Abstract
Background
Symptom monitoring is considered the first step toward self-care management (actions to manage altered symptom status) to avert worsening heart failure (HF). However, empirical evidence demonstrating that symptom monitoring leads to adequate self-care management is lacking. We examined the relationship of adherence to regular symptom monitoring with adequate self-care management in HF patients.
Methods and Results
A total of 311 HF patients (60 years, 35% female) were divided into three groups by adherence to two symptom monitoring behaviors (monitoring daily weights and lower extremity edema). Patients who were adherent to both symptom monitoring behaviors formed the adherent group (15.1%). Those adherent to either of the symptom monitoring behaviors formed the partially adherent group (28.9%). Those adherent to neither of the symptom monitoring behaviors formed the non-adherent group (56.0%). Adjusted odds of performing adequate self-care management were increased by 225% (95% CI 1.13-4.48) and 344% (95% CI 1.55-7.62) for the partially adherent and adherent symptom monitoring groups compared to the non-adherent group, respectively.
Conclusion
Adequacy of self-care management was predicted by adherence to symptom monitoring behaviors. This finding suggests that regular symptom monitoring facilitates performance of adequate self-care management, which may contribute to a decrease in preventable hospitalizations in HF.
Heart failure (HF) is a serious health concern in the United States, with high mortality and rehospitalization rates. Approximately half of the patients who are diagnosed with HF will die within five years.1 Although HF rehospitalization rates have decreased over 10 years from 1998 to 2008,2 HF remains the most common reason for rehospitalizations among Medicare beneficiaries.3 A majority of rehospitalizations due to worsening HF are preventable with active engagement in self-care.4,5 For example, Lee and colleagues found that patients who used a symptom diary to monitor their day-to-day weight and symptoms, such as dyspnea and swelling, had fewer hospitalizations and/or deaths over 3 months than patients who did not use he diary.4 Thus, if patients are aware of early symptoms and signs of HF exacerbation with regular symptom monitoring, they can undertake an appropriate action in a timely manner, which may, in turn, contribute to a decrease in HF readmissions.
Self-care is conceptualized as a naturalistic decision making process by patients to maintain physiological stability (self-care maintenance) and respond to changes in their symptom status (self-care management).6 Self-care maintenance consists of two components, monitoring symptoms and adhering to treatment regimens. Self-care management includes the following processes: recognizing altered symptom status, evaluating the changes in symptoms, deciding what actions to take, performing treatment strategies (e.g., take extra diuretics and call to clinicians), and evaluating the results of actions taken.6 It is suggested that patients who monitor symptoms are able to detect and interpret escalating symptoms in a timely manner and initiate successful self-care management.6 However, the empirical evidence demonstrating the relationship between adherence to symptom monitoring behaviors and engagement in self-care management is lacking.
The purpose of this study was to examine the relationship of adherence to regular symptom monitoring, which is defined as always checking weights and lower extremity edema, with adequate self-care management (e.g., evaluating altered symptom status and undertaking treatment strategies) among HF patients who experienced dyspnea or edema in the past month. The first specific aim was to describe self-care management behaviors among three groups of patients based on adherence to two types of symptom monitoring behaviors (i.e., monitoring weights and lower extremity edema): patients who were adherent to (1) both symptom monitoring behaviors; (2) either of the symptom monitoring behaviors; and (3) neither of the symptom monitoring behaviors. The second specific aim was to examine whether membership in one of the three symptom monitoring adherence groups predicted adequacy of self-care management after controlling for the following demographic and clinical variables: age, gender, marital status, ethnicity, the Charlson Comorbidity Index, New York Heart Association [NYHA] functional class, etiology of HF, and diuretic medication therapy.
Methods
The investigation was a cross-sectional, observational examination of the association between adherence to regular symptom monitoring and adequate self-management in patients with HF. Patients were enrolled from HF clinics from six large community hospitals and academic medical centers in Kentucky, Georgia, and Indiana. Institutional Review Board approval was obtained at all sites. All patients who agreed to participate in the study provided signed, informed consent and visited the General Clinical Research Center to complete questionnaire packets and interviews.
Patients
Prospectively patients were identified by physicians and nurse practitioners. Research nurses approached eligible patients, explained the study in detail, and obtained informed consent if the patients agreed to participate in the study. Patients who met the following criteria were eligible for the study: (1) confirmed diagnosis of HF; (2) dyspnea and/or edema over the past one month; (3) stable dosage of medications for at least three months; (4) no myocardial infarction within the three months prior to starting the study; (5) no referral for heart transplant; (6) free of noncardiac serious or life-threatening comorbid conditions (e.g., end-stage renal or liver disease); (7) free of obvious cognitive impairment that prevented providing informed consent and completing the questionnaire packets; and (8) English-speaking.
Measurements
Symptom Monitoring Behaviors
In this study, symptom monitoring behaviors were defined as monitoring weight and lower extremity edema, and assessed with two items from the self-care maintenance subscale of the Self-Care of Heart Failure Index (SCHFI).7 Patients were asked how frequently they weighed themselves and checked lower extremity swelling in the last month and could rate these items on a scale of 1 (never or rarely) to 4 (always). Patients were considered adherent to symptom monitoring if they reported monitoring always. The following three patient groups were created based on levels of adherence to the two items (weight and lower extremity edema monitoring): adherent to (1) both items (i.e., adherent group); (2) either of the items (i.e., partially adherent group); and (3) neither of the items (i.e., non-adherent group).
Self-Care Management
Self-care management was measured with the self-care management subscale of the SCHFI. The self-care management subscale is comprised of six items capturing symptom recognition (i.e., shortness of breath or edema), implementation of treatment strategies (i.e., taking an extra diuretic dose, restricting fluid and sodium intake, and seeking advice from healthcare providers), and treatment strategy evaluation. Patients could rate items related to the implementation of treatment strategies on a 4-point Likert scale and items related to symptom recognition and treatment strategy evaluation on a 5-point Likert scale. The scores were standardized to range from 0 to 100, with higher scores indicating better self-care management. A score of 70 or greater (based on prior evidence) was considered adequate self-care management.7 Its reliability and validity have been supported in previous studies.7
Sociodemographic and Clinical data
Data on age, gender, ethnicity, marital status, and medication regimens were collected via patient interview and medical records review. The interview format of the Charlson Comorbidity Index was used to obtain total comorbidity scores by taking into account the number and seriousness of comorbid conditions.8 Data on left ventricular ejection fraction (LVEF) and HF etiology were collected from the medical records. Patients were categorized as having either non-preserved systolic function (LVEF ≤ 40%) or preserved systolic function (LVEF > 40%) with a cutoff of 40%. NYHA functional classification was determined by trained research nurses via in-depth structured patient interviews.
Statistical Analyses
Data were analyzed by SAS (version 9.3). Descriptive statistics including frequency distributions, means, and standard deviations were used to describe sociodemographic and clinical characteristics. Chi-square tests or Fisher's exact tests of independence for categorical variables and one-way analysis of variance (ANOVA) for continuous variables were used to compare the differences in sociodemographic and clinical characteristics among three symptom monitoring adherence groups (i.e., adherent, partially adherent, and non-adherent groups). Bonferroni post-hoc test was performed if F-tests for ANOVA were significant (p-value < 0.05).
Univariable and multivariable logistic regression analyses were conducted to explore the association between the levels of symptom monitoring adherence and the adequacy of self-care management. An outcome variable (self-care management) was dichotomized for binary variables with the cutpoint of 70.7 Covariates included in the multivariable model were age, gender, marital status, ethnicity, the Charlson Comorbidity Index, NYHA functional class, etiology of HF, and diuretic medication therapy. The covariates were selected based on previous studies9-11 and comparison of sample characteristics among the three groups. Receiver Operating Characteristic curves were used to assess model fit.
Results
Sample Characteristics
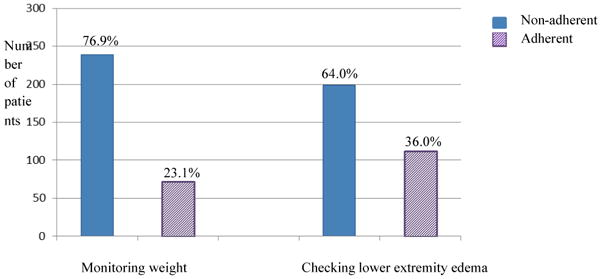
The sample (N= 311) was predominantly male, white, and married or cohabitating (Table 1). More than half of the sample were in NYHA functional class III/IV and had non-preserved systolic function with LVEF ≤ 40%. Average levels of self-care management were generally low with the mean score of below 70, which is the cutpoint for the adequacy of self-care management.7 Less than half the total sample reported that they always monitored their weights (72/311) and lower extremity edema (112/311) (Figure 1). As described previously, three adherence groups were formed based on adherence to two symptom monitoring behaviors. A total of 15.1% (47/311) of patients were in the adherent group, 28.9% (90/311) in the partially adherent group, and 56.0% (174/311) in the non-adherent group.
Table 1. Sample Characteristics (N=311).
| Total (N = 311) | Non-adherent (N = 174) | Partially adherent (N = 90) | Adherent (N = 47) | p-value | |
|---|---|---|---|---|---|
| Age, years | 60 (±11.9) | 59 (±12.5) | 61 (±10.2) | 63 (±11.9) | 0.056 |
|
| |||||
| Gender | 0.503 | ||||
| Male | 201 (64.6%) | 117 (67.2%) | 54 (60.0%) | 30 (63.8%) | |
| Female | 110 (35.4%) | 57 (32.8%) | 36 (40.0%) | 17 (36.2%) | |
|
| |||||
| Marital Status | 0.052 | ||||
| Single/divorced/widow | 126 (40.5%) | 63 (36.2%) | 46 (51.1%) | 17 (36.2%) | |
| Married/co-habitating | 185 (59.5%) | 111 (63.8%) | 44 (48.9%) | 30 (63.8%) | |
|
| |||||
| Ethnicity | 0.006 | ||||
| White | 206 (66.2%) | 105 (60.3%) | 61 (67.8%) | 40 (85.1%) | |
| Minority | 105 (33.8%) | 69 (39.7%) | 29 (32.2%) | 7 (14.9%) | |
|
| |||||
| NYHA class | 0.777 | ||||
| I/II | 112 (36.0%) | 62 (35.6%) | 31 (34.4%) | 19 (40.4%) | |
| III/IV | 199 (64.0%) | 112 (64.4%) | 59 (65.6%) | 28 (59.6%) | |
|
| |||||
| Ischemic etiology of HF | 220 (70.7%) | 113 (64.9%) | 68 (75.6%) | 39 (83.0%) | 0.027 |
|
| |||||
| LVEF | 0.155 | ||||
| ≤ 40% | 200 (64.3%) | 107 (61.5%) | 57 (63.3%) | 36 (76.6%) | |
| > 40% | 111 (35.7%) | 67 (38.5%) | 33 (36.7%) | 11 (23.4%) | |
|
| |||||
| Charlson Comorbidity Index | 3.3 (±1.9) | 3.2 (±1.8) | 3.6 (±2.0) | 3.5 (±2.1) | 0.152 |
|
| |||||
| Self-care Management† | 55.5 (±20.5) | 49.4 (±19.4) | 59.9 (±19.3) | 70.0 (±17.6) | <.001 |
|
| |||||
| Medications | |||||
| ACEI or ARB (n=310) | 254 (81.9%) | 148 (85.1%) | 71 (79.8%) | 35 (74.5%) | 0.202 |
| Beta Blocker (n=309) | 267 (86.4%) | 149 (85.6%) | 75 (85.2%) | 43 (91.5%) | 0.542 |
| Diuretics | 245 (78.8%) | 124 (71.3%) | 75 (83.3%) | 46 (97.9%) | <.001 |
Note. Values are mean (±SD) or n (%).
NYHA=New York Heart Association; HF= Heart Failure; ACEI = angiotensin converting enzyme inhibitor; ARB = angiotensin receptor blocker
Significant group difference among all three groups
Figure 1. Adherence to Symptom Monitoring Behaviors (N=311).
The demographic and clinical variables that differentiated among the three groups were ethnicity and etiology of HF. Patients in the adherent group were more likely to be white and have ischemic heart disease as the underlying etiology of HF than patients in the partially adherent and non-adherent groups. Diuretics were prescribed more often in patients in the adherent group than patients in the other two groups. Self-care management scores were significantly different among groups. The percentage of patients who performed adequate self-care management (self-care management scores of ≥ 70) were 38.3% (18/47) in the adherent, 25.6% (23/90) in the partially adherent, and 13.2% (23/174) in the non-adherent group.
Comparison of Self-care Management among Symptom Monitoring Adherence Groups
Of the total sample, 13.2% of patients failed to identify changes in symptoms (Table 2). None of the patients in the adherent group failed to recognize their symptoms, while approximately one out of five patients in the non-adherent group did not recognize symptom changes.
Table 2. Self-care Management Behaviors by Symptom Monitoring Adherence Groups (N=311).
| Total (N = 311) | Non-adherent (N = 174) | Partially adherent (N = 90) | Adherent (N = 47) | p-value | |
|---|---|---|---|---|---|
| Symptom Recognition | <.001 | ||||
|
| |||||
| Not recognized | 41 (13.2%) | 33 (19.0%) | 8 (8.9%) | 0 (0.0%) | |
| Not quickly | 30 (9.6%) | 22 (12.6%) | 5 (5.6%) | 3 (6.4%) | |
| Somewhat quickly | 44 (14.1%) | 23 (13.2%) | 15 (16.7%) | 6 (12.8%) | |
| Quickly | 85 (27.3%) | 52 (29.9%) | 25 (27.8%) | 8 (17.0%) | |
| Very quickly | 111 (35.7%) | 44 (25.3%) | 37 (41.1%) | 30 (63.8%) | |
|
| |||||
| Restrict Sodium Intake | 0.011 | ||||
|
| |||||
| Not likely | 29 (9.3%) | 21 (12.1%) | 7 (7.8%) | 1 (2.1%) | |
| Somewhat likely | 64 (20.6%) | 40 (23.0%) | 18 (20.0%) | 6 (12.8%) | |
| Likely | 79 (25.4%) | 51 (29.3%) | 16 (17.8%) | 12 (25.5%) | |
| Very likely | 139 (44.7%) | 62 (35.6%) | 49 (54.4%) | 28 (59.6%) | |
|
| |||||
| Restrict Fluid Intake | <.001 | ||||
|
| |||||
| Not likely | 95 (30.5%) | 66 (37.9%) | 24 (26.7%) | 5 (10.6%) | |
| Somewhat likely | 65 (20.9%) | 40 (23.0%) | 19 (21.1%) | 6 (12.8%) | |
| Likely | 74 (23.8%) | 40 (23.0%) | 17 (18.9%) | 17 (36.2%) | |
| Very likely | 77 (24.8%) | 28 (16.1%) | 30 (33.3%) | 19 (40.4%) | |
|
| |||||
| Take an Extra Diuretics | 0.030 | ||||
|
| |||||
| Not likely | 112 (36.0%) | 67 (38.5%) | 34 (37.8%) | 11 (23.4%) | |
| Somewhat likely | 44 (14.1%) | 30 (17.2%) | 10 (11.1%) | 4 (8.5%) | |
| Likely | 63 (20.3%) | 36 (20.7%) | 19 (21.1%) | 8 (17.0%) | |
| Very likely | 92 (29.6%) | 41 (23.6%) | 27 (30.0%) | 24 (51.1%) | |
|
| |||||
| Call HealthCare Providers for Guidance | 0.265 | ||||
|
| |||||
| Not likely | 93 (29.9%) | 53 (30.5%) | 28 (31.1%) | 12 (25.5%) | |
| Somewhat likely | 57 (18.3%) | 27 (15.5%) | 19 (21.1%) | 11 (23.4%) | |
| Likely | 67 (21.5%) | 46 (26.4%) | 13 (14.4%) | 8 (17.0%) | |
| Very likely | 94 (30.2%) | 48 (27.6%) | 30 (33.3%) | 16 (34.0%) | |
|
| |||||
| Evaluation of Treatment Strategies (helpful or not) | <.001 | ||||
|
| |||||
| Did not try anything | 62 (19.9%) | 43 (24.7%) | 12 (13.3%) | 7 (14.9%) | |
| Not sure | 48 (15.4%) | 33 (19.0%) | 12 (13.3%) | 3 (6.4%) | |
| Somewhat sure | 74 (23.8%) | 49 (28.2%) | 19 (21.1%) | 6 (12.8%) | |
| Sure | 67 (21.5%) | 27 (15.5%) | 22 (24.4%) | 18 (38.3%) | |
| Very sure | 60 (19.3%) | 22 (12.6%) | 25 (27.8%) | 13 (27.7%) | |
Note. Values are n (%).
Among four possible treatment strategies to ameliorate worsening symptoms, reduced sodium intake was the most likely to be performed while taking an extra diuretic was the least likely to be done by all patients. There were significant group differences with regard to limitation of sodium and fluid intake, and taking extra diuretics; however, there was no group difference in obtaining medical advice from healthcare providers (Table 2).
When dyspnea or lower extremity edema was experienced, about one of five patients did not do anything. Only half of the patients who took actions to relieve worsening symptoms were sure or very sure of the effectiveness of their actions. Compared to patients in the partially adherent or non-adherent groups, more patients in the adherent group responded to altered symptom status and reported that they were sure or very sure of the effectiveness of their actions.
Association between Symptom Monitoring Adherence Groups and Adequate Self-care Management
Adequacy of self-care management was significantly associated with membership in one of the three symptom monitoring adherence groups. In a univariate model, compared to patients in the non-adherent group, the odds of performing adequate self-care management were two times and four times higher in patients in the partially adherent (odds ratio [OR] 2.27; 95% confidence interval [CI] 1.19 - 4.33) and adherent groups (OR 4.10; 95% CI 1.97 – 8.54), respectively.
A full multivariable logistic regression model was presented in Table 3. The symptom monitoring adherence group and diuretic therapy were significant independent predictors of adequate self-care management. The adjusted odds of performing adequate self-care management were increased by 225% (95% CI 1.13-4.48) and 344% (95% CI 1.55-7.62) for the partially adherent and adherent groups, respectively. Patients who were prescribed diuretics were at six times higher odds of engaging in adequate self-care management than patients who were not, after adjusting for other variables in the model (OR 5.99; 95% CI 1.76 - 20.36).
Table 3. Logistic Regression (N=311).
| Odds Ratio | 95% Confidence Interval | p-value | |
|---|---|---|---|
| Age | 1.01 | 0.98 - 1.03 | 0.583 |
|
| |||
| Female (vs. Male) | 0.72 | 0.37 - 1.39 | 0.329 |
|
| |||
| Married/co-habitating (vs. Single/separated/widowed) | 1.34 | 0.72 - 2.51 | 0.354 |
|
| |||
| White (vs. Minority) | 1.36 | 0.70 - 2.65 | 0.362 |
|
| |||
| Charlson Comorbidity Index | 0.92 | 0.79 - 1.07 | 0.286 |
|
| |||
| NYHA Class III/IV (vs. I/II) | 1.83 | 0.93 – 3.61 | 0.080 |
|
| |||
| Non-ischemic Etiology of Heart Failure (vs. Ischemic) | 0.73 | 0.36 - 1.51 | 0.397 |
|
| |||
| Diuretic Prescription | 5.99 | 1.76 – 20.36 | 0.004 |
|
| |||
| Symptom Monitoring Adherence Groups (vs. non-adherent group) | 0.005 | ||
| Partially Adherent Group | 2.25 | 1.13 - 4.48 | 0.020 |
| Adherent Group | 3.44 | 1.55 - 7.62 | 0.002 |
Note. NYHA=New York Heart Association
Model p-value <0.001
Discussion
Results of this study contribute to the body of literature suggesting the importance of regular symptom monitoring to adequate self-care management. Adequacy of self-care management was predicted by adherence to symptom monitoring behaviors measured by always monitoring weight and lower extremity edema. Patients who engaged in both symptom monitoring behaviors were more likely to identify altered symptom status, implement treatment strategies to relieve worsening HF status, and evaluate the effectiveness of their responses.
Monitoring signs and symptoms for congestion is important because one of the most common reasons for hospitalizations in patients with HF is volume overload.12 Because weight gain alone does not always reflect HF deterioration,13 it is important to simultaneously monitor a range of signs and symptoms of volume overload, including weight gain and lower extremity edema.4 However, of 311 patients in this study only 15% reported that they performed daily weight and lower extremity edema monitoring. More than half of the patients did not monitor their symptoms on a daily basis even though they experienced dyspnea or lower extremity edema during the past month.
Poor adherence to symptom monitoring has been demonstrated in previous studies. More than half of patients with HF do not weigh themselves daily.14-20 Only 9% of patients who were recently discharged from the hospital due to decompensated HF reported monitoring for symptoms of worsening HF.17
Reasons for not monitoring signs and symptoms of congestion may be related to a lack of knowledge and motivation. Less than 40% of patients with HF were unaware that swelling of the legs and ankles, waking up at night due to shortness of breath, and weight gain were signs and symptoms of worsening HF.21 Patients simply do not know that they should monitor their weight or are not informed of the importance of daily weight monitoring by their healthcare providers.14,16 Patients decide not to weigh themselves because they do not know how to use the information, even if they are aware of the importance of this behavior.16,22 Gallagher suggests that poor adherence to symptom monitoring is related to patients' misconception about HF, which is perceived as an acute illness. 23 As patients believe HF is present when symptoms are present, they may not value daily symptom monitoring when they do not experience symptoms limiting their daily activities.
The notion that adhering to symptom monitoring facilitates self-care management behaviors to relieve altered symptom status is supported by this study. Patients in the adherent symptom monitoring group were more likely to recognize changes in symptoms (dyspnea or lower extremity edema) in a timely manner, respond to those changes, and evaluate the effectiveness of the responses as compared to patients in non-adherent group in our study. It has been demonstrated that regular symptom monitoring using weight and/or symptom diaries is beneficial in reducing recurrent hospitalizations and deaths in randomized controlled trials. 4,24 Thus, regular monitoring of symptoms is an important step for patients with HF to recognize worsening HF and take appropriately actions in a timely manner to reduce frequent hospitalizations.
Dickson and colleagues introduced and defined three types of patients based on their self-care capacities: patients who are novice, inconsistent, and expert in self-care.25 A self-care expert is characterized as one who routinely performs “body listening,” makes a link between altered symptom status and its causes, chooses rational decisions about the changes, depends on lessons learned from previous experiences of symptom management, and reassesses the effectiveness of the actions taken.26
According to this self-care typology, patients in the adherent group in this study can be categorized as self-care experts because they performed adequate self-care management when symptoms of worsening HF occurred. Patients who vigilantly monitor their symptoms may have sufficient knowledge of HF mechanisms and causes of HF symptoms, and a good understanding of what to do to prevent HF exacerbation; however, it is beyond the purpose of this study to show whether patients in the adherent group had a better understanding of HF as compared to patients in the partially adherent and non-adherent groups in this study.
One interesting finding in this study is the association between prescribed diuretics and self-care management. Diuretic prescription was an independent predictor of adequate self-care management, although the 95% CI for diuretic prescription in the logistic regression was wide. Diuretics are considered the first-line treatment for patients with HF to achieve symptom control by preventing fluid overload. Flexible diuretic titration by capable patients is recommended in HF guideline and consensus statements.27,28 Patients in the adherent group were prescribed diuretics more and were more likely to take extra diuretics if changes in symptoms occurred than patients in the partially adherent and non-adherent groups in this study. Patients who were prescribed diuretics might have learned about flexible diuretic regimens from their healthcare providers and adjusted their diuretic dosage based on their symptoms, although this is speculation as we did not collect information on flexible diuretic titration by patients.
Limitations of this study include limited generalizability. The sample in this study, which was predominantly male and white, makes it difficult to draw inferences from this study sample to all HF patients. Symptom monitoring behaviors and self-care management were assessed based on self-reporting, which may be subject to recall or social desirability bias. Of many signs and symptoms reflecting HF status, weight and lower extremity edema were selected because monitoring daily weight and edema is recommended activity by the Heart Failure Society of America.29 Because weight gain and lower extremity edema are commonly experienced by patients with HF12,30 and have objective measures (e.g., weight and indentation on skin after pressure), patients may be able to more easily compare and detect daily changes in weight and edema than daily changes in other symptoms, such as dyspnea, which is significantly influenced by daily activities
Conclusion
Adherence to regular symptom monitoring was associated with adequate self-care management. This result supports the conclusion that engaging in symptom monitoring is the first step in recognition of altered body states that prompts patients to proceed to appropriate self-care management in order to mitigate worsening symptoms. This, in turn, may decrease preventable hospitalizations due to failure to seek care in a timely manner. Thus, healthcare providers shouuld stress the importance of regularly monitoring signs and symptoms of HF exacerbation to patients.
What is new?
More than half of the patients with heart failure (HF) did not monitor their symptoms on a daily basis even though they experienced dyspnea or lower extremity edema during the past month
Patients who were adherent to both monitoring weight and lower extremity edema were 3.4 times more likely to perform adequate self-care management.
It is important that healthcare providers stress the importance of monitoring a group of relevant signs and symptoms of HF exacerbation to patients
Acknowledgments
NIH # R01 NR008567 from the National Institute of Nursing Research and a Center grant from NIH National Institute of Nursing Research # 1P20NR010679. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Contributor Information
Kyoung Suk Lee, University of Wisconsin-Madison, College of Nursing, Madison, Wisconsin.
Terry A. Lennie, University of Kentucky, College of Nursing, Lexington, Kentucky.
Sandra B. Dunbar, School of Nursing, Emory University, Atlanta, Gorgia.
Susan J. Pressler, School of Nursing, University of Michigan, Ann Arbor, Michigan.
Seongkum Heo, University of Arkansas for Medical Sciences, College of Nursing, Little Rock, Arkansas.
Eun Kyeung Song, Department of Nursing, College of Medicine, University of Ulsan, Ulsan, South Korea.
Martha Biddle, University of Kentucky, College of Nursing, Lexington, Kentucky.
Debra K. Moser, Professor and Gill Endowed Chair of Nursing, University of Kentucky, College of Nursing, Lexington, Kentucky.
References
- 1.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics--2013 update: a report from the american heart association. Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998-2008. Jama. 2011;306:1669–78. doi: 10.1001/jama.2011.1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 4.Lee KS, Lennie TA, Warden S, Jacobs-Lawson JM, Moser DK. A Comprehensive Symptom Diary Intervention to Improve Outcomes in Patients With HF: A Pilot Study. J Card Fail. 2013;19:647–54. doi: 10.1016/j.cardfail.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 5.Annema C, Luttik ML, Jaarsma T. Reasons for readmission in heart failure: Perspectives of patients, caregivers, cardiologists, and heart failure nurses. Heart Lung. 2009;38:427–34. doi: 10.1016/j.hrtlng.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 6.Riegel B, Dickson VV. A situation-specific theory of heart failure self-care. J Cardiovasc Nurs. 2008;23:190–6. doi: 10.1097/01.JCN.0000305091.35259.85. [DOI] [PubMed] [Google Scholar]
- 7.Riegel B, Lee CS, Dickson VV, Carlson B. An update on the self-care of heart failure index. J Cardiovasc Nurs. 2009;24:485–97. doi: 10.1097/JCN.0b013e3181b4baa0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 9.Cameron J, Worrall-Carter L, Riegel B, Lo SK, Stewart S. Testing a model of patient characteristics, psychologic status, and cognitive function as predictors of self-care in persons with chronic heart failure. Heart Lung. 2009;38:410–8. doi: 10.1016/j.hrtlng.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 10.Dickson VV, Buck H, Riegel B. Multiple comorbid conditions challenge heart failure self-care by decreasing self-efficacy. Nurs Res. 2013;62:2–9. doi: 10.1097/NNR.0b013e31827337b3. [DOI] [PubMed] [Google Scholar]
- 11.Lee CS, Riegel B, Driscoll A, et al. Gender differences in heart failure self-care: a multinational cross-sectional study. Int J Nurs Stud. 2009;46:1485–95. doi: 10.1016/j.ijnurstu.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Albert N, Trochelman K, Li J, Lin S. Signs and symptoms of heart failure: are you asking the right questions? Am J Crit Care. 2010;19:443–52. doi: 10.4037/ajcc2009314. [DOI] [PubMed] [Google Scholar]
- 13.Lewin J, Ledwidge M, O'Loughlin C, McNally C, McDonald K. Clinical deterioration in established heart failure: what is the value of BNP and weight gain in aiding diagnosis? Eur J Heart Fail. 2005;7:953–7. doi: 10.1016/j.ejheart.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 14.van der Wal MH, Jaarsma T, Moser DK, Veeger NJ, van Gilst WH, van Veldhuisen DJ. Compliance in heart failure patients: the importance of knowledge and beliefs. Eur Heart J. 2006;27:434–40. doi: 10.1093/eurheartj/ehi603. [DOI] [PubMed] [Google Scholar]
- 15.Lupon J, Gonzalez B, Mas D, et al. Patients' self-care improvement with nurse education intervention in Spain assessed by the European Heart Failure Self-Care Behaviour Scale. Eur J Cardiovasc Nurs. 2008;7:16–20. doi: 10.1016/j.ejcnurse.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 16.Ni H, Nauman D, Burgess D, Wise K, Crispell K, Hershberger RE. Factors influencing knowledge of and adherence to self-care among patients with heart failure. Arch Intern Med. 1999;159:1613–9. doi: 10.1001/archinte.159.14.1613. [DOI] [PubMed] [Google Scholar]
- 17.Moser DK, Doering LV, Chung ML. Vulnerabilities of patients recovering from an exacerbation of chronic heart failure. Am Heart J. 2005;150:984. doi: 10.1016/j.ahj.2005.07.028. [DOI] [PubMed] [Google Scholar]
- 18.Holst M, Willenheimer R, Martensson J, Lindholm M, Stromberg A. Telephone follow-up of self-care behaviour after a single session education of patients with heart failure in primary health care. Eur J Cardiovasc Nurs. 2007;6:153–9. doi: 10.1016/j.ejcnurse.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 19.Artinian NT, Magnan M, Sloan M, Lange MP. Self-care behaviors among patients with heart failure. Heart Lung. 2002;31:161–72. doi: 10.1067/mhl.2002.123672. [DOI] [PubMed] [Google Scholar]
- 20.Gary R. Self-care practices in women with diastolic heart failure. Heart Lung. 2006;35:9–19. doi: 10.1016/j.hrtlng.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 21.Baker DW, Asch SM, Keesey JW, et al. Differences in education, knowledge, self-management activities, and health outcomes for patients with heart failure cared for under the chronic disease model: the improving chronic illness care evaluation. J Card Fail. 2005;11:405–13. doi: 10.1016/j.cardfail.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 22.Jaarsma T, Abu-Saad HH, Dracup K, Halfens R. Self-care behaviour of patients with heart failure. Scand J Caring Sci. 2000;14:112–9. [PubMed] [Google Scholar]
- 23.Gallagher R. Self management, symptom monitoring and associated factors in people with heart failure living in the community. Eur J Cardiovasc Nurs. 2010;9:153–60. doi: 10.1016/j.ejcnurse.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 24.Wright SP, Walsh H, Ingley KM, et al. Uptake of self-management strategies in a heart failure management programme. Eur J Heart Fail. 2003;5:371–80. doi: 10.1016/s1388-9842(03)00039-4. [DOI] [PubMed] [Google Scholar]
- 25.Dickson VV, Deatrick JA, Riegel B. A typology of heart failure self-care management in non-elders. Eur J Cardiovasc Nurs. 2008;7:171–81. doi: 10.1016/j.ejcnurse.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 26.Riegel B, Lee CS, Dickson VV. Self care in patients with chronic heart failure. Nat Rev Cardiol. 2011;8:644–54. doi: 10.1038/nrcardio.2011.95. [DOI] [PubMed] [Google Scholar]
- 27.Dickstein K, Cohen-Solal A, Filippatos G, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM) Eur Heart J. 2008;29:2388–442. doi: 10.1093/eurheartj/ehn309. [DOI] [PubMed] [Google Scholar]
- 28.Lindenfeld J, Albert NM, Boehmer JP, et al. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010;16:e1–194. doi: 10.1016/j.cardfail.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 29.Self-Care: Following Your Treatment Plan and Dealing with Your Symptoms. St. Paul, MN: Heart Failure Society of America; 2006. [Google Scholar]
- 30.Friedman MM, Quinn JR. Heart failure patients' time, symptoms, and actions before a hospital admission. J Cardiovasc Nurs. 2008;23:506–12. doi: 10.1097/01.JCN.0000338928.51093.40. [DOI] [PubMed] [Google Scholar]


