Abstract
Background
The acquisition of flatfoot by an adult is thought to primarily be caused by posterior tibial tendon dysfunction, although some other causes, such as congenital flexible flatfoot or an accessory navicular, may also be responsible. The objective of this study was to evaluate the bone rotation of each joint in the medial longitudinal arch (MLA) and compare the response in healthy feet with that in flat feet by analyzing the reconstructive three-dimensional (3D) CT image data during weightbearing.
Methods
CT scans of 20 healthy feet and 24 feet with flatfoot deformity were taken in non-load condition followed by full-body weightbearing condition. Images of the tibia and MLA bones (first metatarsal bone, cuneiforms, navicular, talus, and calcaneus) were reconstructed into 3D models. The volume merge method in three planes was used to calculate the bone-to-bone relative rotations.
Findings
Under loading conditions, the flatfoot dorsiflexed more in the first tarsometatarsal joint, and everted more in the talonavicular and talocalcaneal joints compared with the healthy foot. The total relative rotation was larger in the flatfoot compared with the healthy foot only in the first tarsometatarsal joint.
Interpretation
Supporting the MLA in the sagittal direction and the subtalar joint in the coronal direction may be useful for treating flatfoot deformity. The first tarsometatarsal joint may play an important role in diagnosing or treating flatfoot deformity.
Keywords: Three-dimensional Image, Flatfoot, Medial Longitudinal Arch, Weightbearing
INTRODUCTION
The arch-shaped structure of the foot, comprising longitudinal and transverse components, sustains the bipedal human body-weight during standing, and transmits it to the ground efficiently from the heel to the toes during walking (Sarrafian, 1983). The longitudinal arch consists of the medial and lateral sides. The medial longitudinal arch (MLA) is major and constructed from the first metatarsal bone, cuneiforms, navicular, talus, and calcaneus. It supports the body-weight, loaded from the tibia to talus, with soft tissues connecting them. Flatfoot deformity is a clinical problem that represents the collapse of the MLA, hindfoot valgus, and forefoot abduction when the foot is loaded (Van Boerum and Sangeorzan, 2003). Patients with intractable, severe flatfoot are treated with various surgical procedures, such as combinations of osteotomy, tendon transfer, or arthrodesis, to achieve realignment of MLA (Chi et al., 1999; Greisberg et al., 2005; Myerson, 1997; Sangeorzan et al., 1993). The etiology can be congenital or acquired. (Mann, 1999) The main etiology of adult acquired flatfoot is considered to be posterior tibial tendon dysfunction (PTTD) (Myerson, 1997), although the transient type of congenital adolescent flexible flatfoot and the asymptomatic type have also been recognized (Dyal et al., 1997; Pedowitz and Kovatis, 1995). Its mechanisms or biomechanics are still unknown and the operative treatments are also still controversial.
Experimentally, many cadaveric studies of MLA have been performed (Huang et al., 1993; Imhauser et al., 2002; Kitaoka et al., 1995; Kitaoka et al., 1998; Kitaoka et al., 2002; Thordarson et al., 1995). Attempts have been made to clarify how the tissues are involved in MLA by resecting the tissue of interest, e.g., a ligament in the plantar arch supportive tissue or posterior tibial tendon (Huang et al., 1993; Kitaoka et al., 1995), and some studies on how the structure of the arch is destroyed and dealt with by foot orthoses or multiple surgical procedures have also been carried out by using cadaveric flatfoot models (Imhauser et al., 2002; Kitaoka et al., 1998; Kitaoka et al., 2002; Thordarson et al., 1995).
Clinically, two-dimensional (2D) examinations of foot prints (Staheli et al., 1987; Tareco et al., 1999), the height of the navicular or cuneiforms, the radiographic talo-first metatarsal angle (Karasick and Schweitzer, 1993; Saltzman et al., 1995; Supple et al., 1992; Younger et al., 2005), and deformations of each joint in MLA on CT images (Ananthakrisnan et al., 1999; Ferri et al., 2008; Greisberg et al., 2003) and so forth were performed to evaluate alignment. However, no study has been hitherto reported, to the best of our knowledge, to examine the load response of MLA three-dimensionally in patients with flatfoot deformity.
The main hypothesis of the present study was that the segmental motions observed at MLA in patients with morphological flatfoot deformity would increase under loading, especially around the mid-hindfoot.
METHODS
A total of 22 subjects were recruited for the present IRB study. All participants provided written informed consent. Twenty healthy feet (10 healthy volunteers, 6 males and 4 females, median age, 35.5 years; range, 21 to 44) and twenty-four feet with symptomatic flatfoot deformity (12 patients, 5 males and 7 females, median age, 34.7 years; range, 20 to 68) were studied. The exclusion criteria were prior foot surgery that could have changed the bone shape. Two orthopedic specialists made the diagnosis of flatfoot deformity based on a clinical examination and feet projection X-rays during loading. The talo-first metatarsal angle was used on the lateral projection. A flatfoot was diagnosed as a foot with a talo-first metatarsal angle of greater than 4 degrees, whereas the angle in a healthy foot was less than 4 degrees and greater than −4 degrees (flatfoot: 14.0 degrees [SD 5.9 degrees], healthy foot: 2.8 degrees [SD 0.6 degrees]) (Karasick and Schweitzer, 1993; Supple et al., 1992). Two individuals with flat feet were diagnosed as PTTD, and the remainder were diagnosed as the transient type of congenital adolescent flat feet. An accessory navicular was found in 11 feet.
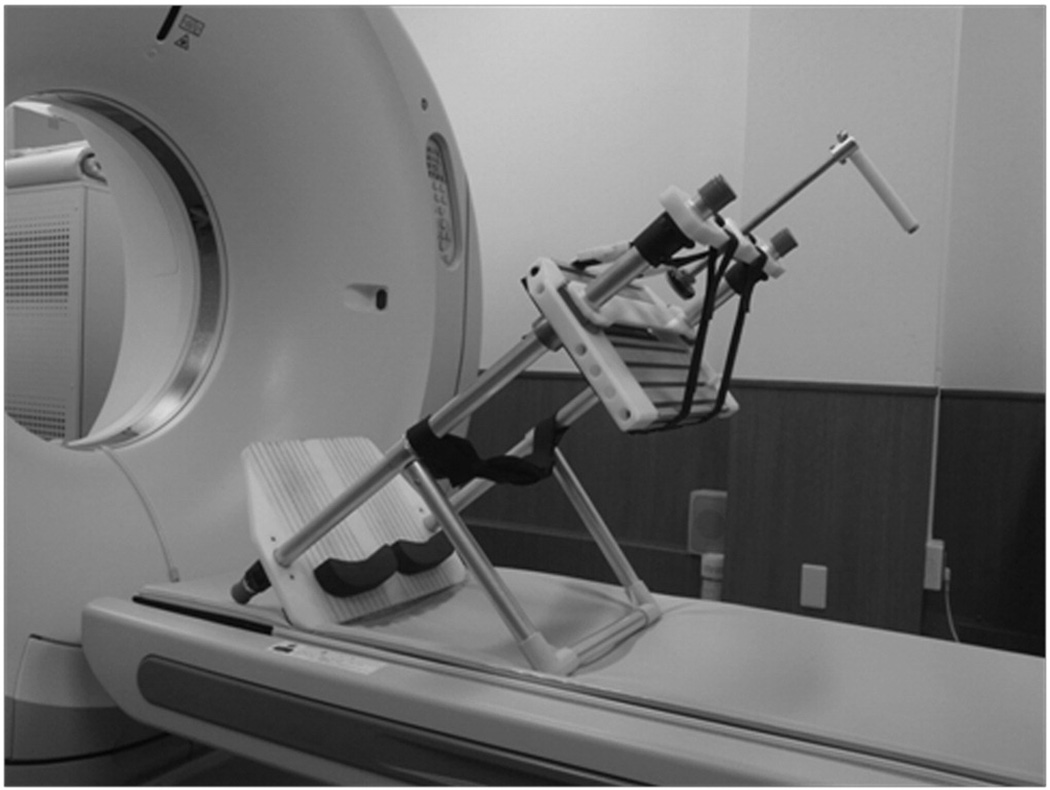
The same custom-made foot loading device that we previously reported was used to apply loads (Figure 1) (Kido et al., 2011a, 2011b). The subjects lay on a CT table, keeping their hips at 50-degree flexion, knees at 90-degree flexion, and feet in a neutral position supported by the device. Both legs were set parallel to the square and lateral device shafts, respectively, with the knee and ankle centers being aligned to the load line. CT images of both feet were scanned from 5 cm proximal of the tibiotalar joint to the sole, using a 64 multi-slice CT scanner. The CT images were taken in a non-load condition, followed by loading with each subject’s weight mimicking full-body-weightbearing. Data were collected for approximately 6 seconds after the load had reached the body weight load.
Figure 1.
The same custom-made foot loading device as reported in the previous studies (Kido et al., 2011a, 2011b).
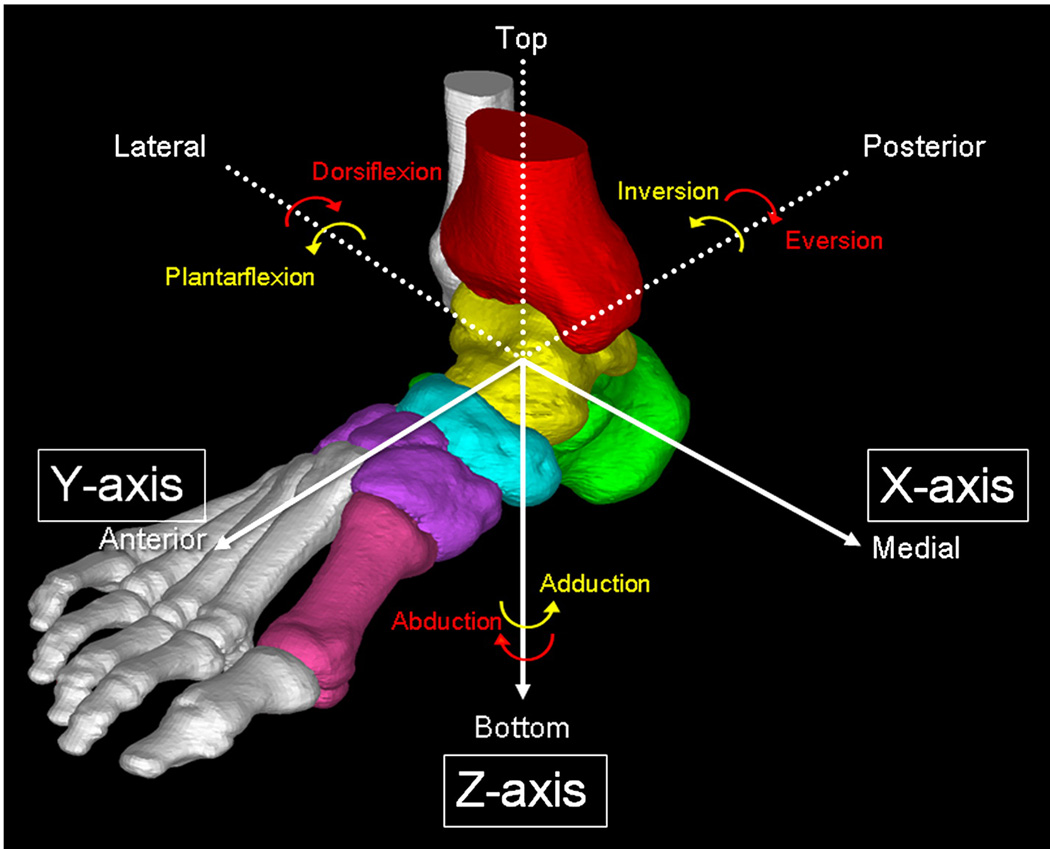
The images of the tibia and MLA bones (first metatarsal bone, cuneiforms, navicular, talus, and calcaneus) were saved in the Digital Imaging and Communications in Medicine (DICOM) format, and reconstructed into a 3D model using a 3D reconstruction software package (Mimics, Materialise Inc., Leuven, Belgium). A threshold level was set to cortical regions of the bones. Medial, middle, and lateral cuneiforms were seen as a single mass of cuneiforms. The 3D models of the intended bones were created after segmentation of them (Figure 2).
Figure 2.
A 3D CT model of the tibia and the MLA bones (first metatarsal bone, cuneiforms, navicular, talus, and calcaneus). A global X–Y–Z coordinate system corresponding anatomical axes was used to describe the orientation of tarsal bones.
Rotations of the MLA bones associated with loading were measured using a validated volume merge technique (Imai et al., 2009; Kido et al., 2011a; Ochia et al., 2006). The rotations of the following bones were calculated: the cuneiforms relative to the navicular at the cuneonavicular joint (Nav-Cun); the first metatarsal bone relative to the cuneiforms at the first tarsometatarsal joint (Cun-M1); the first metatarsal bone relative to the talus (Tal-M1); and the first metatarsal bone relative to the tibia (Tibio-M1). A global X-Y-Z coordinate system corresponding to anatomical axes was used to describe the orientation of tarsal bones in the unloaded condition. The Z-axis was set along the tibial shaft through the center of the ankle, and the Y-axis was set parallel to the projection of a line connecting the center of the heel and the second metatarsal head on a plane perpendicular to the Z-axis. The X-axis was determined according to a right-hand rule from the Y-axis and Z-axis. The coronal (XY) plane, sagittal (XZ) plane, and transverse (YZ) plane were defined from these X-Y-Z axes (Figure 2). A local coordinate system was defined for each tarsal bone with its origin at the volume center of each bone and the same orientations as the X-Y-Z axes. The rotations of the tarsal bones under loading were expressed using Eulerian angles. Dorsiflexion, eversion, and abduction were presented with a plus sign, and plantarflexion, inversion, and adduction were presented with a negative sign (Kido et al., 2011a; Kitaoka et al., 1995; Kitaoka et al., 1998; Kitaoka et al., 2002). The sum of the square root of the rotations about the 3 axes was also evaluated as the total rotation. The rotations of tarsal bones in the healthy foot were compared with those in the flatfoot. The results are presented as the mean ± standard deviation (SD). Differences in the load response between healthy and flat feet were analyzed by a one-tailed unpaired t-test using Bonferroni’s adjustment with a P value less than 0.002.
RESULTS
The subjects did not complain any discomfort during loading.
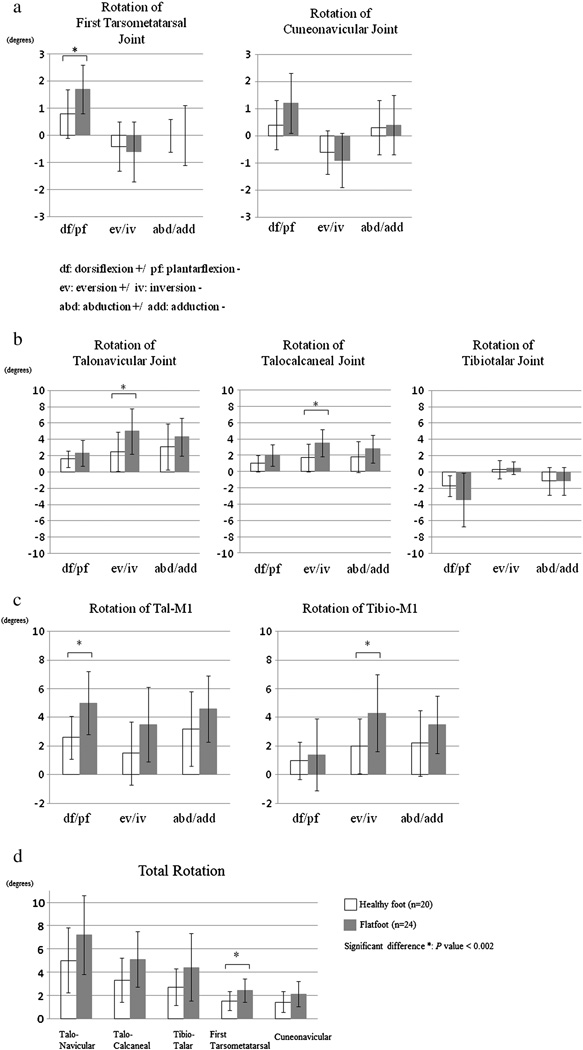
The rotations of the joints and the bone-to-bone relationships are summarized in Table 2 and shown in Figures 3a, 3b, 3c and 3d. The load responses of the tarsal bones of the left and right feet were different (data not shown).
Table 2.
Comparison of the load response between live and cadaver feet for the talo-1st metatarsal rotation, tibio-1st metatarsal rotation and adjacent MLA joints.
| Present study (live foot) |
Kitaoka et al. (1998) (cadaver foot) |
Blackman et al. (2009) (cadaver foot) |
|||||
|---|---|---|---|---|---|---|---|
| Healthy | Flatfoot | Difference | P value | Difference | Difference | ||
| 1st Tarsometatarsal joint (Cun-M1) |
df+/pf− | 0.8° (0.9°) | 1.7° (0.9°) | 0.9°* | <0.002 | N.R. | N.R. |
| ev+/iv− | −0.4° (0.9°) | −0.6° (1.1°) | −0.2° | 0.2585 | N.R. | N.R. | |
| abd+/add− | 0.0° (0.6°) | 0.0° (1.1°) | 0.0° | 0.5169 | N.R. | N.R. | |
| total rotation | 1.5° (0.8°) | 2.4° (1.0°) | 0.9°* | <0.002 | N.R. | N.R. | |
| Cuneonavicular joint (Nav-Cun) |
df+/pf− | 0.4° (0.9°) | 1.2° (1.1°) | 0.8° | 0.0071 | N.R. | N.R. |
| ev+/iv− | −0.6° (0.8°) | −0.9° (1.0°) | −0.3° | 0.1491 | N.R. | N.R. | |
| abd+/add− | 0.3° (1.0°) | 0.4° (1.1°) | 0.1° | 0.3400 | N.R. | N.R. | |
| total rotation | 1.4° (0.9°) | 2.1° (1.1°) | 0.7° | 0.0143 | N.R. | N.R. | |
| Talonavicular joint (Tal-Nav) |
df+/pf− | 1.6° (1.0°) | 2.3° (1.6°) | 0.7° | 0.0600 | 10.5° (6.6°)* | 1.47° (2.07°)* |
| ev+/iv− | 2.5° (2.4°) | 5.0° (2.8°) | 2.5°* | <0.002 | 8.1° (3.8°)* | 2.98° (1.74°)* | |
| abd+/add− | 3.1° (2.8°) | 4.3° (2.3°) | 1.2° | 0.0631 | 13.6° (5.0°)* | 3.02° (2.2°*) | |
| total rotation | 5.0° (2.8°) | 7.2° (3.4°) | 2.2° | 0.0121 | N.R. | N.R. | |
| Talocacaneal joint (Tal-Cal) |
df+/pf− | 1.0° (1.0°) | 2.0° (1.3°) | 1.0° | 0.0021 | N.R. | N.R. |
| ev+/iv− | 1.7° (1.7°) | 3.5° (1.7°) | 1.8°* | <0.002 | N.R. | N.R. | |
| abd+/add− | 1.8° (1.9°) | 2.8° (1.7°) | 1.0° | 0.0465 | N.R. | N.R. | |
| total rotation | 3.3° (1.9°) | 5.1° (2.4°) | 1.8° | 0.0043 | N.R. | N.R. | |
| Tibiotalar joint (Tib-Tal) |
df+/pf− | −1.7° (1.3°) | −3.4° (3.3°) | −1.7° | 0.0176 | N.R. | N.R. |
| ev+/iv− | 0.3° (1.1°) | 0.5° (0.8°) | 0.2° | 0.3053 | N.R. | N.R. | |
| abd+/add− | −1.1° (1.7°) | −1.1° (1.7°) | 0.0° | 0.4782 | N.R. | N.R. | |
| total rotation | 2.7° (1.6°) | 4.4° (2.9°) | 1.7° | 0.0130 | N.R. | N.R. | |
| Talo-1st metatarsal rotation (Tal-M1) |
df+/pf− | 2.6° (1.5°) | 5.0° (2.2°) | 2.4°* | <0.002 | 10.4° (3.6°)* | 4.89° (3.59°)* |
| ev+/iv− | 1.5° (2.2°) | 3.5° (2.6°) | 2.0° | 0.0067 | 10.9° (6.0°)* | 0.57° (1.68°)* | |
| abd+/add− | 3.2° (2.6°) | 4.6° (2.3°) | 1.4° | 0.0325 | 11.7° (4.4°)* | 3.98° (3.30°)* | |
| total rotation | 5.2° (2.3°) | 8.0° (3.4°) | 2.8°* | <0.002 | N.R. | N.R. | |
| Tibio-1st metatarsal rotation(Tibio-M1) |
df+/pf− | 1.0° (1.3°) | 1.4° (2.5°) | 0.4° | 0.2756 | N.R. | N.R. |
| ev+/iv− | 2.0° (1.9°) | 4.3° (2.7°) | 2.3°* | <0.002 | N.R. | N.R. | |
| abd+/add− | 2.2° (2.3°) | 3.3° (2.0°) | 1.1° | 0.0538 | N.R. | N.R. | |
| total rotation | 4.0° (2.1°) | 6.4° (2.7°) | 2.4°* | <0.002 | N.R. | N.R. | |
N.R.: not reported
df: dorsiflexion +/ pf: plantarflexion
ev: eversion +/ iv: inversion
abd: abduction +/ add: adduction
Data are expressed as mean (SD).
Significant difference: P value < 0.002 in this study. P value < 0.05 in cadaveric studies.
Figure 3.
a) The rotation of the first metatarsal bone under loading relative to the cuneiforms at the first tarsometatarsal joint, and the cuneiforms relative to the navicular at the cuneonavicular joint. b) The rotation of the navicular under loading relative to the talus at the talonavicular joint, and the calcaneus relative to the talus at the talocalcaneal joint, and the talus relative to the tibia at the tibiotalar joint. c) The relative bone-to-bone rotation of the first metatarsal bone relative to the talus and tibia. d) The total relative rotation in MLA joints and the tibiotalar joint. The data of the healthy foot (n=20) was expressed by white bars and that of the flatfoot (n=24) was expressed by black bars.
The rotation of the first metatarsal bone under loading relative to the cuneiforms at the first tarsometatarsal joint (Cun-M1) was more dorsiflexed in the flatfoot as compared to the healthy foot (flatfoot: mean 1.7 degrees [SD 0.9 degrees], healthy foot: mean 0.8 degrees [SD 0.9 degrees], P = 0.0012). In the flatfoot, the navicular under loading relative to the talus at the talonavicular joint was more everted as compared to the healthy foot (flatfoot: mean 5.0 degrees [SD 2.8 degrees], healthy foot: mean 2.5 degrees [SD 2.4 degrees], P = 0.0015). Compared with the healthy foot, the calcaneus in the flatfoot was more everted (flatfoot: mean 3.5 degrees [SD 1.7 degrees], healthy foot: mean 1.7 degrees [SD 1.7 degrees], P = 0.0005) relative to the talus at the talocalcaneal joint under loading. The compositions of the Tal-Nav, Nav-Cun and Cun-M1 vectors and the first metatarsal bone relative to the talus (Tal-M1) were more dorsiflexed (flatfoot: mean 5.0 degrees [SD 2.2 degrees], healthy foot: mean 2.6 degrees [SD 1.5 degrees], P < 0.0001) compared to the healthy foot. The compositions of the Tibio-Tal, Tal-Nav, Nav-Cun and Cun-M1 vectors and the first metatarsal bone relative to the tibia (Tibio-M1) were more everted as compared to the healthy foot (flatfoot: mean 4.3 degrees [SD 2.7 degrees], healthy foot: mean 2.0 degrees [SD 1.9 degrees], P = 0.0015). Based on the available measurements, no significant differences were observed in the rotations of the other joints or in the bone-to-bone relationships.
The largest total rotation was observed in the talonavicular joint (flatfoot: mean 7.2 degrees [SD 3.4 degrees], healthy foot: mean 5.0 degrees [SD 2.8 degrees]), followed in order by talocalcaneal joint (flatfoot: mean 5.1 degrees [SD 2.4 degrees], healthy foot: mean 3.3 degrees [SD 1.9 degrees]), tibiotalar joint (flatfoot: mean 4.4 degrees [SD 2.9 degrees], healthy foot: mean 2.7 degrees [(SD 1.6 degrees]), first tarsometatarsal joint (flatfoot: mean 2.4 degrees [SD 1.0 degrees], healthy foot: mean 1.5 degrees [SD 0.8 degrees]), and cuneonavicular joint (flatfoot: mean 2.1 degrees [SD 1.1 degrees], healthy foot: mean 1.4 degrees [SD 0.9 degrees]). The total relative rotation between the non-load and full-body-weightbearing load conditions was significantly larger in the flatfoot than in the healthy foot only in the first tarsometatarsal joint (flatfoot: mean 2.4 degrees [SD 1.0 degrees], healthy foot: mean 1.5 degrees [SD 0.8 degrees], P =0.0008), and in the talo-first metatarsal bone (flatfoot: mean 8.0 degrees [SD 3.4 degrees], healthy foot: mean 5.2 degrees [SD 2.3 degrees], P =0.0019) and the tibio-first metatarsal bone (flatfoot: mean 6.4 degrees [SD 2.7 degrees], healthy foot: mean 4.0 degrees [SD 2.1 degrees], P =0.0014) relationships. With the numbers available, no significant difference was found between the left and right feet (data not shown).
DISCUSSION
The arch of the foot, only seen in plantigrade homo sapiens, is a distinctive structure that supports the body-weight and transmits it to the ground. It is three-dimensional and complex, consisting of twelve bones from the calcaneus in the hindfoot to metatarsal bones in the forefoot, and soft tissues such as many ligaments, capsules, and intrinsic or extrinsic muscles. However, no three-dimensional study has been performed to date. In the present study, 3D load responses of bones in MLA under full-body-weightbearing were measured in vivo with a high accuracy for the first time, and differences of the rotational change in position among the MLA bones were demonstrated between the flatfoot and healthy foot.
There has so far been no in vivo study evaluating the load response of forefoot bones. Many cadaveric studies have been reported that analyzed the intact structure of MLA. Manter (1946) demonstrated the transmission of compressive force when a 60 Ib (27.2 kg) axial load was applied to the talus. Kitaoka et al. (1995) attached a kinematic sensor to the tarsal bones of an amputated leg and measured the response of the bone position relative to the fixed tibia upon axial loads of 667 N (68.1 kg). They analyzed the first metatarsal bone position difference relative to the tibia between non-load and full-body-weightbearing load conditions. Subsequently, they used a method to simulate tendon loads in an amputated leg, and analyzed the first metatarsal bone position difference relative to the talus in the same way (Kitaoka et al., 2002). Our noninvasive method ensured the measurement of the relative bone-to-bone rotation angle, and it was considered to be comparable to the reported method when an axial load was applied and the rotation angle of the tibia was very small. The direction of each relative rotation of an intact cadaver foot was the same as that of the living healthy foot (Table 1). Compared to the study involving tendon loading, the values of all rotations were very similar. No documented data are available concerning the load response of the first tarsometatarsal and cuneonavicular joint in the cadaver foot. For the living healthy foot, a weak load response of about only one degree in those joints has been reported. Similarly, Wanivenhaus et al. (1989) demonstrated that there was only a small passive motion in the first tarsometatarsal joint by investigating 100 intact cadaver feet. Moreover, Manter (1946) evaluated that the compressive force in the first tarsometatarsal joint was about one-ninth the load (6.8 Ib (3.1 kg)) in the talus. These literature data may support our present results.
Table 1.
Comparison of each direction and total rotation between live and cadaver feet for the talo-1st metatarsal and tibio-1st metatarsal rotation.
| Present study (healthy live foot) | Kitaoka et al. (1994, 2002) (intact cadaver foot) |
|||||
|---|---|---|---|---|---|---|
| Each direction | Total rotation | Each direction | Total rotation | |||
| df+/pf− | 2.6° (1.5°) | 5.2° (2.3°) | 3.2° (2.3°) | N.R. | ||
| Talo-1st metatarsal rotation |
ev+/iv− | 1.5° (2.2°) | 1.3° (3.5°) | |||
| abd+/add− | 3.2° (2.6°) | 2.5° (2.2°) | ||||
| df+/pf− | 1.0° (1.3°) | 4.0° (2.1°) | + | 7.7° (1.8°) | ||
| Tibio-1st metatarsal rotation |
ev+/iv− | 2.0° (1.9°) | + | |||
| abd+/add− | 2.2° (2.3°) | + | ||||
N.R.: not reported
df: dorsiflexion +/ pf: plantarflexion
ev: eversion +/ iv: inversion
abd: abduction +/ add: adduction
Data are expressed as mean (SD).
Flatfoot models were employed in some cadaveric studies and the response of MLA bones on loading was quantified. There are two studies that evaluated the load response of the first metatarsal bone relative to the talus. Kitaoka et al. (1998) made a PTTD flatfoot model with almost all of the talar ligaments resected and with only the posterior tibial tendon unloaded. They examined the difference in the load response in intact cadaver feet and flatfoot models (Table 2). Blackman et al. (2009) used a kinematic sensor inserted into the tarsal bone and measured the relative bone-to-bone rotation using Cardan angles. They made a soft tissue-attenuated PTTD flatfoot model to simulate the tendon loads (unloading only the posterior tibial tendon) after added longitudinal incision to specific ligaments and repeated periodic load to the cadaveric foot, and compared the load response of a flatfoot model with an intact cadaver on 491 N (50.1 kg) axial loading. In the current study, the rotations of the first metatarsal bone relative to the talus were significantly dorsiflexed in patients with flatfoot deformity. The difference in the quantity of bone rotation in the direction in the current study was consistent with those observed by Blackman et al. (2009) (Table 2). The value was smaller than the literature data. Moreover, a similar study of Blackwood et al. (2005), in which the sagittal plane range of motion of the metatarsals was increased when the hindfoot was in valgus, is consistent with this study. Supporting the talo-first metatarsal bone relationship in the sagittal direction may be useful for treating the flatfoot deformity.
More efforts were focused on the adjacent MLA joints. Compared to the healthy feet, the flat feet dorsiflexed about one degree more around the first tarsometatarsal joint, and everted approximately two degrees more around the talonavicular and talocalcaneal joints, and the total rotation in the three planes increased by approximately one degree in the first tarsometatarsal joint. No significant difference was observed in any other joint planes. We previously evaluated the load response difference between the flatfoot and healthy foot at the hindfoot and reported that the flatfoot plantarflexed more in the tibiotalar joint, dorsiflexed more in the talocalcaneal joint, and everted more in the talonavicular and talocalcaneal joints compared with the healthy foot (Kido et al., 2011a). However, only the talonavicular and talocalcaneal joints in the hindfoot of the flatfoot were confirmed to evert more as the result of multiple comparisons of all the MLA joints. Supporting the talonavicular and talocalcaneal joints in the coronal direction may be useful for treating the flatfoot deformity. There are few studies about the load response of the first tarsometatarsal joint. According to Mizel (1993), the plantar first metatarsal first cuneiform ligament was only important for its sagittal stability in cadaveric feet, and the ligament was thought to be more flexible in flat than in healthy feet. Greisberg et al. (2003) compared the relative position of MLA bones in flat feet to those in healthy feet on weightbearing CT in the sagittal plane. They observed osteoarthritis in the cuneonavicular joint as well as sagittal subluxation in the first tarsometatarsal joint, and evaluated that the cuneiforms relative to the navicular in the cuneonavicular joint in flat feet dorsiflexed 15 degrees more than in healthy controls. It may not be appropriate to compare the present study to their static study. Taking into consideration that the difference in the sagittal bone rotation between the flatfoot and healthy foot during weightbearing in the present study was only one degree in both cuneonavicular and first tarsometatarsal joints, other motions such as walking or running might increase the load on the forefoot. Moreover, the total rotation difference of one degree between the flatfoot and healthy foot in the first tarsometatarsal joint may be small, but this joint may play an important role in the diagnosis and treatment of the flatfoot deformity.
The relation between the talus and first metatarsal bone has been widely used in clinics to evaluate flatfoot deformity. In the present study, the first metatarsal bone dorsiflexed more significantly relative to the talus in patients with flatfoot deformity. Moreover, the first metatarsal bone everted more significantly relative to the tibia in patients with flatfoot deformity. As for the individual planes or joints in the MLA with the flatfoot deformity, the sagittal instability in dorsiflexion was seen in the first tarsometatarsal joint and the coronal instability in eversion was recognized in the subtalar joints. In the treatment of the flatfoot deformity, it might be necessary to provide supports both for the MLA in the sagittal direction and for the subtalar joints in the coronal direction.
The total rotation was the largest in the talonavicular joint, which is considered to be mainly because the joint was on the top of the triangular structure and loaded the most, as previously reported (Manter, 1946; Sarrafian, 1983). Moreover, among the MLA joints, the talonavicular, cuneonavicular, and first tarsometatarsal joints are saddle-like and thus share force when they are loaded. Although two joints are at least laterally sustained (the cuneonavicular joint by the cuboid and the first tarsometatarsal joint by the second metatarsal bone), the talonavicular joint is thought to carry the highest load.
One limitation of this study is that the objectives were primarily concerned with transient flatfoot from adolescence. Niki et al. (2001) created a flatfoot model loading the posterior tibial tendon with the peritalar soft tissues resected, while evaluating the load response of only the hindfoot in the MLA. Moreover, we assume left and right feet of individual subjects as independent samples to reduce the radiation dose in CT examination, because the loading device applies loads similarly to the left and right feet (Kido et al., 2011b). Furthermore, as we reported (Kido et al., 2011a), loading tends to extend over the hindfoot, and the method used to apply the foot load may be non-physiological when tarsal bones cannot be tensioned well because the gastrocnemius does not produce much tension in the knee flexion position. However, in a supine position, the lower limb joints of flexion contracture patients can be easily bent when applying a load to the sole, which could reduce the accuracy and reproducibility of the data. Therefore, a foot loading device was created for applying sufficient weightbearing in the knee flexion position during imaging. Moreover, the coefficient of variation in the measured values of the loading force of the foot was reported. In addition, the measurements of bone motion are accompanied with a high standard deviation that also existed in the earlier studies using cadavers each other. There might be an issue of soft tissue flexibility related to flatfoot deformity from person to person.
The present method might be applicable to basic research on classifying flatfoot deformity or analyzing its development, as well as to clinical analysis for evaluating foot disorders with some deformity and deciding the surgical procedures, although it still has some drawbacks that need to be improved.
ACKNOWLEDGEMENTS
This work was supported in part by MEXT KAKENHI 21500411 and NIH/NCCAM 1R01AT006692-01A1. We thank T. Kaji for providing helpful comments on the statistical analysis.
REFERENCES
- Ananthakrisnan D, Ching R, Tencer A, Hansen ST, Sangeorzan BJ. Subluxation of Talocalcaneal Joint in Adults Who Have Symptomatic Flatfoot. J Bone Joint Surg Am. 1999;81:1147–1154. doi: 10.2106/00004623-199908000-00010. [DOI] [PubMed] [Google Scholar]
- Blackman AJ, Blevins JJ, Sangeorzan BJ, Ledoux WR. Cadaveric flatfoot model: ligament attenuation and Achilles tendon overpull. J Orthop Res. 2009;27:1547–1554. doi: 10.1002/jor.20930. [DOI] [PubMed] [Google Scholar]
- Blackwood CB, Yuen TJ, Sangeorzan BJ, Ledoux WR. The midtarsal joint locking mechanism. Foot Ankle Int. 2005;26:1074–1080. doi: 10.1177/107110070502601213. [DOI] [PubMed] [Google Scholar]
- Chi TD, Toolan BC, Sangeorzan BJ, Hansen ST., Jr. The lateral column lengthening and medial column stabilization procedures. Clin Orthop Relat Res. 1999;365:81–90. doi: 10.1097/00003086-199908000-00011. [DOI] [PubMed] [Google Scholar]
- Dyal CM, Feder J, Deland JT, Thompson FM. Pes planus in patients with posterior tibial tendon insufficiency: asymptomatic versus symptomatic foot. Foot Ankle Int. 1997;18:85–88. doi: 10.1177/107110079701800208. [DOI] [PubMed] [Google Scholar]
- Ferri M, Scharfenberger AV, Goplen G, Daniels TR, Pearce D. Weightbearing CT Scan of Severe Flexible Pes Planus Deformities. Foot Ankle Int. 2008;29:199–204. doi: 10.3113/FAI.2008.0199. [DOI] [PubMed] [Google Scholar]
- Greisberg J, Assal M, Hansen ST, Sangeorzan BJ. Isolated medial column stabilization improves alignment in adult-acquired flatfoot. Clin Orthop Relat Res. 2005;435:197–202. doi: 10.1097/01.blo.0000157658.17056.46. [DOI] [PubMed] [Google Scholar]
- Greisberg J, Hansen ST, Sangeorzan B. Deformity and degeneration in the hindfoot and midfoot joints of the adult acquired flatfoot. Foot Ankle Int. 2003;24:530–534. doi: 10.1177/107110070302400704. [DOI] [PubMed] [Google Scholar]
- Huang CK, Kitaoka HB, An KN, Chao EY. Biomechanical Evaluation of Longitudinal Arch Stability. Foot Ankle. 1993;14:353–357. doi: 10.1177/107110079301400609. [DOI] [PubMed] [Google Scholar]
- Imai K, Tokunaga D, Takatori R, Ikoma K, Maki M, Ohkawa H, et al. In vivo three-dimensional analysis of hindfoot kinematics. Foot Ankle Int. 2009;30:1094–1100. doi: 10.3113/FAI.2009.1094. [DOI] [PubMed] [Google Scholar]
- Imhauser CW, Abidi NA, Frankel DZ, Gavin K, Siegler S. Biomechanical evaluation of the efficacy of external stabilizers in the conservative treatment of acquired flatfoot deformity. Foot Ankle Int. 2002;23:727–737. doi: 10.1177/107110070202300809. [DOI] [PubMed] [Google Scholar]
- Karasick D, Schweitzer ME. Tear of the posterior tibial tendon causing asymmetric flatfoot: radiologic findings. AJR Am J Roentgenol. 1993;161:1237–1240. doi: 10.2214/ajr.161.6.8249732. [DOI] [PubMed] [Google Scholar]
- Kido M, Ikoma K, Imai K, Maki M, Takatori R, Tokunaga D, et al. Load response of the tarsal bones in patients with flatfoot deformity: in vivo 3D study. Foot Ankle Int. 2011a;32:1017–1022. doi: 10.3113/FAI.2011.1017. [DOI] [PubMed] [Google Scholar]
- Kido M, Ikoma K, Imai K, Maki M, Takatori R, Tokunaga D, et al. The accuracy and reproducibility of the original loading device of the foot and ankle for the CT scan. In Japanese. J Jpn Soc Surg Foot. 2011b;32:85–88. [Google Scholar]
- Kitaoka HB, Lundberg A, Luo ZP, An KN. Kinematics of the normal arch of the foot and ankle under physiologic loading. Foot Ankle Int. 1995;16:492–499. doi: 10.1177/107110079501600806. [DOI] [PubMed] [Google Scholar]
- Kitaoka HB, Luo ZP, An KN. Three-dimensional analysis of flatfoot deformity: cadaver study. Foot Ankle Int. 1998;19:447–451. doi: 10.1177/107110079801900705. [DOI] [PubMed] [Google Scholar]
- Kitaoka HB, Luo ZP, Kura H, An KN. Effect of foot orthoses on 3-dimensional kinematics of flatfoot: a cadaveric study. Arch Phys Med Rehabil. 2002;83:876–879. doi: 10.1053/apmr.2002.32681. [DOI] [PubMed] [Google Scholar]
- Mann RA. Surgery of the Foot and Ankle. 7th ed. Louis: Mosby, St; 1999. [Google Scholar]
- Manter JT. Distribution of compression forces in the joints of the human foot. Anat Rec. 1946;96:313–321. doi: 10.1002/ar.1090960306. [DOI] [PubMed] [Google Scholar]
- Mizel MS. The role of the plantar first metatarsal first cuneiform ligament in weightbearing on the first metatarsal. Foot Ankle. 1993;14:82–84. doi: 10.1177/107110079301400205. [DOI] [PubMed] [Google Scholar]
- Myerson MS. Adult acquired flatfoot deformity: treatment of dysfunction of the posterior tibial tendon. Instr Course Lect. 1997;46:393–405. [PubMed] [Google Scholar]
- Niki H, Ching RP, Kiser P, Sangeorzan BJ. The effect of posterior tibial tendon dysfunction on hindfoot kinematics. Foot Ankle Int. 2001;22:292–300. doi: 10.1177/107110070102200404. [DOI] [PubMed] [Google Scholar]
- Ochia RS, Inoue N, Renner SM, Lorenz EP, Lim TH, Andersson GB, et al. Three-dimensional in vivo measurement of lumbar spine segmental motion. Spine (Phila Pa 1976) 2006;31:2073–2078. doi: 10.1097/01.brs.0000231435.55842.9e. [DOI] [PubMed] [Google Scholar]
- Pedowitz WJ, Kovatis P. Flatfoot in the Adult. J Am Acad Orthop Surg. 1995;3:293–302. doi: 10.5435/00124635-199509000-00005. [DOI] [PubMed] [Google Scholar]
- Saltzman CL, Nawoczenski DA, Talbot KD. Measurement of the Medial Longitudinal Arch. Arch Phys Med Rehabil. 1995;76:45–49. doi: 10.1016/s0003-9993(95)80041-7. [DOI] [PubMed] [Google Scholar]
- Sangeorzan BJ, Mosca V, Hansen ST., Jr. Effect of calcaneal lengthening on relationships among the hindfoot, midfoot, and forefoot. Foot Ankle. 1993;14:136–141. doi: 10.1177/107110079301400305. [DOI] [PubMed] [Google Scholar]
- Sarrafian SK. Anatomy of the Foot and Ankle. 3rd ed. Philadelphia: Lippincott; 1983. [Google Scholar]
- Staheli LT, Chew DE, Corbett M. The longitudinal arch. A survey of eight hundred and eighty-two feet in normal children and adults. J Bone Joint Surg Am. 1987;69:426–428. [PubMed] [Google Scholar]
- Supple KM, Hanft JR, Murphy BJ, Janecki CJ, Kogler GF. Posterior tibial tendon dysfunction. Semin Arthritis Rheum. 1992;22:106–113. doi: 10.1016/0049-0172(92)90004-w. [DOI] [PubMed] [Google Scholar]
- Tareco JM, Miller NH, MacWilliams BA, Michelson JD. Defining flatfoot. Foot Ankle Int. 1999;20:456–460. doi: 10.1177/107110079902000711. [DOI] [PubMed] [Google Scholar]
- Thordarson DB, Schmotzer H, Chon J. Reconstruction with tenodesis in an adult flatfoot model. A biomechanical evaluation of four methods. J Bone Joint Surg Am. 1995;77:1557–1564. doi: 10.2106/00004623-199510000-00011. [DOI] [PubMed] [Google Scholar]
- Van Boerum DH, Sangeorzan BJ. Biomechanics and pathophysiology of flat foot. Foot Ankle Clin. 2003;8:419–430. doi: 10.1016/s1083-7515(03)00084-6. [DOI] [PubMed] [Google Scholar]
- Wanivenhaus A, Pretterklieber M. First tarsometatarsal joint: anatomical biomechanical study. Foot Ankle. 1989;9:153–157. doi: 10.1177/107110078900900401. [DOI] [PubMed] [Google Scholar]
- Younger AS, Sawatzky B, Dryden P. Radiographic assessment of adult flatfoot. Foot Ankle Int. 2005;26:820–825. doi: 10.1177/107110070502601006. [DOI] [PubMed] [Google Scholar]