Abstract
Spatial variation in childhood asthma and a recent increase in prevalence indicate that environmental factors play a significant role in the etiology of this important disease. Socioeconomic position (SEP) has been associated inversely and positively with childhood asthma. These contradictory results indicate a need for systematic research about SEP and asthma. Pathways have been suggested for effects of SEP on asthma at both the individual and community level. We examined the relationship of prevalent asthma to community-level indicators of SEP among 5762 children in 12 Southern California, using a multilevel random effects model. Estimates of community-level SEP were derived by summarizing census block group-level data using a novel method of weighting by the proportion of the block groups included in a community-specific bounding rectangle that contained 95% of local study subjects. Community characteristics included measures of male unemployment, household income, low education (i.e. no high school diploma), and poverty. There was a consistent inverse association between male unemployment and asthma across the inter-quartile range of community unemployment rates, indicating that asthma rates increase as community SEP increases. The results were robust to individual-level confounding, methods for summarizing census block group data to the community level, scale of analysis (i.e. community-level vs. neighborhood-level) and the modeling algorithm. The positive association between SEP and prevalent childhood asthma might be explained by differential access to medical care that remains unmeasured, by the hygiene hypothesis (e.g. lower SES may associate with higher protective exposures to endotoxin in early life), or by SEP acting as a proxy for unmeasured neighborhood characteristics.
Keywords: USA, neighborhood, childhood asthma, multi-level modeling, socioeconomic position, contextual factors
Introduction
Childhood asthma is now the leading chronic disease of children amongst industrialized countries (Centers for Disease Control and Prevention, 2003). In the United States, prevalent asthma rose from 3.4% to 5.5% between 1980 to 1996 in children 0–14 years of age (Mannino, Homa, Akinbami, Moorman, Gwynn, & Redd, 2002). The increase in prevalence, as well as large variation in prevalence between settings, within the U.S. and globally, has yet to be fully explained (Basagana, Sunyer, Kogevinas, Zock, Duran-Tauleria, Jarvis et al., 2004; Beasley, Ellwood, & Asher, 2003; Cagney & Browning, 2004; Federico & Liu, 2003; Juhn, Sauver, Katusic, Vargas, Weaver, & Yunginger, 2005; Pearce, Douwes, & Beasley, 2000; Pearce, Pekkanen, & Beasley, 1999; Redd, 2002). Similarly, the etiology of childhood asthma remains unclear. Current research is focused on both genetic and environmental factors. While genetic factors may predispose a child to asthma, geographical heterogeneity along with the rise in prevalence indicate that environmental factors probably contribute to the pathogenesis of asthma. There is a large literature examining associations of asthma with an individual’s housing characteristics, including home dampness, indoor allergens, environmental tobacco smoke, dietary factors and social position (Billings & Howard, 1998; Gold & Wright, 2005; Mielck, Reitmeir, & Wjst, 1996). Although findings remain mixed, collectively the studies suggest an effect of the built and social environment on asthma onset and severity.
Lower socioeconomic position (SEP) has been associated with severity of asthma in children and is linked with racial/ethnic disparities in the U.S. (Gold & Wright, 2005; Mielck, Reitmeir, & Wjst, 1996), although reasons for this relationship are not well understood. Lower SEP may act as a proxy for causal environmental effects, such as elevated air pollution exposure (O’Neill, Jerrett, Kawachi, Levy, Cohen, Gouveia et al., 2003) and poor housing conditions (Shapiro & Stout, 2002). Theoretically, geographic variation in asthma may be broken down into pathways operating at the individual level (i.e. “compositional” effects) and at the community level (i.e. “contextual” effects) (Diez Roux, 2002). Although compositional effects can be adequately controlled with individual-level variables, contextual effects imply independent or interactive contributions to health from the social and environmental place in which an individual lives or works (e.g. neighborhood crime that might result in increased stress and other behaviors not well measured by readily available individual-level variables). Research on the impact of the social environment on childhood asthma has traditionally focused on individual-level exposures, for example socioeconomic status of the family (King, Mannino, & Holguin, 2004; Mielck, Reitmeir, & Wjst, 1996; Ortega, Belanger, Paltiel, Horwitz, Bracken, & Leaderer, 2001; Pearce, Beasley, Burgess, & Crane, 1998; Wright, 2004); however, research about these compositional effects has not completely explained differences in asthma between communities. Potential contextual effects on asthma have been proposed (Gold & Wright, 2005), indicating the need for a multilevel approach to studies of childhood asthma epidemiology (Merlo, Chaix, Yang, Lynch, & Rastam, 2005). Multilevel models have only rarely been used to explore how the socioeconomic environment can impact asthma (Basagana, Sunyer, Kogevinas et al., 2004; Cagney & Browning, 2004), and few studies have focused specifically on childhood asthma (Juhn, Sauver, Katusic et al., 2005; Nepomnyaschy & Reichman, 2006). The purpose of this paper is to analyze the relationship between community socioeconomic characteristics and asthma among school children in southern California using a multilevel model.
Methods
Study Design and Subjects
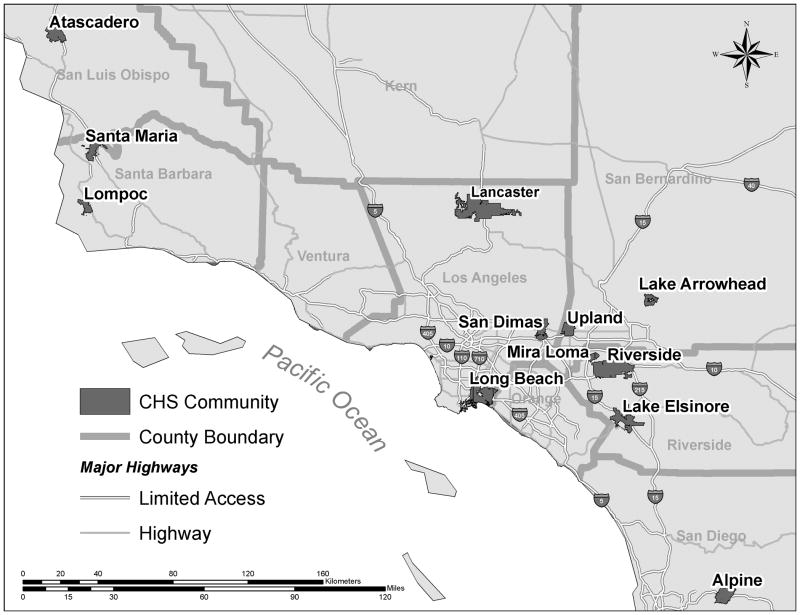
The Children’s Health Study (CHS) is a study of the long-term effects of air pollution and other risk factors on the respiratory health of children. The study originally comprised 12 southern California communities with 5762 participants (79% participation rate) (McConnell, Berhane, Gilliland, London, Islam, Gauderman et al., 2002b) (See Figure 1 for map of community and respondent locations). Children in the 4th, 7th and 10th grades were recruited in 1993 and 1996 and followed through high school graduation. Associations of asthma with housing characteristics, obesity, air pollution, family history and exercise have been previously described (Gauderman, Avol, Lurmann, Kuenzli, Gilliland, Peters et al., 2005; Gilliland, Berhane, Islam, McConnell, Gauderman, Gilliland et al., 2003; Kunzli, McConnell, Bates, Bastain, Hricko, Lurmann et al., 2003; London, James Gauderman, Avol, Rappaport, & Peters, 2001; McConnell, Berhane, Gilliland, Islam, Gauderman, London et al., 2002a; McConnell, Berhane, Gilliland et al., 2002b; McConnell, Berhane, Yao, Jerrett, Lurmann, Gilliland et al., 2006). A detailed description of the selection of communities, subject recruitment, and survey methods to assess demographic, household, activity, and baseline medical characteristics has also been reported (Peters, Avol, Navidi, London, Gauderman, Lurmann et al., 1999). The current analysis is the first examination of the contextual effects of SEP on asthma in the CHS.
Figure 1.
CHS communities and distribution of participants.
Written informed consent was obtained from a parent or legal guardian for all study subjects. The University of Southern California’s institutional review board approved the study protocol.
Dependent Variables
A questionnaire was completed at study entry by parents or legal guardians of subjects to collect information about children’s baseline characteristics. The main outcome of interest was lifetime doctor-diagnosed asthma and valid data was obtained for 96.8% of participants (N=5581). By using lifetime asthma as a dependent variable, our results might be biased if participants of lower SEP did not have access to health care comparable with subjects of higher SEP. Thus, we performed a sensitivity analysis that substituted severe wheeze (i.e. ever wheezed for 3+ days/week for more than 1 month, or shortness of breath with wheezing, or awakened by wheezing, or emergency room/overnight hospital visit for wheezing) as the dependent variable. Wheeze is a common symptom of asthma that is more easily recognized by parents without a doctor diagnosis and is more specific than cough (Warren, 1999).
Individual Variables
Socioeconomic position and other demographic, medical and home environmental exposures have been examined in the CHS with respect to childhood asthma (Gauderman, Avol, Lurmann et al., 2005; Gilliland, Berhane, Islam et al., 2003; Peters, Avol, Navidi et al., 1999). Variables of interest here include age of the child (centered on 10 years of age), race/ethnicity, gender, height, age- and sex-adjusted body mass index below the 10th percentile or in the 90th percentile, cohort group (defined by year and subject’s grade at enrollment: 1993 in 4th, 7th or 10th grade or 1996 in 4th grade), current vitamin use, hay fever symptoms in the last 12 months, current medical insurance coverage and parental history of asthma. Parental education (12 grades or less, some college, and college and/or graduate education) was used as an indicator of individual-level SEP. Housing characteristics included air conditioning, gas stove, carpet in subject’s bedroom, any current daily smokers, pests, plants, pets, water damage or mildew in the home. Residential distance to the nearest freeway or major road (i.e. indicators of traffic-related pollution) and in utero tobacco smoke exposure have been previously associated with increased risk for prevalent asthma in previous CHS studies (Gauderman, Avol, Lurmann et al., 2005; Gilliland, Li, & Peters, 2001; McConnell, Berhane, Yao et al., 2006). In sensitivity analyses, we examined these measures as potential confounders but neither significantly changed the contextual effects of primary interest to this analysis. We also evaluated the effect of number of siblings as an indicator of exposure to early life infections or related exposures (Ramsey & Celedon, 2005).
Community Socioeconomic Variables
Estimates of community-level socioeconomic characteristics were calculated by aggregating data associated with census block groups where study subjects lived. Data from the U.S. 1990 census was used to estimate community conditions at baseline since study enrollment began in 1993. Because subjects were recruited through schools, residential locations cluster together; therefore, to compensate for clustering of study subjects, a Geographic Information System was used to derive community-level estimates weighted by the proportion of the census block groups included in a community-specific bounding rectangle that contained 95% of local study subject residences (Tatalovich, Wilson, Milam, Jerrett, & McConnell, 2006).
Characteristics of interest at the community level have previously been suggested as measures of SEP that were associated with health effects (Haan, Kaplan, & Camacho, 1987; Jin, Shah, & Svaboda, 1994; Juhn, Sauver, Katusic et al., 2005; Wissow, Gittelsohn, Szklo, Starfield, & Mussman, 1988). They included community measures of median household income, proportion of respondents with low education (i.e. no high school diploma), the unemployment-to-population ratio (UPR) for males (i.e. number employed divided by total population of working age), and percent living in poverty (U.S. Census Bureau, 1992). Male unemployment (as opposed to general or female unemployment) was considered in this study since the relationship between employment and health is more apparent for males than for females during the period prior to study baseline (Jin, Shah, & Svaboda, 1994; Sorensen & Verbrugge, 1987). In a sensitivity analysis, female and total unemployment were substituted for male unemployment.
Hispanic ethnicity was of interest as a potential effect modifier of the association between community SEP and asthma. In the U.S., Mexican Americans, particularly those born outside of the U.S., have been shown to have the lowest low rates of asthma compared with other ethnic groups, (Arif, Delclos, Lee, Tortolero, & Whitehead, 2003; Holguin, Mannino, Anto, Mott, Ford, Teague et al., 2005; National Center for Health Statistics, 2002). Hispanic Americans also have less access to health care, lower median family income and more children living in poverty than other ethnicities in the U.S. (Dougherty, Meikle, Owens, Kelley, & Moy, 2005; Public Policy Institute of California, 2001). The contradiction that some foreign-born Hispanic populations have lower SEP but better health outcomes than other ethnic populations in the United States, including asthma, is known as the Latino Paradox. For example, in a multi-ethnic cross-sectional study of adults in Chicago, foreign-born Latinos were shown to have less prevalent asthma than subjects of other ethnicities, including U.S.-born Latinos, when living within immigrant neighborhoods (Cagney, Browning, & Wallace, 2005).
Statistical Analysis
A multilevel random effects model was designed to relate lifetime asthma at baseline to community-level socioeconomic characteristics adjusting for individual-level covariates. Previous statistical analyses of CHS data have utilized similar models to examine community-level effects (Berhane, Gauderman, Stram, & Thomas, in press; Gilliland, Berhane, Rappaport, Thomas, Avol, Gauderman et al., 2001; Hoffman, Gilliland, Eley, Harlan, Stephenson, Stanford et al., 2001; McConnell, Berhane, Gilliland, Molitor, Thomas, Lurmann et al., 2003).
A hierarchical logistic regression model with random effects for the 12 CHS communities was fitted in SAS using the GLIMMIX procedure with a binomial distribution assumption and a logit link (SAS Institute Inc., 2002). Random effects accounted for community lifetime asthma unexplained by individual- or community-level risk factors. To ascertain the impact of adjusting for specific individual-level covariates on community-level effects, six models featuring different levels of adjustment were tested (refer to Table 3 footnotes). All models included key demographic variables (age, race and ethnicity, gender, and cohort group), and model 1 was adjusted only for these variables. Model 2 added parental education, which was included in subsequent models so that these results would be adjusted for individual SEP. Model 3 added medical insurance to account for possible diagnostic bias resulting from differential access to care. Model 4 adjusted for a total of 21 covariates that follow the adjustment used by Peters et al. in their original CHS study (Peters, Avol, Navidi et al., 1999). Model 5 added census block group population density. Finally, model 6 derived a parsimonious model by entering all 22 covariates from model 5 into a backwards manual stepwise regression using a cutoff value of p=0.10. We then attempted to re-enter variables excluded during this process using the same cutoff value. The resultant model contained covariates for cohort group, African-American race, gender, age, age- and sex-specific body mass index below the 10th percentile or in the 90th percentile, parental education, medical insurance coverage, parental history of asthma, hay fever, plants in the home, pets in the home, gas stove in the home and mildew in the home. Estimates derived for individual-level covariates represented the adjusted log odds ratio for lifetime asthma at baseline.
Table 3.
Odds ratio for community-level socioeconomic characteristics and unexplained lifetime asthma across the inter-quartile range (models 1–6).
| Community Socioeconomic Parameter |
Model 1a (n=5364) | Model 2b (n=5364) | Model 3c (n=5263) | Model 4d (n=3687) | Model 5e (n=3481) | Model 6f (n=4092) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR IQR | 95% CI | P | OR IQR | 95% CI | P | OR IQR | 95% CI | P | OR IQR | 95% CI | P | OR IQR | 95% CI | P | OR IQR | 95% CI | P | |
| Median Income | 1.01 | 0.88, 1.15 | 0.93 | 0.99 | 0.87, 1.14 | 0.92 | 0.98 | 0.86, 1.13 | 0.8 | 0.94 | 0.83, 1.06 | 0.32 | 0.93 | 0.82, 1.07 | 0.3 | 0.98 | 0.89, 1.09 | 0.76 |
| % Poverty | 0.89 | 0.72, 1.09 | 0.26 | 0.92 | 0.74, 1.14 | 0.42 | 0.94 | 0.75, 1.17 | 0.55 | 1.04 | 0.84, 1.28 | 0.75 | 1.03 | 0.81, 1.31 | 0.83 | 0.97 | 0.82, 1.16 | 0.75 |
| % Male Unemployment | 0.81 | 0.73, 0.90 | <0.01 | 0.83 | 0.73, 0.93 | <0.01 | 0.83 | 0.74, 0.95 | <0.01 | 0.88 | 0.77, 1.01 | 0.06 | 0.86 | 0.75, 0.99 | 0.03 | 0.88 | 0.78, 0.99 | 0.03 |
| % Low Education | 0.92 | 0.78, 1.09 | 0.33 | 0.93 | 0.79, 1.11 | 0.44 | 0.95 | 0.8, 1.14 | 0.6 | 0.96 | 0.82, 1.13 | 0.64 | 0.95 | 0.75, 1.15 | 0.61 | 0.96 | 0.84, 1.10 | 0.53 |
Model 1 adjusted for community, age, race, gender and cohort group.
Model 2 adjusted as in model 1 plus parental education.
Model 3 adjusted as in model 2 plus medical insurance coverage.
Model 4 adjusted as in model 3 plus air conditioning in home, gas stove in home, carpet in child’s room, parental history of asthma, any smokers in the home, hay fever in child, pest in home, plants in home, pets in home, regular vitamin use, body mass index, height, water damage in home and mildew in home.
Model 5 adjusted as in model 4 plus census block group population density.
Model 6 adjusted for community, age, African-American race, gender, cohort group, parental education, medical insurance coverage, gas stove in home, parental history of asthma, hay fever in child, plants in home, pets in home, body mass index, and mildew in home.
Because the SAS procedure GLIMMIX uses pseudo-likelihood estimations which can underestimate fixed effects and standard errors, the HLM software (Scientific Software International Inc., 2005) was used in a sensitivity analysis to replicate all of the main analyses using single-stage mixed effects models capable of producing exact solutions. The patterns of effects were similar for models in HLM, so we only report results from the SAS procedure GLIMMIX.
When assigning contextual exposures to study subjects, the spatial scale and geographic zone used to configure the unit of analysis can influence results generated from analysis due to changes in population characteristics; this is known as the modifiable areal unit problem (MAUP) (Jerrett & Finkelstein, 2005). To confirm that our results were not subject to such bias due to our community-level apportionment of socioeconomic characteristics, all iterations of modeling with the GLIMMIX procedure were rerun using a single-stage design which replaced community-specific measures of SEP with census block group measures specific for individual subjects. Individual-level covariates were modeled simultaneously with estimators of smaller neighborhood socioeconomic characteristics, with clustering on the census block group to adjust the estimate of variance for clustering of study subjects within communities (Williams, 2000). Models were run with STATA software using the cluster function (Stata Corporation, 2003). Because the pattern of effects was similar using both approaches, we only present results derived from the SAS procedure GLIMMIX.
Our method for measuring community-level socioeconomic characteristics (i.e. 95% minimum bounding rectangle) could have introduced bias if contextual effects were not clustered by 95% of population density; thus, the second-stage analysis was repeated using two alternative methods of measurement: (1) estimates from specific census block groups containing subjects were weighted by the proportion of the community sample living within those census block groups, and (2) data pertaining to all census block groups that contained study subjects were summarized, unweighted (Tatalovich, Wilson, Jerrett, Milam, & McConnell, 2006). Our results were not affected by the configuration of this measurement so only results utilizing the 95% minimum bounding rectangle are presented.
Results
Individual-level covariates in the parsimonious model revealed a number of significant associations with lifetime asthma (Table 1). African-American race, age- and sex-adjusted body mass index and male gender were positively associated with lifetime asthma. Mildew and pets in the home were positively associated with asthma, while having plants in the home was inversely associated. Having a parental history of asthma and symptoms of hay fever in the last year both increased the odds for asthma. Subjects with current medical insurance coverage were more likely to be asthmatic at study baseline. Finally, a measure of family SEP, parental education, suggested a positive association between asthma and low SEP, consistent across two categories indicating education below college graduation compared to college graduates (non-significant).
Table 1.
Individual-level associations for lifetime asthma (model 6).
| Risk Factor | N (%)a | OR | 95% CI | p-value |
|---|---|---|---|---|
| Subject Characteristics | ||||
| BMIb | ||||
| Below 10th percentile | 551 (10.69) | 0.75 | 0.54, 1.03 | 0.08 |
| 10th–90th percentile | 4129 (80.13) | - | - | - |
| 90th percentile | 473 (9.18) | 1.43 | 1.06, 1.93 | 0.02 |
| African-American Race | 256 (4.59) | 1.87 | 1.23, 2.86 | <0.01 |
| Male Gender | 2712 (48.59) | 1.95 | 1.34, 1.95 | <0.01 |
| Age (years)c | - | 0.87 | 0.70, 1.07 | 0.18 |
| Hay feverd | 909 (17.64) | 2.37 | 1.92, 2.91 | <0.01 |
| Medical Care & SEP | ||||
| Medical insurance coverage | 4603 (84.33) | 1.59 | 1.17, 2.18 | <0.01 |
| Parental education | ||||
| High school or less | 1894 (35.02) | 1.27 | 0.97, 1.65 | 0.08 |
| Some college | 2351 (43.47) | 1.22 | 0.96, 1.56 | 0.10 |
| College or greater | 1163 (21.51) | - | - | - |
| Co-exposures | ||||
| Mildew in home | 1514 (28.10) | 1.33 | 1.09, 1.62 | <0.01 |
| Plants in home | 2005 (36.49) | 0.79 | 0.65, 0.96 | 0.02 |
| Pets at home | 4356 (78.05) | 1.32 | 1.02, 1.70 | 0.04 |
| Gas stove in home | 4323 (79.03) | 1.22 | 0.97, 1.53 | 0.09 |
| Family History | ||||
| Parental history of asthmae | 1007 (19.56) | 3.67 | 1.11, 4.45 | <0.01 |
Subject number varied due to missing values
Age- and sex-adjusted body mass index
Age was centered on 10 years of age
Hay fever symptoms in the last 12 months
Medical diagnosis of asthma in either biological parent
Characteristics of the 12 study communities are shown in Table 2. Across the 12 communities, median income ranged from $31,938 in Long Beach to $57,815 in Upland (mean: $39,498; standard deviation: $7,003). Percent poverty ranged from 14.2% in Santa Maria to 3.8% in Upland (mean: 9.2%; standard deviation: 3.2). Percent male unemployment ranged from 5.5% in Santa Maria to 2.2% in Atascadero (mean: 4.5%; standard deviation: 1.1). Finally, percent low education ranged from 29.5% in Santa Maria to 9.9% in Lake Arrowhead (mean: 20.1%; standard deviation: 5.9). There was medium-to-high correlation between these four variables, in general; male unemployment was most highly correlated with percent poverty (r2=0.54) and least correlated with median income (r2=0.26). White Non-Hispanic was the majority race/ethnicity in all communities except Santa Maria, where Hispanic race/ethnicity was most prevalent. Long Beach was the most ethnically diverse community, while Lake Arrowhead was the least diverse (88.4% White). Prevalence of asthma was highest in Atascadero (21.5%) and lowest in Mira Loma (11.5%).
Table 2.
Characteristics of CHS communities
| Community | N | Crude Asthma Prevalence (%) |
Male Unemployment (%)a |
Median Family Income ($)a |
Education Below High School Diploma (%)a |
Below Poverty (%)a |
White Non- Hispanic |
Race/Ethnicity (%)a | Asian | Other | CHS Participants of Hispanic Ethnicity (%) |
CHS Participants with Medical Insurance Coverage (%) |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hipsanic | African American |
||||||||||||
| Alpine | 478 | 13.39 | 4.38 | 39,295 | 18.11 | 8.51 | 82.19 | 9.99 | 1.31 | 1.59 | 4.93 | 16.08 | 88.06 |
| Atascadero | 404 | 21.53 | 2.18 | 34,739 | 16.09 | 7.85 | 84.47 | 8.32 | 2.13 | 1.13 | 3.96 | 14.22 | 87.98 |
| Lake Elsinore | 483 | 14.49 | 4.51 | 37,283 | 23.41 | 8.79 | 70.44 | 16.27 | 2.56 | 1.73 | 8.99 | 27.42 | 82.33 |
| Lake Arrowhead | 516 | 13.95 | 4.61 | 42,095 | 9.87 | 7.42 | 88.39 | 8.01 | 0.65 | 0.86 | 2.09 | 18.32 | 84.18 |
| Lancaster | 450 | 15.78 | 4.74 | 41,089 | 18.67 | 9.19 | 65.58 | 14.99 | 6.91 | 3.58 | 8.94 | 28.29 | 88.31 |
| Lompoc | 472 | 12.50 | 5.07 | 35,024 | 18.60 | 12.19 | 52.31 | 21.74 | 6.51 | 5.05 | 14.39 | 26.56 | 88.09 |
| Long Beach | 469 | 13.22 | 5.46 | 31,938 | 25.87 | 13.11 | 33.30 | 24.08 | 13.35 | 14.31 | 14.96 | 22.88 | 85.56 |
| Mira Loma | 460 | 11.52 | 4.99 | 41,521 | 26.96 | 6.87 | 57.70 | 23.70 | 2.68 | 2.24 | 13.66 | 41.09 | 78.34 |
| Riverside | 518 | 13.71 | 5.42 | 34,984 | 22.51 | 12.35 | 40.72 | 26.80 | 9.10 | 5.11 | 18.27 | 40.58 | 80.16 |
| San Dimas | 459 | 18.08 | 3.54 | 44,799 | 19.43 | 5.54 | 59.57 | 20.80 | 5.46 | 5.90 | 8.27 | 31.47 | 87.86 |
| Santa Maria | 451 | 13.53 | 5.53 | 33,390 | 29.50 | 14.21 | 27.73 | 38.95 | 1.86 | 5.21 | 26.25 | 62.72 | 68.10 |
| Upland | 421 | 14.01 | 2.92 | 57,815 | 11.85 | 3.81 | 68.97 | 12.70 | 3.81 | 8.42 | 6.11 | 16.51 | 92.33 |
|
| |||||||||||||
| All Communities | 5581 | 14.55 | 4.45 | 39,498 | 20.07 | 9.15 | 60.95 | 18.86 | 4.69 | 4.59 | 10.90 | 28.33 | 84.28 |
Data obtained from U.S. Census 1990.
Across all six models, there was an inverse association between male unemployment and lifetime asthma (Table 3). This association was statistically significant at the 0.05 level for all models except for the highly adjusted model 4, where missing observations reduced the sample size by 40%. Results from the parsimonious model showed an odds ratio for lifetime asthma of 0.88 (95% CI 0.78, 0.99) across the inter-quartile range (IQR) of communities and 0.71 (95% CI 0.52, 0.97) across the full range (data not shown). When stratified by Hispanic ethnicity, the inverse effect for % male unemployment was slightly stronger amongst Hispanics (OR IQR 0.85, 95% CI 0.67, 1.08), while it remained stable amongst non-Hispanics (OR IQR 0.88, 95% CI 0.75, 1.03), but this difference was not statistically significant. An inverse association was also found between % male unemployment and severe wheeze in the parsimonious model (OR IQR 0.93, 95% CI 0.83, 1.04). In general, the pattern of effects for all community socioeconomic characteristics from models examining severe wheeze was similar to the main results (data not shown). There was no effect for female unemployment (OR IQR 0.99, 95% CI 0.82, 1.20), while the effect for total unemployment was very similar to that for male unemployment, but with wider confidence intervals (OR IQR 0.89, 95% CI 0.76, 1.05). This suggests that it is the variation in male unemployment that is responsible for the results we have observed.
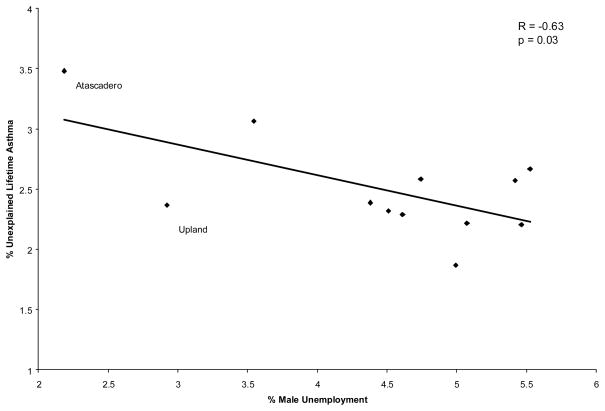
A scatter plot of community unexplained lifetime asthma versus percent male unemployment revealed two outliers, Atascadero and Upland (Figure 2). Sensitivity analyses were performed to ascertain how estimates might change if one or the other community was excluded. When Atascadero was removed from the model, the association between community male unemployment and prevalent asthma was diminished and rendered non-significant (OR IQR 0.94, 95% CI 0.80, 1.10). When Upland was removed, the original association became more negative and remained statistically significant (OR IQR 0.84, 95% CI 0.74, 0.96). Both communities are points of influence; however, since each community in the survey represents approximately 500 individuals, we cannot justify excluding these communities in the analysis.
Figure 2.
Scatter plot of unexplained lifetime asthma and percent male unemployment across study communities (n=12); Atascadero and Upland are influential communities.
Missing values in our dataset reduced our sample by 26.7% in the parsimonious model. Missing cases were generally from households with significantly less education, lower socioeconomic status, fewer air conditioners and pets, and less mildew, and were more likely to be Hispanic. Missing subjects also tended to be from communities with greater average population density (data not shown). This suggests that we were missing subjects from the lower end of the SEP distribution in our analysis. In a sensitivity analysis, we included subjects with missing data in the parsimonious model using an indicator variable for individuals with missing values for each covariate (White & Thompson, 2005). When covariates with missing data are correlated to the outcome of interest, this method can produce biased estimators; in our case, relevant covariates were generally weakly correlated to lifetime asthma (data not shown). After this adjustment, the OR IQR for community percent male unemployment was similar to the original estimate (OR IQR 0.87, 95% CI 0.78, 0.98), suggesting that missing values did not bias our results.
Discussion
We evaluated the association between community-level SEP and asthma, after controlling for individual-level effects. There was lower prevalence of asthma in communities with contextual markers of low SEP, which was significant for community average male unemployment. Percent poverty and low education were less strongly protective. The results were robust to methods for summarizing census block group data to the community level (i.e. 95% bounding rectangle vs. weighted or unweighted methods), the scale of analysis (i.e. community-level vs. census block group-level), confounding by compositional factors, and the modeling algorithm.
Medical insurance coverage was strongly associated with asthma at the individual level. However, access to medical care and disparities in quality of care may vary both within and between communities (Gold & Wright, 2005), for instance, depending on the relative location of medical facilities (Garrett, 1997; McLafferty & Grady, 2004; McLafferty, 2003). Therefore, communities and neighborhoods with relatively lower access to care may have more undiagnosed cases of asthma than places with easy access to care. The inverse effect for low community SEP could be explained if lower rates of asthma resulted from reduced access to health care in low SEP populations or from less accurate self-reporting of doctor-diagnosed asthma by low SEP parents. With respect to the former, by adjusting for individual-level medical insurance coverage we would expect to confirm that the observed association is not due to access to health services (Callahan & Cooper, 2005; Kempe, Beaty, Crane, Stokstad, Barrow, Belman et al., 2005). While insurance coverage was a predictor of prevalent asthma in models 3 through 6, adjustment for insurance coverage in model 3 did not confound the association observed between community male unemployment and asthma in model 2 (see Table 3). Due to the cross-sectional design of this study, this may indicate that children diagnosed with asthma prior to study baseline were more likely to obtain medical insurance subsequently, but it is also possible that the variable about insurance coverage did not capture complex differences in access to and the quality of care. In our study, parents were only asked “does this child have any health plan or health insurance?”, at study entry; thus, in communities with higher unemployment, such an indicator may not measure increased interruptions in continuity of care that may be brought on by periods of unemployment within families, and it will not account for under-diagnosis that may occur among children with less comprehensive health plans (e.g. Medicaid) in such families (Vivier, 2005). Therefore, reduced access to diagnostic care in communities with high unemployment could explain the lower rates of asthma. While we did not have an independent measure of insurance coverage within communities, we averaged subject-level data on insurance coverage by community and examined its relationship with male unemployment. There was a significant inverse association, meaning places with higher unemployment had lower insurance coverage (r2=0.60; p=0.04). Male unemployment might therefore be a proxy for entire communities with reduced access to care (e.g. there may be fewer specialists, who may be more likely to diagnose health problems). That the association between male unemployment and severe wheeze was slightly less negative than the association for lifetime asthma also supports the idea that differential access to medical insurance may partially explain our results.
Another possible explanation for the observed inverse effect for low SEP is the hygiene hypothesis (Gold & Wright, 2005). This hypothesis suggests that reduced infectious challenge in early childhood may contribute to the development and severity of asthma as a result of failure to develop immunological tolerance (Ramsey & Celedon, 2005). While the biological plausibility of this hypothesis remains under study (Borchers, Keen, & Gershwin, 2005; Bufford & Gern, 2005), it would predict that lower rates of asthma might be expected in communities with higher unemployment, if children in these communities were more likely to be exposed to infectious challenges. Recent evidence from the International Study of Asthma and Allergies in Childhood (ISAAC) has shown a general trend of highly developed countries having relatively more prevalent asthma than less developed countries (Beasley, Ellwood, & Asher, 2003), which generally have greater childhood communicable disease burden (Lopez, 2005; Murray & Lopez, 1997). Within countries, lower rates of asthma have been observed among children growing up in close proximity to farm animals, suggesting a protective effect of early childhood exposure to endotoxin and other bacterial compounds (Von Ehrenstein, Von Mutius, Illi, Baumann, Bohm, & von Kries, 2000). Strachan first suggested this hypothesis after observing that having a greater number of older siblings was associated with reduced prevalence of atopy in children (Strachan, 1989), and this initial observation has been followed-up by other studies which show exposure to siblings leads to increased exposure to allergens and viral infection for children (Karmaus & Botezan, 2002; Randi, Altieri, Chatenoud, Chiaffarino, & La Vecchia, 2004). As a sensitivity analysis, we further adjusted our parsimonious model for number of siblings in the first stage of model 6. At the individual-level, each additional sibling conferred a reduction in risk for asthma (OR 0.88; 95% CI 0.81, 0.95), causing a slight weakening in the community-level effect for male unemployment (OR IQR 0.89, 95% CI 0.79, 1.00). This attenuation of the effect of community SEP is what would be expected if the hygiene effect were partially responsible for our community-level results.
Cagney et al. (2004) found no association between a measure of community socioeconomic deprivation and asthma, but they did observe that greater collective efficacy within communities was protective. Collective efficacy is defined as shared expectations and effort that lead to beneficial community resource (Cagney & Browning, 2004). Our study focused on using measures of community deprivation, yet an emerging literature on measures of social capital, including collective efficacy, indicates that deprivation measures may not completely explain the mechanisms that potentially exist where contextual effects of SEP occur (Sampson, Morenoff, & Earls, 1999). The inverse effect for male unemployment was stronger amongst Hispanics than non-Hispanics (difference not statistically significant), and communities with a greater proportion of Hispanic subjects tended to be communities with higher male unemployment (r2= 0.35; p=0.04), results which are suggestive of the Latino Paradox. While the main effect for Hispanic ethnicity was not statistically significant in our analysis (results not shown), the slightly more protective effect of high unemployment amongst the Hispanic strata suggests that communities of Hispanics have a collective advantage against asthma compared to communities of other racial-ethnic groups, in the context of low SEP. A protective effect of social capital on markers of health in Hispanic-American communities has been suggested as an explanation for this trend (Cagney, Browning, & Wallace, 2005; Denner, Kirby, Coyle, & Brindis, 2001).
The environmental justice literature has highlighted a spatial relationship between communities of color and exposure to harmful air pollutants in southern California (Morello-Frosch, Pastor, Porras, & Sadd, 2002), which suggests that associations between community SEP and asthma may be driven by measures of residential segregation rather than deprivation (Morello-Frosch & Lopez, 2006). In a sensitivity analysis, we tested measures of community racial composition and neighborhood stability derived from the U.S. 1990 census as measures of SEP which may relate to segregation. We found no main effects of these variables on asthma prevalence, nor did they confound the association between community male unemployment and asthma.
In this study, we used the UPR to represent unemployment, as opposed to the unemployment rate (UR). The UPR is thought to better capture unemployment in populations featuring discouraged workers, who are not considered a part of the labor force and are thus excluded from the UR (Jones & Riddell, 1999). Given the economic recession in the United States in the late 1980s and early 1990s, which is the period during which lifetime asthma would have occurred in our cohort, the UPR may be a more appropriate measure than the UR in our study. Furthermore, southern California has a disproportionately high number of undocumented immigrants who make up the actual labor force (U.S. Census Bureau, 1994). Undocumented immigrants may be less likely to report that they are actively seeking work on the U.S. Census, thus excluding them from Census estimates of the labor force which are used as the denominator for the UR. In contrast, the UPR includes all individuals 16 years of age or older in the denominator and may be more sensitive to communities in our study which have a smaller or larger presence of undocumented immigrants. In a sensitivity analysis, we substituted the UR (U.S. Census Bureau, 1992) into model 6 (in Table 3) and observed a similar but a slightly diminished relative risk for the effect of community unemployment on prevalent asthma (RR IQR 0.91, 95% CI 0.83–1.00). The stronger protective effect that we observe when the UPR was used may reflect lower rates of asthma in communities with undocumented immigrants from Mexico, a population with especially low rates of asthma, in spite of their SEP (i.e. the Latino Paradox) (Holguin, Mannino, Anto et al., 2005). Alternatively, it may reflect under-diagnosis of asthma in communities hit hardest by economic recession and subsequent joblessness (i.e. discouraged workers).
Although there is considerable interest in the role of SEP in geographic differences in rates of asthma (Federico & Liu, 2003; Gold & Wright, 2005), there has been relatively little systematic study of this issue compared to investigation of other risk factors. Few studies have explored the effects of SEP on childhood asthma using a multilevel model. Juhn et al. (2005) found a borderline significant positive association between mean family income (assigned to the subject’s census tract at birth) and incident asthma (Juhn, Sauver, Katusic et al., 2005). Their results are not completely comparable to ours because of differences in assignment of community of residence (i.e. at birth vs. at study entry) and individual-level adjustment (i.e. very reduced number of risk factors vs. comprehensive in ours). While results for mean family income were inconclusive in our analysis, the similarity in the relationship between SEP and asthma supports the findings here. In contrast, Nepomnyaschy and Reichman (2006) observed a positive association between asthma at a young age and residence in census tracts with higher rates of renter-occupied housing and vacancies, a marker for low SEP neighborhoods (Nepomnyaschy & Reichman, 2006). There are many differences in study design and sample composition, but their results with prevalent asthma suggest the opposite relationship between SEP and asthma than we observed. Basagana et al. (2004) also found a positive association between dichotomous measures of low SEP and adult asthma in community settings across Europe, Australia, New Zealand and the US (Basagana, Sunyer, Kogevinas et al., 2004). Results presented in this paper contribute to the growing body of evidence suggesting a role for SEP in explaining geographic patterns of asthma. The direction of this SEP-asthma relationship, however, still seems unclear, with divergent findings emerging from different scales of analysis, underlying populations and study designs.
We found a contrast between the individual- and community-level effects of SEP on asthma. While we observed a protective relationship between high unemployment and asthma at the community level, asthma rates were higher in families with lower parental education. Other studies have generally found increased rates of asthma associated with individual-level effects of low SEP (Gold & Wright, 2005; Mielck, Reitmeir, & Wjst, 1996), results which are consistent with the observed increased rates of asthma associated with individual-level insurance coverage and lower parental education in our study. In contrast to our observation of protective community-level effects of lower SEP, increased rates of asthma have been observed in impoverished inner cities in the U.S. (Federico & Liu, 2003). Contextual factors have been proposed to explain the increased rates of asthma observed in inner cities, including the absence of community facilities (e.g. park space, fast food restaurants) that could affect health behaviors such as exercising and consuming a high fat diet, resulting in elevated risks for asthma (Gold & Wright, 2005). Stress arising from conditions in low SEP communities (e.g. poor housing, violence, unemployment) also might have a role in asthma exacerbation and increased asthma rates (Chen, Hanson, Paterson, Griffin, Walker, & Miller, 2006; Liu, Coe, Swenson, Kelly, Kita, & Busse, 2002; Marmot, 2001; Wright, Mitchell, Visness, Cohen, Stout, Evans et al., 2004; Wright, Rodriguez, & Cohen, 1998). The range of contextual SEP in our communities did not represent the extremes found in inner cities, so associations with SEP in inner cities are not directly analogous for our study, nor could our results be expected to be generalizable to the inner city setting.
Estimates of contextual effects may be underestimated in our analysis. We used 1990 Census data to derive community-level socioeconomic characteristics, and this may have resulted in non-differential misclassification bias in estimating the true community-level characteristics for the time our study was conducted in 1993. Furthermore, the measurement of contextual effects can be biased if there is collinearity with compositional effects that are included in the same model (Oakes, 2004). In our analysis, we adjusted for some covariates at the individual-level (e.g. hay fever, medical insurance coverage) that may also be on the causal pathway for community-level SEP effects; in effect, we may have over-adjusted the between-community differences in asthma, overstating the reduction in between-community variability in unexplained asthma. We evaluated the effect of removal of medical insurance coverage and hay fever from the first stage of analysis and estimates of contextual effects grew stronger for all four community socioeconomic characteristics, but the changes were small. For example, the odds ratio across the IQR for community male unemployment in model 6 after excluding hay fever decreased from 0.88 to 0.85 (95% CI 0.76, 0.95). Thus, the true effect for male unemployment may be stronger than we measured, and observed effects for other community-level characteristics, and their statistical significance, may also be attenuated by our adjustment for covariates potentially on the causal pathway.
We sought to explain residual differences in between-community asthma prevalence with community indicators of SEP in a population-based cohort. In doing so, we used a multilevel modeling framework to estimate contextual effects which account for random effects at the community-level, as well as for potential confounders at the individual level. While many studies about contextual effects use jurisdictional boundaries to define community characteristics, we used a novel method of spatial and statistical analysis to derive characteristics of community SEP which better reflect the residential locations which subjects inhabit. Our results reveal a consistent protective effect for community unemployment, one that persisted even with the inclusion of many individual risk factors and with smaller units of analysis (i.e., census block groups). We have hypothesized some mechanisms that may explain this association. In general, unemployment has been associated with risky health behaviors and worse health outcomes (Catalano, 1991; Ferrie, Martikainen, Shipley, Marmot, Stansfeld, & Smith, 2001; Jerrett, Eyles, & Cole, 1998). Although our results do not fall into this general pattern, other research has indicated a protective effect of lower SEP at the community scale. Future studies may examine the impact that type of medical insurance coverage has on contextual effects of SEP. Further investigation into the links between contextual SEP and asthma is warranted.
Acknowledgments
This study was supported by the National Institute of Environmental Health Science (Grant 5R03ES014046-02) and the Canadian Institutes of Health Research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Mr. Ketan Shankardass, University of Southern California Los Angeles, CA UNITED STATES
Rob S McConnell, Email: rmcconne@usc.edu, University of Southern California.
Joel Milam, Email: milam_j@ccnt.usc.edu, University of Southern California.
Kiros Berhane, Email: kiros@usc.edu, University of Southern California.
Zaria Tatalovich, Email: tatalovi@usc.edu, University of Southern California.
John P Wilson, Email: jpwilson@usc.edu, University of Southern California.
Michael Jerrett, Email: jerrett@usc.edu, University of Southern California.
References
- Arif AA, Delclos GL, Lee ES, Tortolero SR, Whitehead LW. Prevalence and risk factors of asthma and wheezing among US adults: an analysis of the NHANES III data. Eur Respir J. 2003;21(5):827–833. doi: 10.1183/09031936.03.00054103a. [DOI] [PubMed] [Google Scholar]
- Basagana X, Sunyer J, Kogevinas M, Zock JP, Duran-Tauleria E, Jarvis D, Burney P, Anto JM. Socioeconomic status and asthma prevalence in young adults: the European Community Respiratory Health Survey. Am J Epidemiol. 2004;160(2):178–188. doi: 10.1093/aje/kwh186. [DOI] [PubMed] [Google Scholar]
- Beasley R, Ellwood P, Asher I. International patterns of the prevalence of pediatric asthma the ISAAC program. Pediatr Clin North Am. 2003;50(3):539–553. doi: 10.1016/s0031-3955(03)00050-6. [DOI] [PubMed] [Google Scholar]
- Berhane K, Gauderman WJ, Stram D, Thomas D. Statistical issues in studies of the long term effects of air pollution: The Southern California Children’s Health Study. Statistical Science. 19(4) (in press) [Google Scholar]
- Billings CG, Howard P. Damp housing and asthma. Monaldi Arch Chest Dis. 1998;53(1):43–49. [PubMed] [Google Scholar]
- Borchers AT, Keen CL, Gershwin ME. Hope for the hygiene hypothesis: when the dirt hits the fan. J Asthma. 2005;42(4):225–247. doi: 10.1081/jas-200051302. [DOI] [PubMed] [Google Scholar]
- Bufford JD, Gern JE. The hygiene hypothesis revisited. Immunol Allergy Clin North Am. 2005;25(2):247–262. v–vi. doi: 10.1016/j.iac.2005.03.005. [DOI] [PubMed] [Google Scholar]
- Cagney KA, Browning CR. Exploring neighborhood-level variation in asthma and other respiratory diseases: the contribution of neighborhood social context. J Gen Intern Med. 2004;19(3):229–236. doi: 10.1111/j.1525-1497.2004.30359.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cagney KA, Browning CR, Wallace DM. Explaining the Latino Asthma Advantage: The Role of Neighborhood Social Context. Population Association of America Annual Meeting; Philadelphia, PA. 2005. [Google Scholar]
- Callahan ST, Cooper WO. Uninsurance and health care access among young adults in the United States. Pediatrics. 2005;116(1):88–95. doi: 10.1542/peds.2004-1449. [DOI] [PubMed] [Google Scholar]
- Catalano R. The health effects of economic insecurity. Am J Public Health. 1991;81(9):1148–1152. doi: 10.2105/ajph.81.9.1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Asthma’s impact on children and adolescents. National Center for Environmental Health; 2003. [Google Scholar]
- Chen E, Hanson MD, Paterson LQ, Griffin MJ, Walker HA, Miller GE. Socioeconomic status and inflammatory processes in childhood asthma: The role of psychological stress. J Allergy Clin Immunol. 2006;117(5):1014–1020. doi: 10.1016/j.jaci.2006.01.036. [DOI] [PubMed] [Google Scholar]
- Denner J, Kirby D, Coyle K, Brindis C. The Protective Role of Social Capital and Cultural Norms in Latino Communities: A Study of Adolescent Births. Hispanic Journal of Behavioral Sciences. 2001;23(1):3–21. [Google Scholar]
- Diez Roux AV. A Glossary for Multilevel Analysis. J Epidemiol Community Health. 2002;56(8):588–594. doi: 10.1136/jech.56.8.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty D, Meikle SF, Owens P, Kelley E, Moy E. Children’s Health Care in the First National Healthcare Quality Report and National Healthcare Disparities Report. Med Care. 2005;43(3 Suppl):I58–63. doi: 10.1097/00005650-200503001-00009. [DOI] [PubMed] [Google Scholar]
- Federico MJ, Liu AH. Overcoming childhood asthma disparities of the inner-city poor. Pediatr Clin North Am. 2003;50(3):655–675. vii. doi: 10.1016/s0031-3955(03)00045-2. [DOI] [PubMed] [Google Scholar]
- Ferrie JE, Martikainen P, Shipley MJ, Marmot MG, Stansfeld SA, Smith GD. Employment status and health after privatisation in white collar civil servants: prospective cohort study. Bmj. 2001;322(7287):647–651. doi: 10.1136/bmj.322.7287.647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrett JE. Health service accessibility and deaths from asthma. Thorax. 1997;52(3):205–206. doi: 10.1136/thx.52.3.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gauderman WJ, Avol E, Lurmann F, Kuenzli N, Gilliland F, Peters J, McConnell R. Childhood asthma and exposure to traffic and nitrogen dioxide. Epidemiology. 2005;16(6):737–743. doi: 10.1097/01.ede.0000181308.51440.75. [DOI] [PubMed] [Google Scholar]
- Gilliland FD, Berhane K, Rappaport EB, Thomas DC, Avol E, Gauderman WJ, London SJ, Margolis HG, McConnell R, Islam KT, Peters JM. The effects of ambient air pollution on school absenteeism due to respiratory illnesses. Epidemiology. 2001;12(1):43–54. doi: 10.1097/00001648-200101000-00009. [DOI] [PubMed] [Google Scholar]
- Gilliland FD, Li YF, Peters JM. Effects of maternal smoking during pregnancy and environmental tobacco smoke on asthma and wheezing in children. Am J Respir Crit Care Med. 2001;163(2):429–436. doi: 10.1164/ajrccm.163.2.2006009. [DOI] [PubMed] [Google Scholar]
- Gilliland FD, Berhane K, Islam T, McConnell R, Gauderman WJ, Gilliland SS, Avol E, Peters JM. Obesity and the risk of newly diagnosed asthma in school-age children. Am J Epidemiol. 2003;158(5):406–415. doi: 10.1093/aje/kwg175. [DOI] [PubMed] [Google Scholar]
- Gold DR, Wright R. Population disparities in asthma. Annu Rev Public Health. 2005;26:89–113. doi: 10.1146/annurev.publhealth.26.021304.144528. [DOI] [PubMed] [Google Scholar]
- Haan M, Kaplan GA, Camacho T. Poverty and health. Prospective evidence from the Alameda County Study. Am J Epidemiol. 1987;125(6):989–998. doi: 10.1093/oxfordjournals.aje.a114637. [DOI] [PubMed] [Google Scholar]
- Hoffman RM, Gilliland FD, Eley JW, Harlan LC, Stephenson RA, Stanford JL, Albertson PC, Hamilton AS, Hunt WC, Potosky AL. Racial and ethnic differences in advanced-stage prostate cancer: the Prostate Cancer Outcomes Study. J Natl Cancer Inst. 2001;93(5):388–395. doi: 10.1093/jnci/93.5.388. [DOI] [PubMed] [Google Scholar]
- Holguin F, Mannino DM, Anto J, Mott J, Ford ES, Teague WG, Redd SC, Romieu I. Country of birth as a risk factor for asthma among Mexican Americans. Am J Respir Crit Care Med. 2005;171(2):103–108. doi: 10.1164/rccm.200402-143OC. [DOI] [PubMed] [Google Scholar]
- Jerrett M, Eyles J, Cole D. Socioeconomic and environmental covariates of premature mortality in Ontario. Soc Sci Med. 1998;47(1):33–49. doi: 10.1016/s0277-9536(98)00008-2. [DOI] [PubMed] [Google Scholar]
- Jerrett M, Finkelstein M. Geographies of risk in studies linking chronic air pollution exposure to health outcomes. J Toxicol Environ Health A. 2005;68(13):1207–1242. doi: 10.1080/15287390590936085. [DOI] [PubMed] [Google Scholar]
- Jin RL, Shah CP, Svaboda TJ. Working Paper for the Population Health Committee. Toronto, Ontario: Ontario Medical Association; 1994. The Health Impact of Unemployment: A Review and Application of Research Evidence. [Google Scholar]
- Jones SR, Riddell WC. The Measurement of Unemployment: An Empirical Approach. Econometrica. 1999;67(1):147–161. [Google Scholar]
- Juhn YJ, Sauver JS, Katusic S, Vargas D, Weaver A, Yunginger J. The influence of neighborhood environment on the incidence of childhood asthma: a multilevel approach. Soc Sci Med. 2005;60(11):2453–2464. doi: 10.1016/j.socscimed.2004.11.034. [DOI] [PubMed] [Google Scholar]
- Karmaus W, Botezan C. Does a higher number of siblings protect against the development of allergy and asthma? A review. J Epidemiol Community Health. 2002;56(3):209–217. doi: 10.1136/jech.56.3.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempe A, Beaty BL, Crane LA, Stokstad J, Barrow J, Belman S, Steiner JF. Changes in access, utilization, and quality of care after enrollment into a state child health insurance plan. Pediatrics. 2005;115(2):364–371. doi: 10.1542/peds.2004-0475. [DOI] [PubMed] [Google Scholar]
- King ME, Mannino DM, Holguin F. Risk factors for asthma incidence. A review of recent prospective evidence. Panminerva Med. 2004;46(2):97–110. [PubMed] [Google Scholar]
- Kunzli N, McConnell R, Bates D, Bastain T, Hricko A, Lurmann F, Avol E, Gilliland F, Peters J. Breathless in Los Angeles: the exhausting search for clean air. Am J Public Health. 2003;93(9):1494–1499. doi: 10.2105/ajph.93.9.1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu LY, Coe CL, Swenson CA, Kelly EA, Kita H, Busse WW. School examinations enhance airway inflammation to antigen challenge. Am J Respir Crit Care Med. 2002;165(8):1062–1067. doi: 10.1164/ajrccm.165.8.2109065. [DOI] [PubMed] [Google Scholar]
- London SJ, James Gauderman W, Avol E, Rappaport EB, Peters JM. Family history and the risk of early-onset persistent, early-onset transient, and late-onset asthma. Epidemiology. 2001;12(5):577–583. doi: 10.1097/00001648-200109000-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez AD. The evolution of the Global Burden of Disease framework for disease, injury and risk factor quantification: developing the evidence base for national, regional and global public health action. Global Health. 2005;1(1):5. doi: 10.1186/1744-8603-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannino DM, Homa DM, Akinbami LJ, Moorman JE, Gwynn C, Redd SC. Surveillance for asthma--United States, 1980–1999. MMWR Surveill Summ. 2002;51(1):1–13. [PubMed] [Google Scholar]
- Marmot M. Inequalities in health. N Engl J Med. 2001;345(2):134–136. doi: 10.1056/NEJM200107123450210. [DOI] [PubMed] [Google Scholar]
- McConnell R, Berhane K, Gilliland F, Islam T, Gauderman WJ, London SJ, Avol E, Rappaport EB, Margolis HG, Peters JM. Indoor risk factors for asthma in a prospective study of adolescents. Epidemiology. 2002a;13(3):288–295. doi: 10.1097/00001648-200205000-00009. [DOI] [PubMed] [Google Scholar]
- McConnell R, Berhane K, Gilliland F, London SJ, Islam T, Gauderman WJ, Avol E, Margolis HG, Peters JM. Asthma in exercising children exposed to ozone: a cohort study. Lancet. 2002b;359(9304):386–391. doi: 10.1016/S0140-6736(02)07597-9. [DOI] [PubMed] [Google Scholar]
- McConnell R, Berhane K, Gilliland F, Molitor J, Thomas D, Lurmann F, Avol E, Gauderman WJ, Peters JM. Prospective Study of Air Pollution and Bronchitic Symptoms in Children with Asthma. Am J Respir Crit Care Med. 2003;168(7):790–797. doi: 10.1164/rccm.200304-466OC. [DOI] [PubMed] [Google Scholar]
- McConnell R, Berhane K, Yao L, Jerrett M, Lurmann F, Gilliland F, Kunzli N, Gauderman J, Avol E, Thomas D, Peters J. Traffic, susceptibility, and childhood asthma. Environ Health Perspect. 2006;114(5):766–772. doi: 10.1289/ehp.8594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLafferty S, Grady S. Prenatal care need and access: a GIS analysis. J Med Syst. 2004;28(3):321–333. doi: 10.1023/b:joms.0000032848.76032.28. [DOI] [PubMed] [Google Scholar]
- McLafferty SL. GIS and health care. Annu Rev Public Health. 2003;24:25–42. doi: 10.1146/annurev.publhealth.24.012902.141012. [DOI] [PubMed] [Google Scholar]
- Merlo J, Chaix B, Yang M, Lynch J, Rastam L. A brief conceptual tutorial of multilevel analysis in social epidemiology: linking the statistical concept of clustering to the idea of contextual phenomenon. J Epidemiol Community Health. 2005;59(6):443–449. doi: 10.1136/jech.2004.023473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mielck A, Reitmeir P, Wjst M. Severity of childhood asthma by socioeconomic status. Int J Epidemiol. 1996;25(2):388–393. doi: 10.1093/ije/25.2.388. [DOI] [PubMed] [Google Scholar]
- Morello-Frosch R, Pastor M, Jr, Porras C, Sadd J. Environmental justice and regional inequality in southern California: implications for future research. Environ Health Perspect. 2002;110(Suppl 2):149–154. doi: 10.1289/ehp.02110s2149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morello-Frosch R, Lopez R. The riskscape and the color line: examining the role of segregation in environmental health disparities. Environ Res. 2006;102(2):181–196. doi: 10.1016/j.envres.2006.05.007. [DOI] [PubMed] [Google Scholar]
- Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997;349(9061):1269–1276. doi: 10.1016/S0140-6736(96)07493-4. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. Asthma Prevalence, Health Care Use and Mortality, 2002. Atlanta: Centers for Disease Control and Prevention (CDC); 2002. [Google Scholar]
- Nepomnyaschy L, Reichman NE. Low birthweight and asthma among young urban children. Am J Public Health. 2006;96(9):1604–1610. doi: 10.2105/AJPH.2005.079400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oakes JM. The (mis)estimation of neighborhood effects: causal inference for a practicable social epidemiology. Social Science and Medicine. 2004;58:1929–1952. doi: 10.1016/j.socscimed.2003.08.004. [DOI] [PubMed] [Google Scholar]
- O’Neill MS, Jerrett M, Kawachi I, Levy JI, Cohen AJ, Gouveia N, Wilkinson P, Fletcher T, Cifuentes L, Schwartz J. Health, wealth, and air pollution: advancing theory and methods. Environ Health Perspect. 2003;111(16):1861–1870. doi: 10.1289/ehp.6334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortega AN, Belanger KD, Paltiel AD, Horwitz SM, Bracken MB, Leaderer BP. Use of health services by insurance status among children with asthma. Med Care. 2001;39(10):1065–1074. doi: 10.1097/00005650-200110000-00004. [DOI] [PubMed] [Google Scholar]
- Pearce N, Beasley R, Burgess C, Crane J. Asthma Epidemiology: Principles and Methods. New York City, NY: Oxford University Press; 1998. [Google Scholar]
- Pearce N, Pekkanen J, Beasley R. How much asthma is really attributable to atopy? Thorax. 1999;54(3):268–272. doi: 10.1136/thx.54.3.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce N, Douwes J, Beasley R. The rise and rise of asthma: a new paradigm for the new millennium? J Epidemiol Biostat. 2000;5(1):5–16. [PubMed] [Google Scholar]
- Peters JM, Avol E, Navidi W, London SJ, Gauderman WJ, Lurmann F, Linn WS, Margolis H, Rappaport E, Gong H, Thomas DC. A study of twelve Southern California communities with differing levels and types of air pollution. I. Prevalence of respiratory morbidity. Am J Respir Crit Care Med. 1999;159(3):760–767. doi: 10.1164/ajrccm.159.3.9804143. [DOI] [PubMed] [Google Scholar]
- Reyes BI, editor. Public Policy Institute of California. A portrait of race and ethnicity in California: an assessment of social and economic well-being. San Francisco, CA: 2001. [Google Scholar]
- Ramsey CD, Celedon JC. The hygiene hypothesis and asthma. Curr Opin Pulm Med. 2005;11(1):14–20. doi: 10.1097/01.mcp.0000145791.13714.ae. [DOI] [PubMed] [Google Scholar]
- Randi G, Altieri A, Chatenoud L, Chiaffarino F, La Vecchia C. Infections and atopy: an exploratory study for a meta-analysis of the “hygiene hypothesis”. Rev Epidemiol Sante Publique. 2004;52(6):565–574. doi: 10.1016/s0398-7620(04)99095-5. [DOI] [PubMed] [Google Scholar]
- Redd SC. Asthma in the United States: burden and current theories. Environ Health Perspect. 2002;110(Suppl 4):557–560. doi: 10.1289/ehp.02110s4557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson RJ, Morenoff JD, Earls F. Beyond social capital: Spatial dynamics of collective efficacy for children. American Sociological Review. 1999;64(5):633–660. [Google Scholar]
- SAS Institute Inc. SAS Version 9.1. Cary, NC: 2002. [Google Scholar]
- Scientific Software International Inc. SSI 6.02a. Lincolnwood, IL: 2005. [Google Scholar]
- Shapiro GG, Stout JW. Childhood asthma in the United States: urban issues. Pediatr Pulmonol. 2002;33(1):47–55. doi: 10.1002/ppul.10029. [DOI] [PubMed] [Google Scholar]
- Sorensen G, Verbrugge LM. Women, work, and health. Annu Rev Public Health. 1987;8:235–251. doi: 10.1146/annurev.pu.08.050187.001315. [DOI] [PubMed] [Google Scholar]
- Stata Corporation. Intercooled Stata 8.1 for Windows. College Station, TX: 2003. [Google Scholar]
- Strachan DP. Hay fever, hygiene, and household size. Bmj. 1989;299(6710):1259–1260. doi: 10.1136/bmj.299.6710.1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tatalovich T, Wilson J, Jerrett M, Milam J, McConnell R. Competing Definitions of Contextual Environments. 2006 doi: 10.1186/1476-072X-5-55. Submitted to Journal of International Health Geographics. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tatalovich Z, Wilson JP, Milam JE, Jerrett ML, McConnell R. Competing definitions of contextual environments. Int J Health Geogr. 2006;5:55. doi: 10.1186/1476-072X-5-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. 1990 Summary Tape File 3 Technical Documentation. Washington, D.C: 1992. [Google Scholar]
- U.S. Census Bureau. Illustrative Ranges of the Distribution of Undocumented Immigrants by State. In: Fernandez EW, Robinson JG, editors. Population Division Technical Working Paper No 8. 1994. [Google Scholar]
- Vivier PM. The impact of Medicaid on children’s healthcare and health. Curr Opin Pediatr. 2005;17(6):759–763. doi: 10.1097/01.mop.0000187189.89542.b5. [DOI] [PubMed] [Google Scholar]
- Von Ehrenstein OS, Von Mutius E, Illi S, Baumann L, Bohm O, von Kries R. Reduced risk of hay fever and asthma among children of farmers. Clin Exp Allergy. 2000;30(2):187–193. doi: 10.1046/j.1365-2222.2000.00801.x. [DOI] [PubMed] [Google Scholar]
- Warren N. Potential Data Sources for Asthma Surveillance at a County and State Level in California. Berkley, CA: Regional Asthma Management and Prevention Initiative; 1999. p. 16. [Google Scholar]
- White IR, Thompson SG. Adjusting for partially missing baseline measurements in randomized trials. Stat Med. 2005;24(7):993–1007. doi: 10.1002/sim.1981. [DOI] [PubMed] [Google Scholar]
- Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000;56(2):645–646. doi: 10.1111/j.0006-341x.2000.00645.x. [DOI] [PubMed] [Google Scholar]
- Wissow LS, Gittelsohn AM, Szklo M, Starfield B, Mussman M. Poverty, race, and hospitalization for childhood asthma. Am J Public Health. 1988;78(7):777–782. doi: 10.2105/ajph.78.7.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AL. The epidemiology of the atopic child: who is at risk for what? J Allergy Clin Immunol. 2004;113(1 Suppl):S2–7. doi: 10.1016/j.jaci.2003.09.050. [DOI] [PubMed] [Google Scholar]
- Wright RJ, Rodriguez M, Cohen S. Review of psychosocial stress and asthma: an integrated biopsychosocial approach. Thorax. 1998;53(12):1066–1074. doi: 10.1136/thx.53.12.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright RJ, Mitchell H, Visness CM, Cohen S, Stout J, Evans R, Gold DR. Community violence and asthma morbidity: the Inner-City Asthma Study. Am J Public Health. 2004;94(4):625–632. doi: 10.2105/ajph.94.4.625. [DOI] [PMC free article] [PubMed] [Google Scholar]