Abstract
Background/Aim:
Yoga is an ancient Indian science as well as the way of life. Pranayama is a part of yoga, which improves pulmonary function in combination of many pranayama, but the aim of our study is to evaluate the effect of only Bhramari pranayama and OM chanting on pulmonary function in healthy individuals.
Materials and Methods:
A total of 82 subjects were randomized into the study group (SG) (n = 41) and control group (CG) (n = 41). Baseline assessment was performed before intervention for both groups. SG practiced Bhramari pranayama and OM chanting for the duration of 10 min (5 min for each practice)/day for the period of 6 days/week for 2 weeks and CG did not practice so. After intervention post-assessment was performed for SG (n = 40) and CG (n = 39). Statistical analysis was performed by Independent samples t-test and Student's paired t-test with the use of Statistical Package for the Social Sciences version 16 (2007, USA).
Results:
The result showed a significant improvement in peak expiratory flow (PEF), forced expiratory flow (FEF)25% and maximal voluntary ventilation (MVV) along with a significant reduction in weight in SG compared with CG in independent samples t-test. Significant improvement in slow vital capacity (SVC), forced expired volume in 1 s (FEV1) along with PEF, FEF25% and MVV; Significant reduction in weight and body mass index were observed in SG unlike in CG in Student's paired t-test. No significant changes were found in forced vital capacity, FEV1 /SVC and FEF50% , between and within the group analysis of SG and CG.
Conclusion:
Bhramari pranayama and OM chanting are effective in improving pulmonary function in healthy individuals.
Keywords: Bhramari pranayama, OM chanting, pulmonary function
INTRODUCTION
Yoga is an ancient Indian science as well as the way of life, which includes practice of specific posture (asana), regulated breathing (pranayama) etc.[1] Breath is the dynamic bridge between body and mind[2] and pranayama (breathing techniques) is one of the most important yogic practices, which can produce different physiological responses in healthy individuals.[3] Pranayama is an art of prolongation and control of breath, which helps to bring the conscious awareness in breathing; to reshape breathing habits and patterns.[2] The persistent conditioning of breathing pattern of pranayama increases the pulmonary function in healthy individuals.[3]
Though, there are various pranayamas in yogic practices the Bhramari pranayama and OM chanting were used as expiratory exercises for bronchial asthma.[4] Bhramari pranayama (humming bee breath) is one of the yogic practice, which involves sitting in sukhasana (ease pose) the subject should inhale through both nostrils and while exhaling produce sound of female humming bee.[4] Combination of A, U (O) and M, i.e., OM is one of the fundamental symbols used in the yoga tradition, which symbolizes the three states of consciousness i.e., waking state, dream state and deep sleep respectively. Though, the sound of OM represents the primal vibration[5] and the OM chanting is an important exhalation exercise it was not included in regular breathing exercises to improve the pulmonary function in bronchial asthma.[4]
There have been many studies on yoga and its effects on physical functions,[3] autonomic variables,[6,7,8,9,10] stress[7,9,10,11,12,13] etc., Though the popularity of pranayama is increasing in the past few years there is lack of studies on the pranayama[3] especially on Bhramari pranayama and OM chanting on pulmonary function which had been used as expiratory exercises for bronchial asthma.[4] To the best of our knowledge there is no previous randomized control trail in combination of Bhramari pranayama and OM chanting on pulmonary functions made us to select this present study with the aims and objective to evaluate the effect of Bhramari pranayama and OM chanting on pulmonary function in healthy individuals.
MATERIALS AND METHODS
Subjects
A total of 82 subjects which consists of 18 male and 64 female with age varied from 18 to 27 years were recruited from our college of naturopathy and yogic sciences, Medical Sciences and Hospital, Institute of Nursing Sciences and College of Physiotherapy. Though, the subjects were from different colleges they were all in the same campus with similar atmosphere and diet. Out of 82 subjects, 80 were non-yoga practitioners and two were practitioners who did not practice since 6-7 months with no reason. The study was conducted in the Department of Physiology of our college of medical sciences and hospital. The study protocol was approved by the institutional ethical committee of our college of medical sciences and hospital. The study was explained to all subjects and their written informed consent had been obtained. The sample size was determined based on the number of subjects who volunteered to participate in the trial. There was no attempt to determine the sample size based on previous effect sizes, which is a limitation of our study.[14] The subjects were recruited by the following criteria; inclusion criteria: Both sex with age between 18 and 30 years. Exclusion criteria: Subjects with the habits of tobacco chewing, smoking and alcoholism; history of any systemic diseases including respiratory tract diseases within the previous 6 weeks; history of regular medication for any diseases; mental illness; who cannot perform the pranayama; engagement in any pranayama/exercise/sports program at present and for the past 6 weeks.[3]
Baseline assessments were performed on 82 subjects (study group [SG] [n = 41] and control group [CG] [n = 41]) on the day prior to their intervention. 79 subjects (SG [n = 40] and CG [n = 39]) contributed to the current analyses at the second assessment after 2 weeks of intervention. The reasons for dropouts attributed to family problem (n = 1) in SG and (n = 1) in CG; and personal problem (n = 1) in CG. Figure 1 shows the illustration of methods of the study.
Figure 1.
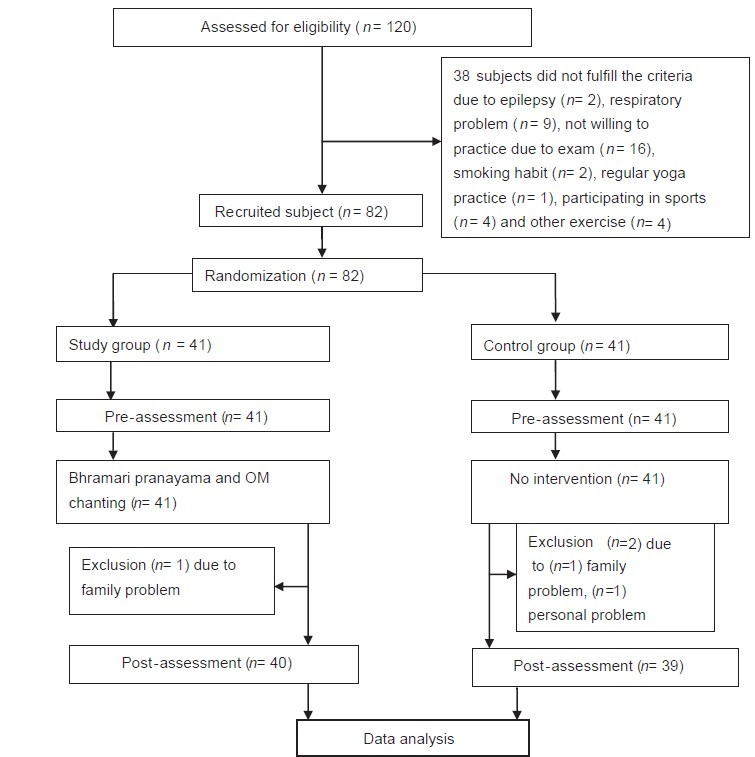
Illustration of methods of study
Randomization
The recruited subjects were randomized into either SG or CG on the day prior to their intervention using the papers with word “study” and “control” were put in an envelope and the paper each subject drew out determined their group.[15] The randomization was done by one of the author who involved in intervention, but he did not involve in any part of the investigation.
Blinding/masking
It was not possible to mask the pranayama intervention from the subjects. However, the investigator who did the pulmonary function test (PFT) was blind to the intervention or SG/CG.[13]
Assessments
Height: By using standard measuring tape, height in cm of each subject was measured. Weight: By using standard weighing machine, the weight in kg of each subject was measured. Body mass index (BMI): By using height and weight in the formula of weight in kg/height in m2 it has been derived.
The following spirometric measures were assessed with the use of computerized spirometric equipment (Schiller Spirovit-SP1); slow vital capacity (SVC), forced vital capacity (FVC) and FEV1 expressed in liter; FEV1 /SVC expressed in percentage; forced expiratory flow (FEF)25% , FEF50% , FEF75% , FEF25-75% and peak expiratory flow (PEF) expressed in liter/second; and maximal voluntary ventilation (MVV) expressed in liter/minute. SVC, FVC maneuver were repeated at least thrice during each measurement and the highest of three acceptable readings were taken as the final values of that sitting.[16] MVV maneuver was done by asking the subjects to breathe in and out rapidly and forcefully through the mouth piece attached with the maneuver up to 12 s continuously without interruption. Maneuver was repeated at least thrice during each measurement and the highest of three acceptable readings were taken as the final values of that sitting.
Interventions
SG practiced the combination of Bhramari pranayama and OM chanting in the morning around 7.45 am-8.45 am under the supervision for the duration of 10 min (5 min for each practice) for the period of 6 days/week for 2 weeks. The procedure used for our interventions are as follows; The Bhramari pranayama: The subjects asked to sit in sukhasana followed by inhalation through both nostrils and while exhaling should produce sound of female humming bee. OM chanting: Subjects were asked to sit in sukhasana and to inhalation deeply and then while exhaling should produce sound (chant) OM with the ability to continue until further exhalation is not possible.[4]
CG did not receive any intervention for the same period.
Data analysis
The data were analyzed statistically by using the statistical package for the social sciences version 16. Statistical analysis of baseline and post-intervention assessments of both SG (n = 40) and CG (n = 39) were done by using independent samples t-test.[13] Pre- and post-assessment of SG (n = 40) and CG (n = 39) were done by using Student's paired t-test. P < 0.05 was considered as significant.
RESULTS
Out of 120 subjects assessed for the eligibility, 38 subjects did not fulfill the criteria and did not include in the study. The recruited 82 subject's baseline assessment was taken before intervention. After intervention post-assessment was taken for 79 subjects those who completed the study successfully and statistical analysis was done to compare groups at baseline and post-intervention between and within the groups. There were no significant differences between the SG and CG at baseline assessment except in weight and FEV1/SVC [Tables 1 and 2].
Table 1.
Demographic variables of study and control group (Independent samples t test)
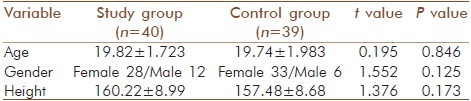
Table 2.
Baseline and post-test assessment with statistical analysis between (Independent samples t-test) and within (Student's paired t test) the study and control groups
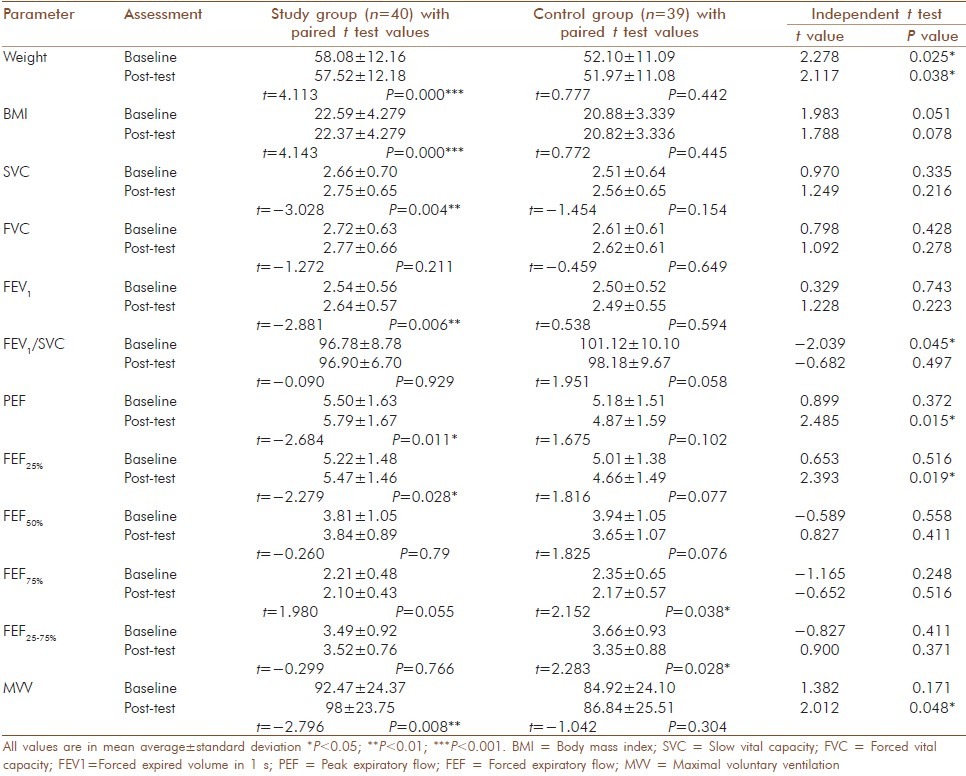
Our result showed the significant increases in PEF, FEF25% and MVV along with a significant reduction in weight in the SG compared with CG, but no significant changes were found between the groups in the rest of the variables in independent samples t-test [Table 2].
The Student paired t-test was used to find the changes in the pre- and post-intervention outcome of within the groups. It showed a significant increase in SVC in SG, but in CG no such significant change was found. FVC was increased insignificantly in both SG and CG. Though the improvements were insignificant, better improvement was seen in SG than CG. Significant increase in FEV1, PEF and FEF25% ; and insignificant increase in FEV1 /SVC were observed in SG, but in CG insignificant reductions were observed.
Though no significant changes in FEF50% in both groups, it increased in SG, but reduced in CG. Significant reduction in FEF75% and FEF25-75% were observed in CG, but no such significant changes were found in SG. MVV significantly increased in SG, but no significant changes found in CG. Along with these results significant reduction in weight and BMI was observed in SG unlike CG [Table 2].
DISCUSSION
The result of our study showed significant increases in PEF, FEF25% and MVV along with a significant reduction in weight in SG compared with CG.
PEF and FEF25% reflects mainly the caliber of the bronchi and larger bronchioles, which are subjected to reflex bronchi constriction. The flow rate is a function of lung volume rather than the effort exerted that is why it is “effort independent flow” and is significantly increased in SG, which is supported by the previous study on “OM” meditators.[17]
The increased PEF, FEF25% and MVV may attribute to voluntary prolongation of inspiration and expiration during pranayama stretched the respiratory muscles to their full extent and the respiratory apparatus was able to work to their maximal capacity;[17] the use of diaphragmatic and abdominal muscles more efficiently[3] during the Bhramari and OM chanting. Improvement of respiratory muscle function helps to reduce the relative load on the muscles and increase maximal sustained ventilatory capacity.[18]
Previous study on yoga showed significant improvement in peak expiratory flow rate (PEFR) at 2-week supporting our study, but improvement in FEV1 and FEF25-75% between the groups did not support our study. Though this result did not support the study, it was found at 8-week.[16]
Between the group analyses there were no significant changes in SVC and FEV1, whereas within the group analysis significant improvement in SVC, FEV1, along with PEF, FEF25% and MVV were observed in SG unlike in CG.
The significant improvement in SVC might be due to the regular practice of Bhramari and OM chanting could attributed to increase in lung volumes and vital capacity by its slow breathing[19,20] slow and deep breathing technique which is commonly used to decrease the work of breathing and accessory muscle activity; to increase the efficiency of breathing; and to improve the ventilation by its slow breath rate and more tidal volume.[18]
Significant improvement in FEV1 might attributed to the development of respiratory musculature incidental to regular practice of pranayama along with its calming effect on mind could reduce emotional stress, wherefore withdrawing the broncho-constrictor effects.[3] So Bhramari and OM chanting may be useful for obstructive pulmonary diseases. Significant improvement in SVC, FEV1 , PEFR and MVV in studies on pranayama in healthy[3] and yogic practices in asthma[21] on pulmonary function; significant improvement in FEV1, MVV, PEFR in previous studies on yoga in healthy,[22] pranayama in hypothyroidism[23] and diabetes;[24] significant improvement in FEV1 and PEF in previous studies where Bhramari and OM chanting were used as expiratory exercise[4] and yoga (including pranayama) based mind body intervention for asthma[16] supporting our study.
Though no significant changes were found in FVC, FEV1 /SVC and FEF 50% in between and within the group analysis, the improvements were better in SG than CG indicates the Bhramari and OM chanting may have some effect on these parameters. Significant increase in FVC was observed in previous studies on deep breathing exercise,[25] on the combination of various pranayama[3] and yoga[22] in healthy individuals; On yogic practices in asthma[21] and in diabetes,[24] but in our study we did not find so.
Though no significant changes were found in FEF75% and FEF25-75% in between the group analysis, significant reduction was found within the group analysis CG unlike SG. It indicates Bhramari and OM chanting may be useful to prevent airflow obstruction. Along with these results significant reduction in weight was observed in SG compared with CG with no significant change in BMI in between group analysis. Though there was a significant difference in weight at baseline that did not affect the result because in within group analysis the significant reduction of both weight and BMI were observed in SG and no such significant changes were observed in CG, indicates the regular practice of pranayama may be useful in correction of overweight/obesity, which is associated with various systemic diseases such as Coronary heart disease, hypertension and even cancer.[26] In the respiratory system, it may be associated with childhood respiratory infections,[27] breathlessness, obstructive sleep apnea,[26] obesity-hypoventilation syndrome, pulmonary atelectasis[28] and restrictive lung disease.[29]
In a study on yogic practices significant decrease in weight and BMI[30] supporting our study. Increased weight is associated with diabetes[26] in which better glycemic control,[24,31] pulmonary functions[24] and stable autonomic functions[31] were obtained with yoga asanas and pranayama. Improvement in PFT in our study may attribute to the following mechanisms and effects of pranayama practices described on various previous studies.
The slow breathing technique of Bhramari and OM chanting may be useful to promotes sympathovagal balance;[10] to improves autonomic functions;[32] and to modify the sympathovagal imbalance, which is common in patient with the chronic obstructive pulmonary disease (COPD).[33] In a previous study on neurohemodynamic correlates of “OM” chanting showed limbic deactivation and similar observations were recorded in vagal nerve stimulation used in the treatment of depression,[34] which is common in COPD, bronchial asthma and can affect the quality of sleep, quality-of-life and diseases condition.[35,36,37]
Stress is an important precipitating factors of asthma,[4] slow and deep breathing has a calming effect on the mind, which is not only helps to de-stress,[38] but also improve the antioxidant status of the individual.[39] Yoga is a form of mind-body medicine, which promotes positive affect and reduce negative affect to increase lung functions and reduce usage of bronchodilator in asthmatics.[40] Yogic breathing exercises (YBE) can reduce cigarette craving acutely, which may reduces the risk of chronic lung disease.[41]
In chronic lung disease, diffusion capacity is impaired and YBE improves it especially in COPD.[30] This effect attributed to the fact that yogic breathings (YB) are more of a vertical breathing by which all the alveoli of both the lungs open-up evenly and provide a vast expanse of alveolar surface membrane about 50 m2 in extent, which is 20 times the entire body surface for exchange of gases;[30] pranayama may affect the milieu at bronchioles and alveoli particularly at alveolocapillary membrane to facilitate diffusion and transport of gases.[21]
Pranayamas are used to calm the body, raise energy levels, increase respiratory stamina, relax the chest muscles and expand the lungs.[21,30] Slow and deep breathing reduces dead space ventilation and refreshes the air throughout lungs[25,38] and induces a generalized decrease in the excitatory pathways regulating respiratory systems.[2] During this breathing lung inflates to the maximum which stimulates pulmonary stretch receptors.[2] The stretch receptors reflex decrease the tracheobronchial smooth muscle tone, which in turn decrease air resistance and increase airway caliber, which causes the lung function test to improve.[17] With pranayama practice one can increase the intake of oxygen up to 5 times[12] and also increase oxygenation at the tissue level.[21] Hence deep breathing exercise, even for a few minutes duration is beneficial for the lung function.[25]
Yoga practices might be interacting with various, somato-neuroendocrine mechanisms[24] and it can be used as psychophysiologic stimuli to increase endogenous secretion of melatonin, which improves sense of well-being.[42] By reducing perceived stress and anxiety, yoga easing respiration and it can be beneficial in the prevention and cure of diseases.[17]
The limitations of our study are we did not do the diffusion capacity, lung volumes and total lung capacity. In the baseline, though there were variations in weight and FEV1 /SVC between SG and CG that did not affect the PFT because it depends on the individual's own weight.
Strength of our study are the first randomized control trial evaluating the effect of only Bhramari pranayama and OM chanting on pulmonary function in the healthy individuals; though the duration of intervention was short, significant improvements were found in pulmonary function in SG, which was not seen in CG. Easy pranayama practices can be done by irrespective of age, sex and religion etc., The results of OM chanting along with Bhramari pranayama suggest that it can also be considered and included as a regular breathing exercise to improve pulmonary function which is not exist so far. Further, studies are required with the more number of sample size and longer duration to find out the effect of each practice separately with underling mechanism.
CONCLUSION
Based on the limitations it can be concluded that these result showed a significant improvement in PEF, FEF25% and MVV with a significant reduction in weight in SG compared with CG in independent samples t-test. Significant improvement in SVC, FEV1, along with PEF, FEF25% and MVV; and significant reduction in weight and BMI in SG unlike CG in Student's paired t-test. It suggests that Bhramari pranayama and OM chanting are effective in improving the pulmonary function in healthy individuals.
ACKNOWLEDGMENTS
We thank Dr. Prashanth Shetty (Principal) Dr. Sujatha and Dr. Shivaprasad Shetty (PG coordinators) of our College of Naturopathy and Yogic sciences, for their support and guidance. We thank Dr. Niranjan Kumar (Medical Director), Dr. Chowti (Principal), Dr. Shoba Nallulwar (HOD of Physiology) and staffs (Department of Physiology) of our college of medical sciences and hospital for granted permission to contact the study and to use equipments. We would like to thank principal and staffs of our Institute of Nursing Sciences and College of Physiotherapy for granted permission and support. We are most thankful for the students participated in our study. We are thankful to Dr. Naveen K. V. and Dr. N. K. Manjunath for their guidance. The last but not the least we are thankful to Mr. MS Jain, our Family members and Friends for their economic, emotional and spiritual support.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Yogitha B, Nagarathna R, John E, Nagendra H. Complimentary effect of yogic sound resonance relaxation technique in patients with common neck pain. Int J Yoga. 2010;3:18–25. doi: 10.4103/0973-6131.66774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ankad RB, Herur A, Patil S, Shashikala GV, Chinagudi S. Effect of short-term pranayama and meditation on cardiovascular functions in healthy individuals. Heart Views. 2011;12:58–62. doi: 10.4103/1995-705X.86016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patil YR, Sawant RS. Effect of bastrika pranayama on pulmonary function. Int J Pharm. 2012;3:204–7. [Google Scholar]
- 4.Saxena T, Saxena M. The effect of various breathing exercises (pranayama) in patients with bronchial asthma of mild to moderate severity. Int J Yoga. 2009;2:22–5. doi: 10.4103/0973-6131.53838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumar S, Nagendra H, Manjunath N, Naveen K, Telles S. Meditation on OM: Relevance from ancient texts and contemporary science. Int J Yoga. 2010;3:2–5. doi: 10.4103/0973-6131.66771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Manjunath NK, Telles S. Effects of sirsasana (headstand) practice on autonomic and respiratory variables. Indian J Physiol Pharmacol. 2003;47:34–42. [PubMed] [Google Scholar]
- 7.Sengupta P. Health impacts of yoga and pranayama: A state-of-the-art review. Int J Prev Med. 2012;3:444–58. [PMC free article] [PubMed] [Google Scholar]
- 8.Vempati RP, Telles S. Yoga-based guided relaxation reduces sympathetic activity judged from baseline levels. Psychol Rep. 2002;90:487–94. doi: 10.2466/pr0.2002.90.2.487. [DOI] [PubMed] [Google Scholar]
- 9.Rampalliwar S, Rajak C, Arjariya R, Poonia M, Bajpai R. The effect of bhramari pranayama on pregnant women having cardiovascular hyper-reactivity to cold pressor. Natl J Physiol Pharm Pharmacol. 2013;3:128–33. [Google Scholar]
- 10.Bhimani NT, Kulkarni NB, Kowale A, Salvi S. Effect of Pranayama on stress and cardiovascular autonomic function. Indian J Physiol Pharmacol. 2011;55:370–7. [PubMed] [Google Scholar]
- 11.Gururaja D, Harano K, Toyotake I, Kobayashi H. Effect of yoga on mental health: Comparative study between young and senior subjects in Japan. Int J Yoga. 2011;4:7–12. doi: 10.4103/0973-6131.78173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nemati A. The effect of pranayama on test anxiety and test performance. Int J Yoga. 2013;6:55–60. doi: 10.4103/0973-6131.105947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rao RM, Nagendra HR, Raghuram N, Vinay C, Chandrashekara S, Gopinath KS, et al. Influence of yoga on postoperative outcomes and wound healing in early operable breast cancer patients undergoing surgery. Int J Yoga. 2008;1:33–41. doi: 10.4103/0973-6131.36795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Telles S, Yadav A, Kumar N, Sharma S, Visweshwaraiah NK, Balkrishna A. Blood pressure and purdue pegboard scores in individuals with hypertension after alternate nostril breathing, breath awareness, and no intervention. Med Sci Monit. 2013;19:61–6. doi: 10.12659/MSM.883743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Santaella DF, Devesa CR, Rojo MR, Amato MB, Drager LF, Casali KR, et al. Yoga respiratory training improves respiratory function and cardiac sympathovagal balance in elderly subjects: A randomised controlled trial. BMJ Open. 2011;1:e000085. doi: 10.1136/bmjopen-2011-000085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vempati R, Bijlani RL, Deepak KK. The efficacy of a comprehensive lifestyle modification programme based on yoga in the management of bronchial asthma: A randomized controlled trial. BMC Pulm Med. 2009;9:37. doi: 10.1186/1471-2466-9-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bora G, Nazir J, Ravi GN. A comparative study of peak expiratory flow rate and breath holding time in normal and ‘OM’ meditators. J Evol Med Dent Sci. 2013;2:4111–9. [Google Scholar]
- 18.Gosselink R. Controlled breathing and dyspnea in patients with chronic obstructive pulmonary disease (COPD) J Rehabil Res Dev. 2003;40(5 Suppl 2):25–33. doi: 10.1682/jrrd.2003.10.0025. [DOI] [PubMed] [Google Scholar]
- 19.Pramanik T, Pudasaini B, Prajapati R. Immediate effect of a slow pace breathing exercise Bhramari pranayama on blood pressure and heart rate. Nepal Med Coll J. 2010;12:154–7. [PubMed] [Google Scholar]
- 20.Jain G, Rajak C, Rampalliwar S. Effect of bhramari pranayama on volunteers having cardiovascular hyper-reactivity to cold pressor test. J Yoga Phys Ther. 2011;1:102. [Google Scholar]
- 21.Singh S, Soni R, Singh KP, Tandon OP. Effect of yoga practices on pulmonary function tests including transfer factor of lung for carbon monoxide (TLCO) in asthma patients. Indian J Physiol Pharmacol. 2012;56:63–8. [PubMed] [Google Scholar]
- 22.Abel AN, Lloyd LK, Williams JS. The effects of regular yoga practice on pulmonary function in healthy individuals: A literature review. J Altern Complement Med. 2013;19:185–90. doi: 10.1089/acm.2011.0516. [DOI] [PubMed] [Google Scholar]
- 23.Swami G, Singh S, Singh KP, Gupta M. Effect of yoga on pulmonary function tests of hypothyroid patients. Indian J Physiol Pharmacol. 2010;54:51–6. [PubMed] [Google Scholar]
- 24.Malhotra V, Singh S, Singh KP, Gupta P, Sharma SB, Madhu SV, et al. Study of yoga asanas in assessment of pulmonary function in NIDDM patients. Indian J Physiol Pharmacol. 2002;46:313–20. [PubMed] [Google Scholar]
- 25.Sivakumar G, Prabhu K, Baliga R, Pai MK, Manjunatha S. Acute effects of deep breathing for a short duration (2-10 minutes) on pulmonary functions in healthy young volunteers. Indian J Physiol Pharmacol. 2011;55:154–9. [PubMed] [Google Scholar]
- 26.Schachter L. Respiratory assessment and management in bariatric surgery. Respirology. 2012;17:1039–47. doi: 10.1111/j.1440-1843.2012.02199.x. [DOI] [PubMed] [Google Scholar]
- 27.Wijga AH, Scholtens S, Bemelmans WJ, de Jongste JC, Kerkhof M, Schipper M, et al. Comorbidities of obesity in school children: A cross-sectional study in the PIAMA birth cohort. BMC Public Health. 2010;10:184. doi: 10.1186/1471-2458-10-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harris AT, Morell D, Bajaj Y, Martin-Hirsch DP. A discussion of airway and respiratory complications along with general considerations in obese patients. Int J Clin Pract. 2010;64:802–6. doi: 10.1111/j.1742-1241.2010.02350.x. [DOI] [PubMed] [Google Scholar]
- 29.Geiling J. Critical care of the morbidly obese in disaster. Crit Care Clin. 2010;26:703–14. doi: 10.1016/j.ccc.2010.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Soni R, Munish K, Singh K, Singh S. Study of the effect of yoga training on diffusion capacity in chronic obstructive pulmonary disease patients: A controlled trial. Int J Yoga. 2012;5:123–7. doi: 10.4103/0973-6131.98230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Singh S, Malhotra V, Singh KP, Madhu SV, Tandon OP. Role of yoga in modifying certain cardiovascular functions in type 2 diabetic patients. J Assoc Physicians India. 2004;52:203–6. [PubMed] [Google Scholar]
- 32.Pal GK, Velkumary S, Madanmohan Effect of short-term practice of breathing exercises on autonomic functions in normal human volunteers. Indian J Med Res. 2004;120:115–21. [PubMed] [Google Scholar]
- 33.Raupach T, Bahr F, Herrmann P, Luethje L, Heusser K, Hasenfuss G, et al. Slow breathing reduces sympathoexcitation in COPD. Eur Respir J. 2008;32:387–92. doi: 10.1183/09031936.00109607. [DOI] [PubMed] [Google Scholar]
- 34.Kalyani BG, Venkatasubramanian G, Arasappa R, Rao NP, Kalmady SV, Behere RV, et al. Neurohemodynamic correlates of ‘OM’ chanting: A pilot functional magnetic resonance imaging study. Int J Yoga. 2011;4:3–6. doi: 10.4103/0973-6131.78171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.De S. Subjective assessment of quality of sleep in chronic obstructive pulmonary disease patient and its relationship with associated depression. Lung India. 2012;29:332–5. doi: 10.4103/0970-2113.102808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Olveira C, Olveira G, Gaspar I, Dorado A, Cruz I, Soriguer F, et al. Depression and anxiety symptoms in bronchiectasis: Associations with health-related quality of life. Qual Life Res. 2013;22:597–605. doi: 10.1007/s11136-012-0188-5. [DOI] [PubMed] [Google Scholar]
- 37.Urrutia I, Aguirre U, Pascual S, Esteban C, Ballaz A, Arrizubieta I, et al. Impact of anxiety and depression on disease control and quality of life in asthma patients. J Asthma. 2012;49:201–8. doi: 10.3109/02770903.2011.654022. [DOI] [PubMed] [Google Scholar]
- 38.Subbalakshmi NK, Saxena SK, Urmimala, D’Souza Urban JA. Immediate effect of ‘nadi-shodhana pranayama’ on some selected parameters of cardiovascular, pulmonary, and higher functions of brain. Thail J Physiol Sci. 2005;18:10–6. [Google Scholar]
- 39.Bhattacharya S, Pandey US, Verma NS. Improvement in oxidative status with yogic breathing in young healthy males. Indian J Physiol Pharmacol. 2002;46:349–54. [PubMed] [Google Scholar]
- 40.Narasimhan L, Nagarathna R, Nagendra H. Effect of integrated yogic practices on positive and negative emotions in healthy adults. Int J Yoga. 2011;4:13–9. doi: 10.4103/0973-6131.78174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shahab L, Sarkar BK, West R. The acute effects of yogic breathing exercises on craving and withdrawal symptoms in abstaining smokers. Psychopharmacology (Berl) 2013;225:875–82. doi: 10.1007/s00213-012-2876-9. [DOI] [PubMed] [Google Scholar]
- 42.Harinath K, Malhotra AS, Pal K, Prasad R, Kumar R, Kain TC, et al. Effects of Hatha yoga and Omkar meditation on cardiorespiratory performance, psychologic profile, and melatonin secretion. J Altern Complement Med. 2004;10:261–8. doi: 10.1089/107555304323062257. [DOI] [PubMed] [Google Scholar]


