Abstract
Context and Aims:
Migraine is an episodic disabling headache requiring long-term management. Migraine management through Yoga therapy would reduce the medication cost with positive health benefits. Yoga has shown to improve the quality of life, reduce the episode of headache and medication. The aim of the present study was to evaluate the efficacy of Yoga as an adjuvant therapy in migraine patients by assessing clinical outcome and autonomic functions tests.
Subjects and Methods:
Migraine patients were randomly given either conventional care (n = 30) or Yoga with conventional care (n = 30). Yoga group received Yoga practice session for 5 days a week for 6 weeks along with conventional care. Clinical assessment (frequency, intensity of headache and headache impact) and autonomic function test were done at baseline and at the end of the intervention.
Results:
Yoga with conventional care and convention care groups showed significant improvement in clinical variables, but it was better with Yoga therapy. Improvement in the vagal tone along with reduced sympathetic activity was observed in patients with migraine receiving Yoga as adjuvant therapy.
Conclusions:
Intervention showed significant clinical improvement in both groups. Headache frequency and intensity were reduced more in Yoga with conventional care than the conventional care group alone. Furthermore, Yoga therapy enhanced the vagal tone and decreased the sympathetic drive, hence improving the cardiac autonomic balance. Thus, Yoga therapy can be effectively incorporated as an adjuvant therapy in migraine patients.
Keywords: Autonomic functions, conventional care, migraine, Yoga
INTRODUCTION
Migraine clinically manifests as hemi-cranial throbbing type of pain associated with nausea, vomiting, heightened sensitivity to light (photophobia) and sound (phonophobia) with or without transient neurological symptoms.[1] Migraine is one of the common primary headache disorders affecting 13% of the population world-wide.[2] Prodromal, headache episode and postdromal phases of migraine are known to impact productivity at work and quality of life, apart from causing cognitive impairment.[3] The burden of migraine impacts affected individuals, their family, and society.[4,5] It is also a risk factor for ischemic cerebral and ischemic cardiovascular diseases.[6] Episodic migraine may lead to chronic migraine, if it is not treated properly it may lead to medication overuse headache and increased risk of suicidal attempt.[7]
Autonomic nervous system (ANS) imbalance explains many of the clinical manifestations of the migraine disorder. Autonomic symptoms (such as nausea, vomiting, or diarrhoea, cutaneous vasoconstriction [pallor], vasodilatation [flushing], piloerection and diaphoresis) are common during acute migraine headaches.[8]
Migraine is a chronic disorder with episodic disabilities and it requires long-term management as well as preventive strategies. The treatment of migraine involves both acute and preventive drugs along with non-pharmacological strategies. Even though in the last few decades much advancement has occurred in the research field of migraine, its treatment does not provide complete relief to many patients. Biofeedback and relaxation have been demonstrated to be useful alternatives to standard medical therapy for both migraine and tension-type headaches.[9] The present study was aimed to evaluate the effect of Yoga as adjuvant therapy in patients with migraine.
SUBJECTS AND METHODS
The present study was approved by the Institutional Ethical Committee. Sixty patients were recruited from a tertiary referral neurology centre. Diagnosis of migraine, with or without aura was done according to the guidelines of International Headache Society, International Classification of Headache Disorders 2nd edition (IHS, ICHD - II)[1] after thorough clinical interview, physical and neurological examination by the neurologist. Both male and female migraine patients between the age group of 15-60 years satisfying the IHS, ICHD - II criteria for migraine without (1.1) or with aura (1.2.1) with a history of at least 2 years of migraine and headache frequency of 5-15/month were recruited for the study. Patients with other medical or neurological illness were not included in the study. Recent head or neck traumas within 2 years were excluded from study. Furthermore female patients who were pregnant or lactating were not recruited for the study. Recruited patients were explained about the nature of study and written informed consent was obtained. Patients were randomized mainly to conventional care only (CC) and conventional care and Yoga therapy (Y) using a concealed allocation protocol. [Study design - Figure 1]
Figure 1.
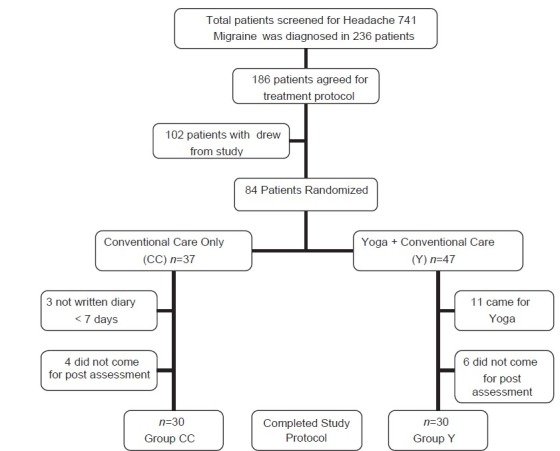
Study design. CC-Conventional care group, Y-Yoga+Conventional care group
Group (CC)
Migraine patients received conventional care for 6 weeks. Patients were advised to maintain headache diary for this period. 1 week after baseline assessment, confirmation of maintaining headache diary was done by telephonic conversation or personal contact. At the end of 6 week post-intervention, assessment was done and headache diary was collected.
Group (Y)
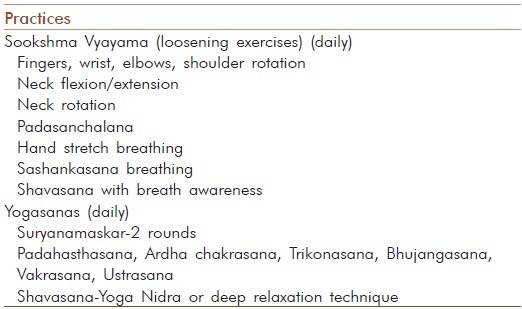
Migraine patients receiving conventional care and Yoga therapy had received Yoga therapy along with conventional care. Patients were scheduled to visit for 30 sessions (5 days a week for 6 weeks) of Yoga. They were asked to maintain headache diary for the full duration of the study and was verified during Yoga session. At the end of 6 weeks, post-intervention assessment was done and headache diary was collected. The Yoga intervention consisted of a daily practice of loosening exercises, breathing exercises, asanas or postures done with awareness and Shavasana [Table 1]. Each Yoga session lasted about an hour. Yoga therapy was imparted by a trained Yoga therapist at the Yoga centre in the institution's premises. Daily record of attendance and compliance to Yoga intervention were maintained.
Table 1.
Yoga module for migraine patients
The subjective variable, headache-specific quality of life was measured as the change in headache-related disability, which was assessed by the headache impact test (HIT-6). The total number of headache episodes, intensity of headaches (0-10 on Visual analog scale) and medication used were noted in headache diary by patients. Self-perceived benefit of the intervention was measured at the end of the 6th week of the treatment period in both groups. Patients rated the perceived benefit of the therapy on a five point scale ranging from “greatly worsened my clinical condition” to “greatly improved my clinical condition.” In addition, they assessed the therapy as “more harmful than helpful,” “neither harmful nor helpful,” or “more helpful than harmful.”
Autonomic function test was done when the subject was headache-free at least 3 days before and after the test. Autonomic function tests were carried out in autonomic laboratory, under all standardized conditions.[10,11,12] Lead II electrocardiogram (ECG) and breathing signals were conveyed through analog digital converter (Power lab, 16 channels data acquisition system, AD Instruments, Australia) with a sampling rate of 1024 Hz. The data were stored and were analyzed offline using an automatic programme that allowed visual checking of the raw ECG and breathing signals. 15 min basal recordings were stored and later analyzed to obtain both time and frequency domain parameters of heart rate variability (HRV) using HRV Analysis Software V1.1 (Power lab 16 channels data Acquisition System, AD instrument, Australia). HRV recording and analysis were performed according to the guidelines of Task force report.[13] An artefact free 5 min segment was analyzed to obtain time domain (Heart rate, standard deviation (SD) of NN interval, square root of the mean of the sum of squares of differences between adjacent R-R intervals) and frequency domain (Total power, low frequency power [LF power], low frequency normalized units, high frequency power [HF power], high frequency normalized units [HFnu], sympathovagal balance [SVB] - LF/HF ratio) parameters of HRV.
Statistical analyses were carried out on statistical package for the social sciences 15.0 software supplied by IBM. Descriptive statistical analysis has been carried out in the present study. Results on continuous measurements were presented on Mean ± SD unpaired t-test was used to compare the variables at the baseline characteristics of the two groups of patients. Paired t-test was used to compare the clinical, HRV, following 6 week intervention. HRV parameters were square root transformed for analysis and presented after back transforming. Level of significance was kept at 0.05.
RESULTS
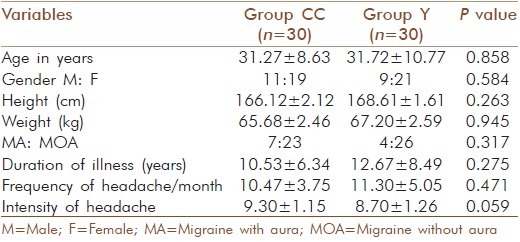
A total of 30 migraine patients were studied under conventional care (Group CC) and 30 patients were studied under Yoga with conventional care (Group Y) group. Both the study groups were identical in demographic variables such as age, gender distribution, height and weight. No significant differences in mean duration of the illness, frequency and intensity were observed among the two groups [Table 2].
Table 2.
Comparison of demographic and clinical details of patients
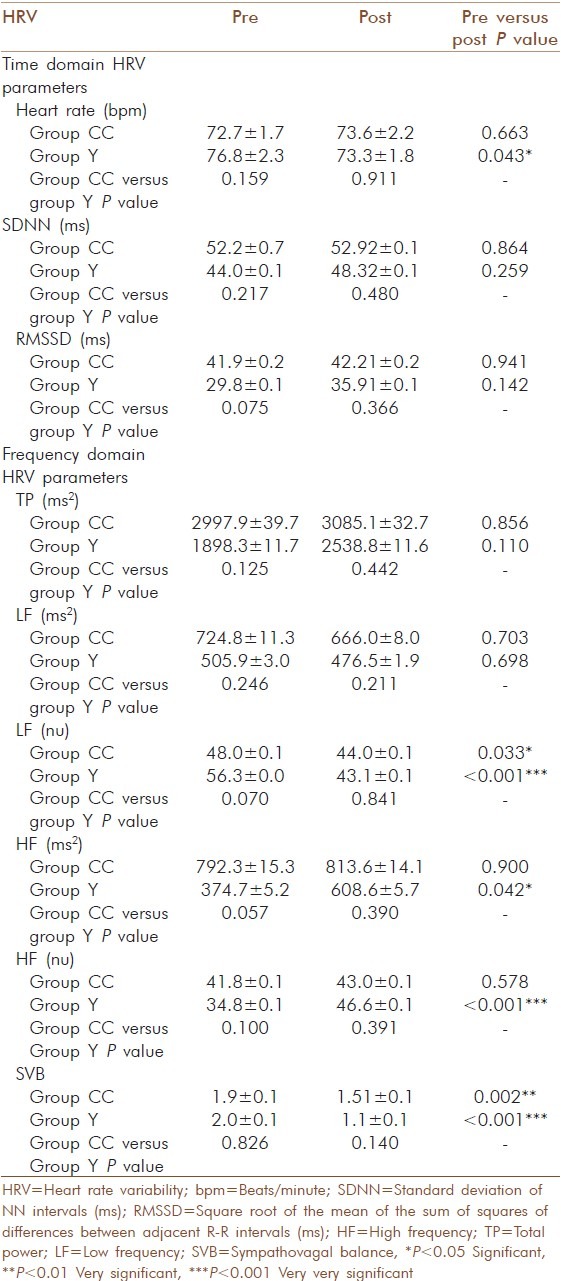
HIT score was found significantly enhanced in group CC (75.43 ± 0.88) compared to group Y 66.60 ± 3.21). No significant difference was observed in the baseline HRV parameters between two groups. Headache frequency, intensity and HIT scores were reduced in both groups of migraine patients [Table 3].
Table 3.
Effect of treatment on clinical variables
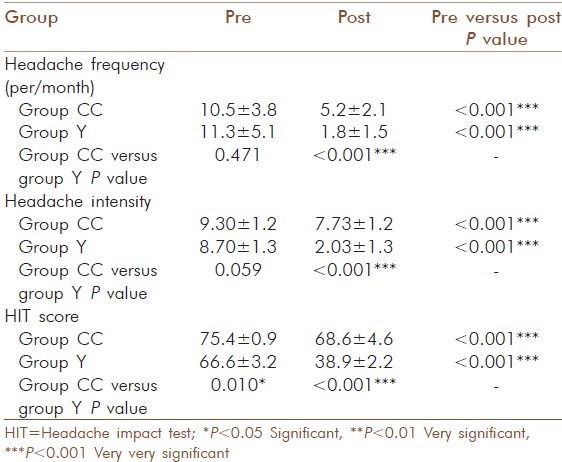
Significant reductions in monthly headache frequency, average pain intensity, and headache-related disability were seen in both the Yoga and CC care groups. However, the group Y showed improvements in all clinical outcome measures to a greater extent [Tables 4 and 5]. Significant reduction in the frequency of headache observed in the group Y compared to group CC Even the intensity of headache also reduced significantly in both groups, which was assessed by visual analogue scale (‘0’ being no pain and ‘10’ being the worst pain). At baseline headache intensity was 9.30 ± 1.15 and 8.70 ± 1.26 in Group CC and Group Y respectively. After the end of 6 weeks intervention migraine patients reported headache intensity as 7.73 ± 1.23 in group CC and 2.03 ± 1.29 in group Y. The group Y has shown significant reduction in heart rate (P < 0.05) compared to group CC. Group Y has shown more reduction in LF nu and SVB than group CC after the intervention but both group have shown statistically significant changes. Group Y has shown statistically significant increased HF power and HFnu [Table 6].
Table 4.
Comparison of self-perceived benefits of the intervention in two groups of migraine patients
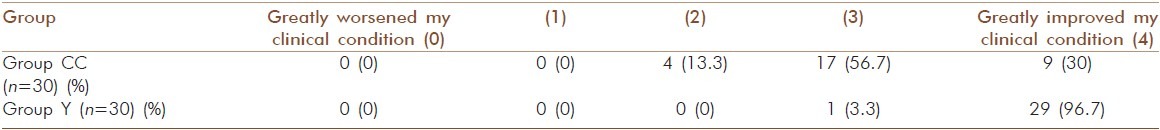
Table 5.
Comparison of the assessment of therapy by two groups of migraine patients
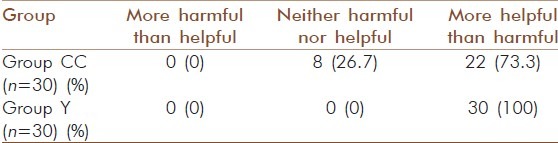
Table 6.
Effect of treatment on HRV parameters in two groups of patients
DISCUSSION
In the present study, migraine patients had very severe impact on their life (HIT score more than 60) at baseline in both the groups. After 6 weeks of intervention, both group showed statistically significant reduction of HIT score. But only Yoga with conventional care group has shown headache has little to no impact on patient's life.
The self-perceived benefit of the intervention was measured at the end of the 6-week treatment period. The patients rated the perceived benefit of the therapy on a five point scale ranging from “greatly worsened my clinical condition” to “greatly improve my clinical condition.” Migraine patients reported that intervention improved their clinical condition except 13.3% patients with conventional care only reported as neutral. In addition, patients assessed the therapy as “more harmful than helpful”, “neither harmful nor helpful,” or “more helpful than harmful.” All patients in Yoga with conventional care and 73.3% of conventional care patients told that therapy was more helpful than harmful. This infers that Yoga intervention with conventional care has better patient's improvement and in turn acceptances, than the conventional care only, without any adverse effects.
The time domain HRV parameters in Yoga with conventional care has shown significant increase in mean R-R interval and reduced heart rate compared to conventional care group at the end of 6 weeks intervention. This denotes an improved vagal tone after Yoga intervention. In frequency domain parameters HF power was increased and LF power was reduced with reduced SVB (LH/HF ratio) reflecting increased parasympathetic and reduced sympathetic tone in patient with Yoga intervention. Low frequency and SVB (LF/HF ratio) were reduced in conventional care group. Considering all HRV parameters, Yoga with conventional care has shown reduction in sympathetic tone as well as increased vagal tone. However in case of conventional care only reduction in sympathetic tone was noted, without much alteration in the vagal tone. Therefore, increasing vagal tone by Yoga intervention may improve cardiovascular health and outcomes.
Along with this the study has demonstrated that migraine patients improved clinically in both groups following 6 weeks of intervention. Reduction in the frequency and intensity was more in the Yoga with conventional care group. Clinical benefits, self-perceived health benefits and improvement in vagal tone with reduced sympathetic tone were found in Yoga with conventional care group.
For migraine treatment, regular exercise is frequently recommended. Many of the studies have reported beneficial effects of aerobic exercise on both frequency and intensity of migraine as well as on the duration of the attacks and on patient's well-being.[14,15] Reduction in pain, stress and anxiety perception in exercising persons may be due to modification in beta endorphin and hormonal secretion levels.[16,17]
However, around 22% of migraine patients complain as exercise was a trigger factor and hence some patients avoid exercise and were physically less active.[18,19] In Yoga, slower movements or even static muscular exercises are done with mindfulness and during the activities; person has to think what they are doing during the act. They also have to feel the movements and develop awareness of body and body motion.[20] Hence Yoga, a slow non-exertional aerobic exercise is more beneficial than pure aerobic exercise. Studies have shown that Yoga - type of mindful slow exercise is better than aerobic exercise or non-aerobic mindful exercise in enhancing mood and alleviating stress and depression.[17]
Yoga has been effective in numerous chronic diseases such as asthma, diabetes, arthritis, fibromyalgia, depression, ischemic heart disease etc., where stress is believed to play an important role.[21] Yoga is shown improvement quality of life, reduce the episodes of headache attack and medication score in chronic tension type headache and migraine.[22,23]
ANS is involved in control of homeostasis as the body's response to this stress and same stress can be a trigger for migraine. One of the main pain relieving factors in migraine patients is sleep and the sympathetic system drive decreases during sleep. On the other hand, relaxation techniques decrease sympathetic system drive, causing a partial relief in migraine headaches. Hence, ANS modulation either by pharmacotherapy or non-pharmacotherapy improves the symptoms.
Yoga has shown to reduce stress arousal patterns, reduce stress hormones such as cortisol[24] and bring stable autonomic balance in health[25] and diseases.[26,27] The mechanism by which Yoga practices bring the changes in ANS can be explained by the following two hypotheses - In one hypothesis, exercise training improves vagal modulation through angiotensin II and nitric oxide (NO). The mechanism of increased vagal tone by exercise may be due to reduction of angiotensin II. Angiotensin II is known to inhibit cardiac vagal activity.[28] Exercise training suppresses Angiotensin II expression.[29] Studies have shown plasma renin activity levels were lower in athletes than in untrained individuals or non-athletes and sedentary individuals. These findings were suggest that athletes with lower plasma renin activity would have lower angiotensin II and higher associated levels of cardiac vagal activity. NO may also play a role in increasing cardiac vagal control and may indirectly inhibit sympathetic influences.[30] Exercise training has been found to improve endothelial function and NO bioavailability, hence indirectly reduces sympathetic activity.[31,32] In another hypothesis, voluntary slow deep breathing and exercises reset the ANS through stretch induced inhibitory signals and hyperpolarization currents propagated through both neural and non-neural tissue which synchronizes neural elements in the heart, lungs, limbic system and cortex. During inspiration, stretching of lung tissue produces inhibitory signals by action of slowly adapting stretch receptors and hyperpolarization current by action of fibroblasts. Both inhibitory impulses and hyperpolarization current synchronize neural elements leading to the modulation of the nervous system and decreased metabolic activity i.e., parasympathetic state,[33] Human information processing during yogic exercises altered at cortical level in the hypothalamus and limbic system which in turn modulates the output of ANS, hypothalamo - pituitary axis and immune responses.[34,35]
Hence Yoga along with convention care has definite effect on migraine frequency and intensity, which were assessed by clinical scales and HRV analysis. Therefore it can reduce the dosage of drug in the conventional care and reduce the pharmacological adverse effects.
CONCLUSION
Significant clinical improvement was observed in both Yoga and Conventional care group with 6 weeks of intervention. Yoga therapy showed an additional beneficiary effect on patients with migraine by reducing frequency and intensity. Hence, Yoga therapy can be used as adjuvant therapy for migraine.
However, evaluation of autonomic parameters in patient with migraine before and after interventions was the novel one. Yoga therapy showed added benefit on autonomic modulation by improving the vagal tone. To conclude autonomic function tests can be used as prognostic indicator, in patient with migraine.
Limitations of the study
The study was not blinded and there was no sham group for Yoga therapy.
ACKNOWLEDGEMENT
Central Council for Research in Yoga and Naturopathy, Department of AYUSH, Ministry of Health and Family Welfare, Government of India, New Delhi.
Footnotes
Source of Support: Central Council for Research in Yoga and Naturopathy, Department of AYUSH, Ministry of Health and Family Welfare, Government of India, New Delhi
Conflict of Interest: None declared
REFERENCES
- 1.Headache Classification Subcommittee of the International Headache Society. The international classification of headache disorders: 2nd edition. Cephalalgia. 2004;24(Suppl 1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 2.Lipton RB, Bigal ME. Migraine: Epidemiology, impact, and risk factors for progression. Headache. 2005;45(Suppl 1):S3–13. doi: 10.1111/j.1526-4610.2005.4501001.x. [DOI] [PubMed] [Google Scholar]
- 3.Merikangas KR, Cui L, Richardson AK, Isler H, Khoromi S, Nakamura E, et al. Magnitude, impact, and stability of primary headache subtypes: 30 year prospective Swiss cohort study. BMJ. 2011;343:d5076. doi: 10.1136/bmj.d5076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Steiner TJ, Scher AI, Stewart WF, Kolodner K, Liberman J, Lipton RB. The prevalence and disability burden of adult migraine in England and their relationships to age, gender and ethnicity. Cephalalgia. 2003;23:519–27. doi: 10.1046/j.1468-2982.2003.00568.x. [DOI] [PubMed] [Google Scholar]
- 5.Lipton RB, Bigal ME, Kolodner K, Stewart WF, Liberman JN, Steiner TJ. The family impact of migraine: Population-based studies in the USA and UK. Cephalalgia. 2003;23:429–40. doi: 10.1046/j.1468-2982.2003.00543.x. [DOI] [PubMed] [Google Scholar]
- 6.Kurth T, Gaziano JM, Cook NR, Logroscino G, Diener HC, Buring JE. Migraine and risk of cardiovascular disease in women. JAMA. 2006;296:283–91. doi: 10.1001/jama.296.3.283. [DOI] [PubMed] [Google Scholar]
- 7.Breslau N, Schultz L, Lipton R, Peterson E, Welch KM. Migraine headaches and suicide attempt. Headache. 2012;52:723–31. doi: 10.1111/j.1526-4610.2012.02117.x. [DOI] [PubMed] [Google Scholar]
- 8.Mosek A, Novak V, Opfer-Gehrking TL, Swanson JW, Low PA. Autonomic dysfunction in migraineurs. Headache. 1999;39:108–17. doi: 10.1046/j.1526-4610.1999.3902108.x. [DOI] [PubMed] [Google Scholar]
- 9.Rains JC, Penzien DB. Behavioral treatment strategies for migraine and tension-type headache: A review of the evidence and future directions. Expert Rev Neurother. 2002;2:749–60. doi: 10.1586/14737175.2.5.749. [DOI] [PubMed] [Google Scholar]
- 10.Netz Y, Lidor R. Mood alterations in mindful versus aerobic exercise modes. J Psychol. 2003 Sep;137:405–19. doi: 10.1080/00223980309600624. [DOI] [PubMed] [Google Scholar]
- 11.Sathyaprabha TN, Satishchandra P, Netravathi K, Sinha S, Thennarasu K, Raju TR. Cardiac autonomic dysfunctions in chronic refractory epilepsy. Epilepsy Res. 2006;72:49–56. doi: 10.1016/j.eplepsyres.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 12.Udupa K, Sathyaprabha TN, Thirthalli J, Kishore KR, Lavekar GS, Raju TR, et al. Alteration of cardiac autonomic functions in patients with major depression: A study using heart rate variability measures. J Affect Disord. 2007;100:137–41. doi: 10.1016/j.jad.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 13.Abhishekh HA, Nisarga P, Kisan R, Meghana A, Chandran S, Trichur Raju, et al. Influence of age and gender on autonomic regulation of heart. J Clin Monit Comput. 2013;27:259–64. doi: 10.1007/s10877-012-9424-3. [DOI] [PubMed] [Google Scholar]
- 14.Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur Heart J. 1996;17:354–81. [PubMed] [Google Scholar]
- 15.Lockett DM, Campbell JF. The effects of aerobic exercise on migraine. Headache. 1992;32:50–4. doi: 10.1111/j.1526-4610.1992.hed3201050.x. [DOI] [PubMed] [Google Scholar]
- 16.Varkey E, Cider A, Carlsson J, Linde M. Exercise as migraine prophylaxis: A randomized study using relaxation and topiramate as controls. Cephalalgia. 2011;31:1428–38. doi: 10.1177/0333102411419681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Darabaneanu S, Overath CH, Rubin D, Luthje S, Sye W, Niederberger U, et al. Aerobic exercise as a therapy option for migraine: A pilot study. Int J Sports Med. 2011 Jun;32:455–60. doi: 10.1055/s-0030-1269928. [DOI] [PubMed] [Google Scholar]
- 18.Long BC, Stavel RV. Effects of exercise training on anxiety: A meta-analysis. J Appl Sport Psychol. 1995;7:167–89. [Google Scholar]
- 19.Petruzzello SJ, Landers DM, Hatfield BD, Kubitz KA, Salazar W. A meta-analysis on the anxiety-reducing effects of acute and chronic exercise. Outcomes and mechanisms. Sports Med. 1991;11:143–82. doi: 10.2165/00007256-199111030-00002. [DOI] [PubMed] [Google Scholar]
- 20.Kelman L. The triggers or precipitants of the acute migraine attack. Cephalalgia. 2007;27:394–402. doi: 10.1111/j.1468-2982.2007.01303.x. [DOI] [PubMed] [Google Scholar]
- 21.Varkey E, Hagen K, Zwart JA, Linde M. Physical activity and headache: Results from the Nord-Trøndelag Health Study (HUNT) Cephalalgia. 2008;28:1292–7. doi: 10.1111/j.1468-2982.2008.01678.x. [DOI] [PubMed] [Google Scholar]
- 22.Khalsa SB. Yoga as a therapeutic intervention: A bibliometric analysis of published research studies. Indian J Physiol Pharmacol. 2004;48:269–85. [PubMed] [Google Scholar]
- 23.Bhatia R, Dureja GP, Tripathi M, Bhattacharjee M, Bijlani RL, Mathur R. Role of temporalis muscle over activity in chronic tension type headache: Effect of yoga based management. Indian J Physiol Pharmacol. 2007;51:333–44. [PubMed] [Google Scholar]
- 24.John PJ, Sharma N, Sharma CM, Kankane A. Effectiveness of yoga therapy in the treatment of migraine without aura: A randomized controlled trial. Headache. 2007;47:654–61. doi: 10.1111/j.1526-4610.2007.00789.x. [DOI] [PubMed] [Google Scholar]
- 25.Vedamurthachar A, Janakiramaiah N, Hegde JM, Shetty TK, Subbakrishna DK, Sureshbabu SV, et al. Antidepressant efficacy and hormonal effects of Sudarshana Kriya Yoga (SKY) in alcohol dependent individuals. J Affect Disord. 2006;94:249–53. doi: 10.1016/j.jad.2006.04.025. [DOI] [PubMed] [Google Scholar]
- 26.Telles S, Nagarathna R, Nagendra HR. Breathing through a particular nostril can alter metabolism and autonomic activities. Indian J Physiol Pharmacol. 1994;38:133–7. [PubMed] [Google Scholar]
- 27.Sathyaprabha TN, Satishchandra P, Pradhan C, Sinha S, Kaveri B, Thennarasu K, et al. Modulation of cardiac autonomic balance with adjuvant yoga therapy in patients with refractory epilepsy. Epilepsy Behav. 2008;12:245–52. doi: 10.1016/j.yebeh.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 28.Sathyaprabha TN, Murthy H, Murthy BT. Efficacy of naturopathy and yoga in bronchial asthma: A self controlled matched scientific study. Indian J Physiol Pharmacol. 2001;45:80–6. [PubMed] [Google Scholar]
- 29.Townend JN, al-Ani M, West JN, Littler WA, Coote JH. Modulation of cardiac autonomic control in humans by angiotensin II. Hypertension. 1995;25:1270–5. doi: 10.1161/01.hyp.25.6.1270. [DOI] [PubMed] [Google Scholar]
- 30.Buch AN, Coote JH, Townend JN. Mortality, cardiac vagal control and physical training - What's the link? Exp Physiol. 2002;87:423–35. doi: 10.1111/j.1469-445x.2002.tb00055.x. [DOI] [PubMed] [Google Scholar]
- 31.Chowdhary S, Townend JN. Role of nitric oxide in the regulation of cardiovascular autonomic control. Clin Sci (Lond) 1999;97:5–17. [PubMed] [Google Scholar]
- 32.Kingwell BA. Nitric oxide as a metabolic regulator during exercise: Effects of training in health and disease. Clin Exp Pharmacol Physiol. 2000;27:239–50. doi: 10.1046/j.1440-1681.2000.03232.x. [DOI] [PubMed] [Google Scholar]
- 33.Routledge FS, Campbell TS, McFetridge-Durdle JA, Bacon SL. Improvements in heart rate variability with exercise therapy. Can J Cardiol. 2010;26:303–12. doi: 10.1016/s0828-282x(10)70395-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jerath R, Edry JW, Barnes VA, Jerath V. Physiology of long pranayamic breathing: Neural respiratory elements may provide a mechanism that explains how slow deep breathing shifts the autonomic nervous system. Med Hypotheses. 2006;67:566–71. doi: 10.1016/j.mehy.2006.02.042. [DOI] [PubMed] [Google Scholar]
- 35.Kulkarni DD, Bera TK. Yogic exercises and health: A psycho-neuro immunological approach. Indian J Physiol Pharmacol. 2009;53:3–15. [PubMed] [Google Scholar]


