Abstract
Mutations in proteins of the desmosome associate with arrhythmogenic cardiomyopathy (AC; also referred to as “ARVC” or “ARVD”). Life-threatening ventricular arrhythmias often occur in the concealed phase of the disease before the onset of structural changes. Among the various potential mechanisms for arrhythmogenesis in AC, in this article we concentrate on the relation between desmosomes and sodium channel function. We review evidence indicating that: 1) loss of desmosomal integrity (including mutations or loss of expression of plakophilin-2; PKP2) leads to reduced sodium current (INa). 2) The PKP2-INa relation could be partly consequent to the fact that PKP2 facilitates proper trafficking of proteins to the intercalated disc 3) PKP2 mutations can be present in patients diagnosed with Brugada syndrome (BrS), thus supporting the previously-proposed notion that AC and BrS are not two completely separate entities, but “bookends” in a continuum of variable sodium current deficiency and structural disease.
Introduction
The intercalated disc embodies the physical continuum between cardiac myocytes, allowing for intercellular communication and synchronization of mechanical and electrical activity. Desmosomes and adherens junctions provide cell-cell adhesion, while gap junctions support electrical coupling. In addition to these electron-dense structures, the intercalated disc hosts a number of other molecular aggregates, necessary for electrical and metabolic function. Of particular relevance to this article is the voltage-gated sodium channel (VGSC) complex, responsible for the rapid depolarization of the cell. For years, the structures of the intercalated disc were considered separate and independent. Moreover, with a few exceptions, the general view was that each molecule had a single function: Connexin43 as the integral component of gap junctions; PKP2 as a scaffold of the desmosome; NaV1.5 as the pore-forming subunit of the sodium channel. The emerging concept, however, is that the components of one structure are not independent from the others. Rather, they interact and work together as part of a “connexome,” a protein interacting network that regulates excitability, cell-cell adhesion and intercellular coupling in the heart. In the present article, we will concentrate on the desmosome and the interaction of its molecular components with the voltage-gated sodium channel (VGSC). Our research seeks a better understanding of arrhythmia mechanisms, and novel ways for diagnosis and risk stratification, in patients suspect or affected with Arrhythmogenic Cardiomyopathy (AC) or with Brugada Syndrome (BrS). The similarities between these two diseases will be discussed.
The desmosome
The desmosome is an electron dense structure formed at a site of cell-cell apposition and constituted by a complex of transmembrane and scaffolding proteins that work together to provide a point of anchoring for intermediate filaments, and a point of adhesion between cells (Redden and Dodge-Kafka, 2011; Tasken et al., 2001). Desmosomal cadherins (desmocollin and desmoglein), bind tightly to each other in the extracellular space, while in the intracellular space the intermediate filament desmin binds to desmoplakin; the interaction between desmoplakin and the desmosomal cadherins occurs mostly through their association with plakophilin and plakoglobin (Bass-Zubek et al., 2008; Redden and Dodge-Kafka, 2011; Tasken et al., 2001).
Mutations in molecules of the desmosome and Arrhythmogenic Cardiomyopathy
Loss of integrity of the desmosome leads to a cardiac disease called “arrhythmogenic cardiomyopathy” or “AC.” (Also called “arrhythmogenic right ventricular cardiomyopathy,” or “arrhythmogenic right ventricular dysplasia,” hence the abbreviations “ARVD” “ARVC” or ARVC/D” found in the literature to refer to this disease)(Basso et al., 2012; van der Zwaag et al., 2009). Approximately 50-70% of the cases of familial AC associate with a mutation in a desmosomal gene(Cox et al., 2011; Marcus et al., 2009). This condition presents with a progressive fibro-fatty infiltration, often (but not always) more prominent in the right ventricular myocardium, and with a high propensity to life-threatening ventricular arrhythmias and progression toward heart failure(Basso et al., 2012). It is considered one of the most relevant causes of juvenile sudden cardiac death, especially in competitive athletes, and its prevalence ranges from 1:2000 to 1:5000(Basso et al., 2009).
The structural changes that affect the myocardium are thought to play an important role in facilitating arrhythmia occurrence in the setting of overt cardiomyopathy. However, it is worth noting that cases of sudden cardiac death, likely due to ventricular fibrillation, sometimes occur in the very early stage of the disease when the macroscopical structural damage is not evident and in fact, sudden cardiac death is the first clinical manifestation of the disease in 20-50% of the index cases, also occurring in the presence of well preserved ventricular function (reviewed in (Sen-Chowdhry et al., 2010)). Investigators have therefore sought to identify molecular pathways by which a mutated desmosomal protein could alter the electrical behavior of the heart. The current view is that molecules of the desmosome interact with gap junctions and with the VGSC, and that failure of these interactions can create a substrate for arrhythmias, particularly in this early phase of the disease (Fig1). Due to space limitations, we concentrate on the desmosome-VGSC interaction. Yet we emphasize that sodium current is unlikely to be the only pro-arrhythmic factor involved. Sodium current itself is not necessarily proarrhythmic and the potential contributing roles of structural changes, altered connexin expression and coupling, and perhaps additional electrophysiological factors, should not be ignored and in fact are somewhat expected, given that these molecules are part of a common protein interacting network (the connexome). The relation between desmosomes and gap junctions has been discussed in several original and review articles(Delmar and McKenna, 2010; Kaplan et al., 2004).
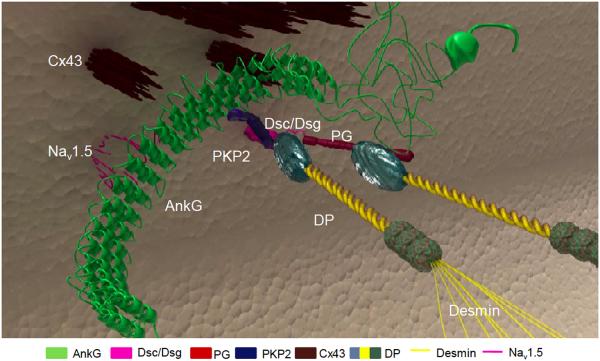
Figure 1.
Diagram illustrating the potential interactions between the voltage-gated sodium channel complex (VGSC), gap junctions and desmosomes. AnkG: ankyrin-G; DSC/Dsg: desmocolin/desmoglein; PG:plakoglobin; PKP2:plakophilin-2; Cx43: connexin43; DP: desmoplakin Reproduced with permission from Sato et al, 2011.
Plakophilin-2 regulates cardiac sodium channel function
Early studies showed that the VGSC resides preferentially at the cardiac intercalated disc(Cohen, 1996; Kucera et al., 2002) and that it can co-precipitate with Cx43 and with Ncadherin(Malhotra et al., 2004). We therefore explored if disruption of desmosomal integrity could alter sodium current (INa). Our studies focused on the desmosomal protein PKP2, given that a) PKP2 mutations are the most common variant in AC(van Tintelen et al., 2006) and b) early-onset ventricular fibrillation and sudden death in the absence of an overt structural cardiomyopathy are often found in PKP2 mutations carriers(van Tintelen et al., 2006). In the first demonstration of a relation between desmosomes and INa, Sato et al(Sato et al., 2009) showed that in cardiac myocytes lacking PKP2, INa was significantly decreased (Fig2). Furthermore, loss of PKP2 expression in cardiac myocytes led to decreased abundance of immunoreactive Nav1.5 (the α-subunit of the VGSC) at sites of cell contact, and optical mapping experiments showed increased reentrant activity and significantly decreased conduction velocity in the absence of PKP2, when compared to controls(Sato et al., 2009). A subsequent study showed that the cytoskeletal adaptor protein Ankyrin-G (AnkG) may play a key role in allowing for the interaction between three molecular components previously considered independent: the desmosome, the gap junction, and the VGSC complex (Fig. 1) (Sato et al., 2011). These observations, limited to the cellular/molecular experiments, prompted us to investigate the susceptibility to VGSC-dependent arrhythmias in hearts deficient in PKP2.
Figure 2.
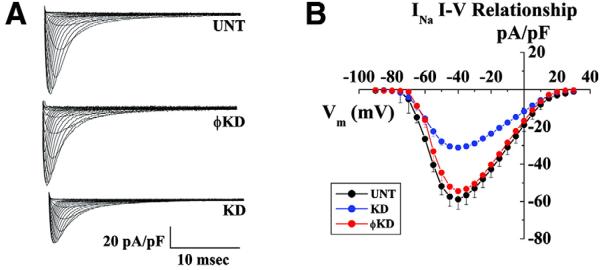
Voltage clamp data from adult rat cardiomyocytes after PKP2 knockdown (KD) and comparison with cells untreated (UNT) or treated with nonsilencing constructs (ΦKD) as control. A: Examples of sodium current recorded in the three conditions. B: Current- voltage relation for the groups described in A. Reproduced with permission from Sato et al, 2009.
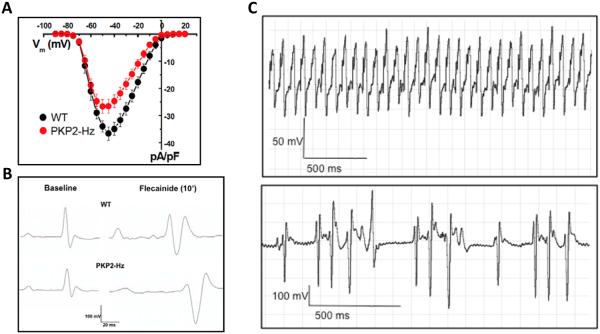
Decreased PKP2 abundance facilitates INa-dependent lethal arrhythmias in vivo
In the vast majority of familial cases where a genetic link is found, AC presents as an autosomal dominant disease. We therefore studied a mouse model with PKP2 haplo-insufficiency (PKP2-Hz), which mimics the clinical situation of patients harboring stop-codon mutations that truncate the protein early in its sequence (such as R79x), with an expected ~50% of PKP2 availability(Cerrone et al., 2012). The mouse model did not show signs of structural cardiomyopathy. Nav1.5 protein abundance was not altered and yet, INa amplitude in isolated ventricular cardiomyocytes was significantly decreased. Furthermore, there was a shift in gating and INa kinetics when compared to wild-type cardiomyocytes(Cerrone et al., 2012). Thus, intrinsic, genetically mediated partial loss of PKP2 reduced INa amplitude to an extent compatible to that observed in cells after loss of PKP2 expression.
To further unmask the consequences of INa deficit, we challenged PKP2-Hz mice with the sodium channel blocker flecainide. Compared to controls, PKP2-Hz animals showed increased sensitivity to drug-induced prolongation of atrial and ventricular conduction time, and decreased conduction velocities in Langendorff-perfused isolated hearts. Furthermore, flecainide injection in vivo caused ventricular arrhythmias and some cases of sudden death in PKP2-Hz animals but not in wild-types(Cerrone et al., 2012) (Fig 3). These results show that PKP2 haploinsufficiency causes reduced INa in murine hearts, documenting for the first time the functional relationship between PKP2 and VGSC in vivo. Whether flecainide would aid in the evaluation of the arrhythmia risk in patients suspect of AC is an interesting area that deserves further investigation.
Figure 3.
Decreased sodium current, conduction defects and ventricular arrhythmias in a mouse model with PKP2 haploinsufficiency (PKP2-Hz). A: sodium current amplitude recorded from PKP2-Hz and control (WT) isolated ventricular myocytes. B: ECG recorded from a wild-type (WT) and PKP2-Hz anesthetized animal in baseline (left) and 10 minutes after flecainide infusion C: Examples of ventricular arrhythmias elicited by flecainide infusion in PKP2-Hz mice. Reproduced with permission from Cerrone et al, 2012.
Additional studies on the relation between desmosomal integrity and the VGSC complex
Separate studies have confirmed the relation between desmosomal integrity, and the structure and/or function of the VGSC. Rizzo et al showed prolonged ventricular activation time, decreased conduction velocity, decreased upstroke velocity and decreased INa amplitude in mice over-expressing a mutation in desmoglein-2(Rizzo et al., 2012). Gomes et al(Gomes et al., 2012) reported that patients with AC harboring desmoplakin-2 mutations showed regional conduction delay in the right ventricle and heterogeneous Nav1.5 distribution. In addition, in a collaborative immunohistochemistry study(Noorman et al., 2013) on heart samples from patients with AC, Noorman et al showed that in most cases, Nav1.5 was reduced at the intercalated disc, even if the distribution of the N-cadherin signal remained normal. Finally, reduced INa amplitude has been observed in PKP2-deficient HL1 cells and in induced pluripotent stem cell-derived cardiomyocytes (iPSC-CMs) from a patient with PKP2 deficiency(Cerrone et al., 2013; Kim et al., 2013). Altogether, the evidence overwhelmingly supports the notion that the amplitude of the sodium current in cardiac myocytes is decreased if desmosomal integrity is disrupted, and that such a disruption can contribute to the arrhythmogenic substrate in patients with AC.
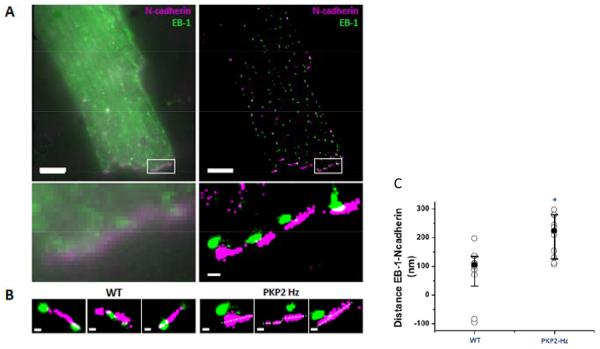
Proposed mechanism of action: PKP2 deficiency impairs microtubule capture and NaV1.5 delivery to the intercalated disc
Our experiments demonstrated that both in vitro and in vivo decreased PKP2 results in decreased amplitude of cardiac INa, without changing Nav1.5 protein abundance detected by western blot. To investigate its mechanism, we used macropatch as well as super-resolution (SR) microscopy methods(Agullo-Pascual et al., 2013; Bhargava et al., 2013; Lin et al., 2011). Macropatch recordings of PKP2-Hz myocytes showed that INa amplitude was reduced only from the region of the intercalated disc. SR- scanning patch clamp revealed that the decreased INa at the intercalated disc was not consequent to reduced single channel unitary conductance. Super-resolution fluorescence microscopy, based on direct stochastic optical reconstruction microscopy revealed that reduced PKP2 abundance correlated with increased distance between the microtubule plus-end tracking protein EB1, and N-cadherin rich sites(Cerrone et al., 2013) (Fig 4). We therefore propose that PKP2 is part of the molecular complex that captures the microtubule plus-end at the intercalated disc, thus allowing for delivery of its cargo, including Nav1.5(Casini et al., 2010; Shaw et al., 2007). Further experiments will be necessary to address this possibility.
Figure 4.
Localization of EB-1 (green) and N-cadherin (purple) in adult mouse ventricular myocytes. A: Image by TIRF (left) or dSTORM (right). Inset enlarged in bottom panels to show increased resolution. B: Comparison between wild type and PKP2-Hz myocytes: clusters in WT (left) are closer to each other than in PKP2-Hz cells (right). C: Dot plot of distance from EB-1 to N-cadherin showing increased separation between the proteins in the PKP2-Hz cells. Reproduced with permission from Cerrone et al, 2013.
It is important to note that loss of PKP2 expression in ventricular myocytes (but not in HL1 cells) also alters gating and kinetics of INa(Sato et al., 2009). This effect cannot be explained by impaired trafficking. Instead, we speculate that it results from the interaction of NaV1.5 with other ancillary molecules that are present (or not) in the particular cell type and in the particular subdomain where the pore-forming protein is expressed. Indeed, we previously showed that the voltage gating of TTX-sensitive channels in adult ventricular myocytes (likely formed mostly –if not only- by NaV1.5) varies depending on the recording site (cell end versus cell midsection; see(Lin et al., 2011)); the latter likely reflects modulation of INa by location-specific partners (see also(Petitprez et al., 2011; Shy et al., 2013). Studies in expression systems have also shown that sodium channel beta subunits modify sodium current behavior(Maltsev et al., 2009), and that the expression and/or phosphorylation state of beta subunits in cardiac myocytes is not homogeneous(Malhotra et al., 2004).These results show that molecular partners that can be abundant in one cell or in one cell region, and absent in another, can change the gating behavior of the same pore-forming protein. Reduced PKP2 expression can modify the interaction of Nav1.5 with other partners that impact on gating properties.
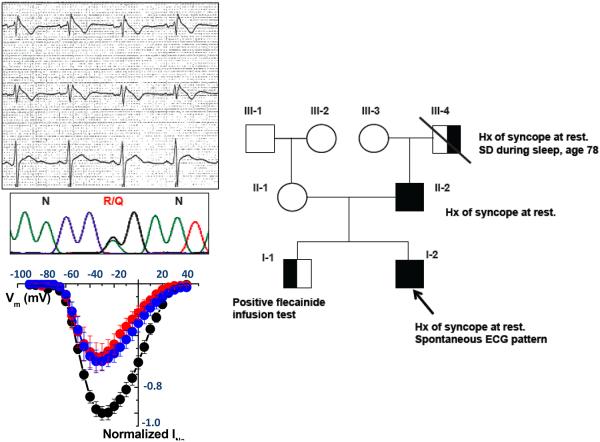
Missense mutations in PKP2 and decreased INa: the link to Brugada Syndrome
Our experiments in PKP2-Hz mice suggested an enhanced sensitivity to pharmacological sodium channel block in the presence of reduced PKP2. Flecainide infusion is a pharmacological challenge used to unmask ECG changes in patients affected with “Brugada Syndrome” (BrS)(Antzelevitch et al., 2005), an inherited channelopathy presenting with a characteristic ECG morphology, i.e. coved ST segment elevation in the right precordial leads, life-threatening ventricular arrhythmias and high risk of sudden cardiac death in the absence of structural cardiomyopathy(Antzelevitch et al., 2005; Priori et al., 2013). A genetic mutation is found in ~30% of clinically diagnosed patients(Ackerman et al., 2011). Of those, most mutations are found in the gene encoding for Nav1.5, and it is generally accepted that arrhythmias in BrS are associated with decreased depolarization reserve(Ackerman et al., 2011). The relation between PKP2 and INa described in the paragraphs above led us to speculate that, if a PKP2 mutation primarily impacts INa function (rather than desmosomal structure), its presence would manifest in a manner clinically similar to BrS. Interestingly, after the initial description of BrS, Corrado et al suggested that this condition could share several clinical features with AC, implying that these were not completely distinct clinical entities(Corrado et al., 2001; Corrado et al., 1999).
We screened by direct sequencing a cohort of 200 patients with clinical diagnosis of BrS and no mutations on the most prevalent genes. We discovered five single amino acid substitutions in five unrelated patients(Cerrone et al., 2013). In order to assess if these missense variants in PKP2 could affect the cardiac INa, we used an HL-1 cell line, stably silenced for the endogenous PKP2. In the absence of PKP2, these cells showed a decrease in endogenous INa. As illustrated in Fig. 5, cells transiently transfected with each one of the PKP2 mutants associated with the BrS phenotype showed significantly decreased INa, when compared with cells transfected with wild type PKP2(Cerrone et al., 2013). Similar results were obtained when we used a line of human iPSC-derived cardiomyocytes from a patient lacking PKP2 at the cell membrane(Awad et al., 2006; Kim et al., 2013). In these cells, INa increased upon transfection with wild type PKP2. Transfection with one of the PKP2 mutants associated with BrS was not able to restore normal INa (Cerrone et al., 2013). These data represent the first evidence that missense mutations in PKP2 can cause a decrease in cardiac INa. When combined with other factors (such as decreased electrical coupling and/or fibrosis), a reduction in INa could facilitate the development of arrhythmias, even in the absence of a structural cardiomyopathy. We propose that PKP2 mutations provide at least part of the molecular substrate of BrS. The inclusion of PKP2 as part of routine BrS genetic testing remains premature; yet, the possibility that some patients showing signs of disease may harbor PKP2 variants should be considered when the genotype is negative for other genes associated with BrS.
Figure 5.
PKP2 mutations associate with Brugada Syndrome and with reduced sodium current. Top left: Representative ECG showing ST elevation, diagnostic for Brugada Syndrome, in one of the five patients carriers of missense mutations on the PKP2 gene, and correspondent electropherograms showing the specific amino acid substitution R635Q. Bottom left: Sodium current amplitude recorded in HL1 cells silenced for PKP2 (PKP2-KD) transfected with the mutant (red), an empty vector (blue) or wild type PKP2 (black). Right: pedigree of the family showing co-segregation between the PKP2 mutation and the clinical phenotype. Reproduced with permission from Cerrone et al, 2013.
Conclusions
We have provided an overview showing that molecules classically defined as belonging to the desmosome interact with the VGSC complex. The association between PKP2 expression and INa has been demonstrated in neonatal and adult ventricular myocytes after PKP2 silencing(Sato et al., 2011; Sato et al., 2009), in HL1 cells stably knocked down for PKP2(Cerrone et al., 2013), in ventricular myocytes from mice heterozygous-null for PKP2(Cerrone et al., 2012) and in human iPSC-CMs obtained from a patient with PKP2 deficiency(Cerrone et al., 2013). The sodium current deficiency has been demonstrated to increase the susceptibility to flecainide-induced arrhythmias in experimental animals(Cerrone et al., 2012), and we have provided evidence showing that the microtubule network is at the crux of the interaction between PKP2, and the VGSC complex(Cerrone et al., 2013). Finally, we summarize recent results indicating that PKP2 mutations in humans may coincide with a BrS phenotype. AC and BrS may not be two completely separate clinical entities, but “bookends” in a continuum of graded sodium current deficiency and structural disease.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCE LIST
- Ackerman MJ, Priori SG, Willems S, et al. HRS/EHRA expert consensus statement on the state of genetic testing for the channelopathies and cardiomyopathies this document was developed as a partnership between the Heart Rhythm Society (HRS) and the European Heart Rhythm Association (EHRA) Heart rhythm. 2011;8:1308–1339. doi: 10.1016/j.hrthm.2011.05.020. [DOI] [PubMed] [Google Scholar]
- Agullo-Pascual E, Reid DA, Keegan S, et al. Super-resolution fluorescence microscopy of the cardiac connexome reveals plakophilin-2 inside the connexin43 plaque. Cardiovascular research. 2013;100:231–240. doi: 10.1093/cvr/cvt191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antzelevitch C, Brugada P, Borggrefe M, et al. Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation. 2005;111:659–670. doi: 10.1161/01.CIR.0000152479.54298.51. [DOI] [PubMed] [Google Scholar]
- Awad MM, Dalal D, Tichnell C, et al. Recessive arrhythmogenic right ventricular dysplasia due to novel cryptic splice mutation in PKP2. Human mutation. 2006;27:1157. doi: 10.1002/humu.9461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bass-Zubek AE, Hobbs RP, Amargo EV, et al. Plakophilin 2: a critical scaffold for PKC alpha that regulates intercellular junction assembly. The Journal of cell biology. 2008;181:605–613. doi: 10.1083/jcb.200712133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basso C, Bauce B, Corrado D, Thiene G. Pathophysiology of arrhythmogenic cardiomyopathy. Nature reviews. Cardiology. 2012;9:223–233. doi: 10.1038/nrcardio.2011.173. [DOI] [PubMed] [Google Scholar]
- Basso C, Corrado D, Marcus FI, Nava A, Thiene G. Arrhythmogenic right ventricular cardiomyopathy. Lancet. 2009;373:1289–1300. doi: 10.1016/S0140-6736(09)60256-7. [DOI] [PubMed] [Google Scholar]
- Bhargava A, Lin X, Novak P, et al. Super-resolution scanning patch clamp reveals clustering of functional ion channels in adult ventricular myocyte. Circulation research. 2013;112:1112–1120. doi: 10.1161/CIRCRESAHA.111.300445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casini S, Tan HL, Demirayak I, et al. Tubulin polymerization modifies cardiac sodium channel expression and gating. Cardiovascular research. 2010;85:691–700. doi: 10.1093/cvr/cvp352. [DOI] [PubMed] [Google Scholar]
- Cerrone M, Lin X, Zhang M, et al. Missense Mutations in Plakophilin-2 Cause Sodium Current Deficit and Associate with a Brugada Syndrome Phenotype. Circulation. 2013 doi: 10.1161/CIRCULATIONAHA.113.003077. e pub ahead of print Dec 18 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerrone M, Noorman M, Lin X, et al. Sodium current deficit and arrhythmogenesis in a murine model of plakophilin-2 haploinsufficiency. Cardiovascular research. 2012;95:460–468. doi: 10.1093/cvr/cvs218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen SA. Immunocytochemical localization of rH1 sodium channel in adult rat heart atria and ventricle. Presence in terminal intercalated disks. Circulation. 1996;94:3083–3086. doi: 10.1161/01.cir.94.12.3083. [DOI] [PubMed] [Google Scholar]
- Corrado D, Basso C, Buja G, Nava A, Rossi L, Thiene G. Right bundle branch block, right precordial stsegment elevation, and sudden death in young people. Circulation. 2001;103:710–717. doi: 10.1161/01.cir.103.5.710. [DOI] [PubMed] [Google Scholar]
- Corrado D, Buja G, Basso C, Nava A, Thiene G. What is the Brugada syndrome? Cardiology in review. 1999;7:191–195. doi: 10.1097/00045415-199907000-00010. [DOI] [PubMed] [Google Scholar]
- Cox MG, van der Zwaag PA, van der Werf C, et al. Arrhythmogenic right ventricular dysplasia/cardiomyopathy: pathogenic desmosome mutations in index-patients predict outcome of family screening: Dutch arrhythmogenic right ventricular dysplasia/cardiomyopathy genotype-phenotype follow-up study. Circulation. 2011;123:2690–2700. doi: 10.1161/CIRCULATIONAHA.110.988287. [DOI] [PubMed] [Google Scholar]
- Delmar M, McKenna WJ. The cardiac desmosome and arrhythmogenic cardiomyopathies: from gene to disease. Circulation research. 2010;107:700–714. doi: 10.1161/CIRCRESAHA.110.223412. [DOI] [PubMed] [Google Scholar]
- Gomes J, Finlay M, Ahmed AK, et al. Electrophysiological abnormalities precede overt structural changes in arrhythmogenic right ventricular cardiomyopathy due to mutations in desmoplakin-A combined murine and human study. European heart journal. 2012;33:1942–1953. doi: 10.1093/eurheartj/ehr472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan SR, Gard JJ, Protonotarios N, et al. Remodeling of myocyte gap junctions in arrhythmogenic right ventricular cardiomyopathy due to a deletion in plakoglobin (Naxos disease) Heart rhythm. 2004;1:3–11. doi: 10.1016/j.hrthm.2004.01.001. [DOI] [PubMed] [Google Scholar]
- Kim C, Wong J, Wen J, et al. Studying arrhythmogenic right ventricular dysplasia with patient-specific iPSCs. Nature. 2013;494:105–110. doi: 10.1038/nature11799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kucera JP, Rohr S, Rudy Y. Localization of sodium channels in intercalated disks modulates cardiac conduction. Circulation research. 2002;91:1176–1182. doi: 10.1161/01.res.0000046237.54156.0a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin X, Liu N, Lu J, et al. Subcellular heterogeneity of sodium current properties in adult cardiac ventricular myocytes. Heart rhythm. 2011;8:1923–1930. doi: 10.1016/j.hrthm.2011.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malhotra JD, Thyagarajan V, Chen C, Isom LL. Tyrosine-phosphorylated and nonphosphorylated sodium channel beta1 subunits are differentially localized in cardiac myocytes. The Journal of biological chemistry. 2004;279:40748–40754. doi: 10.1074/jbc.M407243200. [DOI] [PubMed] [Google Scholar]
- Maltsev VA, Kyle JW, Undrovinas A. Late Na+ current produced by human cardiac Na+ channel isoform Nav1.5 is modulated by its beta1 subunit. The journal of physiological sciences : JPS. 2009;59:217–225. doi: 10.1007/s12576-009-0029-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus FI, Zareba W, Calkins H, et al. Arrhythmogenic right ventricular cardiomyopathy/dysplasia clinical presentation and diagnostic evaluation: results from the North American Multidisciplinary Study. Heart rhythm. 2009;6:984–992. doi: 10.1016/j.hrthm.2009.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noorman M, Hakim S, Kessler E, et al. Remodeling of the cardiac sodium channel, connexin43, and plakoglobin at the intercalated disk in patients with arrhythmogenic cardiomyopathy. Heart rhythm. 2013;10:412–419. doi: 10.1016/j.hrthm.2012.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petitprez S, Zmoos AF, Ogrodnik J, et al. SAP97 and dystrophin macromolecular complexes determine two pools of cardiac sodium channels Nav1.5 in cardiomyocytes. Circulation research. 2011;108:294–304. doi: 10.1161/CIRCRESAHA.110.228312. [DOI] [PubMed] [Google Scholar]
- Priori SG, Wilde AA, Horie M, et al. HRS/EHRA/APHRS Expert Consensus Statement on the Diagnosis and Management of Patients with Inherited Primary Arrhythmia Syndromes: Document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart rhythm. 2013;10:1932–1963. doi: 10.1016/j.hrthm.2013.05.014. [DOI] [PubMed] [Google Scholar]
- Redden JM, Dodge-Kafka KL. AKAP phosphatase complexes in the heart. Journal of cardiovascular pharmacology. 2011;58:354–362. doi: 10.1097/FJC.0b013e31821e5649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizzo S, Lodder EM, Verkerk AO, et al. Intercalated disc abnormalities, reduced Na(+) current density, and conduction slowing in desmoglein-2 mutant mice prior to cardiomyopathic changes. Cardiovascular research. 2012;95:409–418. doi: 10.1093/cvr/cvs219. [DOI] [PubMed] [Google Scholar]
- Sato PY, Coombs W, Lin X, et al. Interactions between ankyrin-G, Plakophilin-2, and Connexin43 at the cardiac intercalated disc. Circulation research. 2011;109:193–201. doi: 10.1161/CIRCRESAHA.111.247023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato PY, Musa H, Coombs W, et al. Loss of plakophilin-2 expression leads to decreased sodium current and slower conduction velocity in cultured cardiac myocytes. Circulation research. 2009;105:523–526. doi: 10.1161/CIRCRESAHA.109.201418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen-Chowdhry S, Morgan RD, Chambers JC, McKenna WJ. Arrhythmogenic cardiomyopathy: etiology, diagnosis, and treatment. Annual review of medicine. 2010;61:233–253. doi: 10.1146/annurev.med.052208.130419. [DOI] [PubMed] [Google Scholar]
- Shaw RM, Fay AJ, Puthenveedu MA, von Zastrow M, Jan YN, Jan LY. Microtubule plus-end-tracking proteins target gap junctions directly from the cell interior to adherens junctions. Cell. 2007;128:547–560. doi: 10.1016/j.cell.2006.12.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shy D, Gillet L, Abriel H. Cardiac sodium channel NaV1.5 distribution in myocytes via interacting proteins: the multiple pool model. Biochimica et biophysica acta. 2013;1833:886–894. doi: 10.1016/j.bbamcr.2012.10.026. [DOI] [PubMed] [Google Scholar]
- Tasken KA, Collas P, Kemmner WA, Witczak O, Conti M, Tasken K. Phosphodiesterase 4D and protein kinase a type II constitute a signaling unit in the centrosomal area. The Journal of biological chemistry. 2001;276:21999–22002. doi: 10.1074/jbc.C000911200. [DOI] [PubMed] [Google Scholar]
- van der Zwaag PA, Jongbloed JD, van den Berg MP, et al. A genetic variants database for arrhythmogenic right ventricular dysplasia/cardiomyopathy. Human mutation. 2009;30:1278–1283. doi: 10.1002/humu.21064. [DOI] [PubMed] [Google Scholar]
- van Tintelen JP, Entius MM, Bhuiyan ZA, et al. Plakophilin-2 mutations are the major determinant of familial arrhythmogenic right ventricular dysplasia/cardiomyopathy. Circulation. 2006;113:1650–1658. doi: 10.1161/CIRCULATIONAHA.105.609719. [DOI] [PubMed] [Google Scholar]