMC free article] [PubMed] [Google Scholar]