Abstract
Introduction
Retained sponges and instruments (RSI) due to surgery are a recognised medical ‘never event’ and have catastrophic implications for patients, healthcare professionals and medical care providers. The aim of this review was to elucidate the extent of the problem of RSI and to identify preventative strategies.
Methods
A comprehensive literature search was performed on MEDLINE®, Embase™, the Science Citation Index and Google™ Scholar for articles published in English between January 2000 and June 2012. Studies outlining the incidence, risk, management and attempts to prevent RSI following surgical intervention were retrieved.
Results
The overall incidence of RSI is low although its incidence is substantially higher in operations performed on open cavities. Sponges are the most commonly retained item when compared with needles and instruments. Clinical presentation is varied, leading to avoidable morbidity, and the error is indefensible medicolegally. Risk factors include emergency operations, operations involving unexpected change in procedure, raised body mass index, and a failure to perform accurate sponge and instrument counts. The existing strategy for prevention is manual counting of sponges and instruments undertaken by surgical personnel. This, however, is fallible. Computer assisted counting of sponges using barcodes and gauze sponges tagged with a radiofrequency identification device aiding manual counting have been trialled recently, with success.
Conclusions
Vigilance among operating theatre personnel is paramount if RSI is to be prevented. Prospective multicentre trials to assess efficacy of new technologies aiding manual counting should be undertaken if this medical error is to be eliminated completely.
Keywords: Retained, Sponges, Foreign bodies, Instruments, Counts, Prevention, Surgery
The retention of foreign bodies (sponges, needles and instruments) in a patient after a surgical procedure is a medical error that often results in adverse consequences for patients and can seriously implicate the healthcare personnel involved. This error is included in the list of 27 ‘never events’ released by the National Quality Forum in the US 1 and also in the guidance issued by the UK Department of Health. 2
Surgery to the wrong patient, the wrong side, the wrong site and retention of foreign bodies after a surgical procedure are entirely preventable causes of morbidity and, perhaps, mortality. 3 Medical negligence in the case of retained sponges and instruments (RSI) is proven easily as a result of the doctrine of res ipsa loquitur (‘the thing itself speaks’). The fact that an object was left in a space where it does not belong becomes indefensible. Medicolegal and compensation costs associated with RSI are high, even if there has been little or no harm to the patient. Costs vary from $37,041 to $2,350,000 (approximately £23,000 to £1,460,000) per incident, with an average cost per case estimated at $95,000 (≈£59,000). 4–6 This review was undertaken to enumerate the extent of the problem of RSI after surgical procedures with the aim of identifying strategies for reducing, if not eradicating, it.
Methods
A comprehensive literature search was performed on MEDLINE®, Embase™, the Science Citation Index and Google™ Scholar for articles published in English between January 2000 and June 2012. Key search words (including retained swabs, sponges, surgical instruments, needles, prevention, risks and surgical counts) were used in combination with the Boolean operators AND, OR and NOT. The search was supplemented using the ‘related article’ function. Bibliographies of selected articles were further searched manually for studies that were missed in the initial electronic search. Older publications were included if relevant.
Incidence
The incidence of RSI varied from 1 in every 1,000 to 1,500 intra-abdominal operations in studies performed in the early 1980s 7,8 while more contemporary studies suggest an incidence of 1 in 5,500 to 1 in 18,760 inpatient operations. 3,9,10 A total of 496 patient safety incidents involving retained sponges and instruments occurring between 1 April 2007 and 31 March 2008 were reported to the UK National Reporting and Learning System. 11
The reasons for the varied incidence of RSI include: the retrospective nature of studies, a reluctance on the part of hospitals and clinicians to disclose these errors publically due to their sensitive nature, incidental discovery of the RSI after many years as patients may remain asymptomatic, and confidentiality requirements of insurance and legal claims hampering publication of data on RSI. 3,12
A surgical sponge is the most commonly reported retained item following surgery while reports of retained needles and instruments are extremely rare. 3,9,12,13 No surgical specialty and no surgical procedure are immune to the problem. Wan et al reviewed 254 cases published between 1963 and 2008, and found the abdominal/pelvic cavity/vaginal vault (74%) to be the most common site for RSI, followed by the thoracic cavity (11%). 14 These findings are similar to those of other studies, 3,9,12,15 thereby implicating the surgical personnel involved in these operations as the prime offenders.
Predisposing risk factors
The risk factors leading to RSI after surgery have been elucidated by two observational studies. 3,12 Gawande et al performed a retrospective case-control analysis of all malpractice claims and incident reports involving RSI filed between 1 January 1985 and 1 January 2001 across 22 hospitals in the US. 3 A total of 60 cases involving 61 RSI events were identified, with 4 hospitals accounting for 83% of cases. For each case of RSI, four patients who had undergone the same procedure as the given patient during the same period were selected as controls. Lincourt et al replicated the above study by performing a case-control analysis involving retrospective review of medical records from a single institution over a ten-year period (January 1996 – December 2005). 12 They cross-referenced the International Classification of Diseases code for unintentionally retained foreign body during surgery with their billing and reimbursement database, and found 30 cases of RSI.
The risk factors for RSI identified in the two studies 3,12 are summarised in Table 1. The results obtained from these two studies are discordant mainly because of the low incidence of retained foreign objects along with the methodology used.
Table 1.
Risk factors for retained foreign objects identified across two retrospective case-control studies
| Study | Risk factors for retained swabs and instruments | p-value | Risk ratio (95% confidence interval) |
|---|---|---|---|
| Gawande 3 | Operations performed on emergency basis | <0.001 | 8.8 (2.4–31.9) |
| Body mass index (per 1 unit increment) | 0.01 | 1.1 (1.0–1.2) | |
| Unexpected change in operation | 0.01 | 4.1 (1.4–12.4) | |
| Multiple surgical teams | 0.1 | 3.4 (0.8–14.1) | |
| Female sex | 0.13 | 0.4 (0.1–1.3) | |
| Estimated blood loss (per 100ml increment) | 0.19 | 1.0 (1.0–1.0) | |
| Change in nursing staff during procedure | 0.24 | 1.9 (0.7–5.4) | |
| Counts of sponges and instruments | 0.76 | 0.6 (0.0–13.9) | |
| Lincourt 12 | Number of major procedures performed | 0.008 | 1.6 (1.1–2.3) |
| Incorrect counts recorded | 0.02 | 16.2 (1.3–197.8) | |
| Multiple surgical teams | >0.05 | 5.4 (0.9–33.1) | |
| Unexpected change in operation | >0.05 | Not mentioned | |
| Operation theatre time | >0.05 | Not mentioned | |
| Procedures performed after 5pm | >0.05 | Not mentioned | |
| Emergency procedures | >0.05 | Not mentioned |
Clinical presentation and management
The clinical presentation of RSI is varied, and depends on the site and type of tissue reaction elicited, as shown in Table 2. 3,8,16,17 Retained surgical sponges may elicit either an exudative or an aseptic fibrous type of tissue reaction. 18 The exudative kind of reaction presents fairly early in the postoperative period, causing infections secondary to bacterial contamination. The aseptic fibrous type of reaction is slow in comparison; it involves fibroblasts leading to formation of adhesions, granulomas or pseudotumours, with patients remaining asymptomatic for many years. 19 Imaging is the key to diagnosis. Computed tomography is the modality of choice to exclude RSI (Fig 1). Plain radiography is also used commonly although it has a false negative rate of 10–25% despite the presence of radiopaque markers on surgical sponges. 20 Magnetic resonance imaging and other relevant radiological techniques such as barium contrast studies may also be used depending on the clinical situation. 17
Table 2.
Clinical presentation of retained sponges and instruments
| ASYMPTOMATIC |
| Detection is incidental |
| SYMPTOMATIC |
| Early |
| Unexplained pain, features of generalised sepsis, formation of abscess |
| Delayed |
| Non-healing wounds, discharging sinuses, mass, signs and symptoms of intestinal obstruction, internal fistulisation, transmural migration and spontaneous expulsion |
Figure 1.
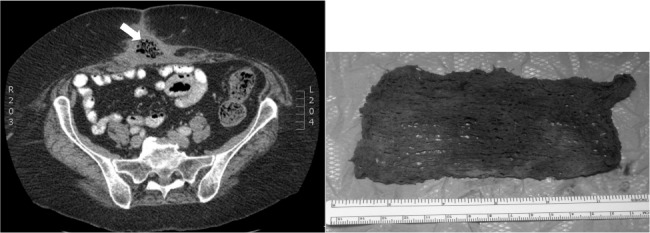
An obese patient developed a wound infection at the site of an incisional hernia repair performed 10 weeks previously. This was treated in the community with negative pressure wound therapy (NPWT). Foul-smelling discharging pus persisted from a wound sinus after cessation of NPWT. Computed tomography (left) showed an area of inflammation with multiple air pockets (arrow) in the subcutaneous tissue of the anterior abdominal wall. Wound exploration under general anaesthesia revealed a sponge (without a radiopaque marker) used for the NPWT dressings in the subcutaneous fat (right). The sponge was removed, the wound healed by secondary intention and the patient made an uneventful recovery.
Retained objects can cause multiple problems (Table 3), and treatment involves surgical removal of the items once diagnosed, even if the patient is asymptomatic. The time interval between initial surgery, diagnosis and removal of RSI is clinically relevant as the morbidity and mortality is much less if the RSI is removed immediately after the offending operation than with delayed diagnosis and retrieval. 19 Needles are less likely to cause serious clinical consequences and are no different from retained metal shrapnel. The evidence for benefits of removal of these items is unclear and needs to be evaluated on a case-by-case basis, weighing up the risks and benefits of performing another operation. 21 In any case, a frank discussion must be had with the patient and appropriate measures must be taken for reporting the incident according to local policy.
Table 3.
Outcomes of patients with reported retained sponges and instruments (n=90) across two retrospective case-control studies 3,12
| Outcomes | Number of cases |
|---|---|
| Death | 1 |
| Readmission to hospital | 40 |
| Reoperation | 62 |
| Intra-abdominal abscess or sepsis | 26 |
| Small bowel obstruction / intestinal fistulation | 10 |
| Visceral perforation | 5 |
Value of counting
Counting of items before and after use, at the time of surgery, is the most widely used method for the screening of RSI, with established protocols in place. 22,23 Egorova et al retrospectively analysed count discrepancy data stored in a web-based ‘near miss’ and patient harm reporting system over a four-year period (2000–2004). 10 Of the 153,263 operations checked, they estimated count discrepancies to occur in 1 in 145 operations (0.69%). The test characteristics of surgical counting as a screening method were determined (sensitivity 77.27%, specificity 99.32%, positive predictive value (PPV) 1.6%, negative predictive value 100%). The low PPV was a result of the low frequency of RSI events (17 true positives, 5 false negatives). The odds of a foreign body being left behind in a patient increased by >100 times when the count was discrepant (positive likelihood ratio 113.3).
Greenberg et al designed a prospective observational field study to estimate the rate of intraoperative count discrepancies. 24 They sought to determine how these discrepancies translate into meaningful problems (misplaced items or RSI), and to examine the relationship between personnel changes and count discrepancies. They observed a total of 2,476 distinct counting episodes during 148 cases (16.6 counting episodes per case) with 8.6 minutes taken for each count to be performed. They found 29 count discrepancies occurring in 19 cases. The majority of discrepancies again involved sponges (45%), followed by instruments (31%) and needles (21%). Of these 29 discrepancies, 59% were due to misplaced items, representing potential RSI, while 41% were due to human error in arithmetic. The analysed causes of count discrepancies across the above two studies are summarised in Table 4, showing that mere counting of sponges and surgical instruments undertaken by allied surgical staff in theatre is prone to error. 10,24
Table 4.
Significant predictors of surgical count discrepancy when count performed in the operating theatre at the time of surgery
| Study | Predictors of count discrepancy |
|---|---|
| Egorova 10 |
|
| Greenberg 24 |
|
Need for preventive strategies
Counting as a screening strategy for RSI is not foolproof. Most studies advocate standardisation, development of local counting protocols, and adherence to counting sponges and instruments preoperatively as well as multiple times intraoperatively. 3,9,12 These protocols are labour intensive and can occupy up to 14% of operative time. 25 This should be followed by detailed inspection by the surgeon of the body cavity, ruling out RSI, prior to closure of the body cavity. Count discrepancies should automatically universally trigger a prompt and thorough search for the item, and if the discrepancy persists, appropriate imaging (radiography/computed tomography) should be performed to look for retained objects.
In 2003 Minnesota became the first state in the US to promulgate legislation requiring ‘never events’ to be disclosed to the public. 26 Cima et al from the Mayo Clinic in Rochester, Minnesota, a high volume tertiary referral facility, audited their experience of RSI retrospectively from 2003 to 2006. 9 They instituted postoperative high-resolution x-ray screening of patients undergoing operations involving body cavities as a routine preventive strategy in a dedicated suite to rule out retained objects before entering the recovery room. A total of 191,168 operations were performed and 68 RSI related events reported; 34 of these were classified as near-miss events, mostly due to incorrect surgical counts, where postoperative x-ray ruled out RSI.
The other 34 cases in the study by Cima et al were true RSI, of which 20 (59%) were found due to routine postoperative high resolution surveillance x-rays. 9 In all of these 20 cases, the surgical counts performed were reported correct at the time of completion of the case. In the 14 remaining cases where counts were incorrect, intraoperative x-rays were done in 4 cases that confirmed RSI. In six cases, x-rays were not performed (in two cases the RSI was coughed up spontaneously, in two cases sponges were retained in the vaginal vault, in one case the retained sponge was retrieved before x-rays were performed and in the final case it was decided against looking for the RSI given the poor clinical condition of the patient). In four cases, RSI were missed despite routine postoperative x-ray screening.
In Mayo Clinic study, therefore, the RSI was discovered within 24 hours of the offending operation in 20 of 34 cases (59%). 9 This was primarily due to routine postoperative x-ray surveillance. Immediate retrieval was possible in 27 cases (21 needed an additional surgical procedure and in 6 cases the RSI was removed without an operation). In the remaining seven cases, it was decided not to attempt removal in six cases while in one case the attempted operative removal failed.
Cima et al’s analysis found no significant association of RSI with risks factors previously identified by Gawande et al 3 and Lincourt et al 12 but confirmed sponges to be most frequently counted during operations as well as the most frequently missed item. 9 They believed that the complex environment of the operating room, multiple distractions, competing tasks and poor communication among the members of the surgical team hampered the sponge and instrument counting process, leading to RSI.
Concerned as an organisation and aiming to reduce RSI incidents to zero, the Mayo Clinic instituted a multidisciplinary, multiphase managerial approach in 2005. 27 They implemented key initiatives (performing defect analysis and policy review), initiated awareness, enhanced communication, and formed a rapid response events leadership team to monitor and control any RSI event. The effect of these initiatives was audited, revealing RSI events to occur once every 69 days compared with once every 16 days previously. They believed that the adoption of preventative strategies such as postoperative x-ray surveillance along with management driven initiatives to change clinical practice were key patient safety processes leading to the reduction of RSI.
Despite the steps taken, as an institution, they were still far away from achieveing their goal of reducing RSI rates to zero. There was a realisation that human efforts of counting sponges needed to be complemented. There was an urgent need to incorporate and evaluate new technologies that could be used to assist existing methods to reduce rates of retained objects.
Advances in sponge counting
A prospective, blinded, experimental clinical trial was conducted for the first time at Stanford University using gauze sponges tagged with a radiofrequency identification (RFID) microchip and a handheld scanning device. 28 A total of 8 patients were enrolled and 28 RFID tagged sponges were placed in them. The handheld device detected all sponges correctly with no false positive or negative results. These results were extremely encouraging. However, some concerns were raised regarding human errors in performing an incorrect scan, the timing of the scan possibly also impacting on the final result and the lack of cost–benefit analyses limiting the full implementation of such technology.
In a separate study, traditional counting protocols were compared with computer assisted counting of sponges using barcodes in a randomised control trial involving 298 patients. 29 The barcode system detected significantly more counting discrepancies than the traditional system, which included misplaced and miscounted sponges. This study highlighted the increased frequency with which count discrepancies go unnoticed when traditional counting methods are applied.
In an effort to completely eliminate RSI, the Mayo Clinic evaluated a data matrix coded sponge (DMS) counting system in addition to standard manual counting protocols. 30 Similar to the barcode system, it included individual unique data matrix coded sponges along with a data matrix scanner, which kept a running count of every sponge introduced and removed from the sterile field. Two internal trials were conducted to assess suitability and, on satisfactory performance in the trials, this technology was fully implemented. Safety performance (incidence of retained sponge products and staff satisfaction) was measured, incorporating DMS to the previously existing RSI risk reduction strategy.
Implementation across the institution was made possible after a two-month period of staff education and training. In the 18-month period following the implementation of the new RSI risk reduction strategy, not a single sponge was reported retained, with a negligible increase in overall operating times, a short learning curve and good acceptance among staff members. This was a considerable feat for an organisation that was averaging a retained sponge every 16 days prior to 2003. 27 Thus, through focused, concerted and coordinated efforts, the Mayo Clinic, Rochester, as an institution, implemented multiple preventive strategies and audited its results serially to show a dramatic improvement and reduction of RSI rates.
Each preventive intervention strategy (surgical counting, postoperative x-ray screening) along with new mentioned technologies has their advantages and disadvantages (Table 5). The operating theatre environment is complex, dynamic and at times stressful, and, consequently, human errors are easily missed. The evidence to support the routine use of the new technologies assisting in manual counting of sponges is currently scant. All major surgical institutions must therefore endeavour to analyse their individual operating theatre practices and put in place standard operating protocols to prevent RSI. An algorithm based on the available evidence for the prevention of RSI is shown in Figure 2.
Table 5.
Advantages and disadvantages of strategies to prevent retained sponges and instruments
| Preventive strategy | Advantages | Disadvantages |
|---|---|---|
| Counting of sponges and instruments 10 |
|
|
| Intraoperative x-ray screening 10 |
|
|
| Routine postoperative high-resolution x-ray surveillance 9 |
|
|
| Sponges tagged with radiofrequency identification chip 28 |
|
|
| Barcoded or data matrix coded sponges as adjunct to existing counting protocols 29,30 |
|
|
RCT = randomised controlled trial
Figure 2.
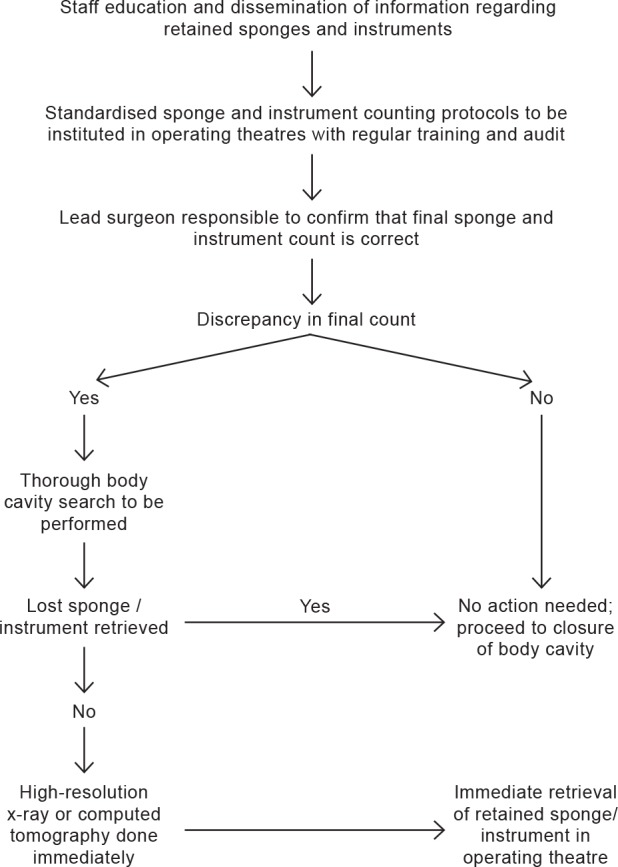
Suggested algorithm to prevent retained sponges and instruments
Conclusions
RSI is an undesirable and preventable cause of surgical morbidity and mortality. As responsible healthcare professionals, we must remain vigilant at all times to the threat posed by RSI. Adoption of new technologies and working alongside industry must be encouraged to assist existing methods of counting processes and protocols. Furthermore, prospective multicentre studies to assess the efficacy of new technologies need to be undertaken urgently. We must learn to work together and take the lead to help build systems that will eliminate RSI completely.
References
- 1.National Quality Forum. Serious Reportable Events In Healthcare – 2011 Update. Washington DC: NQF: 2011 [Google Scholar]
- 2.Department of Health. The ‘Never Events’ List 2011/12. London: DH; 2011 [Google Scholar]
- 3.Gawande AA, Studdert DM, Orav EJet al Risk factors for retained instruments and sponges after surgery. N Engl J Med 2003; 348: 229–235 [DOI] [PubMed] [Google Scholar]
- 4.Berkowitz S, Marshall H, Charles A. Retained intra-abdominal surgical instruments: time to use nascent technology? Am Surg 2007; 73: 1,083–1,085 [PubMed] [Google Scholar]
- 5.Dippolito A, Braslow BM, Lombardo Get al How David beat Goliath: history of physicians fighting frivolous lawsuits. OPUS 12 Scientist 2008; 2: 1–8 [Google Scholar]
- 6.Weeks WB, Foster T, Wallace AE, Stalhandske E. Tort claims analysis in the Veterans Health Administration for quality improvement. J Law Med Ethics 2001; 29: 335–345 [DOI] [PubMed] [Google Scholar]
- 7.Jason RS, Chisolm A, Lubetsky HW. Retained surgical sponge simulating a pancreatic mass. J Natl Med Assoc 1979; 71: 501–503 [PMC free article] [PubMed] [Google Scholar]
- 8.Hyslop JM, Maull KI. Natural history of the retained surgical sponge. South Med J 1982; 75: 657–660 [DOI] [PubMed] [Google Scholar]
- 9.Cima RR, Kollengode A, Garnatz Jet al Incidence and characteristics of potential and actual retained foreign object events in surgical patients. J Am Coll Surg 2008; 207: 80–87 [DOI] [PubMed] [Google Scholar]
- 10.Egorova NN, Moskowitz A, Gelijns Aet al Managing the prevention of retained surgical instruments: what is the value of counting? Ann Surg 2008; 247: 13–18 [DOI] [PubMed] [Google Scholar]
- 11.National Patient Safety Agency. Surgical Safety Can Be Improved through Better Understanding of Incidents Reported to a National Database. London: NPSA; 2009 [Google Scholar]
- 12.Lincourt AE, Harrell A, Cristiano Jet al Retained foreign bodies after surgery. J Surg Res 2007; 138: 170–174 [DOI] [PubMed] [Google Scholar]
- 13.Gibbs VC, Coakley FD, Reines HD. Preventable errors in the operating room: retained foreign bodies after surgery – Part I. Curr Probl Surg 2007; 44: 281–337 [DOI] [PubMed] [Google Scholar]
- 14.Wan W, Le T, Riskin L, Macario A. Improving safety in the operating room: a systematic literature review of retained surgical sponges. Curr Opin Anaesthesiol 2009; 22: 207–14 [DOI] [PubMed] [Google Scholar]
- 15.Stawicki SP, Evans DC, Cipolla Jet al Retained surgical foreign bodies: a comprehensive review of risks and preventive strategies. Scand J Surg 2009; 98: 8–17 [DOI] [PubMed] [Google Scholar]
- 16.Zantvoord Y, van der Weiden RM, van Hooff MH. Transmural migration of retained surgical sponges: a systematic review. Obstet Gynecol Surv 2008; 63: 465–471 [DOI] [PubMed] [Google Scholar]
- 17.Sakorafas GH, Sampanis D, Lappas Cet al Retained surgical sponges: what the practicing clinician should know. Langenbecks Arch Surg 2010; 395: 1,001–1,007 [DOI] [PubMed] [Google Scholar]
- 18.Sturdy JH, Baird RM, Gerein AN. Surgical sponges: a cause of granuloma and adhesion formation. Ann Surg 1967; 165: 128–134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lauwers PR, Van Hee RH. Intraperitoneal gossypibomas: the need to count sponges. World J Surg 2000; 24: 521–527 [DOI] [PubMed] [Google Scholar]
- 20.Choi BI, Kim SH, Yu ESet al Retained surgical sponge: diagnosis with CT and sonography. Am J Roentgenol 1988; 150: 1,047–1,050 [DOI] [PubMed] [Google Scholar]
- 21.Greenberg CC, Gawande AA. Retained foreign bodies. Adv Surg 2008; 42: 183–191 [DOI] [PubMed] [Google Scholar]
- 22.Association of periOperative Registered Nurses. Perioperative Standards and Recommended Practices. Denver: AORN; 2008 [Google Scholar]
- 23.Association for Perioperative Practice. Standards and Recommendations for Safe Perioperative Practice. Harrogate: AfPP; 2007 [Google Scholar]
- 24.Greenberg CC, Regenbogen SE, Lipsitz SRet al The frequency and significance of discrepancies in the surgical count. Ann Surg 2008; 248: 337–341 [DOI] [PubMed] [Google Scholar]
- 25.Christian CK, Gustafson ML, Roth EMet al A prospective study of patient safety in the operating room. Surgery 2006; 139: 159–173 [DOI] [PubMed] [Google Scholar]
- 26.Adverse Events Reporting System. Minnesota Department of Health. http://www.health.state.mn.us/patientsafety/ae/ (cited December2012).
- 27.Cima RR, Kollengode A, Storsveen ASet al A multidisciplinary team approach to retained foreign objects. Jt Comm J Qual Patient Saf 2009; 35: 123–132 [DOI] [PubMed] [Google Scholar]
- 28.Macario A, Morris D, Morris S. Initial clinical evaluation of a handheld device for detecting retained surgical gauze sponges using radiofrequency identification technology. Arch Surg 2006; 141: 659–662 [DOI] [PubMed] [Google Scholar]
- 29.Greenberg CC, Diaz-Flores R, Lipsitz SRet al Bar-coding surgical sponges to improve safety: a randomized controlled trial. Ann Surg 2008; 247: 612–616 [DOI] [PubMed] [Google Scholar]
- 30.Cima RR, Kollengode A, Clark Jet al Using a data-matrix-coded sponge counting system across a surgical practice: impact after 18 months. Jt Comm J Qual Patient Saf 2011; 37: 51–58 [DOI] [PubMed] [Google Scholar]


