Abstract
Objectives:
Employee control over work times has been associated with favorable psychosocial and health-related outcomes, but the evidence regarding sleep quality remains inconclusive. We examined cross-sectional and prospective associations between work time control and sleep disturbances in a large working population, taking into account total hours worked.
Methods:
The data were from a full-panel longitudinal cohort study of Finnish public sector employees who responded to questions on work time control and sleep disturbances in years 2000-2001, 2004-2005, 2008-2009, and 2012. The analysis of cross-sectional associations was based on 129,286 person measurements from 68,089 participants (77% women) aged 17-73 years (mean 43.1). Data from 16,503 participants were used in the longitudinal analysis. Log-binomial regression analysis with the generalized estimating equations method was used.
Results:
Consistently in both cross-sectional and longitudinal models, less control over work time was associated with greater sleep disturbances in the total population and among those working normal 40-hour weeks. Among participants working more than 40 hours a week, work time that was both very high (cross-sectional prevalence ratio compared to intermediate work time control [PR] 1.32, 95% confidence interval [CI] 1.05-1.65) and very low (PR 1.23, 95% CI 1.08-1.39) was associated with sleep disturbances, after adjustment for potential confounding factors.
Conclusions:
These data suggest that having few opportunities to influence the duration and positioning of work time may increase the risk of sleep disturbances among employees. For persons working long hours, very high levels of control over working times were also associated with increased risk of sleep disturbances.
Citation:
Salo P, Ala-Mursula L, Rod NH, Tucker P, Pentti J, Kivimäki M, Vahtera J. Work time control and sleep disturbances: prospective cohort study of Finnish public sector employees. SLEEP 2014;37(7):1217-1225.
Keywords: epidemiology, cohort studies, work schedule tolerance, sleep initiation, maintenance disorders
INTRODUCTION
Allowing employees the opportunity to influence the duration and positioning of their work time, that is work time control, has been associated with increased job satisfaction and reduced risk of work-family conflict, self-reported health problems, registered sickness absence, and disability pension, particularly in relation to musculoskeletal or mental disorders.1–7 Conversely, low work time control has been linked to sleep disturbances,1,8–12 and to common work-related stressors, such as job strain (i.e., a combination of high job demands and low job control at work), long working hours, and overcommitment to work.13–15 The importance of reducing sleep disturbances is underlined by observed associations between sleep disturbance and increased morbidity, especially in relation to mental disorders, temporary and permanent work disability, and even increased risk of premature death.16–23
Given that work time control represents a means of reducing stress at work, a link between low work time control and increased risk of sleep disturbances is plausible. However, to date, studies that have examined the association between work time control and sleep disturbances are limited and provide inconsistent results.1,8–12 In two cross-sectional studies, low work time control was associated with poorer sleep quality.1,8 Other studies have found that employees who lack individual flexibility to determine their days off and who also have highly variable work times determined by the employer are more likely to report sleep problems.1,8,9 However, in another study it was additionally found that employees with high work time control also experienced greater sleep problems when their work schedules were more variable.12 In shift workers, ability to influence scheduling of work shifts was not clearly associated with disturbed sleep.10,11
The reasons for the inconsistencies in previous results are unknown but may be due in part to small sample sizes, varying definitions of work time control, heterogeneity in the study designs, and differences in the sources of data (e.g., company records vs. open internet surveys). Furthermore, few studies have taken into account the possibility that the association between work time control and risk of sleep disturbances may depend on total hours worked. Long weekly work hours predict shorter and more disturbed sleep,15 probably because the time for unwinding after the end of work is reduced and the actual time available to sleep is restricted.24 Such restrictions may limit the possibilities for enhancing sleep through other means, such as improved work time control. Hence those who work long hours may be more likely to experience curtailed or impaired sleep, irrespective of their level of work time control. Finally, it is possible that in some cases, flexibility may promote behavior that results in greater sleep disturbance. For example, individual flexibility in working hours can be associated with setting oneself high goals, leading to self-inflicted unhealthy work schedules and excessive work load.1
In this prospective observational cohort study of public sector employees, our objective was to examine the relation between work time control and sleep disturbances using both cross-sectional and longitudinal designs in a large well-described working population. Given that high job control, including work time control, may decrease the likelihood of work-related stress,25 it is hypothesized that providing workers with control over their work hours will also reduce the risk of sleep disturbances. Furthermore, we examined the role of long working hours in the association between work time control and sleep, as the health implications of work time control might differ between employees working standard hours and those working extended hours. We hypothesized that the association between work time control and sleep disturbances might be weaker among those working long hours because of the impact that long work hours have on unwinding and the time available for sleeping. With up to 68,089 employees and 129,286 person measurements, this study is to our knowledge, the largest study so far in this field of research.
MATERIAL AND METHODS
Study Population and Design
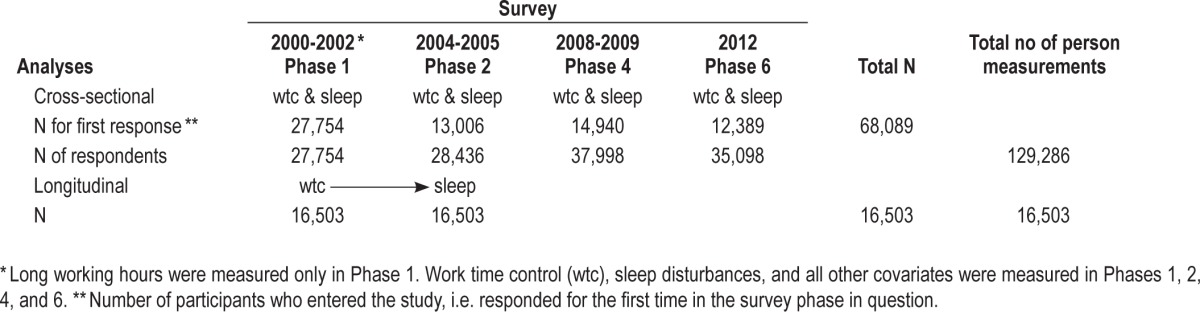
This study is based on data from the Finnish Public Sector study.5,7 In Phase 1 in 2000-2001, a total of 32,299 (response rate 67%) local government employees in 10 towns in Finland aged 17-65 responded to a survey regarding health and well-being. Surveys have since been repeated in 2004-2005 (Phase 2, N = 37,953, response rate 65%), 2006 (Phase 3, N = 34,418, 69%, no sleep measurement), 2008-2009 (Phase 4, N = 48,495, 69%), 2010 (Phase 5, N = 37,567, 69%), and 2012 (Phase 6, N = 39,194, 69%), targeting all full-time employees of those organizations. In Phases 2 and 4 we additionally included those participants who, after joining the cohort, had transferred to other organizations, or had become entrepreneurs. In all analyses, we included only participants who were working full time and had complete data within one measurement point. The final sample for the cross-sectional analysis comprised 68,089 participants, of whom 27,754 (41%) joined the study population at Phase 1, 13,006 (19%) at Phase 2, 14,940 (22%) at Phase 4, and 12,389 (18%) at Phase 6 (Table 1). Participants (77% women) were aged 17-73 years (mean 43.1, SD 10.0) at the time of their first survey response with complete data. The longitudinal analysis covered the 16,503 participants who had responded to questions about work time control, working hours (measured only in Phase 1), and covariates in Phase 1, and sleep disturbances in Phase 2.
Table 1.
Study design and number of participants and person measurements for the cross-sectional and longitudinal analyses
The study was approved by the Ethics committee of the Finnish Institute of Occupational Health.
Work Time Control
Work time control was measured with 7 items relating to the respondent's ability to influence the following: (1) total length and (2) beginning and ending times of a working day, (3) taking breaks during a working day, (4) attending to personal affairs during a working day, (5) scheduling of work shifts, (6) taking vacations and paid days off, and (7) taking unpaid leave.5 Internal consistency (Cronbach α) between the items was 0.84 at the time of the first survey response. All items were assessed on a Likert-type response scale ranging from 1 (very little) to 5 (very much) and the mean of the items was calculated (response to ≥ 4 items was required). The mean was rounded to the nearest whole number to indicate work time control score: 1 = very low, 2 = low, 3 = intermediate, 4 = high, and 5 = very high work time control.
Working Hours
Working hours, measured at Phase 1 only, were derived from the self-reports of the number of contracted working hours as well as the estimated weekly mean of extra and overtime working hours. These numbers were summed and dichotomized into ≤ 40 h/week or > 40 h/week.
Sleep Disturbances
Self-reported sleep disturbances were measured with the Jenkins Sleep Problem Scale26 at Phases 1, 2, 4, 5, and 6. Individual items addressed the occurrence of the following sleep problems: difficulty falling asleep, difficulty maintaining sleep during the night, early morning awakenings, and non-restorative sleep—items corresponding to the nighttime insomnia symptoms specified by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV). Participants reported how frequently they had experienced each of the 4 symptoms during the past 4 weeks (response scale from 1 = never to 6 = every night). For participants who reported more than one insomnia symptom, their most frequent symptom was used to assess the frequency of sleep disturbances, dichotomized as no sleep disturbances (symptoms 0-4 nights/week) or sleep disturbances (symptoms 5-7 nights/week).
Covariates
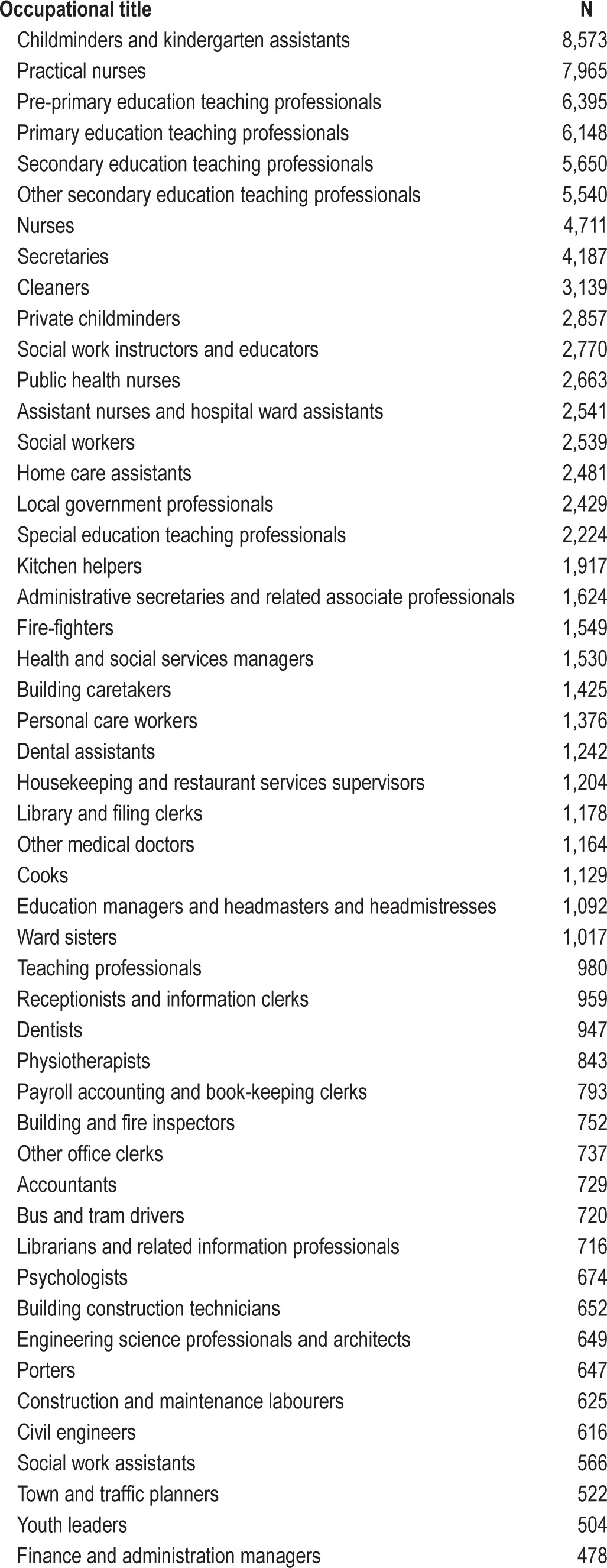
Sociodemographic characteristics of age, sex, occupational status, and type of job contract (permanent/temporary) were drawn from employers' records. Occupational status was divided into higher-grade non-manual workers (e.g., teachers, physicians), lower-grade non-manual workers (e.g., registered nurses, technicians), and manual workers (e.g., cleaners, maintenance workers) according to the occupational title classification of Statistics Finland.27 Appendix 1 shows the 50 most common occupational titles in the Finnish Public Sector data. Data on marital status (married or cohabited/single) and work schedule (day work/night or shift work) were obtained from the survey responses.
Health behaviors comprised self-reports of current smoking (no/yes), alcohol consumption (grams of pure alcohol per week),28 body mass index (BMI), and physical activity. Participants reported their average weekly consumption of beer, wine, and spirits in portions. Those data were transformed into grams of pure alcohol. BMI was calculated from self-reported height and weight (kg/m2). Participants also reported the amount of their physical activity and whether it was equal to walking, fast walking, jogging, or running. Physical activity was measured as metabolic equivalent task (MET) hours per day.29
Self-rated health was measured on a 5-point scale using the item: “How would you estimate your current state of health?”30 The scale was dichotomized to indicate suboptimal (scores 1-3) and good (scores 4-5) self-rated health. Psychological distress was measured by the 12-item version of the General Health Questionnaire (GHQ),31 with caseness coded as positive if the participant endorsed ≥ 4 items of psychological problems during preceding weeks. Symptoms of anxiety (continuous outcome) were quantified by the 6-item Trait Anxiety Inventory.32
Statistical Analysis
Associations between the covariates and work time control were analyzed using the χ2 test (categorical variables) or analysis of variance (continuous variables). In these analyses, we included the first measurement of each participant if they had responded more than once.
We pooled data from all 4 points of measurement that included questions on work time control, sleep disturbances, and all the covariates, i.e., Phases 1, 2, 4, and 6. Phases 3 and 5 included data on work time control and sleep disturbances, but not all the covariates. The cross-sectional analysis thus comprised 129,286 person measurements from 68,089 participants. The cross-sectional association between work time control and sleep disturbances was analyzed with repeated measures log-binomial regression analysis using the generalized estimating equations (GEE) method.33,34 The repeated measurements were nested within participants, i.e., while the individual participants contributed more than one observation to the dataset, the interdependence of the within-participant observations was taken into account in estimating the standard errors.
In the crude model, we calculated prevalence ratios (PR) and their 95% confidence intervals (CI) of sleep disturbances by the degree of work time control, adjusted for the survey year. We then sequentially adjusted for (1) age, sex, and socioeconomic position, and (2) all the above listed + marital status, type of job contract, night/shift work, health behaviors, self-rated health, psychological distress, and anxiety. As the associations of alcohol consumption35 and BMI36 with health may be U-shaped, these covariates were included in the fully adjusted model both as linear and squared terms. Intermediate work time control was chosen for the reference category instead of very low or very high work time control, because those extreme scores comprised significantly fewer observations (very low work time control n = 11,004, very high n = 3,795) than the intermediate score (n = 46,496). For comparison, we also analyzed the association of work time control with self-reported suboptimal health, as lower work time control has previously been shown to predict poorer self-rated health.37
In the cross-sectional design, we analyzed the interaction between work time control and long working hours using data only from Phase 1, because long working hours were not measured in any other phases. This subsample included only those 26,796 participants who responded to the Phase 1 survey and had complete data on all variables. With similar adjustments to the original cross-sectional analysis, the association between work time control and sleep disturbances in Phase 1 was analyzed in subgroups according to working hours (≤ 40 h/ week and > 40 h/week).
The interaction between work time control and long working hours was further investigated in a longitudinal analysis using a log-binomial regression analysis with the generalized estimating equations (GEE) method. We evaluated prospectively whether the association between work time control in Phase 1 and sleep disturbances in Phase 2 depended on working hours (hours/week ≤ 40 or > 40) by including the term “work time control × working hours” in the model. Because of a significant interaction, we carried out analyses separately for those who reported working ≤ 40 h/week or > 40 h/week at Phase 1. The longitudinal analysis included complete data from 16,503 participants who had responded to questions about working hours, measured only in Phase 1. All the covariates, including time 1 sleep disturbances, were derived from Phase 1.
All analyses were performed using the SAS statistical software, version 9.2 (SAS Institute, Inc., Cary, NC).
RESULTS
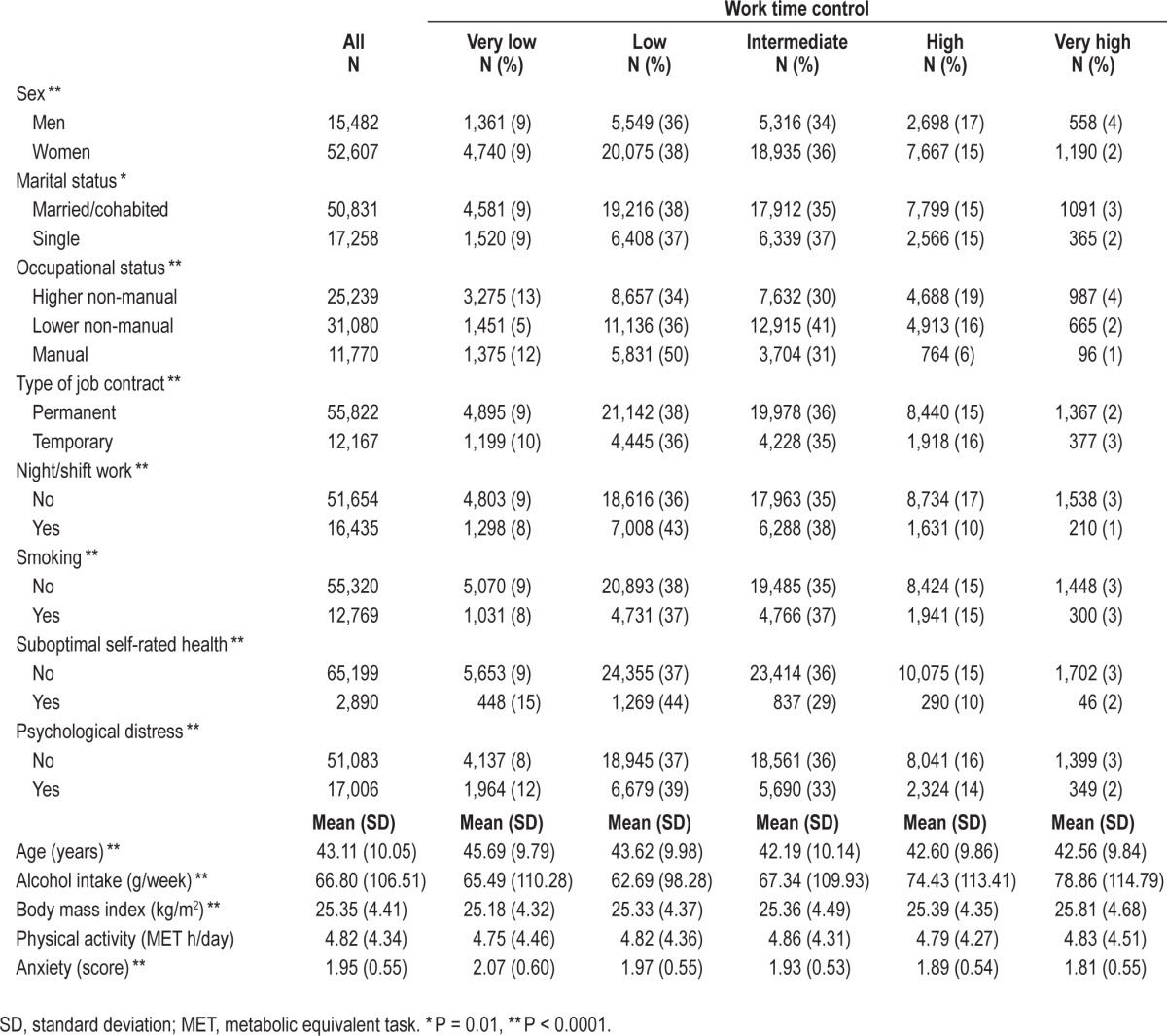
Very low work time control was reported by 6,101 participants (9%), low by 25,624 (38%), intermediate by 24,251 (35%), high by 10,365 (15%), and very high work time control by 1,748 (3%) participants at study entry. Very low or low work time control were associated with older age, manual occupational status (very low was also associated with higher non-manual occupational status which included school teachers), nonsmoking, lower physical activity, suboptimal self-rated health, and psychological distress (Table 2). The lower the work time control score, the higher the levels of anxiety. High or very high work time control was associated with male sex, higher occupational status, day work, good self-rated health, no psychological distress, and higher alcohol intake.
Table 2.
Characteristics of the study sample. For each of the 68,089 participants, data are reported for their first response included in the analysis (Phase 1, 2, 4, and 6)
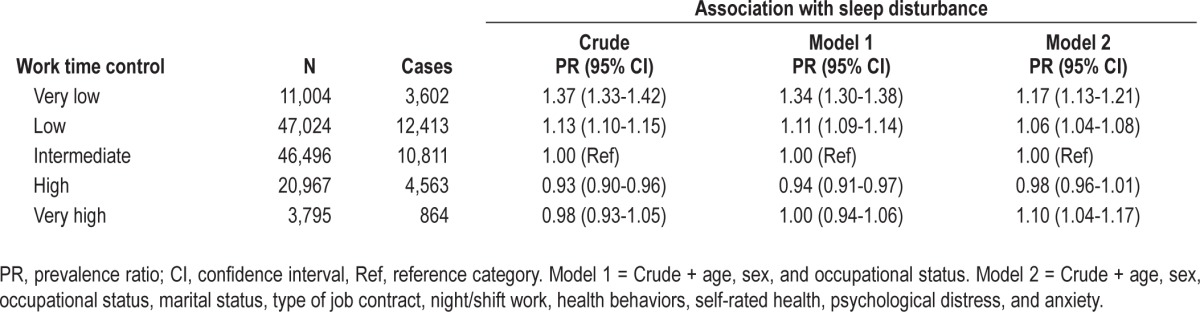
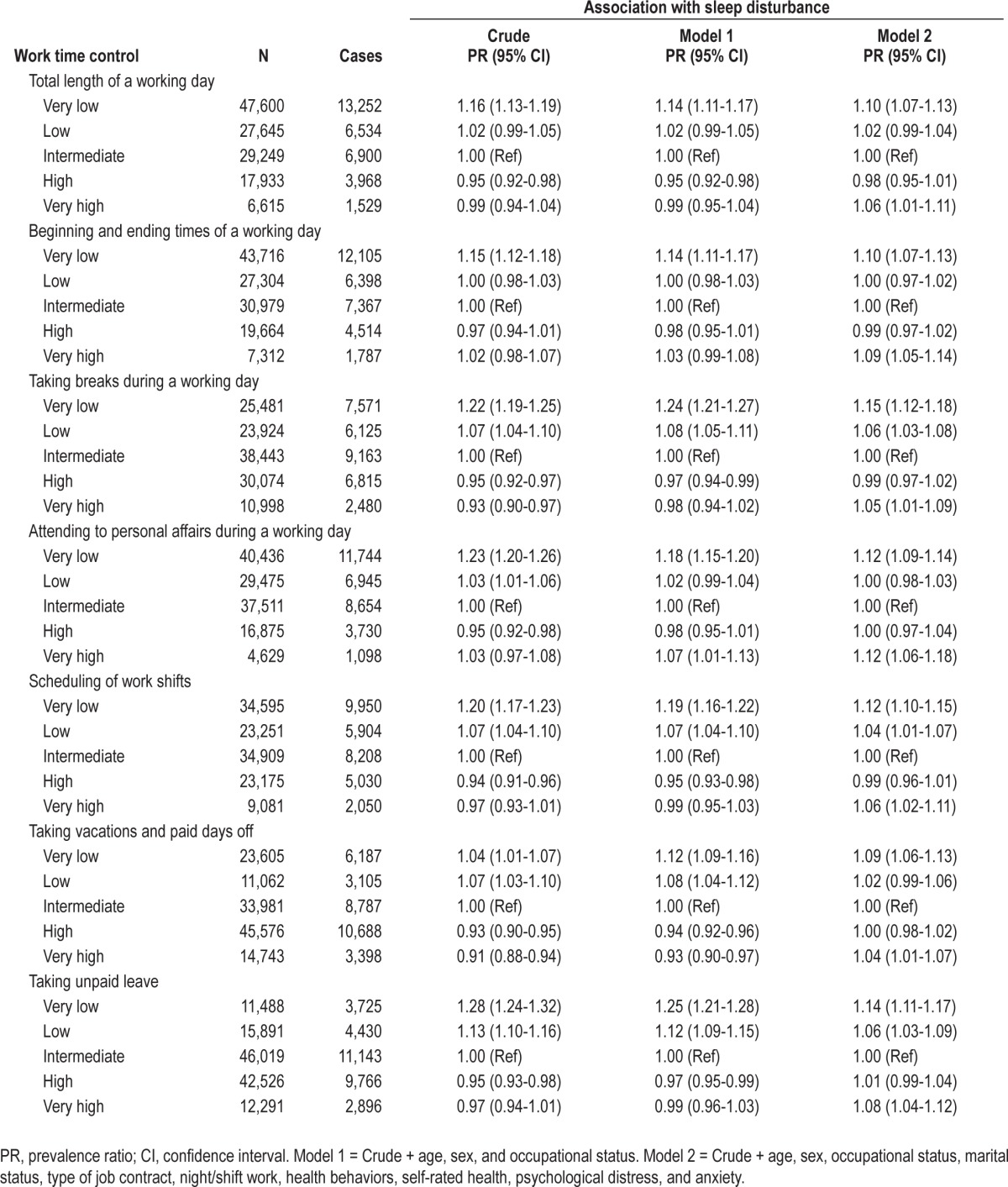
In the cross-sectional analysis, a linear trend (P < 0.0001) was observed in the crude model. Very low (PR 1.37, 95% CI 1.33-1.42) and low work time control (PR 1.13, 95% CI 1.10-1.15) were associated with higher prevalence of sleep disturbances compared to those with intermediate work time control after adjustment for survey year only (Table 3). High work time control was associated with lower sleep disturbance prevalence (PR 0.93, 95% CI 0.90-0.96), whereas there was no association between very high work time control and disturbed sleep. In the fully adjusted model, however, the association between very high work time control and sleep disturbances was increased to 1.10 (95% CI 1.04-1.17) compared to intermediate work time control. Associations between very low and low work time control with sleep disturbances were attenuated to 1.17 (95% CI 1.13-1.21) and 1.06 (95% CI 1.04-1.08), respectively, and the association with high work time control disappeared after full adjustments. We also performed a subsidiary analysis examining all 7 items separately, and the results were similar across the items (Appendix 2).
Table 3.
Cross-sectional association between work time control and sleep disturbances (5-7 nights/week) in the Finnish Public Sector study (129,286 person measurements from repeated measures in 2000-2012)
Excluding shift workers did not substantially alter the pattern of results, and there was no statistically significant interaction between work time control and shift work on sleep disturbances (Pinteraction = 0.256). Certain professions may have inherently less control over their work times because of the nature of the job. Therefore, we performed further subsidiary analyses using a more detailed categorization of occupational titles (30 categories based on the 2 first digits of the occupational title classification of Statistics Finland27) as a covariate instead of the occupational status variable with three categories (upper non-manual, lower non-manual, manual worker). In the fully adjusted model, very low work time control was associated with 1.20 times (95% CI 1.16-1.23) greater risk of sleep disturbances than intermediate work time control. The corresponding figures were 1.08 (95% CI 1.05-1.10) for low work time control, 0.97 (95% CI 0.95-1.01) for high work time control, and 1.09 (95% CI 1.03-1.16) for very high work time control. Furthermore, the U-shaped association between work time control and sleep was also found when analyzing main occupational categories ([1] senior officials and managers, professionals; [2] technicians and associate professionals, clerks; [3] service and care workers; [4] skilled agricultural workers, craft and related trades workers, plant and machine operators and assemblers, elementary occupations27) separately (all P-values < 0.004 for quadratic term of continuous work time control score).
For comparison, we analyzed the association between work time control and self-reported suboptimal health, which showed stronger associations in general (very low work time control: crude PR 1.85, 95% CI 1.71-2.00; very high work time control crude PR: 0.72, 95% CI 0.59-0.86 compared to intermediate work time control) and a clearer linear association after full adjustments (very low work time control PR 1.37, 95% CI 1.27-1.48; low work time control PR 1.15, 95% CI 1.09-1.21; high work time control PR 0.88, 95% CI 0.81-0.96; very high work time control PR 0.83, 95% CI 0.70-0.99).
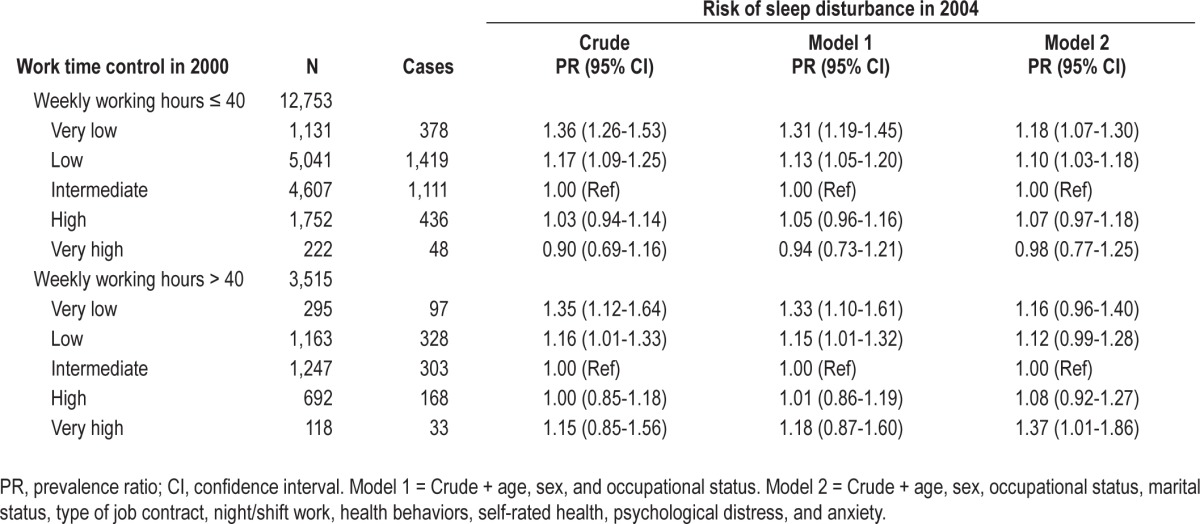
An interaction between weekly working hours and work time control was observed (P = 0.04). Among participants who worked up to 40 h/week (n = 21,044), a linear trend was observed (P < 0.001) in the fully adjusted model, but only very low work time control was statistically significantly associated with higher prevalence of sleep disturbances when compared to intermediate work time control (PR 1.12, 95% CI 1.04-1.21) (Figure 1). Among participants working > 40 h/week (n = 5,975), very high work time control was associated with 1.32-fold (95% CI 1.05-1.65) higher prevalence of sleep disturbances, whereas the prevalence was lower among participants with high work time control (PR 0.87, 95% CI 0.76-0.99) compared to those with intermediate work time control, after full adjustments. Very low work time control was associated with 1.23-fold (95% CI 1.08-1.39) and low work time control with 1.16-fold (95% CI 1.05-1.29) prevalence of sleep disturbances.
Figure 1.
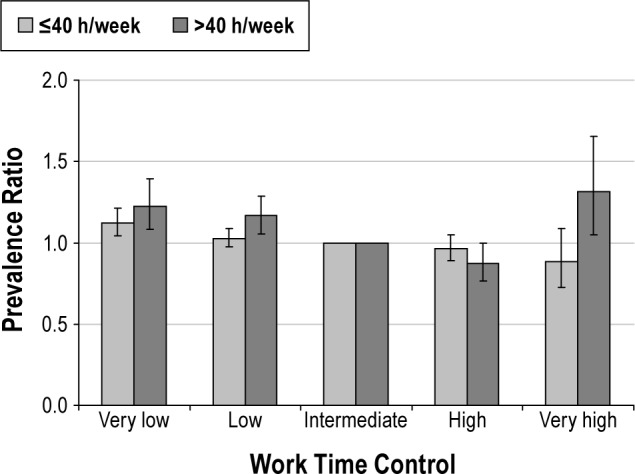
Cross-sectional association between work time control and sleep disturbances (5-7 nights/week) among participants working ≤ 40 h/ week (n = 21,044) or > 40 h/week (n = 5,975).
In the longitudinal analysis of the subsample with data on working hours, a similar association between work time control and sleep disturbances was found as in the cross-sectional analysis (Table 4). Among participants who worked > 40 h/week (n = 3,565), very high work time control in Phase 1 was associated a 1.37-fold (95% CI 1.01-1.86) prevalence of sleep disturbances in Phase 2 compared to participants with intermediate work time control, after full adjustments. Corresponding figures were 1.08 (95% CI 0.92-1.27) for high work time control, 1.12 (95% CI 0.99-1.28) for low work time control, and 1.16 (95% CI 0.96-1.40) for very low work time control. These associations did not reach statistical significance at conventional levels, possibly due to limited statistical power. Among those who worked up to 40 h/week (n = 12,938), very low (PR 1.18, 95% CI 1.07-1.30) and low (PR 1.10, 95% CI 1.03-1.18) work time control was associated with higher prevalence of sleep disturbances compared with intermediate work time control, after full adjustments.
Table 4.
Longitudinal association between work time control and sleep disturbances (5-7 nights/week) by work hours in the Finnish Public Sector study from 2000 to 2004 (sample size 16,503 employees)
DISCUSSION
Our analysis of up to 68,089 adults suggests that low work time control is associated with an increased risk of disturbed sleep. However, this association differed between employees working up to 40-hours week and those working longer hours. Among participants working up to 40-hours week, the association was linear: the higher the work time control the lower the risk of sleep disturbances. In contrast, both very low and very high levels of work time control were associated with an increased risk of sleep disturbances among participants working longer hours. These patterns of associations were robust to adjustments for demographic characteristics, health behaviors, self-rated health, and psychological distress. Although the observed effect sizes were only moderate, both cross-sectional and longitudinal analyses supported these findings.
The observed association between low work time control and sleep disturbance is in line with a substantial body of evidence linking lack of control over work time with unfavorable psychosocial and health outcomes.1–5,7,8 Many previous studies have shown a graded association, without interruptions in this pattern from the lowest to the highest levels of work time control.1–5,7 This accords with our results for participants working 40 hours per week or less. The exact mechanisms underlying these associations are unknown. For workers with low work time control, the lack of flexibility may restrict their opportunities to match their work hours with their circadian rhythms. Impaired sleep may also result from a lack of flexibility that increases work-life conflict, e.g., by making it harder to combine the requirements of the work schedule with extra-work commitments such as family or other caring duties. Conversely, workers with higher levels of work time control may be able to use this flexibility to improve their person-job fit.38
Working long hours can have positive as well as negative effects on employee health, depending on the underlying motivations and personal circumstances. For example, employees with good social support may have better tolerance of long working hours, and at the same time benefit from the improved financial security that paid overtime work provides.39 Some workers may welcome the opportunity to work longer hours for financial or other reasons, albeit potentially at the expense of inadequate sleep. Our measure of work time control included an assessment of the ability to influence the total length of one's working day. Thus, the association between very high work time control and increased sleep complaints might be explained in terms of self-imposed long work hours resulting in insufficient time being left for recuperation in the evening, leading to disturbed sleep.
Our measurement of work time control did not differentiate between formally having the opportunity to influence one's work hours and actually utilizing such opportunities. If a policy of flexibility is not exercised in practice (e.g., due to overcommitment, fear of being laid off or fear of losing a competition for a promotion) then the benefits associated with increased control over work times and schedules are likely to be lost.40 Employees with very long work hours might include a large proportion of those not exercising their high work time control—a potential explanation for the counterintuitive finding linking high work time control to increased sleep disturbance. This finding is in line with the suggestion by Costa and his colleagues that individual flexibility in work times may lead to excessive work load and unhealthy schedules.1 However, empirical evidence in this regard is scarce, with only one study having reported a cross-sectional association between high work time control and poorer sleep among employees with highly variable work schedules.12
It is noteworthy that the observed association between very high work time control and poor sleep may be specific to sleep-related outcomes. In the comparable analysis using self-rated health as the outcome, the association remained linear after full adjustments, even among those working long hours. Thus we conclude that low work time control seems generally to be associated with greater risk of sleep disturbances, but in the subgroup of those working long hours, very high work time control also seems to mark an increased risk of disrupted sleep.
Our study has some notable strengths, including reliance on prospective data from a large sample, enabling longitudinal analysis and the use of multiple measurements in the cross-sectional analysis where repeated measurements were nested within participants. The large dataset also enabled us to analyze work time control in categories based on the actual scores rather than arbitrary cut-points, such as median or tertiles, which would have reduced our chances of identifying the U-shaped association among those working long hours. Study limitations include limited generalizability as our sample comprised predominantly female (77%), racially homogeneous (white) Finnish public sector employees. The data included a range of different occupations that may have inherently different possibilities to control work time. This wide range can be seen as a strength, but may also be a source for bias. However, additional analyses controlling the type of occupation in more detail or examining the association within the four main occupational categories did not alter the results. Nevertheless, future replications of this design in other sectors of employment would be valuable.
Overtime work has also been shown to be related to poor cognitive performance in middle age and increased risk of incident coronary heart disease, independently of conventional risk factors.41,42 Further research is needed to evaluate whether the increased health risk at the extreme ends of the work time control scale is specific to sleep, whether it affects other behavioral and health-related outcomes, and whether the evolution of sleep disturbances underlie the link between long working hours and coronary health.
The current study identifies risk groups that merit the attention of occupational health practitioners. Sleep disturbances have been shown to predict somatic and mental disorders contributing to sickness absence and work disability19–21 and to be associated with increased mortality.43–46 If the associations observed in this study were causal, those reporting very low work time control could be expected to benefit from improved influence over their working times. Those reporting very high work time control, while working long hours could benefit from ergonomic advice/training on work time planning, in order that they might achieve better sleep.
DISCLOSURE STATEMENT
This was not an industry supported study. The Finnish Public Sector Study is supported by the EU ERA-AGE2 program funded by the Academy of Finland (project 264944), and the participating organizations. Dr. Kivimäki is supported by the NIH/National Institute on Aging (R01AG034454-01); the National Heart, Lung, and Blood Institute (R01HL036310-20A2), USA; the New OSH ERA research program, EU; the UK Medical Research Council (K013351); the Finnish Work Environment Foundation; and a professorial fellowship from the Economic and Social Research Council. The authors have indicated no financial conflicts of interest.
Appendix 1.
List of the 50 most common occupational groups in the Finnish Public Sector data
Appendix 2.
The association between individual items of work time control and sleep disturbance
Footnotes
A commentary on this article appears in this issue on page 1159.
REFERENCES
- 1.Costa G, Sartori S, Åkerstedt T. Influence of flexibility and variability of working hours on health and well-being. Chronobiol Int. 2006;23:1125–37. doi: 10.1080/07420520601087491. [DOI] [PubMed] [Google Scholar]
- 2.Moen P, Kelly E, Huang Q. Work, family and life-course fit: Does control over work time matter? J Vocat Behav. 2008;73:414–25. doi: 10.1016/j.jvb.2008.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jansen NW, Kant I, Nijhuis FJ, et al. Impact of worktime arrangements on work-home interference among Dutch employees. Scand J Work Environ Health. 2004;30:139–48. doi: 10.5271/sjweh.771. [DOI] [PubMed] [Google Scholar]
- 4.Joyce K, Pabayo R, Critchley JA, et al. Flexible working conditions and their effects on employee health and wellbeing. Cochrane Database Syst Rev. 2010;(2):CD008009. doi: 10.1002/14651858.CD008009.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ala-Mursula L, Vahtera J, Kouvonen A, et al. Long hours in paid and domestic work and subsequent sickness absence: does control over daily working hours matter? Occup Environ Med. 2006;63:608–16. doi: 10.1136/oem.2005.023937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Olsen KM, Dahl S. Working time: implications for sickness absence and the work-family balance. Int J Soc Welfare. 2010;19:45–83. [Google Scholar]
- 7.Vahtera J, Laine S, Virtanen M, et al. Employee control over working times and risk of cause-specific disability pension: the Finnish Public Sector Study. Occup Environ Med. 2010;67:479–85. doi: 10.1136/oem.2008.045096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Janssen D, Nachreiner F. Health and psychosocial effects of flexible working hours. Rev Saude Publica. 2004;38(Suppl):11–8. doi: 10.1590/s0034-89102004000700003. [DOI] [PubMed] [Google Scholar]
- 9.Takahashi M, Iwasaki K, Sasaki T, et al. Worktime control-dependent reductions in fatigue, sleep problems, and depression. Appl Ergon. 2011;42:244–50. doi: 10.1016/j.apergo.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 10.Viitasalo K, Kuosma E, Laitinen J, et al. Effects of shift rotation and the flexibility of a shift system on daytime alertness and cardiovascular risk factors. Scand J Work Environ Health. 2008;34:198–205. doi: 10.5271/sjweh.1228. [DOI] [PubMed] [Google Scholar]
- 11.Eriksen CA, Kecklund G. Sleep, sleepiness and health complaints in police officers: the effects of a flexible shift system. Ind Health. 2007;45:279–88. doi: 10.2486/indhealth.45.279. [DOI] [PubMed] [Google Scholar]
- 12.Kubo T, Takahashi M, Togo F, Liu X, Shimazu A, Tanaka K, Takaya M. Effects on employees of controlling working hours and working schedules. Occup Med (Lond) 2013;63:148–51. doi: 10.1093/occmed/kqs234. [DOI] [PubMed] [Google Scholar]
- 13.Ota A, Masue T, Yasuda N, et al. Psychosocial job characteristics and insomnia: a prospective cohort study using the Demand-Control-Support (DCS) and Effort-Reward Imbalance (ERI) job stress models. Sleep Med. 2009;10:1112–7. doi: 10.1016/j.sleep.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 14.de Lange AH, Kompier MA, Taris TW, et al. A hard day's night: a longitudinal study on the relationships among job demands and job control, sleep quality and fatigue. J Sleep Res. 2009;18:374–83. doi: 10.1111/j.1365-2869.2009.00735.x. [DOI] [PubMed] [Google Scholar]
- 15.Virtanen M, Ferrie JE, Gimeno D, et al. Long working hours and sleep disturbances: the Whitehall II prospective cohort study. Sleep. 2009;32:737–45. doi: 10.1093/sleep/32.6.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Elwood P, Hack M, Pickering J, Hughes J, Gallacher J. Sleep disturbance, stroke, and heart disease events: Evidence from the Caerphilly cohort. J Epidemiol Community Health. 2006;60:69–73. doi: 10.1136/jech.2005.039057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miranda H, Viikari-Juntura E, Punnett L, Riihimäki H. Occupational loading, health behavior and sleep disturbance as predictors of low-back pain. Scand J Work Environ Health. 2008;34:411–9. doi: 10.5271/sjweh.1290. [DOI] [PubMed] [Google Scholar]
- 18.Jansson-Fröjmark M, Lindblom K. A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychosom Res. 2008;64:443–9. doi: 10.1016/j.jpsychores.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 19.Salo P, Vahtera J, Hall M, et al. Using repeated measures of sleep disturbances to predict future diagnosis-specific work disability: a cohort study. Sleep. 2012;35:559–69. doi: 10.5665/sleep.1746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salo P, Oksanen T, Sivertsen B, et al. Sleep disturbances as a predictor of cause-specific work disability and delayed return to work. Sleep. 2010;33:1323–31. doi: 10.1093/sleep/33.10.1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sivertsen B, Overland S, Pallesen S, et al. Insomnia and long sleep duration are risk factors for later work disability. The Hordaland Health Study. J Sleep Res. 2009;18:122–8. doi: 10.1111/j.1365-2869.2008.00697.x. [DOI] [PubMed] [Google Scholar]
- 22.Mallon L, Broman JE, Hetta J. Sleep complaints predict coronary artery disease mortality in males: A 12-year follow-up study of a middle-aged Swedish population. J Intern Med. 2002;251:207–16. doi: 10.1046/j.1365-2796.2002.00941.x. [DOI] [PubMed] [Google Scholar]
- 23.Phillips B, Mannino DM. Do insomnia complaints cause hypertension or cardiovascular disease? J Clin Sleep Med. 2007;3:489–94. [PMC free article] [PubMed] [Google Scholar]
- 24.Geurts SA, Sonnentag S. Recovery as an explanatory mechanism in the relation between acute stress reactions and chronic health impairment. Scand J Work Environ Health. 2006;32:482–92. doi: 10.5271/sjweh.1053. [DOI] [PubMed] [Google Scholar]
- 25.Karasek R, Brisson C, Kawakami N, et al. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3:322–55. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- 26.Jenkins CD, Stanton BA, Niemcryk SJ, et al. A scale for the estimation of sleep problems in clinical research. J Clin Epidemiol. 1988;41:313–21. doi: 10.1016/0895-4356(88)90138-2. [DOI] [PubMed] [Google Scholar]
- 27.Statistics Finland. Classification of occupations. Helsinki: Statistics Finland; 2001. [Google Scholar]
- 28.Rimm EB, Williams P, Fosher K, et al. Moderate alcohol intake and lower risk of coronary heart disease: Meta-analysis of effects on lipids and haemostatic factors. BMJ Clin Res. 1999;319:1523–8. doi: 10.1136/bmj.319.7224.1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kujala UM, Kaprio J, Sarna S, et al. Relationship of leisure-time physical activity and mortality: The Finnish Twin Cohort. JAMA. 1998;279:440–4. doi: 10.1001/jama.279.6.440. [DOI] [PubMed] [Google Scholar]
- 30.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- 31.Holi MM, Marttunen M, Aalberg V. Comparison of the GHQ-36, the GHQ-12 and the SCL-90 as psychiatric screening instruments in the Finnish population. Nord J Psychiatry. 2003;57:233–8. doi: 10.1080/08039480310001418. [DOI] [PubMed] [Google Scholar]
- 32.Spielberger CD, Gorsuch RL, Lushene R, et al. Palo Alto: Consulting Psychologists Press Inc; 1983. Manual for the State-Trait Anxiety Inventory (form Y) [Google Scholar]
- 33.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162:199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 34.Lipsitz SR, Kim K, Zhao L. Analysis of repeated categorical data using generalized estimating equations. Stat Med. 1994;13:1149–63. doi: 10.1002/sim.4780131106. [DOI] [PubMed] [Google Scholar]
- 35.Vahtera J, Poikolainen K, Kivimäki M, Ala-Mursula L, Pentti J. Alcohol intake and sickness absence: a curvilinear relation. Am J Epidemiol. 2002;156:969–76. doi: 10.1093/aje/kwf138. [DOI] [PubMed] [Google Scholar]
- 36.Neovius K, Johansson K, Kark M, Neovius M. Obesity status and sick leave: a systematic review. Obes Rev. 2009;10:17–27. doi: 10.1111/j.1467-789X.2008.00521.x. [DOI] [PubMed] [Google Scholar]
- 37.Ala-Mursula L, Vahtera J, Pentti J, et al. Effect of employee worktime control on health: a prospective cohort study. Occup Environ Med. 2004;61:254–61. doi: 10.1136/oem.2002.005983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Baltes BB, Briggs TE, Huff JW, et al. Flexible and compressed workweek schedules: A meta-analysis of their effects on work-related criteria. J Appl Psychol. 1999;84:496–513. [Google Scholar]
- 39.Tucker P, Rutherford C. Moderators of the relationship between long work hours and health. J Occup Health Psychol. 2005;10:465–76. doi: 10.1037/1076-8998.10.4.465. [DOI] [PubMed] [Google Scholar]
- 40.Kossek E, Michel J. Flexible work schedules. In: Zedeck S, editor. APA Handbook of industrial and organisational psychology (Vol. 1) Washington, DC: American Psychological Association; 2010. [Google Scholar]
- 41.Virtanen M, Singh-Manoux A, Ferrie JE, et al. Long working hours and cognitive function: the Whitehall II Study. Am J Epidemiol. 2009;169:596–605. doi: 10.1093/aje/kwn382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Virtanen M, Ferrie JE, Singh-Manoux A, et al. Overtime work and incident coronary heart disease: the Whitehall II prospective cohort study. Eur Heart J. 2010;31:1737–44. doi: 10.1093/eurheartj/ehq124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mallon L, Broman JE, Hetta J. Sleep complaints predict coronary artery disease mortality in males: a 12-year follow-up study of a middle-aged Swedish population. J Intern Med. 2002;251:207–16. doi: 10.1046/j.1365-2796.2002.00941.x. [DOI] [PubMed] [Google Scholar]
- 44.Kripke DF, Garfinkel L, Wingard DL, et al. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–6. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 45.Hublin C, Partinen M, Koskenvuo M, et al. Heritability and mortality risk of insomnia-related symptoms: a genetic epidemiologic study in a population-based twin cohort. Sleep. 2011;34:957–64. doi: 10.5665/SLEEP.1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rod NH, Vahtera J, Westerlund H, et al. Sleep disturbances and cause-specific mortality: Results from the GAZEL cohort study. Am J Epidemiol. 2011;173:300–9. doi: 10.1093/aje/kwq371. [DOI] [PMC free article] [PubMed] [Google Scholar]


