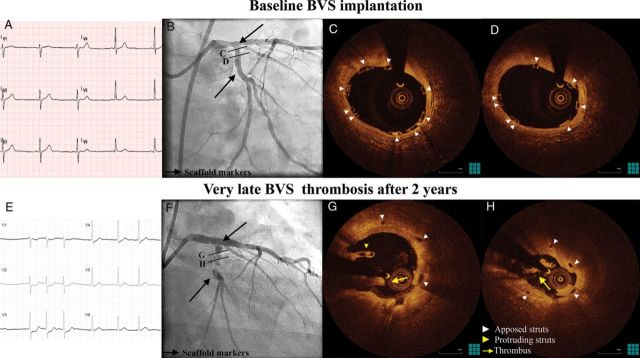
A 57-year-old gentleman was admitted with unstable angina with dynamic ECG changes (E), 4 days after discontinuation of dual antiplatelet therapy (DAT) with aspirin and clopidogrel. He had undergone staged percutaneous coronary intervention with bioresorbable vascular scaffold (BVS; ABSORB 1.1, Abbott Vascular, Santa Clara, CA, USA) implantation in the ostial left circumflex artery (LCx) 2 years ago (Panels A–D), followed by everolimus-eluting metal stent implantation in the distal left main and proximal left anterior descending artery, with balloon dilation of the LCx ostium. Fractional flow reserve of the LCx post-intervention was 0.88.
At presentation, angiography showed a filling defect in the scaffolded segment (Panel F). Optical coherence tomography revealed intracoronary thrombus and scaffold pattern irregularities (Panels G and H). The patient was treated with thrombectomy and everolimus-eluting metal stent implantation and discharged on aspirin and prasugrel.
To our knowledge, this is the first reported case of very late BVS thrombosis. Bioresorbable scaffolds have been suggested as an alternative to metal platform drug-eluting stents, aiming to reduce very late stent complications, by providing transient support and being completely integrated into the vascular wall after this period. Although, at 24 months significant bioresorption is expected to have occurred with restoration of local vasomotion, there is still evidence of scaffold struts. In our case, scaffold thrombosis was observed together with scaffold pattern irregularities. The possibility that the observed irregularities were induced by the balloon dilation performed during left main metal stent implantation, subsequently leading to thrombosis, cannot be excluded. Importantly, the event occurred 4 days after DAT discontinuation, suggesting a need for individualized duration of DAT in complex cases treated with BVS.
Funding: Funding to pay the Open Access publication charges for this article was provided by Thoraxcentre, Erasmus University, Rotterdam, NL.