Abstract
Background:
Nonspecific chronic low back (nCLBP) pain is prevalent among adult population and often leads to functional limitations, psychological symptoms, lower quality of life (QOL), and higher healthcare costs. The purpose of this study was to determine the efficacy of Iyengar yoga therapy on pain intensity and health related quality of life (HRQOL) with nCLBP.
Aim of the Study:
To compare the effect of Iyengar yoga therapy and conventional exercise therapy on pain intensity and HRQOL in nonspecific chronic low back pain.
Materials and Methods:
Experimental study with random sampling technique.
Subjects/Intervention:
Sixty subjects who fulfilled the selection criteria were randomly assigned to Iyengar yoga (yoga group, n = 30) and control group (exercise group, n = 30). Participants completed low back pain evaluation form and HRQOL-4 questionnaire before their intervention and again 4 weeks and 6 month later. Yoga group underwent 29 yogic postures training and exercise group had undergone general exercise program for 4 weeks.
Statistics:
Repeated measures analysis of variance (ANOVA) was used to analyze group differences over time, while controlling for baseline differences.
Results:
Patients in both groups experienced significant reduction in pain and improvement in HRQOL. In visual analogue scale (VAS) yoga group showed reduction of 72.81% (P = 0.001) as compared to exercise group 42.50% (P = 0.001). In HRQOL, yoga group showed reduction of 86.99% (P = 0.001) as compared to exercise group 67.66% (P = 0.001).
Conclusion:
These results suggest that Iyengar yoga provides better improvement in pain reduction and improvement in HRQOL in nonspecific chronic back pain than general exercise.
Keywords: Health related quality of life, Iyengar yoga, nonspecific chronic low back pain, visual analog scale
INTRODUCTION
Low back pain is a major health care problem in industrialized societies, and inadequate strength of trunk muscles appears to be related to the development of chronic low back pain. Several authors have described the important role of strong abdominal muscles in both postural control and prevention of low back injury.[1]
It is one of the most common physical ailments affecting millions of people worldwide, and constitutes a significant public health problem. It also interferes with an individual's ability to work, and negatively affects overall quality of life (QOL).
Over the last decade, yoga has been promoted with increasing enthusiasm for the treatment of low back pain. Of the various schools of yoga, Iyengar yoga is a form of hatha yoga created by BKS Iyengar and stresses on strength, balance, breathing, and alignment of the body postures.[2]
It allows the use of various assistive devices such as chairs, or blocks to aid balance and straps to facilitate stretching. It can be performed by anyone at any age and level of fitness. Because the body can be supported and balanced by these techniques, beginners can achieve many postures that would otherwise be literally, out of reach.[3]
Low back pain is a complex and individual experience that is often difficult for patients to fully describe and measurement of health-related quality of life (HRQOL) is another way to assess patients' subjective perspective on their pain experience and its adverse impact on their lives.[4] Although the therapeutic application of Iyengar yoga for nonspecific lower back pain (nCLBP) is currently offered at Iyengar Yoga Centers, there has been no published scientific evaluation of the intervention on HRQOL. Thus, the purpose of this study was to determine the efficacy of Iyengar yoga therapy on pain intensity and HRQOL with nCLBP.
MATERIALS AND METHODS
Design/setting
The study was carried out in C. U. Shah physiotherapy college outpatient department (OPD), Surendranagr, Gujarat during the period of January 2012 to December 2012. Physicians were informed about the study through pamphlets and flyers. Subjects were recruited through physicians and self-referral.
Selection criteria
The inclusion criteria were: History of nLBP with symptoms persisting for 3 months. Subjects had to be 18 years of age and ambulatory. Individuals were excluded if their LBP was due to nerve root compression, disc prolapse, spinal stenosis, tumor, spinal infection, ankylosing spondylosis, spondylolisthesis, kyphosis or structural scoliosis, or a widespread neurological disorder. Individuals were excluded if they presented as presurgical candidates, were involved in litigation or compensation, displayed a compromised cardiopulmonary system, were pregnant, had a body mass index (BMI) of more than 35, were experiencing major depression or substance abuse, and were practitioners of yoga. Ethical clearance has been obtained from the institutional scientific and ethical committee.
Randomization
Subjects signed informed consent and completed low back pain evaluation form and Health related quality of life questionnaire (HRQOL-4) during the preintervention assessment. Subjects were then randomized to yoga group (n = 30) or exercise group (n = 30) using a random number generating table. Data collectors were blind to the subject's treatment status.
Procedure
Subjects in both yoga and exercise group received lecture of 1 h duration on physical therapy education regarding CLBP, 2 weeks prior to the commencement of the program. Instructional handouts were given to help subjects use the information they received.
In addition, yoga group subjects had to attend classes by a yoga instructor (1 h per week) for 4 weeks. They were also asked to practice yoga at home (30 min, 5 days a week).
Subjects in exercise group were taught specific exercises that strengthening and stretching of the abdominal and back muscles, depending on the clinical findings and were asked to practice them for 3 days a week with five repetitions in three sets with 30-s pauses per set to begin with and repetitions were gradually increased until they reached 15 for 4 weeks.
Subjects in both the groups were asked to attend the post-intervention assessment, at the end of the program. Six months after program completion, HRQOL-4 questionnaire was mailed to all subjects. Subjects were asked to complete and return the questionnaire in stamped, self-addressed envelopes to the researchers. Results from the posttreatment and 6-month follow-up assessments were compared to baseline measurements.
Intervention
Yoga group intervention
BKS Iyengar who has taught yoga for 70 years and has applied therapeutic variations of classical poses to many health problems including CLBP.[3] It was posited that Iyengar yoga therapy would progressively rehabilitate LBP by addressing imbalances in the musculoskeletal system that affect spinal alignment and posture. The wide range of postures and supportive props employed by this method serve to enhance alignment, flexibility, mobility, and stability in all muscles and joints that affect spinal alignment and posture.
A variety of props were used including sticks, mats, belts, blocks, chairs, wall ropes, benches, boxes, stools, trestle, and weights. These props were used to provide external support to facilitate relaxation, to provide traction, and to bring awareness to specific regions of the body. Many muscle groups were targeted by Iyengar yoga with the aim of lengthening constricted or stiff muscles and strengthening core postural muscles that were underutilized including muscles of the abdomen, diaphragm, hamstrings, quadriceps, hip adductors and lateral rotators, buttocks, muscles of the lumbar, and thoracic areas of the back.
The intervention consisted of 29 postures [Table 1]. Poses from the following categories were used: Supine, seated, standing, forward bends, twists, and inversions. No back bending poses were introduced at this stage of recovery to reduce the risk of reinjury. Back bending poses require a proper progression of musculoskeletal retraining and can be harmful if done without implementation of complex musculoskeletal actions.[5]
Table 1.
Yoga postures
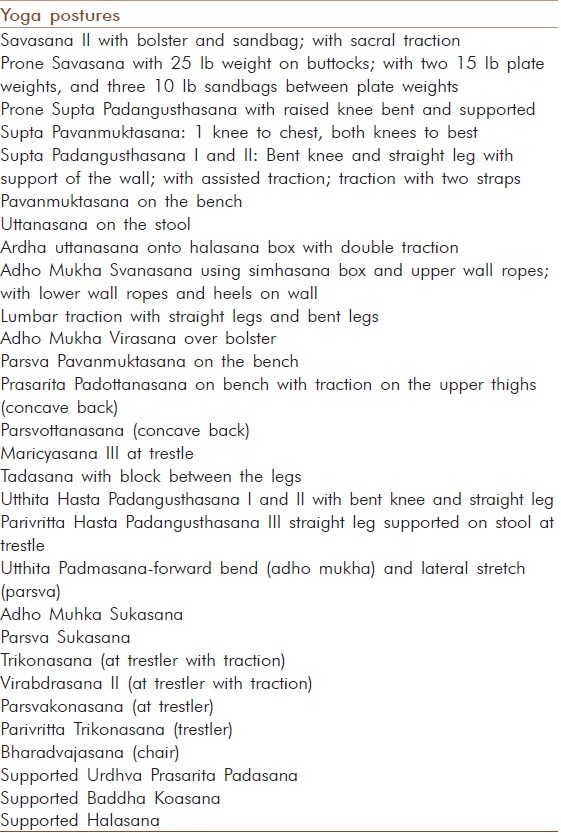
Initially, restorative poses were done to relieve pain and muscle tension. Then poses were introduced that lengthened muscles attaching to the spine and pelvis in positions with the spine fully supported. Next standing poses were introduced to open the hips and groins and to teach how to use their legs and arms to lengthen pelvic and spinal tissues. Twists were taught to access the deeper layer of back muscles to help realign the vertebra, increase inter vertebral disc space, and decrease possible impingement of nerve roots. Inversions were included to reverse the compressive effects of gravity on the intervertebral disc space. Subjects were gradually progressed from simple poses to progressively more challenging poses. Throughout the intervention, instructors focused on correcting imbalances in muscles affecting spinal alignment and posture as they were revealed in the poses. At the program end, yoga subjects were encouraged to continue yoga therapy at home.
Exercise group intervention
Exercise group (n = 30) have received strengthening and stretching of the abdominal and back muscles, depending on the clinical findings.[6] They were instructed to refrain from performing specific exercises for the low back other than those assigned for the study and to refrain from performing strenuous activities outside of normal activities of daily living.[7]
Before the exercise program, soft tissue flexibility and range of motion of these patients were increased through stretching exercises, with 5-10 min relaxation periods (warm up). The exercise program was performed 3 days a week with 5 repetitions in 3 sets with 30-s pauses per set to begin with and repetitions were gradually increased until they reached 15. During the exercises, importance of neutral spinal position was repeatedly stressed. The entire program lasted for 4 weeks.
Outcome measures
Pain intensity: The visual analogue scale (VAS) was used to measure the subject's current level of pain intensity. VAS involves a 10 cm horizontal line with no pain anchored at the left end and pain as bad as it could be anchored at the right end. The patients were asked to place a mark on the line that represented the severity of his or her pain at the moment.
-
HRQOL: In HRQOL-4, the first question asks respondents to rate their general health on a scale from excellent to poor. We dichotomized these responses as either “fair/poor” or “good/very good/excellent.” The other three questions asked about respondents' assessment of their health in the previous 30 days:
- “How many days was your physical health, which includes physical illness or injury, not good?” (Physical distress).
- “How many days was your mental health, which includes stress, depression, and problems with emotions, not good?” (Mental distress).
- “How many days did poor physical or mental health keeps you from doing your usual activities, such as self-care, work, or recreation?” (Activity limitation).
We dichotomized these three HRQOL variables in terms of their frequency in the previous 30 days (≥14 being frequent or <14 being infrequent). Jiang 2006 stated a minimum 14-day period because clinicians and clinical researchers often use this period as a marker for clinical depression and anxiety disorders, and longer duration of symptoms is associated with a higher level of activity limitation.[8] Centers for Disease Control and Prevention's (CDC) HRQOL-4 is a short, reliable, and valid tool to assess HRQOL in CLBP patients.[9]
Statistical analysis
The obtained data was analyzed with SPSS-16 for inter and intragroup comparisons. Inter group analysis was done using independent t-test and intragroup analysis was done using repeated measures ANOVA. Level of significance was fixed at 0.05.
RESULTS
Subject characteristics
Eighty subjects from the 146 referrals (self/physician) could satisfy the inclusion and exclusion criteria, and 60 among them (75%) gave the consent to be part of the study. Majority of the subjects (54, 90%) could complete the program of 4 weeks (26 in yoga and 28 in exercise group). Four subjects in the yoga group could not complete for the following reasons: Quit from the study (one), herniated disc during the study (one), and symptomatic osteoarthritis and was unwilling to perform active yoga postures for fear of aggravating the condition (two). Two subjects in the exercise group could not complete for the following reasons: Lost to follow-up (one) and became ineligible (one).
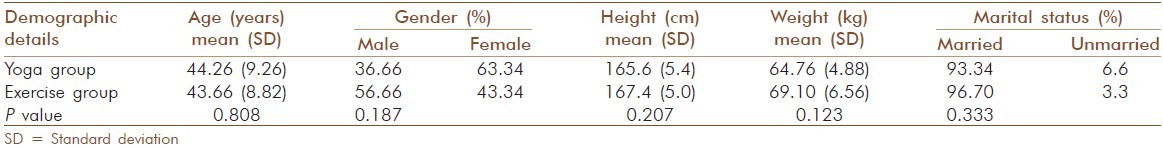
Independent t-test revealed nonsignificant differences in demographics (age, sex, height, weight, and marital status) between the yoga and exercise groups (P < 0.05) [Table 2].
Table 2.
Demographic details of group 1 and 2
Comparison of study outcomes in the yoga and control groups
No significance differences between groups were found at baseline on outcome variables such as pain intensity, physically unhealthy days, mentally unhealthy days, and activity limitation days by the yoga group compared to the exercise group. Analysis of pain intensity, physically unhealthy days, mentally unhealthy days, and activity limitation days shows significant changes within and between yoga and exercise group.
Analysis of pain intensity
At baseline, the mean VAS score was 6.73 (0.94) and 6.73 (0.90) for the yoga group and the exercise group, respectively [Figure 1]. After the 4-weeks intervention, the mean score fell to 3.8 (1.00) for the yoga group (43.54%) and to 5.3 (0.82) for the exercise group (21.25%). At the 6-month follow-up, the mean VAS score was 1.83 (1.12) for the yoga group (72.81%) and 3.87 (0.73) for the exercise group (42.50%) [Table 3]. Repeated measures ANOVA of baseline, 4 weeks and 6 months showed significant difference (P < 0.05) in both the groups.
Figure 1.

Savasana
Table 3.
Pre and post values of pain intensity and HRQOL scores in group 1 and 2
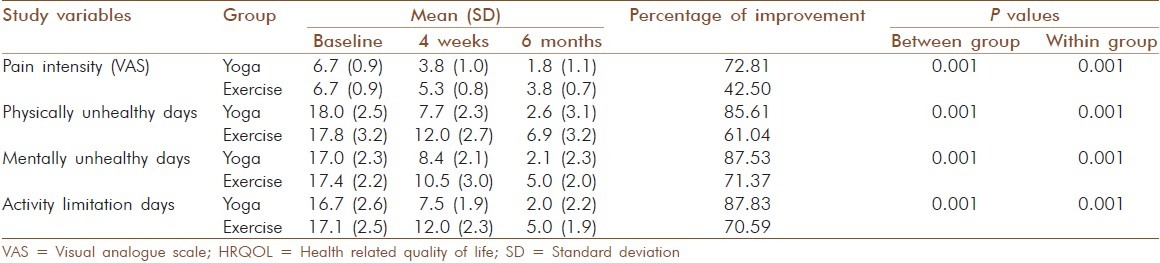
Analysis of physically unhealthy days
The mean physically unhealthy days at baseline was 18.06 (2.54) and 17.86 (3.25) for the yoga group and the exercise group, respectively [Figure 2]. After the 4-weeks intervention, the mean score fell to 7.7 (2.33) for the yoga group (57.37%) and to 12.07 (2.78) for the exercise group (32.42%). At the 6-month follow-up, the mean physically unhealthy days was 2.60 (3.13) for the yoga group (85.61%) and 6.96 (3.29) for the exercise group (61.04%) [Table 3]. Repeated measures ANOVA at baseline, after 4 weeks and 6 months shows significant difference (P < 0.05) in both the groups.
Figure 2.

Adho_Mukho_Virasana
Analysis of mentally unhealthy days
The mean mentally unhealthy days at baseline was 17.00 (2.34) and 17.46 (2.28) for the yoga and exercise group, respectively [Figure 2]. After the 4-weeks intervention, the mean score fell to 8.46 (2.12) for the yoga group (50.24%) and to 10.53 (3.01) for the exercise group (39.7%). At the 6-month follow-up, the mean mentally unhealthy days was 2.12 (2.38) for the yoga group (87.53%) and 5.00 (2.09) for the exercise group (71.37%) [Table 3]. Repeated measures ANOVA at baseline, after 4 weeks and 6 months shows significant difference (P < 0.05) in both the groups.
Analysis of activity limitation days
The mean activity limitation days at baseline was 16.76 (2.68) and 17.10 (2.57) for the yoga group and the exercise group, respectively [Figure 2]. After the 4-weeks intervention, the mean score fell to 7.53 (1.96) for the yoga group (55.08%) and to 12.03 (2.30) for the exercise group (29.69%). At the 6-month follow-up, the mean activity limitation days was 2.04 (2.22) for the yoga group (87.83%) and 5.03 (1.91) for the exercise group (70.59%) [Table 3]. Repeated measures ANOVA at baseline, after 4 weeks and 6 months shows significant difference (P < 0.05) in both the groups.
DISCUSSION
The results of the study support the hypothesis that yoga therapy confers greater benefits to HRQOL in CLBP patients. It was demonstrated that 4-week yoga therapy intervention caused a significant reduction in pain intensity, physically unhealthy days, mentally unhealthy days, and activity limitation days compared to the control group. The significant improvements by yoga subjects were maintained at the 6-month follow-up, indicating that the yoga intervention is associated with longer lasting reductions in pain outcomes and QOL than controlled intervention.
In addition, the majority of subjects in the yoga group rated yoga as having a large impact on their LBP and as having great importance to the management and recovery of LBP. Improvements in several outcome variables compared favorably to similar studies using active treatment strategies such as exercise, physical therapy protocols incorporating flexibility and strengthening exercises, and cognitive behavioral therapy.
The reduction in pain intensity due to yoga was greater or equal to the reduction reported in the studies reported here.[10,11] Present findings of decreased pain and improvement in HRQOL following yoga reflect reported decreases in pain status[12] and improvement in HRQOL[13] after yoga.
Iyengar (1976) claims that the standing poses are crucial for recovery from LBP, it is challenging to obtain the correct alignment in the posture that is necessary for pain relief in the learning phase. In such a short intervention, discomfort from improper alignment may have reduced perceived efficacy of yoga intervention on long-held negative cognitions and beliefs about the efficacy of yoga on CLBP. We also believe that efficacy of yoga intervention would be enhanced by doing fewer and less challenging poses.
Other interventions for LBP that have been evaluated in high-quality randomized, controlled trials include exercise and manipulation,[14] the Alexander technique,[15] and cognitive behavioral treatment.[16] Comparing the findings of this study with these other interventions suggests that group yoga may improve in outcome variables than exercise and manipulation, cognitive behavioral treatment, and six sessions of 1-to-1 Alexander technique.
Future studies should be done to determine whether yoga therapy can alter behavioral changes and to determine the mechanisms responsible for the behavioral effects of Iyengar yoga therapy on nCLBP.
CONCLUSION
These results suggest that Iyengar yoga provides better improvement in pain reduction and HRQOL in nonspecific chronic back pain than general exercise.
ACKNOWLEDGEMENT
I would like to thank the all the subjects and my friends who worked tirelessly to make this study a success.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Foster DN, Fulton MN. Back pain and the exercise prescription. Clin Sport Med. 1991;10:197–209. [PubMed] [Google Scholar]
- 2.Signet Market Research. Yoga survey 2000. Yoga Journal. 2000 [Google Scholar]
- 3.Iyengar BK. Light on yoga. New York: Schocken Books; 1976. [Google Scholar]
- 4.Turk DC, Okifuji A. Psychological aspects of pain. In: Warfield CA, Bajwa ZH, editors. Principles and Practice of Pain Medicine. New York: McGraw-Hill; 2004. pp. 139–56. [Google Scholar]
- 5.Williams K, Steinberg L, Petronis J. Therapeutic application of Iyengar yoga for healing chronic low back pain. Int J Yoga Ther. 2003;13:55–67. [Google Scholar]
- 6.Sahrmann SA. “Diagnosis and Treatment of Movement Impairment Syndromes”. St. Louis: Mosby; 2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mayer JM, Ralph L, Look M, Erasala GN, Verna JL, Matheson LN, et al. Treating acute low back pain with continuous low-level heat wrap therapy and/or exercise: A randomized controlled trial. Spine J. 2005;5:395–403. doi: 10.1016/j.spinee.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 8.Jiang Y, Hesser JE. Associations between health-related quality of life and demographics and health risks. Results from Rhode Island's 2002 behavioral risk factor survey. Health Qual Life Outcomes. 2006;4:14. doi: 10.1186/1477-7525-4-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aslan UB, Cavlak U, Yagci N. Reliability and validity of the Turkish version of the CDC HRQOL-4 scale in patients with chronic low back pain. Pak J Med Sci. 2010;26:875–9. [Google Scholar]
- 10.Frost H, Klaber Moffett JA, Moser JS, Fairbank JC. Randomized controlled trial for evaluation of fitness programme for patients with chronic low back pain. BMJ. 1995;310:151–4. doi: 10.1136/bmj.310.6973.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kankaanpaa M, Taimela S, Airaksinen O, Hanninen O. The efficacy of active rehabilitation in chronic low back pain. Effect on pain intensity, self experienced disability, and lumbar fatigability. Spine (Phila Pa 1976) 1999;24:1034–42. doi: 10.1097/00007632-199905150-00019. [DOI] [PubMed] [Google Scholar]
- 12.Vidyasagar JV, Prasad BN, Reddy V, Raju PS, Jayshankar M, Sampath K. Effects of yoga practices in non-specific low back pain. Clin Proc NIMS. 1989;4:160–4. [Google Scholar]
- 13.Patel NK, Newstead AH, Ferrer RL. The effects of yoga on physical functioning and health related quality of life in older adults: A systematic review and meta-analysis. J Altern Complement Med. 2012;18:902–17. doi: 10.1089/acm.2011.0473. [DOI] [PubMed] [Google Scholar]
- 14.UK BEAM Trial Team. United Kingdom back pain exercise and manipulation (UK BEAM) randomised trial: Effectiveness of physical treatments for back pain in primary care. BMJ. 2004;329:1377. doi: 10.1136/bmj.38282.669225.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Little P, Lewith G, Webley F, Evans M, Beattie A, Middleton K, et al. Randomised controlled trial of Alexander technique lessons, exercise, and massage (ATEAM) for chronic and recurrent back pain. BMJ. 2008;337:a884. doi: 10.1136/bmj.a884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lamb SE, Hansen Z, Lall R, Castelnuovo E, Withers EJ, Nichols V, et al. Back Skills Training Trial investigators. Group cognitive behavioural treatment for low-back pain in primary care: A randomised controlled trial and cost effectiveness analysis. Lancet. 2010;375:916–23. doi: 10.1016/S0140-6736(09)62164-4. [DOI] [PubMed] [Google Scholar]


