Abstract
This review provides an update on asthma in Hispanics, a diverse group tracing their ancestry to countries previously under Spanish rule. A marked variability in the prevalence and morbidity from asthma remains among Hispanic subgroups in the United States and Hispanic America. In the United States, Puerto Ricans and Mexican Americans have high and low burdens of asthma, respectively (the “Hispanic Paradox”). This wide divergence in asthma morbidity among Hispanic subgroups is multifactorial, likely reflecting the effects of known (secondhand tobacco smoke, air pollution, psychosocial stress, obesity, inadequate treatment) and potential (genetic variants, urbanization, vitamin D insufficiency, and eradication of parasitic infections) risk factors. Barriers to adequate asthma management in Hispanics include economic and educational disadvantages, lack of health insurance, and no access to or poor adherence with controller medications such as inhaled corticosteroids. Although considerable progress has been made in our understanding of asthma in Hispanic subgroups, many questions remain. Studies of asthma in Hispanic America should focus on environmental or lifestyle factors that are more relevant to asthma in this region (e.g., urbanization, air pollution, parasitism, and stress). In the United States, research studies should focus on risk factors that are known to or may diverge among Hispanic subgroups, including but not limited to epigenetic variation, prematurity, vitamin D level, diet, and stress. Clinical trials of culturally appropriate interventions that address multiple aspects of asthma management in Hispanic subgroups should be prioritized for funding. Ensuring high-quality healthcare for all remains a pillar of eliminating asthma disparities.
Keywords: asthma, Hispanics, genetics, risk factors
Eight years ago, we reviewed potential explanations for the marked variability in asthma morbidity among Hispanic subgroups, both in the United States and Latin America (1). Given limited knowledge, we advocated for research in well-defined Hispanic subgroups, while also emphasizing the need to broaden access to healthcare for Hispanics (1).
The purpose of this review is to provide an update on asthma in Hispanics. First, we show current demographics and indicators of asthma morbidity in Hispanics. Second, we assess recent findings on selected (known or potential) risk factors for asthma in Hispanics. Third, we review new studies on the diagnosis and management of asthma in Hispanics. Finally, we discuss future directions in this field.
The Hispanic Population
The term “Hispanic,” as defined by the U.S. 2010 Census, refers to any peoples with roots in Spain or areas previously under Spanish rule, including Mexico, large parts of Central and South America, and some Caribbean Islands (2).
Hispanic America is geographically, racially, and economically diverse (Table 1) (3). Over the last decade, Hispanic America saw reductions in health and education inequalities yet continued to demonstrate substantial income inequalities (4). Most Hispanic American countries have achieved reductions in infant mortality rates in parallel with increments in their gross domestic product and human development index (3–5).
Table 1:
Demographic and Healthcare Data for Selected Hispanic American Countries
| Country | Per Capita GDP* (∆ from 2005) | HDI† | IMR‡ (∆ from 2005) | Life Expectancy§ | Health Spending|| (∆ from 2005) | Asthma Mortality¶ | Urban Population** (%) |
|---|---|---|---|---|---|---|---|
| Argentina | $17,900 (18.8%) | 0.811 | 10.2 (−5.0) | 77.32 | $892 (126%) | 14.7 | 92 |
| Chile | $18,200 (39.9%) | 0.819 | 7.2 (−1.6) | 78.27 | $1,075 (118%) | 23.5 | 89 |
| Colombia | $10,700 (33.4%) | 0.719 | 15.5 (−5.5) | 75.02 | $432 (111%) | 19.6 | 75 |
| Costa Rica | $12,500 (7.1%) | 0.773 | 9.0 (−1.0) | 78.06 | $943 (159%) | 18.0 | 64 |
| Guatemala | $5,200 (1.9%) | 0.581 | 24.3 (−11.6) | 71.46 | $214 (55%) | 33.0 | 49 |
| Mexico | $15,400 (32.0%) | 0.775 | 16.3 (−4.7) | 76.86 | $620 (30%) | 27.1 | 78 |
| Nicaragua | $4,400 (57.4%) | 0.599 | 21.1 (−8.0) | 72.45 | $125 (76%) | 41.8 | 57 |
| Peru | $10,600 (55.7%) | 0.741 | 20.9 (−11.0) | 72.98 | $289 (125%) | 25.8 | 77 |
| Commonwealth of Puerto Rico (possession of the United States) | $16,300 (−20.2%) | — | 8.0 (−0.2) | 79.07 | — | 33.0 | 99 |
Definition of abbreviations: GDP = gross domestic product; HDI = Human Development Index; IMR = infant mortality rate.
The GDP is total market value of all final goods and services produced in a country in a given year, equal to the total consumer investment, and government spending, plus the value of exports, minus the value of imports in 2012 U.S. dollars. Change corrected for inflation based on 2004 U.S. dollars. Source: CIA World Factbook, January 2014 (3).
The HDI is calculated using various indicators for quality of life, while also accounting for GDP per capita in terms of Purchasing Power Parity and percentage of the population below the poverty line. Source: Human Development Report 2012 rankings, August 2013. Human development = very high (0.805–0.955); high (0.712–0.796); medium (0.536–0.710); low (0.304–0.534) (4).
The IMR is the number of children dying under a year of age divided by 1,000 live births. Source: CIA World Factbook, August 2013 (3).
Average number of years to be lived by a group of people born in the same year, if mortality at each age remains constant in the future. Source: CIA World Factbook, August 2013 (3).
Health care spending per capita in current U.S. dollars. Source: The World Bank, World Development Indicators, August 2013 (5).
Per 10,000 deaths based on International Classification of Diseases 10th revision codes. Most recent available data used: 2009 Argentina, Chile, Costa Rica, Nicaragua; 2008 Colombia, Guatemala; 2007 Peru, Puerto Rico. Source: Pan American Health Organization Regional Health Observatory, September 2013 (167).
Percentage of the population living in an urban environment. Information from 2010. Source: CIA World Factbook, August 2013 (3).
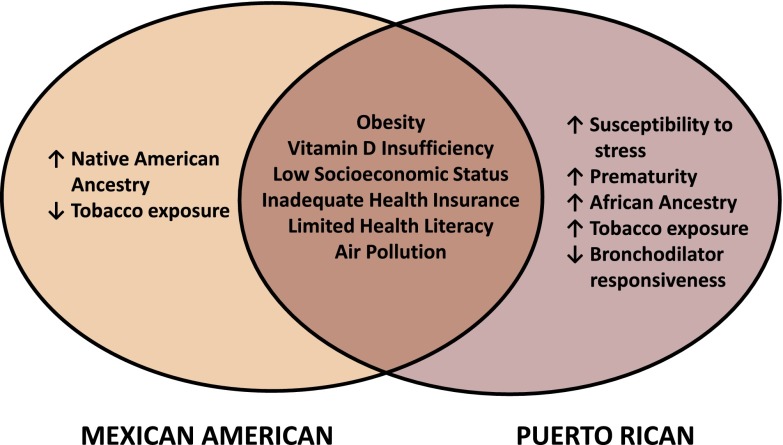
In 2010, there were 50.5 million Hispanics composing 16% of the U.S. population (2). Hispanics remain the largest growing minority in the United States (2). Persons of Mexican origin are the largest subgroup within the Hispanic population and increased by 54% since 2000 (Figure 1). The Hispanic population is diversely distributed, with persons of Mexican origin living mostly on the West Coast and the South; those of South American origin being more likely to reside in the South and the Northeast; and those of Puerto Rican, Dominican, and Cuban origin being more likely to reside in the Northeast (2).
Figure 1.
Hispanic population by origin in the U.S. Census, 2000 and 2010.
Compared with non-Hispanic (NH) whites, Hispanics are more likely to be poor (25.4% vs. 13%) (6). Compared with other ethnic groups, Hispanics are least likely to have advanced degrees (6). Hispanics are less likely to have health insurance than NH whites or Blacks: ∼29% of Hispanics are uninsured (6), with Mexican Americans least likely to be insured (7).
Prevalence, Morbidity, and Mortality of Asthma in Hispanics
Hispanic America
Phase III of the International Study of Asthma and Allergies in Childhood (ISAAC) in Hispanic America showed continued marked variability in the prevalence of ever-asthma in school-aged children (Table 2) (8). An altitude over 2,000 m was correlated with lower asthma prevalence, a finding that could be explained by natural selection, environmental factors, or changes in trunk-to-limb ratio (8).
Table 2:
International Study of Asthma and Allergies in Childhood Phase Three: Estimated Prevalence of Asthma or Asthma Symptoms in 13- to 14-Year-Old Children in Selected Hispanic American Countries
| Country | N | Current Wheeze (%) | Asthma Ever (%) |
|---|---|---|---|
| Argentina | 12,716 | 12.5 | 9.3 |
| Bolivia | 3,257 | 13.5 | 12.3 |
| Chile | 13,793 | 15.3 | 15.1 |
| Costa Rica | 2,436 | 27.3 | 23.2 |
| Cuba | 3,026 | 17.8 | 30.9 |
| Ecuador | 6,096 | 16.6 | 10.9 |
| El Salvador | 3,260 | 30.8 | 24.0 |
| Honduras | 2,675 | 22.0 | 18.3 |
| Mexico | 29,723 | 8.7 | 6.9 |
| Nicaragua | 3,263 | 13.8 | 15.2 |
| Peru | 3,022 | 19.6 | 33.1 |
Data from Reference 8.
A study of 5,978 subjects aged 1 to 59 years in Colombia yielded nationwide estimates of the prevalence of ever-asthma and current asthma symptoms of ∼23 and ∼12%, respectively (9, 10). In one of few studies including rural areas of Hispanic America, a comparison of the prevalence of asthma in 6,821 Afro-Ecuadorian children living in urban and rural areas showed a strikingly similar prevalence of symptoms (10.1% vs. 9.4%, respectively) (11).
Even though assessing asthma mortality remains challenging for some Hispanic American countries, Table 1 lists such rates for selected countries. One study found that asthma mortality rates in Argentina decreased from the 1980s to the 1990s and speculated that this may be due to increased use of inhaled corticosteroids (ICS) (12).
United States
In the United States, the prevalence of asthma remains more variable among Hispanic subgroups than across broadly defined racial/ethnic groups (Table 3). Among children and adults in the National Health Interview Survey (2001–2010), the prevalence of current asthma was highest in Puerto Ricans (16.1%) and lowest in Mexican Americans (5.4%), with intermediate values for NH whites (7.7%) and NH Blacks (11.2%) (18). Other studies have estimated that the prevalence of asthma (13–17, 19) or asthma morbidity (17) is highest in Puerto Ricans and lowest in Mexican Americans or Central Americans, with intermediate estimates in South Americans, Cubans, and Dominicans (13, 16).
Table 3:
Estimates of the Prevalence (as Percentages) of Asthma or Asthma Outcomes in Hispanic and Hispanic Populations in the United States
| Study | Age Range of Participants | Outcome | Non-Hispanic White | Non-Hispanic Black | Hispanic (All) | Puerto Rican | Mexican | Dominican | Cuban | Other Hispanic | South American | Central American |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Leong et al. (13) | NHIS (2006–2008) all ages | Lifetime asthma | 12.2 | 13.7 | 9.9 | 21.8 | 8 | |||||
| Current asthma | 7.8 | 9.5 | 6.3 | 14.2 | 4.9 | |||||||
| Asthma attacks | 4.2 | 4.9 | 3.6 | 8.4 | 2.8 | |||||||
| CHIS (2007) all ages | Lifetime asthma | 14.8 | 20.1 | 11.2 | 23.5 | 10.3 | 18.0* | 16.6 | 9.2 | |||
| Lara et al. (16) | Ages 2–17 yr, n = 46,511 | Lifetime asthma | 12.7 | 15.8 | 12.4 | 25.8 | 10.1 | 14.9 | 14.9 | 11.6 | ||
| Asthma attacks | 5.8 | 7.5 | 5.13 | 11.8 | 4.0 | 5.3 | 5.9 | 4.7 | ||||
| Dumanovsky and Matte (17) | Ages ≥ 18 yr, n = 19,400 | Asthma attacks | 3.3 | 5.9 | 6.6 | 11.8 | 5.4† | 10.4† | ||||
| 3.8‡ | 2.2‡ | |||||||||||
| Akinbami et al. (18) | All ages | Current asthma | 7.7 | 11.2 | ∼6.5 | 16.1 | 5.4 | |||||
| Rose et al. (19) | Ages ≥ 18 yr | Lifetime asthma | 9.2 | 9.6 | 17.0 | 7.5 | 7.3 | |||||
| Current asthma | 3.5 | 3.6 | 9.2 | 3.0 | 2.4 | |||||||
| Eldeirawi et al. (21) | Ages 2 mo–16 yr | Lifetime asthma | 8.5† | |||||||||
| 2.8‡ | ||||||||||||
| Wheezing (last 12 mo) | 21.4† | |||||||||||
| 12.6‡ | ||||||||||||
| Cohen et al. (23) | Ages 5–13 yr | Lifetime asthma | 35.3§ | |||||||||
| 41.3|| | ||||||||||||
| Hospitalized for asthma, ever | 36.5§ | |||||||||||
| 48.7|| |
Definition of abbreviations: CHIS = California Health Interview Survey; NHIS = National Health Interview Survey.
Two or more Hispanic subgroups.
Born in the United States.
Born in home country.
Puerto Ricans living in the Bronx, NY.
Puerto Ricans living in Puerto Rico.
Mexican Americans have a relatively low prevalence of asthma, but those born in the United States have a higher risk of asthma than those born in Mexico (14, 20, 21). A higher degree of acculturation may also increase the risk of asthma in Mexican Americans (22). In contrast to these findings, Puerto Rican children living in Puerto Rico have higher odds of ever-asthma or hospitalizations for asthma (by ∼27–30%) than those living in the U.S. Northeast (23).
Puerto Ricans continue to share a disproportionate burden of asthma attacks in the United States (24). Among children with asthma in Rhode Island, Dominicans and Puerto Ricans were shown to have lower disease control but higher use of the emergency department (ED) for asthma than NH whites (25, 26). Puerto Ricans and Mexican Americans were previously reported to have the highest and lowest mortality rates from asthma, respectively, of any ethnic group in the U.S. mainland (27). Although overall asthma mortality rates have decreased in the United States (28), ethnic minorities (including Hispanics) continued to have higher asthma mortality rates than whites in 2009 (29).
Potential Risk Factors for Asthma in Hispanics
Racial Ancestry and Genetics
Hispanic is an ethnicity and not a race: Hispanics can be of any race. Most Hispanics have variable proportions of European, Native American, and African ancestry (1). For example, Mexicans, Mexican Americans, and Costa Ricans living in the Central Valley of Costa Rica have, on average, a higher proportion of Native American ancestry (ranging from 35–64%) but a lower proportion of African ancestry (ranging from 3–5%) than Puerto Ricans (in whom Native American ancestry ranges between 12 and 15% and African ancestry ranges between 18 and 25%) (30–32).
Recent results suggest that racial ancestry influences lung function in Hispanic subgroups (30, 31), with more inconsistent findings for asthma per se (33, 34). Variation in trunk-to-limb ratio is unlikely to fully account for ancestral effects on lung function (35).
Consistent with findings in African American adults without asthma (36), African ancestry was linearly and inversely associated with FEV1 or FVC (but not with FEV1/FVC) in Puerto Rican children (with or without asthma) (31). On the other hand, Native American ancestry has been positively associated with FEV1 and FVC (but inversely associated with chronic obstructive pulmonary disease) in adults in New Mexico (37) and Costa Rica (30). Taken together, these results may partly explain the “Hispanic Paradox”—the wide divergence in the burden from airway diseases (asthma or chronic obstructive pulmonary disease) between subjects of Mexican descent (predominantly of European and Native American ancestry) and Puerto Ricans (predominantly of European and African ancestry). Whether genetic or environmental factors underlie ancestral effects on lung function is largely unknown.
Findings from genome-wide association studies (GWAS) and other studies suggest that a significant proportion of asthma-susceptibility variants are relevant to all ethnic groups, whereas others may be more relevant to particular ethnic groups (38–42). To date, no ethnic-specific asthma-susceptibility gene or variant has been confidently identified in Hispanic subgroups. A few asthma-susceptibility loci that were initially identified in subjects of European descent have been replicated at the single-nucleotide polymorphism (SNP) level in subjects of Puerto Rican and Mexican descent (e.g., the 17q21 locus [43, 44] and IL33 [39]). Conversely, an asthma-susceptibility locus initially identified in Costa Ricans (TLSP) (40, 41) has been replicated in subjects of European and African descent (38, 45) as well as in a sample of combined Hispanic subgroups (38).
Insufficient statistical power and false-positive results may explain lack of replication of some GWAS findings or discovery of ethnic-specific loci for asthma in Hispanics. However, common variants identified by GWAS explain only part of the heritability of complex diseases such as asthma (46), with likely modest additional gains from studying rare variants (47). Thus, studies of gene-by-gene and gene-by-environment interactions, as well as epigenetics, are needed in Hispanic subgroups.
A few studies have focused on interactions between genetic variants and environmental or lifestyle (EL) factors (including sex [41, 48], SHS [49], allergens [50, 51], and air pollution [44]) on asthma in Hispanics. Using a candidate-gene approach, interactions between SNPs in IL10 or TGFB1 and dust mite allergen on asthma exacerbations or airway responsiveness were reported in Costa Ricans, with replication in NH whites (50, 51). Limited statistical power or insufficient replication has precluded confident identification of gene-by-environment interactions on asthma in Hispanic subgroups, in whom epigenetics has also been insufficiently studied.
Socioeconomic Status and Urbanization
Hispanic America faces unique challenges, as a high proportion of its population is now urban in the context of high rates of poverty, a polluted environment, and limited access to sanitation (4, 52). Consistent with worldwide literature (53), low socioeconomic status (SES) in/near urban areas, high levels of inequality, and urbanization are associated with childhood asthma in Hispanic America (54–57).
In the United States, Puerto Ricans and Mexican Americans are disproportionately represented among the poor but have widely divergent burdens from asthma (58, 59). SES was shown to be inversely associated with asthma in Mexican American children and young adults in San Francisco, California (60). In another report, Puerto Rican ethnicity was associated with asthma in children in the U.S. mainland, even after adjustment for multiple indicators of SES (61). Together with previous results (1), these findings suggest that low SES is differentially correlated with unidentified factors affecting asthma risk in Puerto Ricans and Mexican Americans.
Stress
A growing body of literature strongly supports an association between stress and asthma (62–64) or asthma morbidity (62, 65–70).
Hispanics in the United States are disproportionately exposed to stressors such as poverty (6), unequal access to social benefits (71), discrimination (72), and physical or sexual abuse (73). Caregiver’s stress or mental illness has been associated with asthma or asthma morbidity in Mexican American (74) and inner-city (∼41% Puerto Rican and ∼33% Mexican American) children in Chicago (75), minority children (∼74% Hispanic) in New York (76), and Puerto Rican children in Puerto Rico or the Bronx (77, 78). Among school-aged children in Puerto Rico, physical or sexual abuse was associated with approximately twofold increased odds of asthma or asthma morbidity (70). The mechanisms underlying this association are unclear but may include dysfunction of the hypothalamic-pituitary-adrenal axis, cortisol insensitivity via down-regulation of receptors (79), abnormal production of inflammatory cytokines (80, 81), and increased susceptibility to environmental exposures (63, 82–84).
Signaling of the pituitary adenylate cyclase-activating polypeptide regulates physiologic stress responses and, together with corticotrophin-releasing hormone, modulates anxiety-related behavior (85). The gene for the PAC1 receptor (ADCYAP1R1) has been implicated in post-traumatic stress disorder (85) and childhood anxiety (86). Exposure to violence was associated with increased DNA methylation of ADCYAP1R1 in Puerto Rican children, in whom such methylation changes were also associated with asthma (87). Moreover, an SNP in the promoter of ADCYAP1R1 (rs2267735) was associated with asthma. Although these findings must be cautiously interpreted pending replication, they suggest that SNPs or DNA methylation in genes involved in stress regulation impacts asthma in Puerto Ricans.
Tobacco Smoke and Air Pollution
Consistent with findings in NHs (88–91), those in Hispanics support a causal association between smoking (including environmental tobacco smoke) or air pollution and asthma morbidity.
Hispanic America.
The prevalence of current smoking varies among Hispanic countries and the United States (see Table E1 in the online supplement). A study in Argentina showed that ∼33% of the population (and ∼13% of adolescents) currently smokes and that ∼60% of the population is exposed to secondhand smoke (SHS) at home (92). In that study, current smoking was associated with current asthma (odds ratio [OR] = 1.8; 95% CI, 1.4–2.4). A study of Mexican adolescents found an equally high prevalence of current smoking in subjects with and without asthma (∼34%) (93).
Residential proximity to a major road (a proxy for traffic-related pollution) has been associated with asthma (94), asthma symptoms, and atopy (95) among children in Lima, where particulate matter (PM) levels are higher than in rural areas of Peru (55). Exposure to aggregate or individual components of traffic exhaust (NO2, ozone, and PM) is common and associated with wheezing (96) and reduced lung function (97) in children in Mexico City, where a sound emissions control policy could prevent as many as 2.99 million asthma attacks (98). In contrast to the prominent role of traffic-related pollution in Mexico City, exposure to volatile organic compounds had a relatively greater estimated effect on asthma morbidity in a study of urban Argentinean children (99).
United States.
Hispanic children are more than 2.5 times more likely to live near heavy traffic than white children in California (100). In a study of a combined sample of Hispanic (n = 3,343) and African American (n = 977) children in five cities in the U.S. mainland and in Puerto Rico, exposure to NO2 (estimated from residential history and prior air monitoring data) in the first year of life was associated with asthma (OR = 1.17; 95% CI, 1.04–1.31) (101). In Puerto Rico, exposure to PM less than 2.5 μm in diameter (PM2.5) or SO2 during the first 3 years of life was also associated with asthma. In another study, yearly mean PM2.5 exposure was not significantly associated with asthma or asthma attacks among Hispanic adults (not differentiated into subgroups) (102).
Few studies have examined interactions between genetic variants or environmental exposures and air pollution on asthma. In a study of 3,023 children (including ∼30% Hispanics, without differentiation among subgroups), homozygosity for the TGFB1-509T allele was associated with asthma in subjects exposed to traffic-related emissions or maternal smoking in early life (103). In another study including 349 Dominican and African American children without asthma, prenatal or early postnatal exposure to cockroach allergen was associated with atopy, particularly among children exposed to polyaromatic hydrocarbons. In a subgroup analysis, this association was stronger in children who were null for a mutation in the gene for glutathione-S-transferase (GSTM1) (104). In another study of urban children (∼50% Hispanic), traffic-related pollution was associated with asthma only in those exposed to violence (63).
Although tobacco use is lower in Mexican Americans than in African Americans or whites, SHS is associated with asthma and nocturnal awakenings from asthma in Mexican American children (105, 106). In a study including African American, Mexican, and Puerto Rican children, in utero SHS was associated with persistent asthma (107) and poor asthma control (108).
Vitamin D
Findings in Hispanic and NH populations have motivated ongoing clinical trials of vitamin D supplementation to prevent asthma or asthma morbidity (109, 110).
Vitamin D insufficiency (a serum 25[OH]D < 30 ng/ml) is common among Hispanic Americans in Argentina, Mexico, and Costa Rica (111–114). In a study of 1,025 Mexican children, 28% of subjects aged 6 to 12 years had vitamin D insufficiency (113), which was more common in urban (43%) than rural (25%) areas. Vitamin D insufficiency was common and associated with asthma morbidity in a study of 616 Costa Rican children (114).
In two studies, vitamin D insufficiency was found in ∼90% of Mexican Americans aged 12 years and older (110) and in more than 44% of school-aged children in Puerto Rico (115). Among 273 children with asthma in Puerto Rico, vitamin D insufficiency was associated with severe exacerbations, with a greater effect estimate in nonatopic children (OR = 6.2; 95% CI, 2–21.6) than in atopic children (OR = 2.0; 95% CI, 1–4.1) (115). Although preliminary, these findings suggest that vitamin D partly impacts asthma exacerbations through nonatopic mechanisms (e.g., steroid responsiveness or immune modulation of viral infections).
Obesity
Obesity is associated with asthma (116, 117), asthma morbidity (118–121), and reduced response to ICS (122, 123) in children and adults, with most—but not all—studies showing a stronger link in female than in male subjects. The explanation for these observations is the subject of intense research (124, 125).
Obesity is becoming increasingly more common in Hispanic America (126–129). In the United States, overweight or obesity is common and associated with asthma in Mexican Americans and Puerto Ricans (130–134). A study of 681,122 children in California found that body mass index was more strongly associated with asthma in Hispanics (predominantly Mexican Americans) than in other ethnic groups (135). Of relevance to Mexican Americans and other Hispanic subgroups with substantial Native American ancestry, a recent systematic review found obesity rates in the United States to be highest in American Indians (136).
Few reports have examined obesity and asthma morbidity in U.S. Hispanics. Among African American and Hispanic (∼29% Mexican and ∼40% Puerto Rican) children, obesity was associated with poor asthma control in boys, regardless of ethnicity. Among girls, however, obesity was more strongly associated with poor asthma control in Mexican Americans (OR = 1.91; 95% CI, 1.12–3.28) (137). Of note, only 17.6% of participants in that study had well-controlled asthma. In a study of Puerto Rican children, adiposity measures other than body mass index (percent body fat, waist circumference, and waist-to-hip ratio) provided a better assessment of obesity and asthma in Puerto Ricans, in whom atopy may mediate the effect of obesity on asthma morbidity (132).
Parasitic Infections
Few studies have examined the complex relation between parasitic infection and asthma in Hispanics (138–141). Data from Hispanic America indicate that chronic parasitic (11, 138, 142) and other infections (142) of childhood are associated with lower risk of atopy, but the effects on asthma are less clear. Allergic sensitization to Ascaris, but not active infections per se, appears to be a risk factor for asthma symptoms (140, 143), an observation that could be explained by migration of Ascaris larvae to the lungs with periodic exposures (140). Sensitization to Ascaris has been associated with asthma morbidity or airway responsiveness among children in Costa Rica (where parasitism is rare) (139) and rural Venezuela (144). A study of Ecuadorean schoolchildren provided some evidence that active parasitic infections might attenuate the association between atopy and wheeze (140) and is supported by the observation of a lower prevalence of atopic wheeze among children with heavy parasite burdens with Trichuris trichiura (145).
A study comparing schoolchildren living in Ecuadorean communities who were and were not treated with antihelminthics over 15 to 17 years found that treatment was associated with a higher prevalence of atopy but did not appear to affect asthma symptoms (138). Ongoing longitudinal studies (146) and clinical trials should help advance this field.
Diagnosis and Management of Asthma in Hispanics
Hispanic America
Recent studies continue to suggest that barriers to diagnosis and management of asthma in Hispanic America include inadequate disease-specific education and healthcare access (e.g., spirometric testing or use of controller medications), both of which can lead to poor asthma control (147). Only 8% of participants in a study of adults and adolescents with current asthma in four Latin American countries and Puerto Rico could be objectively classified as having well-controlled disease, even though ∼60% believed that their asthma was completely or well controlled (147).
Over the last few years, implementation of nationwide programs that focused on improving education, diagnosis, and (particularly) treatment has been correlated with reduced use of specialty care (148), increased use of controller medications (149), and decreased morbidity/mortality from asthma (148, 149) among children and adults in El Salvador, Chile, and Costa Rica.
United States
Recent studies suggest that language barriers (150), lack of health insurance (151, 152), inadequate health literacy (153), and cultural beliefs continue to contribute to asthma morbidity among U.S. Hispanics.
Hispanics continue to be less likely to be prescribed or adhere to controller medications such as ICS (154–156). A nationwide study of 2,499 children showed that although the use of preventive asthma medications increased in all ethnic groups from 1988 through 2004 to 2005 through 2008, Mexican Americans were 40% less likely to use preventive asthma medications than whites at the end of follow-up (95% CI for OR, 0.4–0.9), even after accounting for health insurance and other covariates (154). In a study of 277 children who were prescribed controller medications for asthma, Puerto Ricans or Dominicans in Rhode Island and Puerto Ricans in Puerto Rico were less likely to adhere to treatment than NH whites in Rhode Island (156). Among all children, family organization and parental beliefs were associated with medication adherence after accounting for SES (156). Nonadherence with controller medications may also be due to concerns about side effects, medication costs, language barriers, and low expectations for asthma control (157, 158).
Inadequate literacy or numeracy (understanding of basic mathematics) may be a barrier to asthma management in children of Mexican (159) and Puerto Rican (153) descent. Among Puerto Rican children (153), low parental numeracy was associated with visits to the ED or urgent care for asthma. Among participants not using ICS, low parental numeracy was associated with nearly threefold increased odds of one or more hospitalizations for asthma (95% CI, 1.4–5.6; P < 0.01) (153).
Subjective perception of lung function may differ by ethnicity (160). In a study of school-aged children, NH whites in Rhode Island had a more accurate perception of their peak flow measurement than either Puerto Ricans in Puerto Rico or Hispanics in Rhode Island. More accurate perception of lung function was in turn associated with decreased healthcare use for asthma (160).
The efficacy of asthma medications may vary across Hispanic subgroups. Puerto Ricans have lower bronchodilator responsiveness than subjects of Mexican descent (161). Genetic variants may explain this finding, but confirmatory studies are needed (162).
A home-based study in Puerto Rico assessed an intervention consisting of educating families of low-income children on culturally appropriate asthma management (163). Such intervention was associated with decreased ED use, hospitalizations, and nighttime symptoms. Findings from this and another study (164) support further assessment of culturally tailored interventions to improve asthma management in Puerto Ricans and other Hispanic subgroups.
Future Directions
Considerable progress has been made in identifying or better understanding potential protective or risk factors for asthma in Hispanic subgroups (Table E2), but many questions remain unanswered.
Studies of asthma in Hispanic America should focus on EL factors that are more relevant to asthma in this region, including urbanization, parasitism, SHS, air pollution, obesity, and stress.
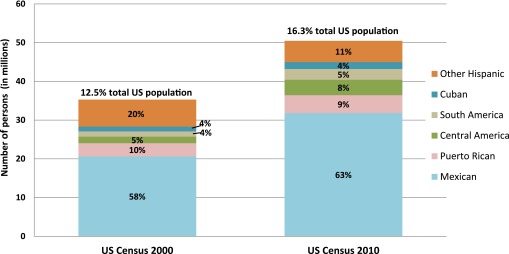
In the United States, studies of asthma in Hispanic subgroups other than Puerto Ricans or Mexican Americans are needed. Further understanding of the “Hispanic Paradox” can be gained by identifying genetic, epigenetic, and EL factors that predispose Puerto Ricans or protect Mexican Americans against asthma (Figure 2). Such factors may include but are not limited to rare genetic variants, DNA methylation, prematurity (165), SHS, diet, and stress. In parallel with this effort, studies of factors that are common in both Puerto Ricans and Mexican Americans and may affect asthma (obesity or vitamin D insufficiency) are needed. Regarding clinical trials, culturally appropriate interventions that address multiple aspects of asthma management should be prioritized for funding.
Figure 2.
Potential explanations for the discrepancy in asthma or asthma morbidity between Mexican Americans and Puerto Ricans (the “Hispanic Paradox”).
The Affordable Care Act (ACA) should improve healthcare access and asthma management in previously uninsured Hispanics (166). However, several barriers may preclude optimal asthma care for those newly insured or those not covered by the ACA (e.g., migrants without legal residency status, children in states not approving Medicaid expansion). Removing residual barriers to care for the insured, coupled with advocacy for broader healthcare access, are essential to optimize asthma care in Hispanics.
Footnotes
Supported by National Institutes of Health grants HL079966, HL073373, and HL117191 (J.C.C.), and Wellcome Trust grant 088862/B/09/Z (P.J.C.).
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org
Originally Published in Press as DOI: 10.1164/rccm.201401-0186PP on April 8, 2014
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Hunninghake GM, Weiss ST, Celedón JC. Asthma in Hispanics. Am J Respir Crit Care Med. 2006;173:143–163. doi: 10.1164/rccm.200508-1232SO. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ennis SR, Rios-Vargas M, Albert NG. The Hispanic population: 2010: 2010 Census Brief. United States Census Bureau, C2010BR-04; May 2011. pp. 1–16
- 3.Central Intelligence AgencyThe world factbook [updated 2014 Mar 27; accessed 2013 Aug 29]. Available from: https://www.cia.gov/library/publications/the-world-factbook/geos/gy.html
- 4.Malik K. Summary human development report 2013. the rise of the south: human progress in a diverse world. United Nations Development Programme. 2013 [accessed 2013 Aug 29]. Available from: http://hdr.undp.org/sites/default/files/hdr2013_en_summary.pdf
- 5.The World Bank. Health expenditure per capita. United Nations [accessed 2013 Aug 23]. Available from: http://data.worldbank.org/indicator/sh.xpd.pcap/countries
- 6.United States Census Bureau. American factbook American community survey-1 year2012[accessed 2013 Aug 29]. Available from: http://factfinder2.census.gov
- 7.Bustamante AV, Fang H, Rizzo JA, Ortega AN. Heterogeneity in health insurance coverage among US Latino adults. J Gen Intern Med. 2009;24:561–566. doi: 10.1007/s11606-009-1069-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mallol J, Solé D, Baeza-Bacab M, Aguirre-Camposano V, Soto-Quiros M, Baena-Cagnani C Latin American ISAAC Group. Regional variation in asthma symptom prevalence in Latin American children. J Asthma. 2010;47:644–650. doi: 10.3109/02770901003686480. [DOI] [PubMed] [Google Scholar]
- 9.To T, Stanojevic S, Moores G, Gershon AS, Bateman ED, Cruz AA, Boulet LP. Global asthma prevalence in adults: findings from the cross-sectional world health survey. BMC Public Health. 2012;12:204. doi: 10.1186/1471-2458-12-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dennis RJ, Caraballo L, García E, Rojas MX, Rondon MA, Pérez A, Aristizabal G, Peñaranda A, Barragan AM, Ahumada V, et al. Prevalence of asthma and other allergic conditions in Colombia 2009-2010: a cross-sectional study. BMC Pulm Med. 2012;12:17. doi: 10.1186/1471-2466-12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cooper PJ, Vaca M, Rodriguez A, Chico ME, Santos DN, Rodrigues LC, Barreto ML. Hygiene, atopy and wheeze-eczema-rhinitis symptoms in schoolchildren from urban and rural Ecuador. Thorax. 2014;69:232–239. doi: 10.1136/thoraxjnl-2013-203818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Neffen H, Baena-Cagnani C, Passalacqua G, Canonica GW, Rocco D. Asthma mortality, inhaled steroids, and changing asthma therapy in Argentina (1990-1999) Respir Med. 2006;100:1431–1435. doi: 10.1016/j.rmed.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 13.Leong AB, Ramsey CD, Celedón JC. The challenge of asthma in minority populations. Clin Rev Allergy Immunol. 2012;43:156–183. doi: 10.1007/s12016-011-8263-1. [DOI] [PubMed] [Google Scholar]
- 14.Subramanian SV, Jun HJ, Kawachi I, Wright RJ. Contribution of race/ethnicity and country of origin to variations in lifetime reported asthma: evidence for a nativity advantage. Am J Public Health. 2009;99:690–697. doi: 10.2105/AJPH.2007.128843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moorman JE, Zahran H, Truman BI, Molla MT Centers for Disease Control and Prevention (CDC) Current asthma prevalence - United States, 2006-2008. MMWR Surveill Summ. 2011;60:84–86. [PubMed] [Google Scholar]
- 16.Lara M, Akinbami L, Flores G, Morgenstern H. Heterogeneity of childhood asthma among Hispanic children: Puerto Rican children bear a disproportionate burden. Pediatrics. 2006;117:43–53. doi: 10.1542/peds.2004-1714. [DOI] [PubMed] [Google Scholar]
- 17.Dumanovsky T, Matte TD. Variation in adult asthma prevalence in Hispanic subpopulations in New York City. J Asthma. 2007;44:297–303. doi: 10.1080/02770900701344140. [DOI] [PubMed] [Google Scholar]
- 18.Akinbami LJ, Moorman JE, Bailey C, Zahran HS, King M, Johnson CA, Liu X. Trends in asthma prevalence, health care use, and mortality in the United States, 2001–2010. NCHS Data Brief. 2012;94:1–8. [PubMed] [Google Scholar]
- 19.Rose D, Mannino DM, Leaderer BP. Asthma prevalence among US adults, 1998-2000: role of Puerto Rican ethnicity and behavioral and geographic factors. Am J Public Health. 2006;96:880–888. doi: 10.2105/AJPH.2004.050039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holguin F, Mannino DM, Antó J, Mott J, Ford ES, Teague WG, Redd SC, Romieu I. Country of birth as a risk factor for asthma among Mexican Americans. Am J Respir Crit Care Med. 2005;171:103–108. doi: 10.1164/rccm.200402-143OC. [DOI] [PubMed] [Google Scholar]
- 21.Eldeirawi K, McConnell R, Freels S, Persky VW. Associations of place of birth with asthma and wheezing in Mexican American children. J Allergy Clin Immunol. 2005;116:42–48. doi: 10.1016/j.jaci.2005.03.041. [DOI] [PubMed] [Google Scholar]
- 22.Eldeirawi KM, Persky VW. Associations of acculturation and country of birth with asthma and wheezing in Mexican American youths. J Asthma. 2006;43:279–286. doi: 10.1080/0277090060022869. [DOI] [PubMed] [Google Scholar]
- 23.Cohen RT, Canino GJ, Bird HR, Shen S, Rosner BA, Celedón JC. Area of residence, birthplace, and asthma in Puerto Rican children. Chest. 2007;131:1331–1338. doi: 10.1378/chest.06-1917. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. CDC health disparities and inequalities report- United States, 2013. MMWR Morb Mortal Wkly Rep. 2013;62:93–160. [Google Scholar]
- 25.Everhart RS, Koinis-Mitchell D, McQuaid EL, Kopel S, Seifer R, Canino G, Fritz G. Ethnic differences in caregiver quality of life in pediatric asthma. J Dev Behav Pediatr. 2012;33:599–607. doi: 10.1097/DBP.0b013e318264c2b7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Canino G, Garro A, Alvarez MM, Colón-Semidey A, Esteban C, Fritz G, Koinis-Mitchell D, Kopel SJ, Ortega AN, Seifer R, et al. Factors associated with disparities in emergency department use among Latino children with asthma. Ann Allergy Asthma Immunol. 2012;108:266–270. doi: 10.1016/j.anai.2012.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Homa DM, Mannino DM, Lara M. Asthma mortality in U.S. Hispanics of Mexican, Puerto Rican, and Cuban heritage, 1990–1995. Am J Respir Crit Care Med. 2000;161:504–509. doi: 10.1164/ajrccm.161.2.9906025. [DOI] [PubMed] [Google Scholar]
- 28.Sly RM. Decreases in Hispanic and non-Hispanic asthma mortality. Ann Allergy Asthma Immunol. 2006;96:76–79. doi: 10.1016/S1081-1206(10)61043-5. [DOI] [PubMed] [Google Scholar]
- 29.American Lung Association. Trends in asthma morbidity and mortality. 2012 [created 2012 Sept; accessed 2013 Sept 29]. Available from: http://www.lung.org/finding-cures/our-research/trend-reports/asthma-trend-report.pdf
- 30.Chen W, Brehm JM, Boutaoui N, Soto-Quiros M, Avila L, Celli BR, Bruse S, Tesfaigzi Y, Celedón JC. Native American ancestry, lung function and COPD in Costa Ricans. Chest. 2014;145:704–710. doi: 10.1378/chest.13-1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brehm JM, Acosta-Perez E, Klei L, Roeder K, Barmada MM, Boutaoui N, Forno E, Cloutier MM, Datta S, Kelly R, et al. African ancestry and lung function in Puerto Rican children J Allergy Clin Immunol 20121291484–1490.e6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Galanter JM, Fernandez-Lopez JC, Gignoux CR, Barnholtz-Sloan J, Fernandez-Rozadilla C, Via M, Hidalgo-Miranda A, Contreras AV, Figueroa LU, Raska P, et al. LACE Consortium. Development of a panel of genome-wide ancestry informative markers to study admixture throughout the Americas. PLoS Genet. 2012;8:e1002554. doi: 10.1371/journal.pgen.1002554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Choudhry S, Burchard EG, Borrell LN, Tang H, Gomez I, Naqvi M, Nazario S, Torres A, Casal J, Martinez-Cruzado JC, et al. Ancestry-environment interactions and asthma risk among Puerto Ricans. Am J Respir Crit Care Med. 2006;174:1088–1093. doi: 10.1164/rccm.200605-596OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vergara C, Caraballo L, Mercado D, Jimenez S, Rojas W, Rafaels N, Hand T, Campbell M, Tsai YJ, Gao L, et al. African ancestry is associated with risk of asthma and high total serum IgE in a population from the Caribbean Coast of Colombia. Hum Genet. 2009;125:565–579. doi: 10.1007/s00439-009-0649-2. [DOI] [PubMed] [Google Scholar]
- 35.Harik-Khan RI, Muller DC, Wise RA. Racial difference in lung function in African-American and White children: effect of anthropometric, socioeconomic, nutritional, and environmental factors. Am J Epidemiol. 2004;160:893–900. doi: 10.1093/aje/kwh297. [DOI] [PubMed] [Google Scholar]
- 36.Kumar R, Seibold MA, Aldrich MC, Williams LK, Reiner AP, Colangelo L, Galanter J, Gignoux C, Hu D, Sen S, et al. Genetic ancestry in lung-function predictions. N Engl J Med. 2010;363:321–330. doi: 10.1056/NEJMoa0907897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bruse S, Sood A, Petersen H, Liu Y, Leng S, Celedón JC, Gilliland F, Celli B, Belinsky SA, Tesfaigzi Y. New Mexican Hispanic smokers have lower odds of chronic obstructive pulmonary disease and less decline in lung function than non-Hispanic whites. Am J Respir Crit Care Med. 2011;184:1254–1260. doi: 10.1164/rccm.201103-0568OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Torgerson DG, Ampleford EJ, Chiu GY, Gauderman WJ, Gignoux CR, Graves PE, Himes BE, Levin AM, Mathias RA, Hancock DB, et al. Mexico City Childhood Asthma Study (MCAAS); Children’s Health Study (CHS) and HARBORS study; Genetics of Asthma in Latino Americans (GALA) Study, Study of Genes-Environment and Admixture in Latino Americans (GALA2) and Study of African Americans, Asthma, Genes & Environments (SAGE); Childhood Asthma Research and Education (CARE) Network; Childhood Asthma Management Program (CAMP); Study of Asthma Phenotypes and Pharmacogenomic Interactions by Race-Ethnicity (SAPPHIRE); Genetic Research on Asthma in African Diaspora (GRAAD) Study. Meta-analysis of genome-wide association studies of asthma in ethnically diverse North American populations. Nat Genet. 2011;43:887–892. doi: 10.1038/ng.888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Galanter JM, Torgerson D, Gignoux CR, Sen S, Roth LA, Via M, Aldrich MC, Eng C, Huntsman S, Rodriguez-Santana J, et al. Cosmopolitan and ethnic-specific replication of genetic risk factors for asthma in 2 Latino populations J Allergy Clin Immunol 201112837–43.e12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hunninghake GM, Lasky-Su J, Soto-Quirós ME, Avila L, Liang C, Lake SL, Hudson TJ, Spesny M, Fournier E, Sylvia JS, et al. Sex-stratified linkage analysis identifies a female-specific locus for IgE to cockroach in Costa Ricans. Am J Respir Crit Care Med. 2008;177:830–836. doi: 10.1164/rccm.200711-1697OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hunninghake GM, Soto-Quirós ME, Avila L, Kim HP, Lasky-Su J, Rafaels N, Ruczinski I, Beaty TH, Mathias RA, Barnes KC, et al. TSLP polymorphisms are associated with asthma in a sex-specific fashion. Allergy. 2010;65:1566–1575. doi: 10.1111/j.1398-9995.2010.02415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Forno E, Lasky-Su J, Himes B, Howrylak J, Ramsey C, Brehm J, Klanderman B, Ziniti J, Melen E, Pershagen G, et al. Genome-wide association study of the age of onset of childhood asthma J Allergy Clin Immunol 201213083–90.e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Galanter J, Choudhry S, Eng C, Nazario S, Rodríguez-Santana JR, Casal J, Torres-Palacios A, Salas J, Chapela R, Watson HG, et al. ORMDL3 gene is associated with asthma in three ethnically diverse populations. Am J Respir Crit Care Med. 2008;177:1194–1200. doi: 10.1164/rccm.200711-1644OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wu H, Romieu I, Sienra-Monge JJ, Li H, del Rio-Navarro BE, London SJ. Genetic variation in ORM1-like 3 (ORMDL3) and gasdermin-like (GSDML) and childhood asthma. Allergy. 2009;64:629–635. doi: 10.1111/j.1398-9995.2008.01912.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.He JQ, Hallstrand TS, Knight D, Chan-Yeung M, Sandford A, Tripp B, Zamar D, Bossé Y, Kozyrskyj AL, James A, et al. A thymic stromal lymphopoietin gene variant is associated with asthma and airway hyperresponsiveness. J Allergy Clin Immunol. 2009;124:222–229. doi: 10.1016/j.jaci.2009.04.018. [DOI] [PubMed] [Google Scholar]
- 46.Manolio TA, Collins FS, Cox NJ, Goldstein DB, Hindorff LA, Hunter DJ, McCarthy MI, Ramos EM, Cardon LR, Chakravarti A, et al. Finding the missing heritability of complex diseases. Nature. 2009;461:747–753. doi: 10.1038/nature08494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hunt KA, Mistry V, Bockett NA, Ahmad T, Ban M, Barker JN, Barrett JC, Blackburn H, Brand O, Burren O, et al. Negligible impact of rare autoimmune-locus coding-region variants on missing heritability. Nature. 2013;498:232–235. doi: 10.1038/nature12170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Raby BA, Soto-Quiros ME, Avila L, Lake SL, Murphy A, Liang C, Fournier E, Spesny M, Sylvia JS, Verner A, et al. Sex-specific linkage to total serum immunoglobulin E in families of children with asthma in Costa Rica. Hum Mol Genet. 2007;16:243–253. doi: 10.1093/hmg/ddl447. [DOI] [PubMed] [Google Scholar]
- 49.Wu H, Romieu I, Sienra-Monge JJ, del Rio-Navarro BE, Anderson DM, Dunn EW, Steiner LL, Lara-Sanchez IdelC, London SJ. Parental smoking modifies the relation between genetic variation in tumor necrosis factor-alpha (TNF) and childhood asthma. Environ Health Perspect. 2007;115:616–622. doi: 10.1289/ehp.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hunninghake GM, Soto-Quiros ME, Lasky-Su J, Avila L, Ly NP, Liang C, Klanderman BJ, Raby BA, Gold DR, Weiss ST, et al. Dust mite exposure modifies the effect of functional il10 polymorphisms on allergy and asthma exacerbations. J Allergy Clin Immunol. 2008;122:93–98. doi: 10.1016/j.jaci.2008.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sharma S, Raby BA, Hunninghake GM, Soto-Quirós M, Avila L, Murphy AJ, Lasky-Su J, Klanderman BJ, Sylvia JS, Weiss ST, et al. Variants in TGFB1, dust mite exposure, and disease severity in children with asthma. Am J Respir Crit Care Med. 2009;179:356–362. doi: 10.1164/rccm.200808-1268OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cooper PJ, Rodrigues LC, Barreto ML. Influence of poverty and infection on asthma in Latin America. Curr Opin Allergy Clin Immunol. 2012;12:171–178. doi: 10.1097/ACI.0b013e3283510967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.da Cunha SS, Pujades-Rodriguez M, Barreto ML, Genser B, Rodrigues LC. Ecological study of socio-economic indicators and prevalence of asthma in schoolchildren in urban Brazil. BMC Public Health. 2007;7:205. doi: 10.1186/1471-2458-7-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rodriguez A, Vaca M, Oviedo G, Erazo S, Chico ME, Teles C, Barreto ML, Rodrigues LC, Cooper PJ. Urbanisation is associated with prevalence of childhood asthma in diverse, small rural communities in Ecuador. Thorax. 2011;66:1043–1050. doi: 10.1136/thoraxjnl-2011-200225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Robinson CL, Baumann LM, Romero K, Combe JM, Gomez A, Gilman RH, Cabrera L, Gonzalvez G, Hansel NN, Wise RA, et al. Effect of urbanisation on asthma, allergy and airways inflammation in a developing country setting. Thorax. 2011;66:1051–1057. doi: 10.1136/thx.2011.158956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Valdivia CG, Caussade LS, Navarro MH, Cerda LJ, Pérez BE, Aquevedo SA, Sánchez DI. Changes in asthma prevalence among school children during a 6 -year period: Influence of socioeconomic status [in Spanish] Rev Med Chil. 2009;137:215–225. [PubMed] [Google Scholar]
- 57.Fattore GL, Santos CA, Barreto ML. Social determinants of childhood asthma symptoms: An ecological study in urban Latin America. J Community Health. 2014;39:355–362. doi: 10.1007/s10900-013-9769-7. [DOI] [PubMed] [Google Scholar]
- 58.Forno E, Celedon JC. Asthma and ethnic minorities: socioeconomic status and beyond. Curr Opin Allergy Clin Immunol. 2009;9:154–160. doi: 10.1097/aci.0b013e3283292207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Forno E, Celedón JC. Health disparities in asthma. Am J Respir Crit Care Med. 2012;185:1033–1035. doi: 10.1164/rccm.201202-0350ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Thakur N, Oh SS, Nguyen EA, Martin M, Roth LA, Galanter J, Gignoux CR, Eng C, Davis A, Meade K, et al. Socioeconomic status and childhood asthma in urban minority youths. The GALA II and SAGE II studies. Am J Respir Crit Care Med. 2013;188:1202–1209. doi: 10.1164/rccm.201306-1016OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Holt EW, Theall KP, Rabito FA. Individual, housing, and neighborhood correlates of asthma among young urban children. J Urban Health. 2013;90:116–129. doi: 10.1007/s11524-012-9709-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Turyk ME, Hernandez E, Wright RJ, Freels S, Slezak J, Contraras A, Piorkowski J, Persky VW. Stressful life events and asthma in adolescents. Pediatr Allergy Immunol. 2008;19:255–263. doi: 10.1111/j.1399-3038.2007.00603.x. [DOI] [PubMed] [Google Scholar]
- 63.Clougherty JE, Levy JI, Kubzansky LD, Ryan PB, Suglia SF, Canner MJ, Wright RJ. Synergistic effects of traffic-related air pollution and exposure to violence on urban asthma etiology. Environ Health Perspect. 2007;115:1140–1146. doi: 10.1289/ehp.9863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sternthal MJ, Jun HJ, Earls F, Wright RJ. Community violence and urban childhood asthma: a multilevel analysis. Eur Respir J. 2010;36:1400–1409. doi: 10.1183/09031936.00003010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Apter AJ, Garcia LA, Boyd RC, Wang X, Bogen DK, Ten Have T. Exposure to community violence is associated with asthma hospitalizations and emergency department visits. J Allergy Clin Immunol. 2010;126:552–557. doi: 10.1016/j.jaci.2010.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wright RJ, Mitchell H, Visness CM, Cohen S, Stout J, Evans R, Gold DR. Community violence and asthma morbidity: the Inner-City Asthma Study. Am J Public Health. 2004;94:625–632. doi: 10.2105/ajph.94.4.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sandberg S, Paton JY, Ahola S, McCann DC, McGuinness D, Hillary CR, Oja H. The role of acute and chronic stress in asthma attacks in children. Lancet. 2000;356:982–987. doi: 10.1016/S0140-6736(00)02715-X. [DOI] [PubMed] [Google Scholar]
- 68.Chen E, Chim LS, Strunk RC, Miller GE. The role of the social environment in children and adolescents with asthma. Am J Respir Crit Care Med. 2007;176:644–649. doi: 10.1164/rccm.200610-1473OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Swahn MH, Bossarte RM. The associations between victimization, feeling unsafe, and asthma episodes among US high-school students. Am J Public Health. 2006;96:802–804. doi: 10.2105/AJPH.2005.066514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cohen RT, Canino GJ, Bird HR, Celedón JC. Violence, abuse, and asthma in Puerto Rican children. Am J Respir Crit Care Med. 2008;178:453–459. doi: 10.1164/rccm.200711-1629OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Torres JM, Wallace SP. Migration circumstances, psychological distress, and self-rated physical health for Latino immigrants in the United States. Am J Public Health. 2013;103:1619–1627. doi: 10.2105/AJPH.2012.301195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Byrd DR. Race/ethnicity and self-reported levels of discrimination and psychological distress, California, 2005. Prev Chronic Dis. 2012;9:E156. doi: 10.5888/pcd9.120042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Crouch J, Hanson R, Saunders B, Kilpatrick D, Resnick H. Income, race/ethnicity, and exposure to violence in youth: results from the national survey of adolescents. J Community Psychol. 2000;28:625–641. [Google Scholar]
- 74.Martin MA, Shalowitz MU, Mijanovich T, Clark-Kauffman E, Perez E, Berry CA. The effects of acculturation on asthma burden in a community sample of Mexican American schoolchildren. Am J Public Health. 2007;97:1290–1296. doi: 10.2105/AJPH.2006.092239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gupta RS, Ballesteros J, Springston EE, Smith B, Martin M, Wang E, Damitz M. The state of pediatric asthma in Chicago’s Humboldt Park: a community-based study in two local elementary schools. BMC Pediatr. 2010;10:45. doi: 10.1186/1471-2431-10-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Vangeepuram N, Galvez MP, Teitelbaum SL, Brenner B, Wolff MS. The association between parental perception of neighborhood safety and asthma diagnosis in ethnic minority urban children. J Urban Health. 2012;89:758–768. doi: 10.1007/s11524-012-9679-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Feldman JM, Ortega AN, Koinis-Mitchell D, Kuo AA, Canino G. Child and family psychiatric and psychological factors associated with child physical health problems: results from the Boricua youth study. J Nerv Ment Dis. 2010;198:272–279. doi: 10.1097/NMD.0b013e3181d61271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lange NE, Bunyavanich S, Silberg JL, Canino G, Rosner BA, Celedon JC.Parental psychosocial stress and asthma morbidity in Puerto Rican twins J Allergy Clin Immunol 2011127734–740.e1–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Miller GE, Chen E. Life stress and diminished expression of genes encoding glucocorticoid receptor and beta2-adrenergic receptor in children with asthma. Proc Natl Acad Sci USA. 2006;103:5496–5501. doi: 10.1073/pnas.0506312103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chen E, Fisher EB, Bacharier LB, Strunk RC. Socioeconomic status, stress, and immune markers in adolescents with asthma. Psychosom Med. 2003;65:984–992. doi: 10.1097/01.psy.0000097340.54195.3c. [DOI] [PubMed] [Google Scholar]
- 81.Marin TJ, Chen E, Munch JA, Miller GE. Double-exposure to acute stress and chronic family stress is associated with immune changes in children with asthma. Psychosom Med. 2009;71:378–384. doi: 10.1097/PSY.0b013e318199dbc3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Clougherty JE, Rossi CA, Lawrence J, Long MS, Diaz EA, Lim RH, McEwen B, Koutrakis P, Godleski JJ. Chronic social stress and susceptibility to concentrated ambient fine particles in rats. Environ Health Perspect. 2010;118:769–775. doi: 10.1289/ehp.0901631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Islam T, Urman R, Gauderman WJ, Milam J, Lurmann F, Shankardass K, Avol E, Gilliland F, McConnell R. Parental stress increases the detrimental effect of traffic exposure on children’s lung function. Am J Respir Crit Care Med. 2011;184:822–827. doi: 10.1164/rccm.201104-0720OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Shankardass K, McConnell R, Jerrett M, Milam J, Richardson J, Berhane K. Parental stress increases the effect of traffic-related air pollution on childhood asthma incidence. Proc Natl Acad Sci USA. 2009;106:12406–12411. doi: 10.1073/pnas.0812910106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ressler KJ, Mercer KB, Bradley B, Jovanovic T, Mahan A, Kerley K, Norrholm SD, Kilaru V, Smith AK, Myers AJ, et al. Post-traumatic stress disorder is associated with PACAP and the PAC1 receptor. Nature. 2011;470:492–497. doi: 10.1038/nature09856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Jovanovic T, Norrholm SD, Davis J, Mercer KB, Almli L, Nelson A, Cross D, Smith A, Ressler KJ, Bradley B. PAC1 receptor (ADCYAP1R1) genotype is associated with dark-enhanced startle in children. Mol Psychiatry. 2013;18:742–743. doi: 10.1038/mp.2012.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chen W, Boutaoui N, Brehm JM, Han YY, Schmitz C, Cressley A, Acosta-Pérez E, Alvarez M, Colón-Semidey A, Baccarelli AA, et al. ADCYAP1R1 and asthma in Puerto Rican children. Am J Respir Crit Care Med. 2013;187:584–588. doi: 10.1164/rccm.201210-1789OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Li S, Williams G, Jalaludin B, Baker P. Panel studies of air pollution on children’s lung function and respiratory symptoms: a literature review. J Asthma. 2012;49:895–910. doi: 10.3109/02770903.2012.724129. [DOI] [PubMed] [Google Scholar]
- 89.Silverman RA, Ito K.Age-related association of fine particles and ozone with severe acute asthma in New York City J Allergy Clin Immunol 2010125367–373.e5 [DOI] [PubMed] [Google Scholar]
- 90.Portnov BA, Reiser B, Karkabi K, Cohen-Kastel O, Dubnov J. High prevalence of childhood asthma in Northern Israel is linked to air pollution by particulate matter: evidence from GIS analysis and Bayesian Model Averaging. Int J Environ Health Res. 2012;22:249–269. doi: 10.1080/09603123.2011.634387. [DOI] [PubMed] [Google Scholar]
- 91.Auerbach A, Hernandez ML. The effect of environmental oxidative stress on airway inflammation. Curr Opin Allergy Clin Immunol. 2012;12:133–139. doi: 10.1097/ACI.0b013e32835113d6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gómez M, Vollmer WM, Caceres ME, Jossen R, Baena-Cagnani CE. Adolescent smokers are at greater risk for current asthma and rhinitis. Int J Tuberc Lung Dis. 2009;13:1023–1028. [PubMed] [Google Scholar]
- 93.Vázquez-Rodríguez CF, Vázquez-Nava F, Vázquez-Rodríguez EM, Morales-Romero J, Iribar-Ibabe MC, Peinado-Herreros J. Smoking in non-student Mexican adolescents with asthma: relation with family structure, educational level, parental approval of smoking, parents who smoke, and smoking friends. Arch Bronconeumol. 2012;48:37–42. doi: 10.1016/j.arbres.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 94.Carbajal-Arroyo L, Barraza-Villarreal A, Durand-Pardo R, Moreno-Macías H, Espinoza-Laín R, Chiarella-Ortigosa P, Romieu I. Impact of traffic flow on the asthma prevalence among school children in Lima, Peru. J Asthma. 2007;44:197–202. doi: 10.1080/02770900701209756. [DOI] [PubMed] [Google Scholar]
- 95.Baumann LM, Robinson CL, Combe JM, Gomez A, Romero K, Gilman RH, Cabrera L, Hansel NN, Wise RA, Breysse PN, et al. Effects of distance from a heavily transited avenue on asthma and atopy in a periurban shantytown in Lima, Peru. J Allergy Clin Immunol. 2011;127:875–882. doi: 10.1016/j.jaci.2010.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Escamilla-Nuñez MC, Barraza-Villarreal A, Hernandez-Cadena L, Moreno-Macias H, Ramirez-Aguilar M, Sienra-Monge JJ, Cortez-Lugo M, Texcalac JL, del Rio-Navarro B, Romieu I. Traffic-related air pollution and respiratory symptoms among asthmatic children, resident in Mexico City: the EVA cohort study. Respir Res. 2008;9:74. doi: 10.1186/1465-9921-9-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Barraza-Villarreal A, Sunyer J, Hernandez-Cadena L, Escamilla-Nuñez MC, Sienra-Monge JJ, Ramírez-Aguilar M, Cortez-Lugo M, Holguin F, Diaz-Sánchez D, Olin AC, et al. Air pollution, airway inflammation, and lung function in a cohort study of Mexico City schoolchildren. Environ Health Perspect. 2008;116:832–838. doi: 10.1289/ehp.10926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bell ML, Davis DL, Gouveia N, Borja-Aburto VH, Cifuentes LA. The avoidable health effects of air pollution in three Latin American cities: Santiago, São Paulo, and Mexico City. Environ Res. 2006;100:431–440. doi: 10.1016/j.envres.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 99.Wichmann FA, Muller A, Busi LE, Cianni N, Massolo L, Schlink U, Porta A, Sly PD. Increased asthma and respiratory symptoms in children exposed to petrochemical pollution. J Allergy Clin Immunol. 2009;123:632–638. doi: 10.1016/j.jaci.2008.09.052. [DOI] [PubMed] [Google Scholar]
- 100.Meng YY, Rull RP, Wilhelm M, Ritz B, English P, Yu H, Nathan S, Kuruvilla M, Brown ER.Living near heavy traffic increases asthma severity Policy Brief UCLA Cent Health Policy Res 2006. Aug:1–5. [PubMed] [Google Scholar]
- 101.Nishimura KK, Galanter JM, Roth LA, Oh SS, Thakur N, Nguyen EA, Thyne S, Farber HJ, Serebrisky D, Kumar R, et al. Early-life air pollution and asthma risk in minority children. The GALA II and SAGE II studies. Am J Respir Crit Care Med. 2013;188:309–318. doi: 10.1164/rccm.201302-0264OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Nachman KE, Parker JD. Exposures to fine particulate air pollution and respiratory outcomes in adults using two national datasets: a cross-sectional study. Environ Health. 2012;11:25. doi: 10.1186/1476-069X-11-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Salam MT, Gauderman WJ, McConnell R, Lin PC, Gilliland FD. Transforming growth factor- 1 C-509T polymorphism, oxidant stress, and early-onset childhood asthma. Am J Respir Crit Care Med. 2007;176:1192–1199. doi: 10.1164/rccm.200704-561OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Perzanowski MS, Chew GL, Divjan A, Jung KH, Ridder R, Tang D, Diaz D, Goldstein IF, Kinney PL, Rundle AG, et al. Early-life cockroach allergen and polycyclic aromatic hydrocarbon exposures predict cockroach sensitization among inner-city children. J Allergy Clin Immunol. 2013;131:886–893. doi: 10.1016/j.jaci.2012.12.666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Quinto KB, Kit BK, Lukacs SL, Akinbami LJ. Environmental tobacco smoke exposure in children aged 3–19 years with and without asthma in the United States, 1999–2010. NCHS Data Brief. 2013;126:1–8. [PubMed] [Google Scholar]
- 106.Akinbami LJ, Kit BK, Simon AE. Impact of environmental tobacco smoke on children with asthma, United States, 2003-2010. Acad Pediatr. 2013;13:508–516. doi: 10.1016/j.acap.2013.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Akuete K, Oh SS, Thyne S, Rodriguez-Santana JR, Chapela R, Meade K, Rodriguez-Cintron W, LeNoir M, Ford JG, Williams LK, et al. Ethnic variability in persistent asthma after in utero tobacco exposure. Pediatrics. 2011;128:e623–e630. doi: 10.1542/peds.2011-0640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Oh SS, Tcheurekdjian H, Roth LA, Nguyen EA, Sen S, Galanter JM, Davis A, Farber HJ, Gilliland FD, Kumar R, et al. Effect of secondhand smoke on asthma control among black and Latino children J Allergy Clin Immunol 20121291478–1483.e7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Paul G, Brehm JM, Alcorn JF, Holguín F, Aujla SJ, Celedón JC. Vitamin D and asthma. Am J Respir Crit Care Med. 2012;185:124–132. doi: 10.1164/rccm.201108-1502CI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ginde AA, Liu MC, Camargo CA., Jr Demographic differences and trends of vitamin D insufficiency in the US population, 1988-2004. Arch Intern Med. 2009;169:626–632. doi: 10.1001/archinternmed.2008.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Durán P, Mangialavori G, Biglieri A, Kogan L, Abeyá Gilardon E. Nutrition status in Argentinean children 6 to 72 months old: results from the National Nutrition and Health Survey (ENNyS) [in Spanish] Arch Argent Pediatr. 2009;107:397–404. doi: 10.1590/S0325-00752009000500005. [DOI] [PubMed] [Google Scholar]
- 112.Hirschler V, Maccallini G, Aranda C, Fernando S, Molinari C. Association of vitamin D with glucose levels in indigenous and mixed population Argentinean boys. Clin Biochem. 2013;46:197–201. doi: 10.1016/j.clinbiochem.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 113.Flores M, Macias N, Lozada A, Sánchez LM, Díaz E, Barquera S. Serum 25-hydroxyvitamin D levels among Mexican children ages 2 y to 12 y: a national survey. Nutrition. 2013;29:802–804. doi: 10.1016/j.nut.2012.12.024. [DOI] [PubMed] [Google Scholar]
- 114.Brehm JM, Celedón JC, Soto-Quiros ME, Avila L, Hunninghake GM, Forno E, Laskey D, Sylvia JS, Hollis BW, Weiss ST, et al. Serum vitamin D levels and markers of severity of childhood asthma in Costa Rica. Am J Respir Crit Care Med. 2009;179:765–771. doi: 10.1164/rccm.200808-1361OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Brehm JM, Acosta-Pérez E, Klei L, Roeder K, Barmada M, Boutaoui N, Forno E, Kelly R, Paul K, Sylvia J, et al. Vitamin D insufficiency and severe asthma exacerbations in Puerto Rican children. Am J Respir Crit Care Med. 2012;186:140–146. doi: 10.1164/rccm.201203-0431OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Beuther DA, Sutherland ER. Overweight, obesity, and incident asthma: a meta-analysis of prospective epidemiologic studies. Am J Respir Crit Care Med. 2007;175:661–666. doi: 10.1164/rccm.200611-1717OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Egan KB, Ettinger AS, Bracken MB. Childhood body mass index and subsequent physician-diagnosed asthma: a systematic review and meta-analysis of prospective cohort studies. BMC Pediatr. 2013;13:121. doi: 10.1186/1471-2431-13-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Carroll CL, Bhandari A, Zucker AR, Schramm CM. Childhood obesity increases duration of therapy during severe asthma exacerbations. Pediatr Crit Care Med. 2006;7:527–531. doi: 10.1097/01.PCC.0000243749.14555.E8. [DOI] [PubMed] [Google Scholar]
- 119.Grammer LC, Weiss KB, Pedicano JB, Kimmel LG, Curtis LS, Catrambone CD, Lyttle CS, Sharp LK, Sadowski LS. Obesity and asthma morbidity in a community-based adult cohort in a large urban area: the Chicago Initiative to Raise Asthma Health Equity (CHIRAH) J Asthma. 2010;47:491–495. doi: 10.3109/02770901003801980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Taylor B, Mannino D, Brown C, Crocker D, Twum-Baah N, Holguin F. Body mass index and asthma severity in the National Asthma Survey. Thorax. 2008;63:14–20. doi: 10.1136/thx.2007.082784. [DOI] [PubMed] [Google Scholar]
- 121.Michelson PH, Williams LW, Benjamin DK, Barnato AE. Obesity, inflammation, and asthma severity in childhood: data from the National Health and Nutrition Examination Survey 2001-2004. Ann Allergy Asthma Immunol. 2009;103:381–385. doi: 10.1016/S1081-1206(10)60356-0. [DOI] [PubMed] [Google Scholar]
- 122.Forno E, Lescher R, Strunk R, Weiss S, Fuhlbrigge A, Celedón JC Childhood Asthma Management Program Research Group. Decreased response to inhaled steroids in overweight and obese asthmatic children. J Allergy Clin Immunol. 2011;127:741–749. doi: 10.1016/j.jaci.2010.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Sutherland ER, Goleva E, Strand M, Beuther DA, Leung DY. Body mass and glucocorticoid response in asthma. Am J Respir Crit Care Med. 2008;178:682–687. doi: 10.1164/rccm.200801-076OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Shore SA. Obesity and asthma: possible mechanisms. J Allergy Clin Immunol. 2008;121:1087–1093. doi: 10.1016/j.jaci.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 125.Litonjua AA, Gold DR.Asthma and obesity: common early-life influences in the inception of disease J Allergy Clin Immunol 20081211075–1084.quiz 1085–1086 [DOI] [PubMed] [Google Scholar]
- 126.Linetzky B, De Maio F, Ferrante D, Konfino J, Boissonnet C. Sex-stratified socio-economic gradients in physical inactivity, obesity, and diabetes: evidence of short-term changes in Argentina. Int J Public Health. 2013;58:277–284. doi: 10.1007/s00038-012-0371-z. [DOI] [PubMed] [Google Scholar]
- 127.Webster PC. Health in Colombia: the chronic disease burden. CMAJ. 2012;184:E293–E294. doi: 10.1503/cmaj.109-4126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Garmendia ML, Corvalan C, Uauy R. Addressing malnutrition while avoiding obesity: minding the balance. Eur J Clin Nutr. 2013;67:513–517. doi: 10.1038/ejcn.2012.190. [DOI] [PubMed] [Google Scholar]
- 129.Loret de Mola C, Pillay TD, Diez-Canseco F, Gilman RH, Smeeth L, Miranda JJ. Body mass index and self-perception of overweight and obesity in rural, urban and rural-to-urban migrants: PERU MIGRANT study. PLoS ONE. 2012;7:e50252. doi: 10.1371/journal.pone.0050252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.US Department of Health and Human Services Office of Minority Health. Obesity and Hispanic Americans. US Department of Health and Human Services Office of Minority Health [accessed 2013 Dec 2]. Available from: http://www.minorityhealth.hhs.gov/templates/content.aspx?lvl=3&lvlID=537&ID=6459
- 131.Ai AL, Appel HB, Huang B, Lee K. Overall health and healthcare utilization among Latino American women in the United States. J Womens Health (Larchmt) 2012;21:878–885. doi: 10.1089/jwh.2011.3431. [DOI] [PubMed] [Google Scholar]
- 132.Forno E, Acosta-Pérez E, Brehm JM, Han YY, Alvarez M, Colón-Semidey A, Canino G, Celedón JC. Obesity and adiposity indicators, asthma, and atopy in Puerto Rican children. J Allergy Clin Immunol. 2014;133:1308–1314. doi: 10.1016/j.jaci.2013.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Forrest KY, Leeds MJ. Prevalence and associated factors of overweight among Mexican-American adolescents. J Am Diet Assoc. 2007;107:1797–1800. doi: 10.1016/j.jada.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 134.Vangeepuram N, Teitelbaum SL, Galvez MP, Brenner B, Doucette J, Wolff MS. Measures of obesity associated with asthma diagnosis in ethnic minority children. J Obes. 2011;2011:517417. doi: 10.1155/2011/517417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Black MH, Smith N, Porter AH, Jacobsen SJ, Koebnick C. Higher prevalence of obesity among children with asthma. Obesity (Silver Spring) 2012;20:1041–1047. doi: 10.1038/oby.2012.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Hutchinson RN, Shin S. Systematic review of health disparities for cardiovascular diseases and associated factors among American Indian and Alaska Native populations. PLoS ONE. 2014;9:e80973. doi: 10.1371/journal.pone.0080973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Borrell LN, Nguyen EA, Roth LA, Oh SS, Tcheurekdjian H, Sen S, Davis A, Farber HJ, Avila PC, Brigino-Buenaventura E, et al. Childhood obesity and asthma control in the GALA II and SAGE II studies. Am J Respir Crit Care Med. 2013;187:697–702. doi: 10.1164/rccm.201211-2116OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Endara P, Vaca M, Chico ME, Erazo S, Oviedo G, Quinzo I, Rodriguez A, Lovato R, Moncayo AL, Barreto ML, et al. Long-term periodic anthelmintic treatments are associated with increased allergen skin reactivity. Clin Exp Allergy. 2010;40:1669–1677. doi: 10.1111/j.1365-2222.2010.03559.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Hunninghake GM, Soto-Quiros ME, Avila L, Ly NP, Liang C, Sylvia JS, Klanderman BJ, Silverman EK, Celedón JC. Sensitization to Ascaris lumbricoides and severity of childhood asthma in Costa Rica. J Allergy Clin Immunol. 2007;119:654–661. doi: 10.1016/j.jaci.2006.12.609. [DOI] [PubMed] [Google Scholar]
- 140.Moncayo AL, Vaca M, Oviedo G, Workman LJ, Chico ME, Platts-Mills TA, Rodrigues LC, Barreto ML, Cooper PJ. Effects of geohelminth infection and age on the associations between allergen-specific IgE, skin test reactivity and wheeze: a case-control study. Clin Exp Allergy. 2013;43:60–72. doi: 10.1111/cea.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Walsh MG. Toxocara infection and diminished lung function in a nationally representative sample from the United States population. Int J Parasitol. 2011;41:243–247. doi: 10.1016/j.ijpara.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 142.Alcantara-Neves NM, Veiga RV, Dattoli VC, Fiaccone RL, Esquivel R, Cruz AA, Cooper PJ, Rodrigues LC, Barreto ML. The effect of single and multiple infections on atopy and wheezing in children. J Allergy Clin Immunol. 2012;129:359–367. doi: 10.1016/j.jaci.2011.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Alcântara-Neves NM, Badaró SJ, dos Santos MC, Pontes-de-Carvalho L, Barreto ML. The presence of serum anti-Ascaris lumbricoides IgE antibodies and of Trichuris trichiura infection are risk factors for wheezing and/or atopy in preschool-aged Brazilian children. Respir Res. 2010;11:114. doi: 10.1186/1465-9921-11-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Hagel I, Cabrera M, Hurtado MA, Sanchez P, Puccio F, Di Prisco MC, Palenque M. Infection by Ascaris lumbricoides and bronchial hyper reactivity: an outstanding association in Venezuelan school children from endemic areas. Acta Trop. 2007;103:231–241. doi: 10.1016/j.actatropica.2007.06.010. [DOI] [PubMed] [Google Scholar]
- 145.Moncayo AL, Vaca M, Oviedo G, Erazo S, Quinzo I, Fiaccone RL, Chico ME, Barreto ML, Cooper PJ. Risk factors for atopic and non-atopic asthma in a rural area of Ecuador. Thorax. 2010;65:409–416. doi: 10.1136/thx.2009.126490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Cooper PJ, Chico ME, Guadalupe I, Sandoval CA, Mitre E, Platts-Mills TA, Barreto ML, Rodrigues LC, Strachan DP, Griffin GE. Impact of early life exposures to geohelminth infections on the development of vaccine immunity, allergic sensitization, and allergic inflammatory diseases in children living in tropical Ecuador: the ECUAVIDA birth cohort study. BMC Infect Dis. 2011;11:184. doi: 10.1186/1471-2334-11-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Maspero JF, Jardim JR, Aranda A, Tassinari C P, Gonzalez-Diaz SN, Sansores RH, Moreno-Cantu JJ, Fish JE. Insights, attitudes, and perceptions about asthma and its treatment: findings from a multinational survey of patients from Latin America. World Allergy Organ J. 2013;6:19. doi: 10.1186/1939-4551-6-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.The global asthma report 2011. Paris, France: The International Union Against Tuberculosis and Lung Disease. pp. 1–76 [accessed 2013 Aug]. Available from http://www.globalasthmareport.org/images/files/Global_Asthma_Report_2011.pdf
- 149.Soto-Martínez M, Avila L, Soto N, Chaves A, Celedón JC, Soto-Quiros ME. Trends in hospitalizations and mortality from asthma in Costa Rica over a 12- to 15-year period. J Allergy Clin Immunol Pract. 2014;2:85–90. doi: 10.1016/j.jaip.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 150.Claudio L, Stingone JA. Primary household language and asthma care among Latino children. J Health Care Poor Underserved. 2009;20:766–779. doi: 10.1353/hpu.0.0164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Van Wie A, Ziegenfuss J, Blewett LA, Davern M. Persistent disparities in health insurance coverage: Hispanic children, 1996 to 2005. J Health Care Poor Underserved. 2008;19:1181–1191. doi: 10.1353/hpu.0.0069. [DOI] [PubMed] [Google Scholar]
- 152.Medeiros JA, Sanchez GR, Valdez RB. Tough times, tough choices: the impact of the rising medical costs on the U.S. Latino electorate’s health care-seeking behaviors. J Health Care Poor Underserved. 2012;23:1383–1398. doi: 10.1353/hpu.2012.0183. [DOI] [PubMed] [Google Scholar]
- 153.Rosas-Salazar C, Ramratnam SK, Brehm JM, Han YY, Acosta-Pérez E, Alvarez M, Colón-Semidey A, Canino G, Apter AJ, Celedón JC. Parental numeracy and asthma exacerbations in Puerto Rican children. Chest. 2013;144:92–98. doi: 10.1378/chest.12-2693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Kit BK, Simon AE, Ogden CL, Akinbami LJ. Trends in preventive asthma medication use among children and adolescents, 1988-2008. Pediatrics. 2012;129:62–69. doi: 10.1542/peds.2011-1513. [DOI] [PubMed] [Google Scholar]
- 155.Crocker D, Brown C, Moolenaar R, Moorman J, Bailey C, Mannino D, Holguin F. Racial and ethnic disparities in asthma medication usage and health-care utilization: data from the National Asthma Survey. Chest. 2009;136:1063–1071. doi: 10.1378/chest.09-0013. [DOI] [PubMed] [Google Scholar]
- 156.McQuaid EL, Everhart RS, Seifer R, Kopel SJ, Mitchell DK, Klein RB, Esteban CA, Fritz GK, Canino G. Medication adherence among Latino and non-Latino white children with asthma. Pediatrics. 2012;129:e1404–e1410. doi: 10.1542/peds.2011-1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Wisnivesky JP, Kattan M, Evans D, Leventhal H, Musumeci-Szabó TJ, McGinn T, Halm EA. Assessing the relationship between language proficiency and asthma morbidity among inner-city asthmatics. Med Care. 2009;47:243–249. doi: 10.1097/MLR.0b013e3181847606. [DOI] [PubMed] [Google Scholar]
- 158.Wu AC, Smith L, Bokhour B, Hohman KH, Lieu TA. Racial/Ethnic variation in parent perceptions of asthma. Ambul Pediatr. 2008;8:89–97. doi: 10.1016/j.ambp.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Bialostozky A, Barkin SL. Understanding sibilancias (wheezing) among Mexican American parents. J Asthma. 2012;49:366–371. doi: 10.3109/02770903.2012.660298. [DOI] [PubMed] [Google Scholar]
- 160.Fritz GK, McQuaid EL, Kopel SJ, Seifer R, Klein RB, Mitchell DK, Esteban CA, Rodriguez-Santana J, Colon A, Alvarez M, et al. Ethnic differences in perception of lung function: a factor in pediatric asthma disparities? Am J Respir Crit Care Med. 2010;182:12–18. doi: 10.1164/rccm.200906-0836OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Choudhry S, Ung N, Avila PC, Ziv E, Nazario S, Casal J, Torres A, Gorman JD, Salari K, Rodriguez-Santana JR, et al. Pharmacogenetic differences in response to albuterol between Puerto Ricans and Mexicans with asthma. Am J Respir Crit Care Med. 2005;171:563–570. doi: 10.1164/rccm.200409-1286OC. [DOI] [PubMed] [Google Scholar]
- 162.Drake KA, Torgerson DG, Gignoux CR, Galanter JM, Roth LA, Huntsman S, Eng C, Oh SS, Yee SW, Lin L, et al. A genome-wide association study of bronchodilator response in Latinos implicates rare variants. J Allergy Clin Immunol. 2014;133:370–378. doi: 10.1016/j.jaci.2013.06.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Canino G, Vila D, Normand SL, Acosta-Pérez E, Ramírez R, García P, Rand C. Reducing asthma health disparities in poor Puerto Rican children: the effectiveness of a culturally tailored family intervention. J Allergy Clin Immunol. 2008;121:665–670. doi: 10.1016/j.jaci.2007.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Lara M, Ramos-Valencia G, González-Gavillán JA, López-Malpica F, Morales-Reyes B, Marín H, Rodríguez-Sánchez MH, Mitchell H. Reducing quality-of-care disparities in childhood asthma: La Red de Asma Infantil intervention in San Juan, Puerto Rico. Pediatrics. 2013;131:S26–S37. doi: 10.1542/peds.2012-1427d. [DOI] [PubMed] [Google Scholar]
- 165.Rosas-Salazar C, Ramratnam S, Brehm J, Han YY, Boutaoui N, Forno E, Acosta-Pérez E, Alvarez M, Colón-Semidey A, Canino G, Celedón JC. Prematurity, atopy and childhood asthma in puerto ricans. J Allergy Clin Immunol. 2014;133:357–362. doi: 10.1016/j.jaci.2013.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.US Department of Health and Human Services. Read the law: the Affordable Care Act, section by section. Washington, D.C: US Department of Health and Human Services; 2012[accessed 2014 Jan 14]. Available from: http://www.hhs.gov/healthcare/rights/law/index.htm
- 167.Pan American Health Organization Regional Mortality Database, 2010 [accessed 2013 Sept 12]. Available from: http://ais.paho.org/phip/viz/mort_chapters_en.asp