Abstract
Myofascial Pain Syndrome (MPS) refers to pain attributed to muscle and its surrounding fascia, which is associated with “myofascial trigger points” (MTrPs). MTrPs in the trapezius has been proposed as the main cause of temporal and cervicogenic headache and neck pain. Literature shows that the prevalence of various musculoskeletal disorders (MSD) among physiotherapists is high. Yoga has traditionally been used to treat MSDs in various populations. But there is scarcity of literature which explains the effects of yoga on reducing MPS of the neck in terms of various physical parameters and subjective responses. Therefore, a pilot study was done among eight physiotherapists with minimum six months of experience. A structured yoga protocol was designed and implemented for five days in a week for four weeks. The outcome variables were Disability of Arm, Shoulder and Hands (DASH) score, Neck Disability Index (NDI), Visual Analogue Scale (VAS), Pressure Pain Threshold (PPT) for Trigger Points, Cervical Range of Motion (CROM) - active & passive, grip and pinch strengths. The variables were compared before and after the intervention. Finally, the result revealed that all the variables (DASH: P<0.00, NDI: P<0.00, VAS: P<0.00, PPT: Left: P<0.00, PPT: Right: P<0.00, Grip strength: left: P<0.00, Grip strength: right: P<0.01, Key pinch: left: P<0.01, Key pinch: right: P<0.01, Palmar pinch: left: P<0.01, Palmar pinch: right: P<0.00, Tip pinch: left: P<0.01, Tip pinch: Right: P<0.01) improved significantly after intervention.
Keywords: Myofascial pain syndrome, physiotherapist, yoga
INTRODUCTION
Pain attributed to muscle and its surrounding fascia is termed as Myofascial Pain. Myofascial Pain Syndrome (MPS) is one of the most common, non-articular forms of musculoskeletal pain.[1,2] Cervical myofascial pain occurs due to either overuse or trauma to the muscles that support the shoulders and neck.[3] MPS is associated with ‘hyperirritable spots’ or ‘trigger points’ (MTrPs) within palpable taut bands of the skeletal muscle or fascia that are painful on compression. These can give rise to characteristic referred pain, tenderness or autonomic nervous system symptoms.[4] Furthermore, MTrPs in the trapezius has been proposed as the main cause of temporal headache,[5] cervicogenic headaches, and neck pain.[6,7] The cervical myofascial pain syndrome is very common in the general population.[8] Cervical pain (neck pain) is the second most common, work-related musculoskeletal disorder in the world. Similar to other Work-Related Musculoskeletal Disorders (WRMSD), the risk factors for the development of neck pain are repetition, awkward posture, static posture, force, long duration of exposure, psychosocial risk factors, and other non-occupational factors. Tasks that need repetition of movement, demand of precision or repetitive light lifting are more likely to lead to MPS, especially in the shoulder and neck region.[9] Previous studies have shown that the prevalence of various musculoskeletal disorders (MSD) among physiotherapists is high.[10,11,12] Physiotherapy is a process of treating patients manually. In this process the therapist often exerts extensive force, in a static awkward posture, while treating the patient. In addition, physiotherapists are exposed to other risk factors such as lifting, carrying, bending, and twisting, lack of reporting of injury, self-treatment, long working hours, and treating many patients in a single shift.[13] These factors are considered to be responsible for the development of musculoskeletal discomfort including neck pain, which is often myofascial in nature. It is further stated in literature that the prevalence of neck pain, including MPS, among physiotherapists is very high; it varies from 15 to 48%.[14,15,16] Musculoskeletal disorders among the workforce affect the performance, productivity, and quality of work,[17,18,19,20,21] which is applicable for the physiotherapists as well. To maintain the quality of work (treatment of the patients), the physiotherapist needs to be free of pain and discomfort. Therapists suffering from musculoskeletal pain often change the way of working, which may adversely affect the quality of treatment. Studies have also shown that MSDs among physiotherapists often lead to early retirement or change in profession.[22] Yoga has been traditionally used to treat MSDs in various populations. However, there is scarcity of literature that explains the effect of yoga on reducing specific MSDs like the Cervical Myofascial Pain Syndrome in terms of various physical parameters and subjective responses.[23] Keeping that in mind a pilot study was planned, to evaluate the effect of yoga on relieving pain, improving the quality of life and productivity among physiotherapists diagnosed to have the cervical myofascial pain syndrome.
SUBJECTS AND METHODS
Study Setting: Tertiary Rehabilitation Center
Study Population: Physiotherapists with cervical myofascial pain syndrome
Recruitment strategy
Inclusion criteria
-
Physiotherapists suffering from the cervical myofascial pain syndrome were included. The diagnosis of MPS was made by an Orthopedic/Rehabilitation Specialist (more than ten years experience treating MPS) using the Simons Criteria,[24] that required five major and at least one of the four minor criteria to be satisfied.
Major criteria:
- Localized spontaneous pain
- Spontaneous pain or altered sensations in the expected referred pain area for the given MTrP
- Taut, palpable band in the accessible muscle
- Exquisite, localized tenderness in a precise point along the taut band
- Some measurably reduced movement range.
Minor criteria:
- Reproduction of spontaneously perceived pain and altered sensations by pressure on MTrP
- Elicitation of local twitch response of muscular fibers by transverse ‘snapping’ palpation or by needle insertion into the MTrP
- Pain relief obtained by muscle stretching or dry dry-needling injection of the MTrP
- Electromyographic demonstration of spontaneous electrical activity, characteristic of active loci in the tender nodule of a taut band in the muscle
Physiotherapists treating more than five patients in a day
Minimum six months of professional experience
Age between 20 years to 35 years.
Exclusion criteria
Diagnosis of any other musculoskeletal disorders
Any other associated problems such as vertebral basilar insufficiency, articular instability, significant cervical spondylosis or arthritis
Any other systemic health problems.
Ethics
The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation. Approval was obtained from the Institutional Review Board before starting the study.
Procedure
Physiotherapists working at a Tertiary Rehabilitation Center, who complained of neck pain, were assessed for the presence of cervical myofascial pain syndrome based on the Simon's Criteria. Ten physiotherapists who were diagnosed with having cervical myofascial pain syndrome were selected, of whom two dropped out due to reasons unrelated to the study, that is, change of employment. Hence, a total of eight physiotherapists with cervical myofascial pain syndrome participated in this study. All the methods and modalities of the experiment were explained to the subjects and signed informed consent was obtained from all the participants. The data collection was handled by a single researcher, to avoid interpersonal bias. The outcome measures were Instrumented Cervical Range of Motion (CROM) - active and passive, Hand Grip and Pinch Strength, using a Jamar Dynamometer (a mechanical dynamometer), Pain Threshold for Trigger Points using a Wagner Pressure Algometer (an instrument for measuring sensitivity to pressure), Disability of Arm, Shoulder, and Hands (DASH) score, Neck Disability Index (NDI), and Short Form 36 (SF 36). Before starting the intervention, all the subjects were asked to fill up a questionnaire, which comprised of DASH, NDI, and SF 36, and the investigators performed the objective measurements. All the parameters were again measured after completion of the intervention.
Program
All the subjects were asked to report to the laboratory fifteen minutes before starting the intervention. The intervention was a four-week program of Hatha Yoga, which included prānāyāma, āsanās, and meditation, specific for the cervical region, for one hour per day. The program, for the first two weeks, was prānāyāma (Anulom Vilom and Nadi Shodhan Pranayama, and Diaphramatic Breathing explained in Figure 1) and Relaxation Training (Shāvasan - Body Scanning, Imagery techniques;Figure 2). In the third and the fourth weeks āsanās (Trikonasan, Tadasan, Vakrasan, Balasan and Vajrasan explained in Figures 3–6), prānāyāma and Relaxation Training were taught. All the āsanās were taught according to the participant's comfort level.
Figure 1.

Anulom- Vilom Pranayam
Figure 2.

Shavasana
Figure 3.

Balasan
Figure 6.

Vakrasan
Figure 4.

Tadasan
Figure 5.

Trikonasan
Measures
Grip strength: Grip strength was measured by the Jamar Hand Grip Dynamometer.[25,26]
Pinch strength: Pinch strength was measured by Jamar Pinch Meter.[27]
Cervical range of motion: Cervical Ranges of Motion (rotation, flexion, extension, and lateral bending) were measured by a Magnetic Inclinometer.[28]
The algometer pain test: (From Wagner Instruments, USA) was performed on prone subjects with TrP areas exposed. Pressure was applied perpendicularly and gradually through an Algometer (1.0 cm2 tip) at each palpated point. When a subject verbally cued pain onset, the pressure level was noted.
Visual Analog Scale (VAS): This is a 10 cm Horizontal line representing the extreme left as ‘no discomfort’ and extreme right as ‘maximum discomfort’. It is a well-validated scale for pain measurement.[29]
Disability of arm, shoulder, and hand: The Disability of Arm, Shoulder, and Hands (DASH) is a questionnaire developed and validated in 1994, by the American Academy of Orthopedic Surgeons, the Council of Musculoskeletal Specialty Societies, and the Institute for Work and Health.[20] DASH was developed to measure physical disability and symptoms of the upper limbs in a heterogeneous population, that is, men and women, and individuals with mild, moderate or severe disability and a wide variety of upper extremity disorders.[31]
Neck disability index: The Neck Disability Index (NDI) was designed to measure neck-specific disability.[32] It was developed from the Oswestry Index[33] for back pain and the Pain Disability Index.[34] The authors were from the Canadian Memorial Chiropractic College in Toronto, Canada. This questionnaire contained ten individual factors concerning pain and activities of daily living, including personal care, lifting, reading, headaches, concentration, work status, driving, sleeping, and recreation, on a six-point Likert scale. Its reliability and validity is well-established.[35]
SF-36: The SF-36 is a multipurpose, short-form health survey, with 36 questions. The experience to date with the SF-36 has been documented in nearly 4000 publications. The two overall health consistent summary scores — Physical Health and Mental Health — were the average of four subscales each. The Physical Heath scale was comprised of physical functioning, role-physical, bodily pain, and general health; Mental Health was comprised of social functioning, role-emotional, mental well-being, and vitality. All items were rated on a five-point scale, with five representing better health. The internal reliability, construct validity, and changes in disease-related symptoms, over time, of the SF-36, have been well-documented.[36]
Statistical tool
Comparative and inferential statistics were carried out using the Statistical Package for Social Studies (SPSS) 17.0.
RESULTS
The total number of participants in this study was eight. All the subjects attended all the given sessions on a regular basis. The demographic data of the subjects is presented in Table 1.
Table 1.
Demographic data
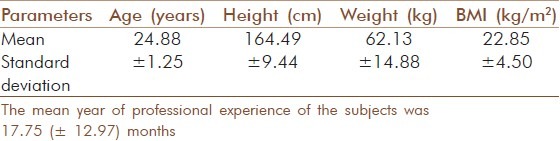
All the outcome measures were compared before starting the treatment and after finishing the treatment. All the outcome measures were compared using the paired t-test. The results are presented in Tables 2–6.
Table 2.
Comparison of grip and pinch strength
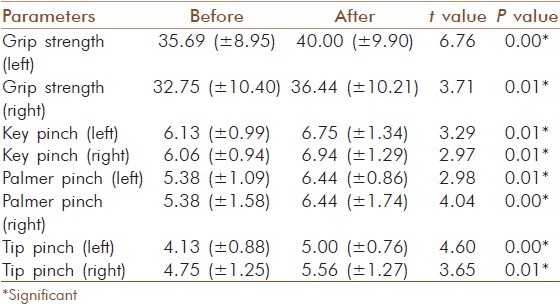
Table 6.
Result of SF 36
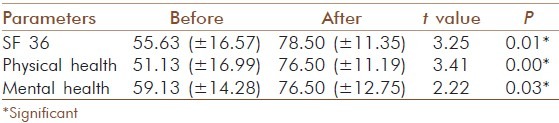
Table 3.
Comparison of cervical range of motion
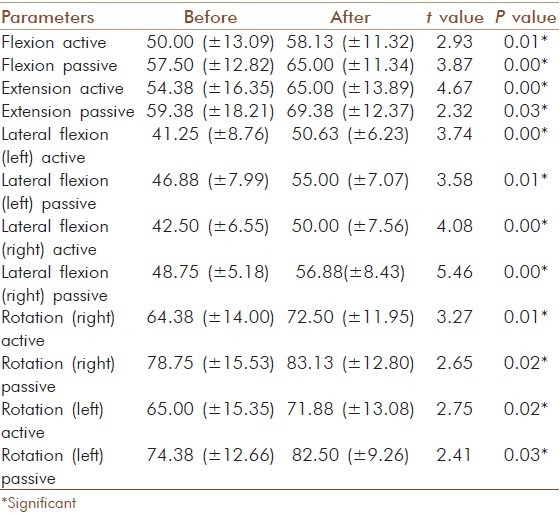
Table 4.
Result of algometry and visual analog scale
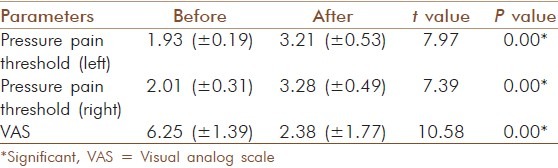
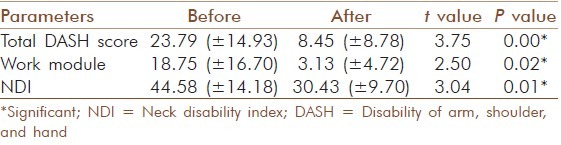
Table 5.
Result of disability of arm, shoulder, and hand and neck disability index
The above table revealed that grip and pinch strength (key, palmar, and tip) for both the hands improved significantly from the baseline condition to the end of intervention.
The above table revealed that both the active and passive range of motion for all the cervical movements improved from the baseline to the end of intervention.
The result of pressure algometry and visual analog scale also showed improvement from the baseline to the end of intervention.
Disability of arm, hand, shoulder and neck also reduced significantly as compared to the baseline levels.
The above table revealed that there was an improvement in the Physical and Mental Health along with the Total Score of SF 36.
DISCUSSION
The results of the present study suggested that the intervention of a planned yoga program led to significant improvement in the quality of health, physical capacity (strength), cervical range of motion, and pressure threshold of the trigger points, and decreased the disability and pain for the physiotherapists who were diagnosed to have cervical myofascial pain syndrome. Several reasons exist to explain the efficacy of Yoga in the therapy for cervical myofascial pain. In the cervical myofascial pain syndrome, breathing is invariably strained, shallow, and mainly thoracic, which in turn affects other rhythmic phenomena like neuronal flow and vital cyclic rhythms with high flat cortisol levels, similar to the chronic arousal response.[37,38] Āsanās and prānāyāma activates the Parasympathetic system, by increasing the local blood flow, which influences the endocrine system and nerve plexuses, affecting the neuronal flow.[39] Deep yogic breathing with prolonged exhalation relaxes most of the skeletal muscles.[40] Āsanās and prānāyāma initiate a ‘relaxation response’[41] in the neuroendocrinal system that harmonizes the physiological system (metabolic, respiratory, cardiovascular, musculoskeletal, and neural) resulting in decreased myofascial tension.[42] Meditation and pranayama, along with relaxing asanas can help individuals deal with the reactive aspects of chronic pain, reducing anxiety and depression effectively.[43] Hatha yoga improves strength, range of motion, balance, and agility, reduces pain, enhances flexibility, muscle tones, and releases muscle tension.[44,45,46,47] Mindfulness meditation helps in the reduction of pain, improvement in physical function, and the quality of life.[48,49] Meditation and prānāyāma have both been found to be helpful in pain management.[39,50] Meditation and prānāyāma techniques included in this intervention study have increased the participants’ mindfulness. The subjects who practice yoga learn about mental focus, which helps people to increase their awareness of non-optimal ways of moving and positioning their body. Subjects also learn how to relax tensed muscles, and to relieve mental stress.[51,52] Moreover, yoga therapy encourages the subjects to heal by resting the area of pain and teaches the proper alignment of bones, muscles, and connective tissues, in movements that minimize the risk factors for discomfort. Therefore, it helps in minimizing and ultimately correcting the underlying physical malfunctions.[53] A study carried out by Kabat-Zinn showed that 65% of the patients with chronic pain, who had not improved with traditional medical care, felt lesser pain after practicing mindfulness meditation for ten weeks.[54] In the present study also similar results were found, which were measured with subjective responses and quantified by a visual analog scale. Apart from pain reduction, there was a significant improvement in the functional capacity and quality of health. Therefore, it was concluded that a planned yoga program for physiotherapists who were suffering from cervical myofascial pain syndrome resulted in significant improvement in pain levels, which in turn could lead to improved quality of treatment. The sample size of the present study was only eight and there was no control group. Therefore, a further study is required to generalize the result of the present study on a larger sample size.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Fricton JR. Myofascial pain syndrome. Neurologic Clinics. 1989;7:413–27. [PubMed] [Google Scholar]
- 2.Shah JP, Danoff JV, Desai MJ, Parikh S, Nakamura LY, Phillips TM, et al. Biochemicals associated with pain and inflammations are elevated in sites near to and remote from active myofascial trigger points. Arch Phys Med Rehabil. 2008;89:16–23. doi: 10.1016/j.apmr.2007.10.018. [DOI] [PubMed] [Google Scholar]
- 3.Duyur CB, Genc H, Altuntas V. Disability and related factors in patients with chronic cervical myofascial pain. Clin Rheumatol. 2009;28:647–54. doi: 10.1007/s10067-009-1116-0. [DOI] [PubMed] [Google Scholar]
- 4.Simons DG. Myofascial pain syndrome: One term but two concepts: A new understanding. J Musculoskeletal Pain. 1995;3:7–13. [Google Scholar]
- 5.Wolfe F, Simons DG, Fricton J, Bennett RM, Goldenberg DL, Gerwin R, et al. The fibromyalgia and myofascial pain syndromes: A preliminary study of tender points and trigger points in persons with fibromyalgia, myofascial pain syndrome and no disease. J Rheumatol. 1992;19:944–51. [PubMed] [Google Scholar]
- 6.Grosshandler SL, Stratas NE, Toomey TC, Gray WF. Chronic neck and shoulder pain: Focusing on myofascial origins. Postgrad Med. 1985;77:149–58. doi: 10.1080/00325481.1985.11698897. [DOI] [PubMed] [Google Scholar]
- 7.Gerwin RD, Dommerholt J, Shah JP. An expansion of Simons’ integrated hypothesis of trigger point formation. Curr Pain Headache Rep. 2004;8:468–75. doi: 10.1007/s11916-004-0069-x. [DOI] [PubMed] [Google Scholar]
- 8.Wright EF. Referred craniofacial pain patterns in patients with temporomandibular disorder. J Am Dent Assoc. 2000;131:1307–15. doi: 10.14219/jada.archive.2000.0384. [DOI] [PubMed] [Google Scholar]
- 9.Henriksson KG, Bäckman E, Henriksson C, de Laval JH. Chronic regional muscular pain in women with precise manipulation work. Scand J Rheumatol. 1996;25:213–23. doi: 10.3109/03009749609069990. [DOI] [PubMed] [Google Scholar]
- 10.Bork BE, Cook TM, Rosecrance JC, Engelhardt KA. Work-related muscu-loskeletal disorders among physical therapists. Phys Therapy. 1996;76:827–35. doi: 10.1093/ptj/76.8.827. [DOI] [PubMed] [Google Scholar]
- 11.Cromie JE, Robertson VJ, Best MO, Best MO. Work-related musculoskeletal disorders in physical therapists: Prevalence severity, risks and responses. Phys Therapy. 2000;80:335–6. doi: 10.1093/ptj/80.4.336. [DOI] [PubMed] [Google Scholar]
- 12.Holder NL, Clark HA, DiBlasio JM, Hughes CL, Scherpf JW, et al. Cause prevalence, and response to occupational musculoskeletal injuries reported by physical therapists and physical therapist assistants. Physical Therapy. 1999;79:642–52. doi: 10.1093/ptj/79.7.642. [DOI] [PubMed] [Google Scholar]
- 13.Cromie JE, Robertson VJ, Best MO. Occupational health in physiotherapy: General health and reproductive outcomes. Aust J Physiother. 2002;48:287–94. doi: 10.1016/s0004-9514(14)60168-9. [DOI] [PubMed] [Google Scholar]
- 14.Alrowayeh HN, Alshatti TA, Aljadi SH, Fares M, Alshamire MM, Alwazan SS. Prevalence, characteristics, and impacts of work-related musculoskeletal disorders: A survey among physical therapists in the State of Kuwait. BMC Musculoskelet Disord. 2010;11:116. doi: 10.1186/1471-2474-11-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cromie JE, Robertson VJ, Best MO. Occupational health and safety in physiotherapy: Guidelines for practice. Aust J Physiother. 2001;47:43–51. doi: 10.1016/s0004-9514(14)60297-x. [DOI] [PubMed] [Google Scholar]
- 16.Nordin NAM, Leonard JH, Thye NC. Work-related injuries among physiotherapists in public hospitals-a Southeast Asian picture. Clinics (Sao Paulo) 2011;66:373–8. doi: 10.1590/S1807-59322011000300002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holden L, Scuffham PA, Hilton MF, Ware RS, Vecchio N, Whiteford HA. Health-related productivity losses increase when the health condition is co-morbid with psychological distress: Findings from a large cross-sectional sample of working Australians. BMC Public Health. 2011;11:417. doi: 10.1186/1471-2458-11-417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rolander B. Work conditions, musculoskeletal disorders and productivity of dentists in public dental care in Sweden. http://www.imh.liu.se . ISBN 2010;978-91-7393-348-3.
- 19.van den Heuvel SG, Ijmker S, Blatter BM, de Korte EM. Loss of productivity due to neck/shoulder symptoms and hand/arm symptoms: Results from the PROMO-Study. J of Occup Rehabil. 2007;17:370–82. doi: 10.1007/s10926-007-9095-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. www.goodhealthsolutions.com.au .
- 21. www.perosh.eu .
- 22.West DJ, Gardner D. Occupational injuries of physiotherapists in North and Central Queensland. Aust J Physiother. 2001;47:179–86. doi: 10.1016/s0004-9514(14)60265-8. [DOI] [PubMed] [Google Scholar]
- 23. http://osha.europa.eu .
- 24.Simons DG, Travell JG, Simons LS. Travell and Simons’ myofascial pain and dysfunction: The trigger point manual. 2nd ed. Baltimore, MD: Williams and Wilkins; 1999. [Google Scholar]
- 25.Crosby CA, Wehbk MA, Mawr B. Hand strength: Normative values. J Hand Surg Am. 1994;19:665–70. doi: 10.1016/0363-5023(94)90280-1. [DOI] [PubMed] [Google Scholar]
- 26.Newman DG, Pearn J, Barnes A, Young CM, Kehoe M, Newman J. Norms for hand grip strength. Arch Dis Child. 1984;59:453–9. doi: 10.1136/adc.59.5.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Debra LH, Kratt A, Bix L. Inter-rater reliability of students using hand and pinch dynamometers. Am J Occup Ther. 2009;63:193–7. doi: 10.5014/ajot.63.2.193. [DOI] [PubMed] [Google Scholar]
- 28.Chiu TT, Sing KL. Evaluation of cervical range of motion and isometric neck muscle strength: Reliability and validity. Clin Rehabil. 2002;16:851–8. doi: 10.1191/0269215502cr550oa. [DOI] [PubMed] [Google Scholar]
- 29.Boonstra AM, Schiphorst Preuper HR, Reneman MF, Posthumus JB, Stewart RE. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int J Rehabil Res. 2008;31:165–9. doi: 10.1097/MRR.0b013e3282fc0f93. [DOI] [PubMed] [Google Scholar]
- 30.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: The DASH (Disabilities of the Arm, Shoulder and Hand) [corrected], The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29:602–8. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 31.McDowell I, Newell C. Measuring health: A guide to rating scales and questionnaires. 2nd ed. Oxford: Oxford University Press; 1996. [Google Scholar]
- 32.Vernon H, Mior S. The Neck Disability Index: A study of reliability and validity. J Manipulative Physiol Ther. 1991;14:409–15. [PubMed] [Google Scholar]
- 33.Fair bank JC, Couper J, Davis JB, O’Brien JP. The Oswestry Low Back Pain disability questionnaire. Physiotherapy. 1980;66:271–3. [PubMed] [Google Scholar]
- 34.Chibnall JT, Tait RC. The Pain Disability Index: Factor structure and normative data. Arch Phys Med Rehabil. 1994;75:1082–6. doi: 10.1016/0003-9993(94)90082-5. [DOI] [PubMed] [Google Scholar]
- 35.Hains F, Waalen J, Mior S. Psychometric properties of the neck disability index. J Manipulative Physiol Ther. 1998;21:75–80. [PubMed] [Google Scholar]
- 36.Sharan D, Jacob BN, Ajeesh PS, Jack B, Bookout RR. The effect of cetylated fatty esters and physical therapy on myofascial pain syndrome of the neck. J Bodyw Mov Ther. 2011;15:363–74. doi: 10.1016/j.jbmt.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 37.Arambula P, Peper E, Kawakami M, Gibney KH. The physiological correlates of Kundalini Yoga meditation: A study of a yoga master. Appl Psychophysiol Biofeedback. 2001;26:147–53. doi: 10.1023/a:1011343307783. [DOI] [PubMed] [Google Scholar]
- 38.Udupa KN, Singh RH, Settiwar RM. Studies on the effect of some yogic breathing exercises (Pranayama) in normal persons. Indian J Med Res. 1975;63:1062–5. [PubMed] [Google Scholar]
- 39.Vallath N. Perspectives on Yoga inputs in the management of chronic pain. Indian J Palliat Care. 2010;16:1–7. doi: 10.4103/0973-1075.63127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nespor K. Psychosomatics of back pain and the use of yoga. Int J Psychosom. 1989;36:72–8. [PubMed] [Google Scholar]
- 41.Benson H. Timeless healing: The power and biology of belief. New York: Scribner; 1996. Timeless healing: The power and biology of belief. [Google Scholar]
- 42.Lazar SW, Bush G, Gollub RL, Fricchione GL, Khalsa G, Benson H. Functional brain mapping of the relaxation response and meditation. Neuroreport. 2000;11:1581–5. [PubMed] [Google Scholar]
- 43.Kim DH, Moon YS, Kim HS, Jung JS, Park HM, Suh HW, et al. Effect of Zen Meditation on serum nitric oxide activity and lipid peroxidation. Prog Neuropsychopharmacol Biol Psychiatry. 2005;292:327–31. doi: 10.1016/j.pnpbp.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 44.Ananthanarayanan TV, Srinivasan TM. Asana-based exercises for the management of low-back pain.:International Association of Yoga Therapists 1994;4:6-15 in Schultz LH, Uyterhoeven S and Sat Khalsa BS, Evaluation of a Yoga Program for Back Pain. J Yoga Phys Therapy. 2011;1(2) http://dx.doi.org/10.4172/2157-7595.1000e103 . [Google Scholar]
- 45.Globus S. What yoga can do for you. Current Health. 2000;2:30. [Google Scholar]
- 46.Spilner M. Flex away back pain. Prevention 1999;53 in Sherman KJ, Cherkin DC, Erro J, Miglioretti DL, Deyo RA. Comparing Yoga, Exercise, and a Self-Care Book for Chronic Low Back Pain, A Randomized, Controlled Trial, Annals of Internal Medicine. 2005;143:849–56. doi: 10.7326/0003-4819-143-12-200512200-00003. [DOI] [PubMed] [Google Scholar]
- 47.Tekur P, Singphow C, Nagendra HR, Raghuram N. Effect of short-term intensive yoga program on pain functional disability and spinal flexibility in chronic low back pain: A randomized control study. J Altern Complement Med. 2008;14:637–44. doi: 10.1089/acm.2007.0815. [DOI] [PubMed] [Google Scholar]
- 48.Morone NE, Greco CM, Weiner DK. Mindfulness meditation for the treatment of chronic low back pain in older adults: A randomized controlled pilot study. Pain. 2008;134:310–9. doi: 10.1016/j.pain.2007.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Morone NE, Rollman BL, Moore CG, Li Q, Weiner DK. A mind-body program for older adults with chronic low back pain: Results of a pilot study. Pain Med. 2009;10:1395–407. doi: 10.1111/j.1526-4637.2009.00746.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Morone NE, Lynch CS, Greco CM, Tindle HA, Weiner DK. “I felt like a new person” the effects of mindfulness meditation on older adults with chronic pain: Qualitative narrative analysis of diary entries. J Pain. 2008;9:41–8. doi: 10.1016/j.jpain.2008.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mehling WE, Hamel KA, Acree M, Byl N, Hecht FM. Randomized, controlled trial of breath therapy for patients with chronic low-back pain. Altern Ther Health Med. 2005;11:44–52. [PubMed] [Google Scholar]
- 52.Sherman KJ, Cherkin DC, Erro J, Miglioretti DL, Deyo RA. Comparing yoga, exercise, and a self-care book for chronic low back pain: A randomized controlled trial. Ann Intern Med. 2005;143:849–56. doi: 10.7326/0003-4819-143-12-200512200-00003. [DOI] [PubMed] [Google Scholar]
- 53.Williams KA, Petronis J, Smith D, Goodrich D, Wu J. Effect of Iyengar yoga therapy for chronic low back pain. Pain. 2005;115:107–17. doi: 10.1016/j.pain.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 54.Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. Gen Hosp Psychiatry. 1982;4:33–47. doi: 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]


