Abstract
Background
To estimate probability of adverse pregnancy outcomes (APOs) among women with and without syphilis through a systematic review of published literatures.
Methodology/Principal Findings
Chinese and English literatures were searched for studies assessing pregnancy outcomes in the presence of maternal syphilis through August 2013. The prevalence estimates were summarized and analyzed by meta-analysis. Fifty-four literatures involving 11398 syphilitic women and 43342 non-syphilitic women were included from 4187 records initially found. Among untreated mothers with syphilis, pooled estimates were 76.8% for all APOs, 36.0% for congenital syphilis, 23.2% for preterm, 23.4% for low birth weight, 26.4% for stillbirth or fetal loss, 14.9% for miscarriage and 16.2% for neonatal deaths. Among syphilitic mother receiving treatment only in the late trimester (>28 weeks), pooled estimates were 64.4% for APOs, 40.6% for congenital syphilis, 17.6% for preterm, 12.4% for low birth weight, and 21.3% for stillbirth or fetal loss. Among syphilitic mothers with high titers (≥1∶8), pooled estimates were 42.8% for all APOs, 25.8% for congenital syphilis, 15.1% for preterm, 9.4% for low birth weight, 14.6% for stillbirth or fetal loss and 16.0% for neonatal deaths. Among non-syphilitic mothers, the pooled estimates were 13.7% for all APOs, 7.2% for preterm birth, 4.5% for low birth weight, 3.7% for stillbirth or fetal loss, 2.3% for miscarriage and 2.0% for neonatal death. Begg's rank correlation test indicated little evidence of publication bias (P>0.10). Substantial heterogeneity was found across studies in the estimates of all adverse outcomes for both women with syphilis (I 2 = 93.9%; P<0.0001) and women without syphilis (I 2 = 94.8%; P<0.0001).
Conclusions/Significance
Syphilis continues to be an important cause of substantial perinatal morbidity and mortality, which reminds that policy-makers charged with resource allocation that the elimination of mother-to-child transmission of syphilis is a public health priority.
Introduction
Mother-to-child transmission (MTCT) of syphilis has been documented since the 15th century, yet, today, continues to cause substantial perinatal morbidity and mortality, even in developed countries, where antenatal health services are strong [1]–[2]. Prenatal screening coupled with appropriate, prompt penicillin treatment in prevention of MTCT of syphilis is feasible, inexpensive, and cost-effective, even in settings where the burden of syphilis among pregnant women is moderate or low [3]–[5]. Yet, despite the tools being available for over 60 y, MTCT of syphilis persists as a public health problem in many rural, urban, and suburban communities [9]. In 2007, the World Health Organization (WHO) launched its initiative for Global Elimination of Congenital Syphilis (CS) as millennium development goals [6]. In response to the call of the WHO, in June 2010, the China's Ministry of Health (MOH) officially launched the first national program specially and directly aimed at controlling syphilis and blocking MTCT of syphilis: the National Program for Prevention and Control of Syphilis in China (2010–2020) [7]. In order to effectively eliminate of MTCT of syphilis and to guide policy and advocacy efforts, global data on the burden of syphilis in pregnancy and associated adverse pregnancy outcomes (APOs) are needed.
Currently, although some estimates for burden of syphilis in pregnancy and associated APOs were available, the global incidence of adverse birth outcomes among syphilitic women remains enough unclear. Over the years, some researchers have been trying to estimate the incidence of APOs resulting from maternal syphilis. For example, the latest meta-analysis by Gomez et al. [8] that is currently the only systematic review assessing this question indicated that approximately 52% of pregnancies in mothers with untreated or inadequately treated syphilis result in some APOs, with estimated proportions: early fetal loss or stillbirth (21%), neonatal death (9%), low birth weight or premature birth (6%), and infection in a live-born infant (15%), and among untreated pregnant women with syphilis, fetal loss and stillbirth were 21% more frequent, neonatal deaths were 9.3% more frequent and prematurity or low birth weight were 5.8% more frequent than among women without syphilis. However, this review didn't assess APOs under the background of different baseline titers and treatment time for maternal syphilis, and didn't include Chinese literatures. In China, there are large study reports to assess adverse outcomes among women with syphilis, while China's literatures are mainly local or single medical institution reports and only include the small sample size of study population, which causes that the findings are not comprehensive and meaningful representation of poor. Overall, most of previous estimates of APOs in women with syphilis have been based on point estimates from single studies.
Today, the full extent of MTCT of syphilis is difficult to measure because there is no definitive test for MTCT transmission; diagnosis based on clinical history and serologic testing in mothers and infants is often unavailable. Additionally, the countries where CS continues to be most problematic often lack even basic testing capacity, let alone more sophisticated laboratory techniques for diagnosis and staging syphilis during pregnancy. However, the large body of literatures from China, where syphilis testing is routinely done during pregnancy, can help address this issue. In order to support the global initiative for elimination of MTCT of syphilis, we conducted a systematic review and meta-analysis with the following objectives: (1) to estimate the APOs among syphilitic women according to baseline titers, treatment or not during pregnancy and gestational age at treatment; (2) to estimate APOs among women without syphilis; and (3) to provide scientific evidence for the prevention of pregnancy loss attributable to MTCT of syphilis.
Methods
Search strategy
PubMed, Cochrane Libraries, China Biology Medicine disc (CBMdisc), Chinese Scientific Journals Fulltext Database (CQVIP), China National Knowledge Infrastructure (CNKI) and Wanfang Data were searched through August 2013 with no restrictions to identify published peer-reviewed research articles assessing pregnancy outcomes in the presence of maternal syphilis by the following search terms: syphilis, pregnancy, adverse birth or pregnancy outcomes, congenital syphilis, preterm, low birth weight, stillbirth, fetal loss or death, abortion or miscarriage, neonatal death, and perinatal death or morbidity or mortality. We also performed a manual search on the reference lists of published articles. The grey literature and conference abstracts were not searched. This review was conducted and reported according to MOOSE guidelines and PRISMA requirements [10]–[11].
Selection criteria
For those studies that not only reported the incidence of birth outcomes among syphilis-infected women, but also reported the incidence among non-syphilitic women, we will meanwhile estimate the range of possible birth outcomes among non-syphilitic women. Our APOs of interest were CS, preterm, low birth weight, stillbirth or early fetal loss, miscarriage and neonatal death. Studies were considered eligible for inclusion in this systematic review if they met the following criteria: (1) studies published in Chinese or English language; (2) studies described pregnancy outcomes among women presumed to have syphilis(i.e. women who were seroreactive for T. pallidum infection, irrespective of the test used); (3) study populations excluded HIV-positive women; (4) sample size for cases was more than 30 syphilitic patients; and (5) the incidences of APOs were reported(or data to calculate them). We excluded review papers, non peer–reviewed local/government reports, conference abstract and presentation in this study. If the same study data were published in both English and Chinese sources, the articles published in Chinese language were excluded from the review. We considered a broad range of study designs, including clinical trials, observational studies, and case series. We also assessed potential studies to ensure that there was no duplication of case series.
Data extraction
Two independent reviewers (JBQ and HLF) assessed eligibility criteria and extracted data, and any disagreements were resolved by discussion. We extracted the following information from all eligible studies: first author and published year; geographical location; study design; study period; syphilis prevalence among mothers; subgroup variables (infection status of syphilis, treatment or not for maternal syphilis, gestational age at treatment, and baseline titers of nontreponemal antibodies); sample size for cases and controls; reported adverse outcomes. Because variations in the definition of APOs exist across countries and cultures, it is extremely difficult to define uniform standards. The early literatures did not always define birth outcomes and in such cases we relied on the outcome terminology in the original papers.
Statistical analysis
We calculated the combined incidence and the corresponding 95% confidence intervals (CI) for all APOs in women with syphilis and women without syphilis. We then also calculated the summary incidence and the corresponding 95%CI for the following selected pregnancy loss. The subgroup analysis for all APOs and specific APOs was performed based on whether women were infected with syphilis, whether syphilitic women were treated during pregnancy (i.e. syphilitic women receiving at least one injection of 2.4 million units of penicillin before delivery), gestational week at treatment (i.e. <12 or 12 to 28 or ≥28 weeks), and maternal baseline titers (i.e. ≥1∶8 or <1∶8) to explore the sources of heterogeneity.
The combined incidence and the corresponding 95% CI were calculated using either fixed-effects models or, in the presence of heterogeneity, random-effects models. Heterogeneity tests were performed using the Cochran Q-test (p<0.10 represents statistically significant heterogeneity) and I2 statistic. Begg's rank correlation test was used to assess publication bias (p<0.10 represents statistical significance). The chi-square test was used to analyze the difference between subgroups (p<0.05 represents statistical significance). The comparison between subgroups was performed using SAS version 9.1, and other data were prepared and analyzed using R software version 3.0.
Results
Study characteristics
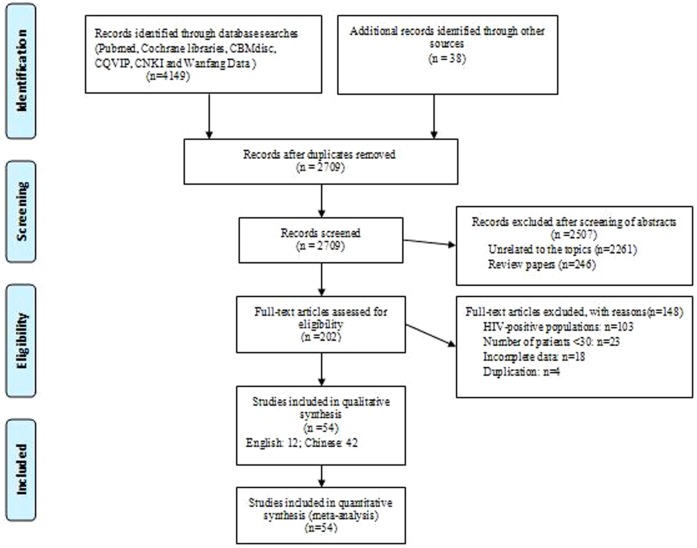
Our initial search criteria identified 4149 articles from six electronic databases and 38 additional articles were identified through reference lists from identified articles. Of these, the majority were excluded after the first screening based on abstracts or titles, mainly because they were review papers, and unrelated to the topics or duplicated titles from different databases (Figure 1). Finally, fifty-four studies [12]–[19], [21]–[24], [32]–[73] were considered eligible in qualitative synthesis. The characteristics of included studies involving 11398 women with syphilis and 43342 women without syphilis and published between 1917 and 2013 were summarized in Table 1. Forty-five studies [22]–[24], [32]–[73] were conducted in China, one [12] in UK, three in USA [13]-[14], [17], one [15] in Zambia, one [16] in Malawi, one [18] in Kenya, one [19] in Tanzania, and one [21] in Russia. All articles belonged to observational studies including retrospective cohort studies, retrospective cases analysis, prospective cohort studies, and prospective surveillance. Twelve studies (21.8%) presented the findings of observational studies that included a “control” arm assessing APOs among women without syphilis. Syphilis prevalence among mothers was reported from 22.1 to 765.7 cases per 10000 pregnant women. Forty-six studies reported on clinical evidence of CS in children. Thirty-four studies reported on preterm birth and fourteen studies reported on low birth weight. Forty-one studies reported on stillbirth or early fetal loss and fifteen studies reported on miscarriage. Twenty studies reported on neonatal death.
Figure 1. Flow chart showing the meta-analysis studies selection.
n, the number of prevalence estimates included in meta-analysis.
Table 1. Characteristics of studies included in a systematic review and meta-analysis to determine the frequency of adverse pregnancy outcomes (APOs) among women with syphilis and women without syphilis.
| Study | Location | Study design | Period | Syphilis prevalence among mothers (1/10000) | Sample size | Subgroup variables | Reported adverse pregnancy outcomes (APOs) |
| Harman/1917 [12] | United kingdom | retrospective cohort | 1917 | 360.0 | Syphilitic mothers: 1001 | mothers with syphilis or without syphilis | Congenital syphilis, and stillbirth and fetal loss, and all APOs |
| Non-syphilitic mothers: 826 | |||||||
| Wammock/1950 [13] | United states of America | retrospective cohort | 1045–1948 | 150.0 | Syphilitic mothers: 61 | mothers with syphilis or without syphilis | Congenital syphilis, preterm birth or low birth weight, stillbirth or fetal loss, and neonatal death, and all APOs |
| Non-syphilitic mothers: 5596 | |||||||
| Ingraham/1950 [14] | United states of America | Prospective cohort | 1940–1949 | 150.0 | Syphilitic mothers: 220 | mothers with syphilis or without syphilis | Congenital syphilis, Stillbirth or fetal loss, neonatal death, preterm birth or low birth weight, and all APOs |
| Non-syphilitic mothers: 10323 | |||||||
| Hira/1990 [15] | Zambia | Prospective surveillance | 1985–1987 | Unknown | Syphilitic mothers: 230 | mothers with syphilis or without syphilis | Congenital syphilis, preterm birth, low birth weight, stillbirth or fetal loss, miscarriage, and all APOs |
| Non-syphilitic mothers: 2647 | |||||||
| McDermott/1993 [16] | Malawi | retrospective cohort | 1987–1990 | 362.0 | Syphilitic mothers: 130 | mothers with syphilis or without syphilis | Stillbirth or fetal loss, and neonatal death, and all APOs |
| Non-syphilitic mothers: 3591 | |||||||
| Barbara/1995 [17] | United states of America | Retrospective analysis | 1991–1992 | Unknown | Syphilitic mothers: 253 | mothers with syphilis or without syphilis | Congenital syphilis, stillbirth or fetal loss, and neonatal death |
| Non-syphilitic mothers: 7929 | |||||||
| Temmerman/2000 [18] | Kenya | Prospective cohort | 1997–1998 | 238.4 | Syphilitic mothers: 275 | mothers with syphilis or without syphilis | Low birth weight, and stillbirth or fetal loss |
| Non-syphilitic mothers: 275 | |||||||
| Deborah WJ/2002 [19] | Tanzania | Prospective cohort | 1997–1999 | 765.7 | Syphilitic mothers: 382 | gestational week at treatment; mothers with syphilis or without syphilis; baseline titers of nontreponemal antibodies | Preterm birth, low birth weight, stillbirth or fetal loss, and all APOs |
| Non-syphilitic mothers: 950 | |||||||
| Tikhonova/2003 [21] | Russia | retrospective cohort | 1995–1999 | Unknown | Syphilitic mothers: 628 | treatment or not | Stillbirth or fetal loss |
| Liu JB/2010 [22] | Shenzhen,China | Prospective cohort | 2002–2007 | 43.4 | Syphilitic mothers: 554 | baseline titers of nontreponemal antibodies | Congenital syphilis |
| Zhu LP/2010 [23] | Shanghai, China | Prospective cohort | 2002–2006 | 27.5 | Syphilitic mothers: 1471 | treatment or not;baseline titers of nontreponemal antibodies;gestational week at treatment | Congenital syphilis |
| Qin JB/2013 [24] | Shenzhen, China | Prospective cohort | 2007–2012 | 30.0 | Syphilitic mothers: 360 | treatment or not;baseline titers of nontreponemal antibodies;gestational week at treatment | Congenital syphilis |
| Lv J/2001 [32] | Guangzhou | Retrospective analysis | 1994–2000 | Unknown | Syphilitic mothers: 64 | treatment or not | Congenital syphilis, preterm birth, stillbirth or fetal loss, and all APOs |
| Xu Y/2001 [33] | Haikou | Retrospective analysis | 1995–2001 | 62.2 | Syphilitic mothers: 48 | treatment or not | Congenital syphilis, preterm birth, stillbirth or fetal loss, miscarriage, neonatal death, and all APOs |
| Lin XH/2002 [34] | Guangzhou | Retrospective analysis | 1998–2000 | 74.0 | Syphilitic mothers: 41 | treatment or not; mothers with syphilis or without syphilis | Congenital syphilis, preterm birth, stillbirth or fetal loss, neonatal death, and all APOs |
| Non-syphilitic mothers: 5532 | |||||||
| Fang SN/2003 [35] | Shenzhen | Retrospective analysis | 1997–2002 | Unknown | Syphilitic mothers: 42 | treatment or not | Congenital syphilis, preterm birth, stillbirth or fetal loss, miscarriage, and all APOs |
| Wang HB/2003 [36] | Shanghai | Retrospective analysis | 1998–2002 | 51.2 | Syphilitic mothers: 21 | treatment or not | Congenital syphilis |
| Kuang YB/2004 [37] | Guangzhou | Prospective cohort | 2001–2003 | 135.4 | Syphilitic mothers: 73 | mothers with syphilis or without syphilis | Preterm birth, stillbirth or fetal loss, and all APOs |
| Non-syphilitic mothers: 5317 | |||||||
| Xu YX/2004 [38] | Shenzhen | Prospective cohort | 2002–2003 | Unknown | Syphilitic mothers: 54 | treatment or not | Congenital syphilis, stillbirth or fetal loss, miscarriage, neonatal death, and all APOs |
| Zhang XM/2004 [39] | Fuzhou | Prospective cohort | 1996–2001 | 69.7 | Syphilitic mothers: 192 | treatment or not;baseline titers of nontreponemal antibodies;gestational week at treatment | Congenital syphilis, preterm birth, low birth weight, stillbirth or fetal loss, miscarriage, neonatal death, and all APOs |
| Li Q/2005 [40] | Dongguan | Retrospective analysis | 2003–2004 | Unknown | Syphilitic mothers: 46 | mothers with syphilis or without syphilis | Congenital syphilis, preterm birth, low birth weight, stillbirth or fetal loss, neonatal death, and all APOs |
| Non-syphilitic mothers: 356 | |||||||
| Zhou H/2006 [41] | Shenzhen | Prospective cohort | 2002–2004 | 42.9 | Syphilitic mothers: 371 | baseline titers of nontreponemal antibodies;gestational week at treatment | Congenital syphilis |
| Gao H/2006 [42] | Zhanjiang | Retrospective analysis | 2002–2005 | Unknown | Syphilitic mothers: 97 | gestational week at treatment | Congenital syphilis, preterm birth, low birth weight, stillbirth or fetal loss, and all APOs |
| Wang CX/2006 [43] | Guangzhou | Retrospective analysis | 1997–2005 | Unknown | Syphilitic mothers: 48 | treatment or not | Congenital syphilis, preterm birth, stillbirth or fetal loss, miscarriage, and all APOs |
| Xuan QS/2006 [44] | Guangzhou | prospective surveillance | 1995–2003 | Unknown | Syphilitic mothers: 286 | gestational week at treatment | Congenital syphilis, preterm birth, low birth weight, stillbirth or fetal loss, miscarriage, neonatal death, and all APOs |
| Zheng RQ/2006 [45] | Shenzhen | Retrospective analysis | 2000–2005 | 87.0 | Syphilitic mothers: 48 | treatment or not | Congenital syphilis, preterm birth, stillbirth or fetal loss, miscarriage, neonatal death, and all APOs |
| Wang X/2007 [46] | Shantou | Retrospective analysis | Unknown | Unknown | Syphilitic mothers: 68 | treatment or not | Congenital syphilis, preterm birth, stillbirth or fetal loss, and all APOs |
| Sun LL/2008 [47] | Shaoguan | Retrospective analysis | 2000–2006 | 91.7 | Syphilitic mothers: 62 | treatment or not | Congenital syphilis, preterm birth, miscarriage, neonatal death, and all APOs |
| Gao JM/2009 [48] | Nanchang | prospective surveillance | 2003–2007 | Unknown | Syphilitic mothers: 82 | no | Congenital syphilis, preterm birth, low birth weight, stillbirth or fetal loss, neonatal death, and all APOs |
| Huang ZM/2009 [49] | Shenzhen | Retrospective analysis | 2005–2007 | Unknown | Syphilitic mothers: 452 | treatment or not;baseline titers of nontreponemal antibodies | Congenital syphilis |
| Li L/2009 [50] | Beijing | Retrospective analysis | 2006–2007 | Unknown | Syphilitic mothers: 121 | treatment or not;gestational week at treatment | Congenital syphilis, preterm birth, stillbirth or fetal loss, and all APOs |
| Wu FY/2009 [51] | Zhejiang | Retrospective analysis | 2006–2008 | 97.7 | Syphilitic mothers: 47 | treatment or not | Congenital syphilis, preterm birth, low birth weight, stillbirth or fetal loss, neonatal death, and all APOs |
| Zhou GJ/2009 [52] | Hefei | Retrospective analysis | 2003–2006 | 110.3 | Syphilitic mothers: 53 | treatment or not | Congenital syphilis, preterm birth, low birth weight, stillbirth or fetal loss, neonatal death, and all APOs |
| Chen JH/2010 [53] | Liuyang | prospective surveillance | 2008–2009 | 77.6 | Syphilitic mothers: 61 | gestational week at treatment | Congenital syphilis, preterm birth, stillbirth or fetal loss, miscarriage, and all APOs |
| Li TH/2010 [54] | Huhehaote | prospective surveillance | 2006–2009 | Unknown | Syphilitic mothers: 168 | treatment or not;gestational week at treatment | Congenital syphilis, preterm birth, stillbirth or fetal loss, and all APOs |
| Shuang JY/2010 [55] | Taiyuan | Retrospective analysis | 2006–2010 | Unknown | Syphilitic mothers: 48 | treatment or not;baseline titers of nontreponemal antibodies | Congenital syphilis, and all APOs |
| Ye GR/2010 [56] | Panzhihua | Prospective cohort | 2008–2010 | Unknown | Syphilitic mothers: 80 | gestational week at treatment | Preterm birth, low birth weight, stillbirth or fetal loss, and all APOs |
| Dai Y/2011 [57] | Yangzhou | Retrospective analysis | 2006–2010 | 60.3 | Syphilitic mothers: 136 | gestational week at treatment | Congenital syphilis, and all APOs |
| Li Z/2011 [58] | Shenzhen | Prospective cohort | 2002–2010 | 26.2 | Syphilitic mothers: 427 | treatment or not | Congenital syphilis |
| Luo ZZ/2011 [59] | Shenzhen | Prospective cohort | 2007–2010 | 23.7 | Syphilitic mothers: 227 | gestational week at treatment; baseline titers of nontreponemal antibodies | All APOs |
| Wang WL/2011 [60] | Zhejiang | Retrospective analysis | 2006–2009 | Unknown | Syphilitic mothers: 52 | treatment or not; gestational week at treatment | Congenital syphilis, preterm birth, stillbirth or fetal loss, and all APOs |
| Yuan XQ/2011 [61] | Chengdu | Retrospective analysis | 2010–2011 | Unknown | Syphilitic mothers: 52 | gestational week at treatment | Congenital syphilis, preterm birth, stillbirth or fetal loss, and all APOs |
| Cao DH/2012 [62] | Zhongshan | Retrospective analysis | 2005–2010 | Unknown | Syphilitic mothers: 41 | treatment or not | Congenital syphilis, preterm birth, low birth weight, stillbirth or fetal loss, miscarriage, neonatal death, and all APOs |
| Chen GJ/2012 [63] | Shenzhen | Prospective cohort | 2004–2009 | 48.7 | Syphilitic mothers: 330 | treatment or not | Congenital syphilis, preterm birth, stillbirth or fetal loss, miscarriage, and all APOs |
| Deng JF/2012 [64] | Shenzhen | Retrospective analysis | 2009–2011 | Unknown | Syphilitic mothers: 58 | treatment or not | Congenital syphilis, preterm birth, and stillbirth or fetal loss, miscarriage, neonatal death, and all APOs |
| Li HS/2012 [65] | Changchun | Retrospective analysis | 2006–2011 | 22.1 | Syphilitic mothers: 33 | treatment or not | Preterm birth, stillbirth or fetal loss, neonatal death, and all APOs |
| Li Z/2012 [66] | Chongzuo | Retrospective analysis | 2004–2011 | Unknown | Syphilitic mothers: 86 | gestational week at treatment | Congenital syphilis, and all APOs |
| Pan P/2012 [67] | Shenzhen | Prospective cohort | 2005 | Unknown | Syphilitic mothers: 584 | no | Congenital syphilis, and all APOs |
| Xu ZY/2012 [68] | Shenzhen | Prospective cohort | 2005–2010 | Unknown | Syphilitic mothers: 772 | gestational week at treatment; baseline titers of nontreponemal antibodies | Congenital syphilis, preterm birth, low birth weight, stillbirth or fetal loss, neonatal death, and all APOs |
| Cui L/2013 [69] | Xinxiang | Retrospective analysis | 2007–2012 | Unknown | Syphilitic mothers: 80 | treatment or not | Congenital syphilis, preterm birth, stillbirth or fetal loss, and all APOs |
| Shi J/2013 [70] | Guangzhou | Retrospective analysis | 2006–2011 | Unknown | Syphilitic mothers: 85 | gestational week at treatment | Congenital syphilis, preterm birth, stillbirth or fetal loss, miscarriage, neonatal death, and all APOs |
| Wei HP/2013 [71] | Beihai | Prospective cohort | 2010–2012 | Unknown | Syphilitic mothers: 89 | gestational week at treatment; baseline titers of nontreponemal antibodies | Congenital syphilis, preterm birth, stillbirth or fetal loss, miscarriage, and all APOs |
| Wu FY/2013 [72] | Qujing | prospective surveillance | 2009–2011 | Unknown | Syphilitic mothers: 56 | treatment or not | Congenital syphilis, preterm birth, stillbirth or fetal loss, and all APOs |
| Xu ZY/2013 [73] | Zhejiang | prospective surveillance | 2009–2011 | Unknown | Syphilitic mothers: 52 | treatment or not | Congenital syphilis, preterm birth, low birth weight, neonatal death, and all APOs |
All APOs among women with and without syphilis
The reported proportion range of all APOs in the original studies is from 12.3% to 95.1% with a median of 49.2% among women with syphilis and from 9.3% to 20.8% with a median of 12.5% among women without syphilis (Table 2). The pooled estimates of all APOs were 47.7% (95%CI: 41.6–54.0) among syphilis-infected women and 13.7% (95%CI: 12.0–15.6) among women without syphilis (Table 2), for an absolute difference of 34.0% (χ2 = 3616.129, P = 0.000) (Table 3). Begg's rank correlation test indicated little evidence of publication bias (P = 0.171 to 0.397) for summary estimates of all APOs among women with and without syphilis (Table 2). Substantial heterogeneity was found across studies in the estimates of all APOs for both women with syphilis (I 2 = 93.9%; P<0.0001) and women without syphilis (I 2 = 94.8%; P<0.0001).
Table 2. Summary estimates of the proportion (%) of adverse pregnancy outcomes (APOs) among women with syphilis and women without syphilis.
| Reported proportion in the original studies | APOs | n | No. of included studies | Summary estimates (95%CI)# | Heterogeneity | Bias assessment | ||
| Range | M (IQR) | |||||||
| Women with syphilis | ||||||||
| All APOs | 12.3%–95.1% | 49.2% (58.0%–37.0%) | 2495 | 5237 | 41 | 47.7% (95%CI: 41.6%–54.0%) | I2 = 93.9%, P<0.0001 | P = 0.397 |
| Congenital syphilis | 0.6%–79.3% | 20.6% (38.2%–10.3%) | 1680 | 9430 | 46 | 20.6% (95%CI: 16.4%–25.6%) | I2 = 95.3%, P<0.0001 | P = 0.403 |
| Preterm birth | 0.9%–39.4% | 15.3% (19.2%–11.0%) | 451 | 4089 | 34 | 14.1% (95%CI: 11.4%–17.3%) | I2 = 81.6%, P<0.0001 | P = 0.272 |
| Low birth weight | 3.6%–29.3% | 17.0% (21.3%–5.8%) | 288 | 2593 | 14 | 13.2% (95%CI: 9.2%–18.5%) | I2 = 89.3%, P<0.0001 | P = 0.133 |
| Miscarriage | 3.1%–14.8% | 5.6% (10.3%–3.7%) | 109 | 1674 | 15 | 6.6% (95%CI: 4.7%–9.3%)) | I2 = 66.0%, P = 0.0002 | P = 0.194 |
| Stillbirth or fetal loss | 2.1%–43.8% | 12.1% (21.6%–7.3%) | 802 | 6558 | 41 | 12.5% (95%CI: 10.0%–15.5%) | I2 = 88.9%, P<0.0001 | P = 0.391 |
| Neonatal death | 1.0%–33.3% | 5.5% (13.4%–2.6%) | 140 | 2413 | 20 | 6.6% (95%CI: 4.1%–10.4%) | I2 = 84.2%, P<0.0001 | P = 0.107 |
| Women without syphilis | ||||||||
| All APOs | 9.3%–20.8% | 12.5% (17.7%–10.9%) | 4640 | 34546 | 9 | 13.7% (95%CI: 12.0%–15.6%) | I2 = 94.8%, P<0.0001 | P = 0.171 |
| Preterm birth | 3.0%–11.8% | 7.6% (9.7%–4.1%) | 1201 | 15011 | 5 | 7.2% (95%CI: 5.6%–9.3%) | I2 = 93.6%, P<0.0001 | P = 0.102 |
| Low birth weight | 1.8%–9.9% | 5.1% (9.5%–1.9%) | 166 | 4313 | 4 | 4.5% (95%CI: 2.0%–10.0%) | I2 = 95.9%, P<0.0001 | P = 0.142 |
| Miscarriage | 62 | 2647 | 1 | 2.3% (95%CI: 1.8%–3.0%) | ||||
| Stillbirth or fetal loss | 1.1%–9.4% | 3.6% (6.4%–1.7%) | 1536 | 42726 | 11 | 3.7% (95%CI: 2.6%–5.1%) | I2 = 97.3%, P<0.0001 | P = 0.230 |
| Neonatal death | 0.8%–4.1% | 2.2% (3.6%–0.8%) | 581 | 27094 | 5 | 2.0% (95%CI: 1.2%–3.3%) | I2 = 96.9%, P<0.0001 | P = 0.181 |
M = Median; IQR = Inter-quartile range; APOs = adverse pregnancy outcomes; CI = Confidence interval.
Summary estimates and their corresponding 95% CI were calculated using either fixed-effects models or, in the presence of heterogeneity, random-effects models.
Table 3. Comparison for summary estimates of the proportion (%) of adverse pregnancy outcomes (APOs) among different subgroups.
| Subgroup | All APOs | Congenital syphilis | Preterm birth | Low birth weight | ||||
| absolute differences | chi-square test | absolute differences | chi-square test | absolute differences | chi-square test | absolute differences | chi-square test | |
| Women with syphilis vs women without syphilis | 34.0% | ?2 = 3616.129, P = 0.000 | 6.9% | χ 2 = 37.312, P = 0.000 | 8.7% | χ 2 = 138.897, P = 0.000 | ||
| Untreated women with syphilis vs women without syphilis | 63.1% | ?2 = 3947.821, P = 0.000 | 16.0% | ?2 = 139.350, P = 0.000 | 18.9% | ?2 = 110.776, P = 0.000 | ||
| Treatment in the third trimester vs women without syphilis | 50.7% | ?2 = 727.296, P = 0.000 | 10.4% | ?2 = 24.696, P = 0.000 | 7.9% | ?2 = 28.440, P = 0.000 | ||
| High titers (≥1∶8) vs women without syphilis | 29.1% | ?2 = 209.950, P = 0.000 | 7.9% | ?2 = 18.044, P = 0.000 | 4.9% | ?2 = 22.790, P = 0.000 | ||
| Untreated women with syphilis vs Treated women with syphilis | 52.6% | ?2 = 1059.165, P = 0.000 | 22.0% | ?2 = 290.433; P = 0.000 | 13.3% | χ 2 = 66.595, P = 0.000 | 17.2% | χ 2 = 53.604,P = 0.000 |
| Treatment in the third trimester vs treatment in the first trimester | 51.1% | ?2 = 126.190, P = 0.000 | 31.0% | ?2 = 69.475, P = 0.000 | 10.8% | χ 2 = 8.885, P = 0.003 | 2.4% | χ 2 = 0.020, P = 0.889 |
| High titers (≥1∶8) vs Low titers (<1∶8) | 31.8% | ?2 = 174.840, P = 0.000 | 21.6% | ?2 = 283.664, P = 0.000 | 12.2% | χ 2 = 55.631, P = 0.000 | 5.5% | χ 2 = 13.853, P = 0.000 |
| Gestational week at treatment for women with syphilis | ?2 trend = 140.168, P = 0.000 | ?2 trend = 95.126, P = 0.000 | χ2trend = 12.509, P = 0.000 | χ2trend = 3.402, P = 0.065 | ||||
Selected APOs among women with and without syphilis
The pooled estimates were 20.6% (95%CI: 16.4–25.6) for CS, 14.1% (95%CI: 11.4–17.3) for preterm, 13.2% (95%CI: 9.2–18.5) for low birth weight, 12.5% (95%CI: 10.0–15.5) for stillbirth or early fetal loss, 6.6% (95%CI: 4.7–9.3) for miscarriage and 6.6% (95%CI: 4.1–10.4) for neonatal deaths among mothers with syphilis (Table 2). For mothers without syphilis, the pooled estimates were 7.2% (95%CI: 5.6–9.3) for preterm, 4.5% (95%CI:2.0–10.0) for low birth weight, 3.7% (95%CI: 2.6–5.1) for stillbirth or early fetal loss, 2.3% (95%CI: 1.8–3.0) for miscarriage and 2.0% (95%CI: 1.2–3.3) for neonatal deaths (Table 2). The absolute differences between syphilitic mothers and non-syphilitic mothers for preterm birth (χ 2 = 37.312, P = 0.000), low birth weight (χ 2 = 138.897, P = 0.000), stillbirth or fetal loss (χ 2 = 937.960, P = 0.000), miscarriage (χ 2 = 46.895, P = 0.000), and neonatal death (χ 2 = 124.340, P = 0.000) were 6.9%, 8.7%, 8.8%, 4.3%, and 4.6%, respectively (Table 3 and Table 4). Begg's rank correlation test indicated little evidence of publication bias (P = 0.102 to 0.403) for summary estimates of selected APOs among women with and without syphilis (Table 2). Substantial heterogeneity was found across studies in the estimates of selected adverse outcomes for both women with syphilis (I2 range: 66–95.3%; all P≤0.0002) and women without syphilis (I2 range: 93.5–97.3%; all P<0.0001).
Table 4. Comparison for summary estimates of the proportion (%) of adverse pregnancy outcomes (APOs) among different subgroups.
| Subgroup | Miscarriage | Stillbirth or fetal loss | Neonatal death | |||
| absolute differences | chi-square test | absolute differences | chi-square test | absolute differences | chi-square test | |
| Women with syphilis vs women without syphilis | 4.3% | χ 2 = 46.895, P = 0.000 | 8.8% | χ 2 = 937.960, P = 0.000 | 4.6% | χ 2 = 124.340, P = 0.000 |
| Untreated women with syphilis vs women without syphilis | 12.6% | χ 2 = 106.857, P = 0.000 | 22.7% | ?2 = 2075.991, P = 0.000 | 14.2% | χ 2 = 415.742, P = 0.000 |
| Treatment in the third trimester vs women without syphilis | 17.6% | ?2 = 285.499, P = 0.000 | ||||
| High titers (≥1∶8) vs women without syphilis | 10.9% | ?2 = 135.901, P = 0.000 | 14.0% | χ 2 = 214.264, P = 0.000 | ||
| Untreated women with syphilis vs Treated women with syphilis | 11.3% | χ 2 = 42.433, P = 0.000 | 21.9% | χ 2 = 407.784, P = 0.000 | 13.0% | χ 2 = 41.721, P = 0.000 |
| Treatment in the third trimester vs treatment in the first trimester | 16.0% | χ 2 = 13.714, P = 0.000 | ||||
| High titers (≥1∶8) vs Low titers (<1∶8) | 11.9% | χ 2 = 66.699, P = 0.000 | 15.2% | χ 2 = 100.451, P = 0.000 | ||
| Gestational week at treatment for women with syphilis | χ2trend = 29.633, P = 0.000 | |||||
Subgroup analysis
The subgroup analysis was performed based on clinical characteristics: treatment or not during pregnancy, gestational week at treatment, and baseline titers of nontreponemal antibodies among women with syphilis for all APOs and selected APOs. After subgroup analysis, the heterogeneity was obviously decreased, although there was still significant heterogeneity for most of subgroups.
“untreated women with syphilis” vs “treated women with syphilis”: the pooled estimates were 76.8% (95%CI: 68.8–83.2) for all APOs, 36.0% (95%CI: 28.0–44.9) for CS, 23.2% (95%CI: 18.1–29.3) for preterm, 23.4% (95%CI: 12.8–38.6) for low birth weight, 26.4% (95%CI: 21.9–31.4) for stillbirth or early fetal loss, 14.9% (95%CI: 11.4–19.4) for miscarriage and 16.2% (95%CI: 10.1–25.1) for neonatal deaths among untreated women with syphilis, and in contrast, 24.2% (95%CI: 18.6–30.8) for all APOs, 14.0% (95%CI: 10.5–18.5) for CS, 9.9% (95%CI: 8.6–11.4) for preterm, 6.2% (95%CI: 3.9–9.8) for low birth weight, 4.5% (95%CI: 3.1–6.4) for stillbirth or early fetal loss, 3.6% (95%CI: 2.5–5.1) for miscarriage and 3.2% (95%CI: 1.1–9.1) for neonatal deaths among syphilitic women receiving treatment during pregnancy (Table 5), for the absolute differences of 52.6%, 22.0%, 13.3%, 17.2%, 21.9%, 11.3%, and 13.0% (all P value = 0.0000), respectively (Table 3 and Table 4). Begg's rank correlation test indicated little evidence of publication bias (P = 0.102 to 0.353) for summary estimates of APOs among untreated and treated women with syphilis (Table 5). Compared with women without syphilis, the untreated women with syphilis had significantly higher proportions of pregnancy loss, and the absolute differences were 63.1% for all APOs (χ2 = 3947.821, P = 0.000), 16.0% for preterm (χ2 = 139.350, P = 0.000), 18.9% for low birth weight (χ2 = 110.776, P = 0.000), 22.7% for stillbirth or early fetal loss (χ2 = 2075.991, P = 0.000), 12.6% for miscarriage (χ 2 = 106.857, P = 0.000) and 14.2% for neonatal deaths (χ 2 = 415.742, P = 0.000) (Table 3 and Table 4).
Table 5. Subgroup analysis based on treatment or not in pregnancy for the proportion (%) of adverse pregnancy outcomes (APOs) among syphilis-infected women.
| Treatment or not in pregnancy | Reported proportion in the original studies | APOs | n | No. of included studies | Summary estimates (95%CI)# | Heterogeneity | Bias assessment | |
| Range | M (IQR) | |||||||
| Untreated women with syphilis | ||||||||
| All APOs | 13.9%–100.0% | 82.7% (89.5%–70.4%) | 1611 | 2651 | 32 | 76.8% (95%CI: 68.8%–83.2%) | I2 = 92.7%, P<0.0001 | P = 0.207 |
| Congenital syphilis | 2.2%–81.8% | 34.4% (68.3%–23.7%) | 887 | 3240 | 33 | 36.0% (95%CI: 28.0%–44.9%) | I2 = 92.9%, P<0.0001 | P = 0.117 |
| Preterm birth | 3.0%–62.5% | 18.2% (28.7%–12.6%) | 179 | 932 | 25 | 23.2% (95%CI: 18.1%–29.3%) | I2 = 6.6%, P<0.0001 | P = 0.102 |
| Low birth weight | 6.8%–50.0% | 29.6% (32.0%–11.3%) | 63 | 403 | 8 | 23.4% (95%CI: 12.8%–38.6%) | I2 = 81.3%, P<0.0001 | P = 0.104 |
| Miscarriage | 6.1%–29.4% | 16.0% (20.0%–7.9%) | 46 | 343 | 10 | 14.9% (95%CI: 11.4%–19.4%) | I2 = 26.4%, P = 0.2012 | P = 0.172 |
| Stillbirth or fetal loss | 7.1%–66.7% | 25.0% (42.1%–17.2%) | 660 | 3001 | 31 | 26.4% (95%CI: 21.9%–31.4%) | I2 = 81.8%, P<0.0001 | P = 0.202 |
| Neonatal death | 1.3%–60.0% | 15.2% (25.9%–7.4%) | 117 | 910 | 16 | 16.2% (95%CI: 10.1%–25.1%) | I2 = 81.5%, P<0.0001 | P = 0.212 |
| Treated women with syphilis* | ||||||||
| All APOs | 2.4%–54.4% | 24.5% (38.2%–15.9%) | 767 | 3711 | 36 | 24.2% (95%CI: 18.6%–30.8%) | I2 = 92.5%, P<0.0001 | P = 0.353 |
| Congenital syphilis | 0.7%–50.8% | 13.9% (21.9%–8.2%) | 621 | 4975 | 35 | 14.0% (95%CI: 10.5%–18.5%) | I2 = 91.1%, P<0.0001 | P = 0.303 |
| Preterm birth | 4.7%–23.3% | 14.6% (32.6%–6.0%) | 180 | 2060 | 28 | 9.9% (95%CI: 8.6%–11.4%) | I2 = 43.1%, P = 0.0089 | P = 0.170 |
| Low birth weight | 2.2%–15.3% | 6.3% (10.7%–2.3%) | 72 | 1457 | 10 | 6.2% (95%CI: 3.9%–9.8%) | I2 = 70.4%, P = 0.0004 | P = 0.139 |
| Miscarriage | 2.1%–6.2% | 4.0% (5.6%–3.2%) | 29 | 862 | 7 | 3.6% (95%CI: 2.5%–5.1%) | I2 = 0%, P = 0.6896 | P = 0.107 |
| Stillbirth or fetal loss | 1.1%–13.5% | 3.4% (8.6%–2.0%) | 98 | 2661 | 24 | 4.5% (95%CI: 3.1%–6.4%) | I2 = 58.5%, P = 0.0002 | P = 0.219 |
| Neonatal death | 1.0%–10.3% | 4.6% (8.1%–1.1%) | 9 | 446 | 5 | 3.2% (95%CI: 1.1%–9.1%) | I2 = 59.0%, P = 0.0449 | P = 0.111 |
M = Median; IQR = Inter-quartile range; APOs = adverse pregnancy outcomes; CI = Confidence interval.
Summary estimates and their corresponding 95% CI were calculated using either fixed-effects models or, in the presence of heterogeneity, random-effects models.
*Syphilitic women receiving at least one injection of 2.4 million units of penicillin before delivery.
“treatment in the third trimester” vs “treatment in the first trimester”: the pooled estimates of all APOs, CS, preterm, low birth weight, and stillbirth or early fetal loss were 64.4% (95%CI: 45.2–79.8), 40.6% (95%CI: 31.3–50.7), 17.6% (95%CI: 11.4–26.5), 12.4% (95%CI: 5.9–24.2), and 21.3% (95%CI: 17.2–26.0), respectively among women with syphilis receiving treatment in the third trimester (i.e.>28 weeks), and 13.3% (95%CI: 7.7–21.8), 10.4% (95%CI: 7.7–14.0), 6.8% (95%CI: 3.7–12.2), 10.0% (95%CI: 2.5–32.4), and 5.3% (95%CI: 2.2–12.1), respectively among syphilitic women who got treatment in the first trimester (i.e.≤12 weeks) (Table 6), for the absolute differences of 51.1% (P = 0.000), 31.1% (P = 0.000), 10.8% (P = 0.003), 2.4% (P = 0.889), and 16.0% (P = 0.000), respectively (Table 3 and Table 4). Begg's rank correlation test indicated little evidence of publication bias (P = 0.101 to 0.134) for summary estimates of APOs among women with syphilis according to gestational week at treatment (Table 6). Compared with non-syphilitic women (Table 3 and Table 4), the syphilis-infected women who received treatment in the third trimester also had evidently increased proportions of adverse outcomes, and the absolute differences were 50.7% for all APOs (χ2 = 727.296, P = 0.000), 10.4% for preterm (χ2 = 24.696, P = 0.000), 7.9% for low birth weight (χ2 = 28.440, P = 0.000), and 17.6% for stillbirth or early fetal loss (χ2 = 285.499, P = 0.000).
Table 6. Subgroup analysis based on gestational week at treatment for the proportion (%) of adverse pregnancy outcomes (APOs) among syphilis-infected women.
| Gestational week at treatment | Reported proportion in the original studies | APOs | n | No. of included studies | Summary estimates (95%CI)# | Heterogeneity | Bias assessment | |
| Range | M (IQR) | |||||||
| Treatment in the first trimester (≤12 weeks) | ||||||||
| All APOs | 6.5%–36.0% | 8.2% (20.6%–6.8%) | 37 | 277 | 8 | 13.3% (95%CI: 7.7%–21.8%) | I2 = 59.8%, P = 0.0149 | P = 0.114 |
| Congenital syphilis | 2.9%–20.8% | 8.2% (9.4%–5.4%) | 39 | 416 | 8 | 10.4% (95%CI: 7.7%–14.0%) | I2 = 32.8%, P = 0.1662 | P = 0.105 |
| Preterm birth | 2.8%–12.0% | 6.5% (11.0%–3.5%) | 10 | 172 | 5 | 6.8% (95%CI: 3.7%–12.2%) | I2 = 0%, P = 0.5053 | P = 0.110 |
| Low birth weight | 2 | 20 | 1 | 10.0% (95%CI: 2.5%–32.4%) | ||||
| Stillbirth or fetal loss | 4.1%–8.0% | 6.1% | 5 | 99 | 2 | 5.3% (95%CI: 2.2%–12.1%) | I2 = 0%, P = 0.4445 | |
| Treatment in the second trimester (12–28 weeks) | ||||||||
| All APOs | 15.6%–65.1 | 40.0% (63.6%–22.6%) | 138 | 447 | 7 | 37.8% (23.7%–54.3%) | I2 = 88.7%, P<0.0001 | P = 0.102 |
| Congenital syphilis | 3.2%–44.7% | 19.1% (27.8%–8.7%) | 249 | 1359 | 13 | 17.6% (95%CI: 11.8%–25.4%) | I2 = 84.1%, P<0.0001 | P = 0.114 |
| Preterm birth | 2.5%–25.0% | 9.7% (19.6%–6.0%) | 32 | 379 | 5 | 10.1% (95%CI: 5.2%–18.5%) | I2 = 65%, P = 0.0220 | P = 0.101 |
| Low birth weight | 1.7%–15.0% | 5 | 140 | 2 | 5.3% (95%CI: 0.6%–35.8%) | I2 = 83.6%, P = 0.0136 | ||
| Stillbirth or fetal loss | 1.7%–7.1% | 6.5% | 6 | 179 | 3 | 4.2% (95%CI: 1.9%–9.1%) | I2 = 27.2%, P = 0.2522 | P = 0.103 |
| Ttreatment in the third trimester (>28 weeks) | ||||||||
| All APOs | 12.0%–100.0% | 68.2% (94.4%–34.5%) | 292 | 540 | 11 | 64.4% (95%CI: 45.2%–79.8%) | I2 = 91.6%, P<0.0001 | P = 0.116 |
| Congenital syphilis | 18.2%–83.3% | 45.0% (60.0%–26.5%) | 428 | 1454 | 15 | 40.6% (95%CI: 31.3%–50.7%) | I2 = 87%, P<0.0001 | P = 0.131 |
| Preterm birth | 5.3%–35.0% | 20.6% (26.9%–12.9%) | 65 | 447 | 7 | 17.6% (95%CI: 11.4%–26.5%) | I2 = 69.2%, P = 0.0035 | P = 0.134 |
| Low birth weight | 3.4%–26.9% | 12.8% (23.9%–5.2%) | 26 | 236 | 4 | 12.4% (95%CI: 5.9%–24.2%) | I2 = 66.1%, P = 0.0315 | P = 0.101 |
| Stillbirth or fetal loss | 17.7%–40.0% | 22.9% (27.7%–18.9%) | 71 | 336 | 6 | 21.3% (95%CI: 17.2%–26.0%) | I2 = 0%, P = 0.8177 | P = 0.107 |
M = Median; IQR = Inter-quartile range; APOs = adverse pregnancy outcomes; CI = Confidence interval.
Summary estimates and their corresponding 95% CI were calculated using either fixed-effects models or, in the presence of heterogeneity, random-effects models.
“high titers” vs “low titers”: the pooled estimates were 42.8% (95%CI: 26.2–61.2) for all APOs, 25.8% (95%CI: 15.4–40.1) for CS, 15.1% (95%CI: 5.2–36.9) for preterm, 9.4% (95%CI: 2.7–27.5) for low birth weight, 14.6% (95%CI: 6.5–29.7) for stillbirth or early fetal loss and 16.0% (95%CI: 12.0–21.1) for neonatal deaths among syphilitic women with high titers, and 11.0% (95%CI: 6.3–18.5) for all APOs, 4.2% (95%CI: 1.9–9.1) for CS, 2.9% (95%CI: 0.8–10.2) for preterm, 3.9% (95%CI: 2.7–5.5) for low birth weight, 2.7% (95%CI: 0.4–15.3) for stillbirth or early fetal loss and 0.8% (95%CI: 0.1–10.2) for neonatal deaths among syphilitic women with low titers (Table 7), for the absolute differences of 31.8% (χ2 = 174.840, P = 0.000), 21.6% (χ2 = 283.664, P = 0.000), 12.2% (χ 2 = 55.631, P = 0.000), 5.5% (χ 2 = 13.853, P = 0.000), 11.9% (χ 2 = 66.699, P = 0.000), and 15.2% (χ 2 = 100.451, P = 0.000), respectively (Table 3 and Table 4). Begg's rank correlation test indicated little evidence of publication bias (P = 0.102 to 0.210) for summary estimates of APOs among women with syphilis according to baseline titers of nontreponemal antibodies (Table 7).Similarly, when compared with women without syphilis, the syphilitic women with high titers also had significantly higher proportions of all APOs (all P value = 0.0000), preterm, low birth weight, stillbirth or early fetal loss as well as neonatal deaths, and the absolute differences were 29%, 8%, 4%, 13%, and 14%, respectively (Table 3 and Table 4).
Table 7. Subgroup analysis based on baseline titers of nontreponemal antibodies for the proportion (%) of adverse pregnancy outcomes (APOs) among syphilis-infected women.
| Maternal baseline titers of nontreponemal antibodies | Reported proportion in the original studies | APOs | n | No. of included studies | Summary estimates (95%CI)# | Heterogeneity | Bias assessment | |
| Range | M (IQR) | |||||||
| Low titers (<1∶8) | ||||||||
| All APOs | 3.7%–24.1% | 9.3% (21.9%–4.9%) | 114 | 1215 | 6 | 11.0% (95%CI: 6.3%–18.5%) | I2 = 87%, P<0.0001 | P = 0.131 |
| Congenital syphilis | 0.2%–21.9% | 4.1% (14.0%–1.3%) | 251 | 3085 | 8 | 4.2% (95%CI: 1.9%–9.1%) | I2 = 94.4%, P<0.0001 | P = 0.210 |
| Preterm birth | 0.5%–9.3% | 3.6% (8.3%–0.9%) | 32 | 998 | 3 | 2.9% (95%CI: 0.8%–10.2%) | I2 = 88%, P<0.0001 | P = 0.130 |
| Low birth weight | 3.4%–5.2% | 3.7% | 31 | 813 | 3 | 3.9% (95%CI: 2.7%–5.5%) | I2 = 0%, P = 0.5164 | P = 0.127 |
| Stillbirth or fetal loss | 0.7%–7.8% | 3.7% | 20 | 813 | 3 | 2.7% (95%CI: 0.4%–15.3%) | I2 = 89.9%, P<0.0001 | P = 0.102 |
| Neonatal death | 0.2%–2.6% | 1.4% | 4 | 708 | 2 | 0.8% (95%CI: 0.1%–10.2%) | I2 = 82.5%, P = 0.0167 | |
| High titers (≥1∶8) | ||||||||
| All APOs | 15.2%–73.7% | 49.3% (63.9%–21.9%) | 182 | 510 | 6 | 42.8% (95%CI: 26.2%–61.2%) | I2 = 92.2%, P<0.0001 | P = 0.111 |
| Congenital syphilis | 2.2%–72.2% | 25.2% (40.7%–15.8%) | 325 | 1161 | 8 | 25.8% (95%CI: 15.4%–40.1%) | I2 = 94.4%, P<0.0001 | P = 0.152 |
| Preterm birth | 2.2%–37.5% | 20.0% (34.4%–5.5%) | 51 | 359 | 3 | 15.1% (95%CI: 5.2%–36.9%) | I2 = 91.8%, P<0.0001 | P = 0.112 |
| Low birth weight | 4.5%–24.7% | 6.3% | 32 | 347 | 3 | 9.4% (95%CI: 2.7%–27.5%) | I2 = 90.9%, P<0.0001 | P = 0.105 |
| Stillbirth or fetal loss | 6.2%–34.2% | 12.8% (29.2%–7.6%) | 57 | 383 | 3 | 14.6% (95%CI: 6.5%–29.7%) | I2 = 88%, P<0.0001 | P = 0.105 |
| Neonatal death | 15.2%–18.1% | 16.7% | 40 | 250 | 2 | 16.0% (95%CI: 12.0%–21.1%) | I2 = 0%, P = 0.5733 | |
M = Median; IQR = Inter-quartile range; APOs = adverse pregnancy outcomes; CI = Confidence interval.
Summary estimates and their corresponding 95% CI were calculated using either fixed-effects models or, in the presence of heterogeneity, random-effects models.
Discussion
In the present study, we quantified the proportion of all APOs and specific APOs among syphilis-infected women and non-syphilitic women using data from fifty-four studies that met eligibility criteria for inclusion in our systematic review and meta-analysis and involved 11398 women with syphilis and 43342 women without syphilis. In the context of WHO's global initiative for the elimination of CS and National Program for Prevention and Control of Syphilis in China (2010–2020), this study could supply helpful information to both clinical doctors and infected mothers, and help to assess progress in elimination of MTCT of syphilis and to guide policy and advocacy efforts. To our knowledge, this is the first time that the epidemic of APOs among women with syphilis was exhaustively reviewed based on clinical features by meta-analysis.
Findings from present study further confirmed the ancient tune that MTCT of syphilis undoubtedly brings about a heavy burden to society. Notwithstanding being easily detectable and treatable in pregnancy, presently, syphilis remains an important cause of birth loss [1], [20], [24]. On average, our review showed that APOs accounted for significantly higher proportions among the offspring of syphilis-infected mothers than among the offspring of mothers without syphilis, especially among syphilis-infected women who didn't receive treatment during pregnancy, or who did not receive treatment until the third trimester, or who had high baseline titers.
Previous studies have confirmed that lack of treatment or postponement of gestational week for first treatment and high baseline titers were independent risk factors of APOs among syphilitic mothers [1], [25]. Our study indicates that, unless testing and treatment of syphilis in pregnancy are universally available, over half of pregnancies in women with syphilis will result in an adverse outcome. In general, our estimates are consistent with previously published data. In order to block MTCT of syphilis and support the global initiative for elimination of CS, WHO has developed 2008 worldwide estimates of maternal syphilis and associated APOs, which indicated that, globally, 520,905 adverse outcomes were estimated to be caused by maternal syphilis, including approximately 212,327 stillbirths or early fetal deaths, 91,764 neonatal deaths, 65,267 preterm or low birth weight infants, and 151,547 infected newborns [9]. Furthermore, WHO also revealed that approximately 66% of adverse outcomes occurred in antenatal care (ANC) attendees who were not tested or were not treated for syphilis, and in 2008, based on the middle case scenario, clinical services likely averted 26% of all APOs [9]. The latest meta-analysis by Gomez et al. [8] showed that approximately 52% of pregnancies in mothers with untreated or inadequately treated syphilis result in some APOs, with estimated proportions: early fetal loss or stillbirth (21%), neonatal death (9%), low birth weight or premature birth (6%), and infection in a live-born infant (15%). Berman [26] indicated that if left untreated, maternal syphilis infection will, in up to 80% of pregnancies, lead to severely APOs, including stillbirth, premature birth, neonatal death, or congenital infection in the newborn. Qin JB et al. [1] confirmed that for mothers who did not receive complete treatment during pregnancy, 18.5% delivered an infant with CS and 48.1% resulted in APOs. It has been estimated that the numbers of fetal/neonatal deaths in Africa each year from untreated maternal syphilis could rival those from HIV infections [27].
Both previous studies and present review indicated that improving quality of ANC is a key point to eliminate MTCT of syphilis and reduce the risk of APOs among women with syphilis. This highlights the importance of absent or insufficient ANC as an independent risk factor for pregnancy loss among syphilis-infected mothers. ANC is not only the best opportunity to treat maternal syphilis, but it is also important for the control of a woman who had received documented adequate treatment for syphilis before pregnancy, and is necessary for the interpretation of a positive serologic test at delivery [28]. Screening and treatment of syphilis during pregnancy is considered to be simple, cheap, and highly cost-effective in prevention of MTCT of syphilis. For these reasons, screening pregnant women during their first ANC is recommended by the WHO [29]. However, presently, approximately one-fifth (20%) of all pregnant women with syphilis did not attend ANC [9]. It is also recognized that the effectiveness of screening and treatment is lower in the third trimester than in the first and second trimesters [30]. Given that screening and treatment for preventing MTCT of syphilis is not 100% effective, primary prevention of syphilis in pregnant women is also an important strategy that needs to be addressed to truly eliminate MTCT of syphilis. Although substantial progress has been made in the utilization of ANC (in 2009 WHO estimated that approximately 81% of all pregnant women had attended at least one ANC visit [9]), MTCT of syphilis occurred for a variety of reasons: many of these visits were too late to avert an adverse outcome, clinics may not have offered testing, testing may not have been affordable, women may not have followed up or received their test results, treatment may not have been available, or treated women may have been reinfected by untreated sexual partners [31].
Our estimates are subject to certain limitations that should be considered when interpreting the results. Firstly, all studies included in our review had an observational design, and most belonged to a retrospective cases analysis. Owing to the inherent differences between experimental and observational study designs and to biases commonly seen in observational data, appropriate caution should be taken in interpreting our results. Nevertheless, an advantage of this review is that we included a comparison group to assess APOs among mothers without syphilis. This gave us the opportunity to estimate the excess adverse outcomes in the presence of maternal syphilis and give a broad idea of the risk of some of the pregnancy loss in syphilis-infected women. Secondly, there was also unacceptable heterogeneity in estimates across studies. We tried to find the sources of heterogeneity by subgroup analysis. After subgroup analysis, the heterogeneity was obviously decreased. However, our estimates have to be viewed with caution because of heterogeneity. Thirdly, because variations in the definition of APOs exist across countries and cultures, it is extremely difficult to define uniform standards. The early literatures did not always define birth outcomes and in such cases we relied on the outcome terminology in the original papers. So the misclassification of APOs may influence the results. Last but not least, our relatively strict inclusion criteria might have introduced selection bias. In present analysis, we only included studies published in Chinese or English language. So the additional research in other populations is warranted to generalize the findings. The limitations of these estimates highlight the urgent need for improved data through stronger national surveillance and monitoring systems.
In summary, present study indicates that syphilis continues to be an important cause of substantial numbers of perinatal deaths and disabilities that could be prevented by early testing and treatment, and also reminds policy-makers charged with resource allocation that the elimination of MTCT of syphilis is a public health priority. Most adverse outcomes occurred among women who were not treated for syphilis or who receiving treatment only in the late trimester or who had high baseline titers. High quality of ANC highlighting early testing and treatment is the only effective means to block MTCT of syphilis. Health education for pregnant women should continue to reinforce the message that untreated maternal syphilis is a danger to the unborn infant, that syphilis can be diagnosed and treated, and that women should attend an antenatal that can perform syphilis screening as soon as they suspect that they are pregnant. Systematic attention to testing, treatment, education, and contact tracing in pregnancy and subsequent late trimester retesting of women at high risk will lower pregnancy loss.
Supporting Information
PRISMA checklist.
(DOC)
PRISMA Flow Diagram.
(DOC)
Acknowledgments
Authors thank editors and reviewers for their suggestions.
Funding Statement
JBQ was supported by the Fundamental Research Funds for Central South University (2012zzts029) and the Hunan Province Innovation Projects (CX2012B076) of China. This work was also supported by the Program of Prevention of Mother-to-Children Transmission of Syphilis in Shenzhen, China. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Qin J, Feng TJ, Yang TB, Hong FC, Lan L, et al. (2014) Risk Factors for Congenital Syphilis and Adverse Pregnancy Outcomes in Offspring of Women With Syphilis in Shenzhen, China: A Prospective Nested Case-Control Study. Sex Transm Dis 41: 13–23. [DOI] [PubMed] [Google Scholar]
- 2. De Santis M, De Luca C, Mappa I, Spagnuolo T, Licameli A, et al. (2012) Syphilis Infection during pregnancy: fetal risks and clinical management. Infect Dis Obstet Gynecol 2012: 430585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hawkes S, Matin N, Broutet N, Low N (2011) Effectiveness of interventions to improve screening for syphilis in pregnancy: a systematic review and meta-analysis. Lancet Infect Dis 11: 684–91. [DOI] [PubMed] [Google Scholar]
- 4. Terris-Prestholt F, Watson-Jones D, Mugeye K, Kumaranayake L, Ndeki L, et al. (2003) Is antenatal syphilis screening still cost effective in sub-Saharan Africa. Sex Transm Infect 79: 375–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kuznik A, Lamorde M, Nyabigambo A, Manabe YC (2013) Antenatal Syphilis Screening Using Point-of-Care Testing in Sub-Saharan African Countries: A Cost-Effectiveness Analysis. PLoS Med 10: e1001545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization (2007) The global elimination of congenital syphilis: rationale and strategy for action. Geneva: World Health Organization. Available: http://www.who.int/reproductivehealth/publications/rtis/9789241595858/en/index.html.
- 7.China Ministry of Health (2010) Notice of the Ministry of Health on Issuing National Program for Prevention and Control of Syphilis in China (2010–2020). Available: http://www.gov.cn/gzdt/2010-06/21/content_1632301.htm.
- 8. Gomez GB, Kamb ML, Newman LM, Mark J, Broutet N, et al. (2013) Untreated maternal syphilis and adverse outcomes of pregnancy: a systematic review and meta- analysis. Bull World Health Organ 91: 217–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Newman L, Kamb M, Hawkes S, Gomez G, Say L, et al. (2013) Global estimates of syphilis in pregnancy and associated adverse outcomes: analysis of multinational antenatal surveillance data. PLoS Med 10: e1001396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, et al. (2000) Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA 283: 2008–12. [DOI] [PubMed] [Google Scholar]
- 11. Moher D, Liberati A, Tetzlaff J, Altman DG (2009) PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harman NB (1917) Staying the plague. London: Methuen & Co.
- 13. Wammock V (1950) Penicillin therapy of the syphilitic pregnant woman: its practical application to a large urban obstetrical service. Am J Obstet Gynecol 59: 806–17. [Google Scholar]
- 14. Ingraham NRJ Jr (1950) The value of penicillin alone in the prevention and treatment of congenital syphilis. Acta Derm Venereol Suppl (Stockh) 31: 60–87. [PubMed] [Google Scholar]
- 15. Hira SK, Bhat GJ, Chikamata DM, Nkowane B, Tembo G, et al. (1990) Syphilis intervention in pregnancy: Zambian demonstration project. Genitourin Med 66: 159–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. McDermott J, Steketee R, Larsen S, Wirima J (1993) Syphilis-associated perinatal and infant mortality in rural Malawi. Bull World Health Organ 71: 773–80. [PMC free article] [PubMed] [Google Scholar]
- 17. McFarlin BL, Bottoms SF (1995) Maternal syphilis in Michigan: the challenge to prevent congenital syphilis. Midwifery 11: 55–60. [DOI] [PubMed] [Google Scholar]
- 18. Temmerman M, Gichangi P, Fonck K, Apers L, Claeys P, et al. (2000) Effect of a syphilis control programme on pregnancy outcome in Nairobi, Kenya. Sex Transm Infect 76: 117–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Watson-Jones D, Gumodoka B, Weiss H, Changalucha J, Todd J, et al. (2002) Syphilis in pregnancy in Tanzania. II.The effectiveness of antenatal syphilis screening and single dose benzathine penicillin treatment for the prevention of adverse pregnancy outcomes. J Infect Dis 186: 948–57. [DOI] [PubMed] [Google Scholar]
- 20. Watson-Jones D, Changalucha J, Gumodoka B, Weiss H, Rusizoka M, et al. (2002) Syphilis in pregnancy in Tanzania.I. Impact of maternal syphilis on outcome of pregnancy. J Infect Dis 186: 940–7. [DOI] [PubMed] [Google Scholar]
- 21. Tikhonova L, Salakhov E, Southwick K, Shakarishvili A, Ryan C, et al. (2003) Congenital syphilis in the Russian Federation: magnitude, determinants, and consequences. Sex Transm Infect 79: 106–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Liu JB, Hong FC, Pan P, Zhou H, Yang F, et al. (2010) A risk model for congenital syphilis in infants born to mothers with syphilis treated in gestation: a prospective cohort study. Sex Transm Infect 86: 292–6. [DOI] [PubMed] [Google Scholar]
- 23. Zhu L, Qin M, Du L, Xie RH, Wong T, et al. (2010) Maternal and congenital syphilis in Shanghai, China, 2002 to 2006. Int J Infect Dis 14: e45–8. [DOI] [PubMed] [Google Scholar]
- 24. Qin JB, Feng TJ, Yang TB, Hong FC, Lan LN, et al. (2014) Maternal and paternal factors associated with congenital syphilis in Shenzhen, China: a prospective cohort study. Eur J Clin Microbiol Infect Dis 33: 221–32. [DOI] [PubMed] [Google Scholar]
- 25. Deperthes BD, Meheus A, O′Reilly K, Broutet N (2004) Maternal and congenital syphilis programmes: Case studies in Bolivia, Kenya and South Africa. Bull World Health Organ 82: 410–6. [PMC free article] [PubMed] [Google Scholar]
- 26. Berman SM (2004) Maternal syphilis: pathophysiology and treatment. Bull World Health Organ 82: 433–8. [PMC free article] [PubMed] [Google Scholar]
- 27. Gloyd S, Chai S, Mercer MA (2001) Antenatal syphilis in sub-Saharan Africa: missed opportunities for mortality reduction. Health Policy Plan 16: 29–34. [DOI] [PubMed] [Google Scholar]
- 28. Lago EG, Rodrigues LC, Fiori RM, Stein AT (2004) Congenital syphilis: identification of two distinct profiles of maternal characteristics associated with risk. Sex Transm Dis 31: 33–37. [DOI] [PubMed] [Google Scholar]
- 29. Saloojee H, Velaphi S, Goga Y, Afadapa N, Steen R, et al. (2004) The prevention and management of congenital syphilis: an overview and recommendations. Bull World Health Organ 82: 424–430. [PMC free article] [PubMed] [Google Scholar]
- 30. Hawkes S, Gomez G, Broutet N (2013) Early antenatal care: does it make a difference to outcomes of pregnancy associated with syphilis? A systematic review and meta-analysis. PLoS ONE 8: e56713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kamb ML, Newman LM, Riley PL, Mark J, Hawkes SJ, et al. (2010) A road map for the global elimination of congenital syphilis. Obstet Gynecol Int 2010: 312798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Li J, Huang CX, Zeng Y, Yang X, Kong X, et al. (2001) Syphilis in pregnancy women. Chin J Obstet Gynecol 36: 456–459. [PubMed] [Google Scholar]
- 33. Xu Y, Lu XY, Ling Y (2001) Treatment of syphilis in pregnancy and its perinatal prognosis. Chin J Obstet Gynecol 36: 460–461. [PubMed] [Google Scholar]
- 34. Lin XH, Wu JJ, Wen JY (2002) Clinical analysis of 41 cases of syphilis during pregnancy. Chin J Healthy Birth & Child Care 13: 3–5. [Google Scholar]
- 35. Fang SN, Zheng LX, Du XH, Tong QS, Li FJ (2003) Effect of pregnancy complicated syphilis on perinatal prognosis. Chin J Public Health 19: 546–547. [Google Scholar]
- 36. Wang HB, Qiu J, Pan Q (2003) Treatment of maternal syphilis and its effect on adverse birth outcomes. JOURNAL OF TONGJI UNIVERSITY(MEDICAL SCIENCE) 24: 449–451. [Google Scholar]
- 37. Kuang YB (2004) The significance of syphilis serial test on pregnant women. Chin Modern Hospital 4: 49–50. [Google Scholar]
- 38. Xu YX, Fang SN, Cai WD (2004) Analysis on epidemic character and prognosis of pregnancy companied with syphilis. Chin Modern Preventive Medicine 31: 411–412. [Google Scholar]
- 39. Zhang XM, Zhang RN, Lin SX, Chen SX, Zhen LY (2004) Clinical analysis of 192 pregnant women infected by syphilis. Clin J Obstet Gynecol 39: 682–686. [PubMed] [Google Scholar]
- 40. Li Q, Huang SR, Wang JW (2005) Affects on gravidas and neonates in cases of late pregnancy complicating with latent syphilis. Maternal and Child Health Care of China 20: 1477–1478. [Google Scholar]
- 41. Zhou H, Pan P, Hong FC, Chen G, Yang F, et al. (2006) Risk factors in association with congenital syphilis. Chin J Dermatol 39: 681–684. [Google Scholar]
- 42. Gao H, Xi HF, He ZJ (2006) Pregnancy selection of women with syphilis. Journal of Guangdong Medical College 24: 596–597. [Google Scholar]
- 43. Wang CX, Zhou XL, Kong X (2006) Maternal syphilis and its treatment. Medical Journal of the Chinese People's Armed Police Force 17: 212–214. [Google Scholar]
- 44. Xuan QS, Zhang XX, Jiang M, Xiao X, Zhou XG (2006) Perinatal outcomes of 286 pregnant women with syphilis treated by benzylpenicillin at different gestations. Chin J Perinat Med 9: 400–403. [Google Scholar]
- 45. Zheng RQ, Wei P, Zhao YQ (2006) Clinical significance in early treatment of syphilis in pregnant women. Chin Modern Preventive Medicine 33: 1035–1036. [Google Scholar]
- 46. Wang X, Liu CF, Xiang XG (2007) Analysis of relationship between treatment of gestational patients complicated with syphilis and perinatal prognosis. Chin Tropical Medicine 7: 951–952. [Google Scholar]
- 47. Sun LL, Chen Y, Zhang P (2008) Penicillin treatment of syphilis in pregnancy and its pregnancy outcomes. Chin J Birth Health & Heredity 16: 81–82. [Google Scholar]
- 48. Gao JM, Li FW, Zhang GF (2009) Analysis of pregnancy outcomes among women with syphilis. Chin J Birth Health & Heredity 17: 81–82. [Google Scholar]
- 49. Huang ZM, Zhou JH, Lou RH, Zhang L, Chen Y, et al. (2009) Impact of TRUST titers and antenatal intervention on incidence of syphilis. Chin Tropical Medicine 9: 1408–1410. [Google Scholar]
- 50. Li L, Liu M, Wang F, Zhang XX (2009) Clinical analysis on 121 pregnant women infected by syphilis. Maternal and Child Health Care of China 24: 4087–4088. [Google Scholar]
- 51. Wu FY, Song J (2009) Treatment of maternal syphilis and adverse pregnancy outcomes. Journal of Zhejiang University of Traditional Chinese Medicine 33: 833. [Google Scholar]
- 52. Zhou GJ, Cong L, Qiu LX, Yao J, Tao RX (2009) Pregnancy outcomes of women with syphilis. Anhui Medicine Journal 30: 308–310. [Google Scholar]
- 53. Chen JH (2010) A discussion of relationship between maternal syphilis and adverse pregnancy outcomes. Chin J Practical Preventive Medicine 17: 1815. [Google Scholar]
- 54. Li TH, Shao LY, Wang R, Yi XM, Wang LH, et al. (2010) The Clinical Analysis of 168 pregnant syphilis patients from 2006 to 2009 in Huhhot. Inner Mongolia Med J 42: 1053–1055. [Google Scholar]
- 55. Shuang JY, Shuang WB (2010) Effect of anti-syphilis treatment and TRUST serum titers on pregnancy outcomes. J Shanxi College of Traditional Chinese Medicine 11: 63–65. [Google Scholar]
- 56. Ye GR, Zhang W, Huang XX (2010) Study on the effect of different curative opportunities on the prognosis of pregnant syphilis. J Military Surgeon in Southwest China 12: 1059–1060. [Google Scholar]
- 57. Dai Y (2011) The relationship between pregnancy syphilis treatment timing and pregnancy outcomes. Chin J Clinical Medicine in Practice 15: 142–143. [Google Scholar]
- 58. Li Z, Tian LS, Luo ZZ, Zhou GM, Yuan J, et al. (2011) Correlation of pregnant syphilis with congenital syphilis. Chin Tropical Medicine 11: 1383–1385. [Google Scholar]
- 59. Luo ZZ, Tian LS, Zhou GM, Yuan J, Yang ZQ, et al. (2011) Risk factors of adverse pregnancy outcome in 227 pregnant patients with syphilis. Chin J Practical Preventive Medicine 18: 1625–1627. [Google Scholar]
- 60. Wang WL, Yang DQ, Ying CX (2011) A analysis of the relationship between treatment of maternal syphilis and adverse pregnancy outcomes. Chin J Rural Medicine and Pharmacy 18: 24–25. [Google Scholar]
- 61. Yuan XQ, Zhou M, He KJ (2011) The impact of different treatment time for maternal syphilis on adverse pregnancy outcomes. Guide of China Medicine 9: 135–136. [Google Scholar]
- 62. Cao DH (2012) Pregnant women with syphilis in Zhongshan city in 2005 to 2010: A clinical analysis of 41 cases. China Modern Doctor 50: 49–50. [Google Scholar]
- 63. Chen GJ, Liu Y, Liu JB, Ma L, Zhang XP, et al. (2012) Adverse pregnancy outcomes in gravidas with syphilis treated during gestation. Chin J Derm Venereol 26: 321–323. [Google Scholar]
- 64. Deng JF, Dai L (2012) Relationship of Treatment Factors and Pregnancy Outcome in 58 Cases of Syphilis in Pregnant Women. Medical Innovation of China 9: 31–32. [Google Scholar]
- 65. Li HS, Tan C, Cao G, Lu JM (2012) Risk factors of mother-to-child transmission of syphilis. Maternal and Child Health Care of China 27: 1496–1498. [Google Scholar]
- 66. Li Z (2012) Treatment time for maternal syphilis and adverse pregnancy outcomes. Guide of China Medicine 10: 227–228. [Google Scholar]
- 67. Pan P, Cai YM, Lu FQ, Hong FC (2012) Effect of benzathine penicillin on pregnant syphilis patients. Chin Tropical Medicine 12: 725–727. [Google Scholar]
- 68. Xu ZY, Qiu LX, Li P, Zhu H, Liang YF, et al. (2012) Retrospective study of 772 pregnant women on the effectiveness of mother-to-child transmission-blocking of syphilis. Chin J Derm Venereol 26: 720–722. [Google Scholar]
- 69. Cui L (2013) Clinical significance of treatment for maternal syphilis. Chin J of Clinical Rational Drug Use 6: 85. [Google Scholar]
- 70. Shi J, Diao YT, Li XW (2013) Study on the pregnancy outcomes and prognosis of different curative opportunities on pregnant syphilis. Chin J Derm Venereol 27: 274–276. [Google Scholar]
- 71. Wei HP, Zhong YJ (2013) Treatment for pregnant syphilis and its effect on perinatal outcomes. Journal of Hainan Medical University 19: 381–383. [Google Scholar]
- 72. Wu FY (2013) Clinical analysis on prognosis of different curative opportunities on maternal syphilis. Chinese and Foreign Medical Research 11: 128. [Google Scholar]
- 73. Xu ZY, Wu MF (2013) Effect of standard treatment for syphilis on pregnancy outcomes. Journal of Jilin University 1: 33. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA checklist.
(DOC)
PRISMA Flow Diagram.
(DOC)