Abstract
This study examined the associations between prenatal exposure to cocaine and other substances and child internalizing behavior problems at Kindergarten. We investigated whether maternal harshness or cumulative environmental risk mediated or moderated this association. Participants consisted of 216 (116 cocaine exposed, 100 non-cocaine exposed) mother-infant dyads participating in an ongoing longitudinal study of prenatal cocaine exposure. Results indicated that, as hypothesized, maternal harshness moderated the association between prenatal cocaine exposure to child internalizing in Kindergarten such that prenatal cocaine exposure increased risk for internalizing problems at high levels of maternal harshness from 7 to 36 months and decreased risk at low levels of harshness. Contrary to hypothesis, the association between prenatal cocaine exposure and child internalizing in Kindergarten was not mediated by maternal harshness or cumulative environmental risk. However, cumulative environmental risk (from 1 month of child age to Kindergarten) was predictive of child internalizing behavior problems at Kindergarten. Results have implications for parenting interventions that may be targeted toward reducing maternal harshness in high risk samples characterized by maternal substance use in pregnancy.
Keywords: Internalizing Behavior Problems, Maternal Harshness, Cocaine exposure
1. Introduction
Prenatal cocaine exposure (CE) has an inhibitory effect on the reuptake of monoamines in the presynaptic junction, leading to an increased concentration of these neurotransmitters in the synaptic cleft and higher activation in the central catecholaminergic systems (Gawin & Ellinwood, 1988; Mayes, 2002). It has been noted that these physiological consequences may be one mechanism for the association between prenatal CE and alterations in arousal, attention, and reactivity to stress. Indeed, recent studies of functional neural activity indicated significantly greater prefrontal activation for CE children compared to controls during a working memory task in the context of high negative emotional arousal, but not under emotionally neutral conditions (Li et al., 2009; Li et al., 2011), suggesting alterations in attentional or regulatory mechanisms in response to negative emotional arousal. Given the risk for prenatal cocaine exposure to alter arousal regulatory systems, a number of studies have hypothesized direct associations between prenatal CE and the development of internalizing behavior problems (Bada et al., 2011; Richardson, Goldschmidt, & Wilford, 2009). However, with the exception of one study reporting a significant association between first trimester cocaine use and internalizing behavior problems at 3 years of child age (Richardson et al., 2009) and one resporting associations between level of cocaine use (none, some, high) and internalizing problemsat 3 and 5 years, most studies have reported non-significant associations from 4 to 13 years of child ages (Accornero, Morrow, Bandstra, Johnson, & Anthony, 2002; Accornero, Anthony, Morrow, Xue, & Bandstra, 2006; Bada et al., 2011; Bennett, Bendersky, & Lewis, 2002; Lester et al., 2009; Yumoto, Jacobson, & Jacobson, 2008).
Instead, most have reported associations between internalizing sympotomatology and other environmental risk variables such as maternal psychological distress (Accornero et al., 2002), caregiver depression (Bada et al., 2011; Bennett et al., 2002), violence (Bada et al., 2011), and cumulative environmental risk (Yumoto et al., 2008) among cocaine exposed cohorts. However, these risk factors often co-occur (Sameroff, Seifer, Baldwin, & Baldwin, 1993) and may be best characterized as cumulative environmental risk for internalizing behavior problems among children. This cumulative environmental risk could be conceptualized as a mediator or intervening variable between the association between prenatal CE and internalizing behavior problems or alternatively as moderating the association between CE and internalizing behavior problems.
With respect to mediation, the literature on maternal substance use indicates that these women are at particularly high risk for experiencing greater psychological distress (Eiden, Foote, & Schuetze, 2007) and violent encounters due to vulnerability to victimization (Eiden, Peterson, & Coleman, 1999), unstable relationships (Lynch & Cicchetti, 1998), and residence in high-risk neighborhoods (Osofsky, Wewers, Hann, & Fick, 1993). Child exposure to violence is subsequently associated with higher risk for internalizing behavior problems across multiple studies (Huang, Wang, & Warrener, 2010; Oravecz, Osteen, Sharpe, & Randolph, 2011). Similarly, higher maternal psychological distress is a robust prospective predictor of children’s internalizing behavior problems (Connell & Goodman, 2002). Further, the risk of developing internalizing behavior problems in early adolescence has been found to rise with the accumulation of risk factors, such as family psychopathology (Ashford, Lier, Timmermans, Cuijpers, & Koot, 2008). Finally, cocaine exposed children are more likely to experience inconsistent and unstable caregiving with greater likelihood of major separations from primary caregivers and lack of stable caregiving routines compared to non-exposed children (Platzman, Coles, Lynch, Bard, & Brown, 2001). The importance of caregiving stability and reliable family routines for children’s well-being has been well established (Zeanah, 2009). Taken together, these aspects of the caregiving environment are likely to co-occur, are likely to vary as a function of maternal substance use, including cocaine, and are known to have a significant impact on children’s internalizing behavior problems.
In addition to cumulative caregiving environmental risk, the quality of parenting experienced by the child may serve as a proximal mediator or moderator of risk. Maternal cocaine use has the potential to alter parenting behavior. Both animal and human studies indicate that mothers with CE had lower plasma oxytocin (sometimes called the “bonding hormone”) compared to non-substance using mothers (Johns, Lubin, Walker, Meter, & Mason, 1997; Light et al., 2004; McMurray, Cox, et al., 2008). This has been demonstrated to be one mechanism for cocaine effects on maternal caregiving or parenting behavior (Light et al., 2004; McMurray, Joyner, et al., 2008). Animal studies examining the effects of cocaine administration on maternal caregiving behavior consistently report lower caregiving quality across multiple domains (Morrell, Basso, & Pereira, 2011). Similarly, a number of parenting dimensions have been examined in the human literature on CE. Results indicate that cocaine using mothers use fewer positive reinforcements and more threats of physical discipline in the toddler/preschool period (Bauman & Dougherty, 1983); display more harshness during different laboratory based interactions at 2 years of age (Eiden, Schuetze, Colder, & Veira, 2011); and are more hostile and intrusive in a structured teaching situation at 3 years of age (Johnson et al., 2002). This aspect of maternal hostility/harshness has also been associated with higher internalizing problems in childhood and adolescence (Bender et al., 2007; Easterbrooks, Bureau, & Lyons-Ruth, 2012). Thus, maternal hostility or harshness across infancy and toddler years may mediate the association between prenatal CE and internalizing behavior problems in kindergarten.
Environmental risk and maternal harshness may also moderate risk for internalizing behavior problems. Theoretical models such as diathesis-stress or dual risk models of development (Ingram & Luxton, 2005), would suggest that the vulnerability posed by prenatal CE would result in higher internalizing behavior problems only in the context of high environmental risk or high maternal harshness. In addition, theories such as differential susceptibility (Belsky & Pluess, 2009) are particularly useful when considering potential protective effects. This theory would suggest that vulnerability due to prenatal substance exposure may not only increase risk for internalizing behavior problems under conditions of high environmental risk or maternal harshness, but also increase the probability for low internalizing behavior problems in positive environmental and parenting contexts.
Finally, it is important to note that maternal cocaine use is a poly-drug issue. The majority of mothers using cocaine also use other substances such as alcohol, cigarettes, and marijuana (B. M. Lester et al., 2003). Cocaine is often used in combination with marijuana and nicotine and cocaine use is often accompanied by drinking during pregnancy. All of these substances have the potential to alter developmental outcomes (Irner, 2012). Thus, the potential effects of cocaine use can only be examined in the context of other substance use during pregnancy by including exposure to these other substances in model testing.
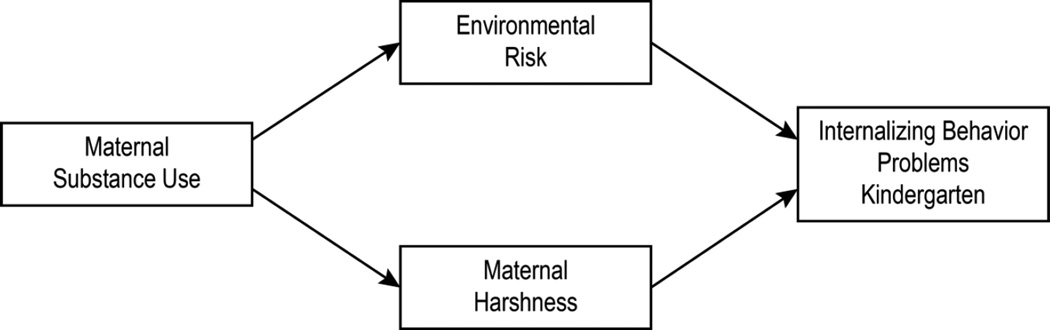
Thus, we examined a conceptual model for development of internalizing behavior problems among cocaine-exposed and demographically similar non-exposed children that included the role of cumulative environmental risk and maternal harshness. In addition to examining potential direct effects of CE on internalizing behavior problems at kindergarten age, two indirect or mediational pathways linking maternal cocaine use to children’s internalizing problems were examined in this study: first, the path from maternal cocaine use → higher maternal harshness from 7 to 36 months → higher internalizing problems in kindergarten or mediation via maternal harshness. Second, the path from maternal cocaine use → higher environmental risk from 1 to 54 months → higher internalizing behavior problems in kindergarten or mediation via environmental risk. Finally, we examined moderation by examining if the association between CE and internalizing problems would be stronger under conditions of higher compared to lower cumulative environmental risk or harsh parenting behavior. We hypothesized that the association between CE and internalizing behavior problems would be stronger under conditions of high environmental risk or high maternal harshness. We examined the role of child gender as a potential moderator of the direct association between CE and internalizing behavior problems. Given the mixed results in prior literature, we did not hypothesize a direction of effect.
2. Material and methods
2.1 Participants
The sample consisted of 216 mother-infant dyads participating in an ongoing longitudinal study of CE (116 cocaine-exposed or CE, 100 not cocaine-exposed or NCE). An outreach worker on the project staff recruited all participants after delivery from two local area hospitals. Mothers ranged in age from 18 to 42 years (M=29.53; SD=6.06). The majority of mothers were African American (72%), were receiving Temporary Assistance for Needy Families (76%) at the time of their first laboratory visit (Years 2001–2004), and were single (66%). Of the 216 children, 106 (49%) were male. All families were recruited from two hospitals serving a predominantly low-income population and the two groups were matched on maternal education, maternal race/ethnicity, and infant gender. Maternal and child assessments were conducted at delivery, 4–8 weeks, 7, 13, 24, 36, and 48 months of child ages, and at kindergarten age. Children born at or before 37 weeks gestation were scheduled for their appointments at chronological age corrected for prematurity until the 24 month assessment. By kindergarten, 55 children in the CE group and 9 children in the NCE group had been removed from parental care and placed in non-parental care at some point between recruitment and kindergarten. All assessments were conducted with the primary caregiver of the child at that time, with the exception of the first assessment when biological mothers were interviewed in addition to the primary caregiver to obtain accurate information about prenatal substance exposure. However, for ease of presentation the terms mother and maternal are used throughout the manuscript when referring to the primary caregiver who was identified as the adult who had legal guardianship of the child and accompanied the child at all appointments. The average child age at kindergarten was 5.52 years (SD = .36, range = 4.8–7.0 years).
2.2 Procedure
All mothers were screened after delivery using a self-report screening form for initial eligibility and matching criteria followed by medical record review. About 2 weeks after delivery, mothers were contacted and scheduled for their first laboratory visit, which took place at the time that their infant was approximately 4–8 weeks old. In the circumstance of a change in custody arrangements, the person who had legal guardianship of the child was contacted and asked to participate. Once a family was recruited into the cocaine group, the closest matching NCE group family (based on maternal education (below high school, high school, above high school), race/ethnicity (White vs. non-White), infant gender) was recruited. However, a significantly higher proportion of mothers in the NCE group declined participation or withdrew before formal enrollment, resulting in a smaller number of families in the control group. Mothers in the comparison group reported not having used any illicit substances other than marijuana. They also tested negative for cocaine or illicit substances other than marijuana based on urine and hair analysis results. Additional exclusionary criteria for all mothers were (a) maternal age younger than 18 years, (b) use of illicit substances other than cocaine or marijuana, and (c) significant medical problems for the infant (e.g., genetic disorders, major perinatal complications, baby in critical care for over 48 hours). Of the women screened at delivery, 126 acknowledged using illicit substances other than cocaine or marijuana at the screening interview and 149 infants had major medical problems. Thus, a total of 275 women were excluded based on these two criteria. Details regarding number of women screened and eligible have been reported in prior publications (e.g., Eiden, Schuetze, & Coles, 2011).
2.3 Assessment of growth and risk status
Three measures of growth were used in this study: birth weight (gm), birth length (cm), and head circumference (cm). All measurements were taken by obstetrical nurses in the delivery room and recorded in the infant’s medical chart. Medical chart review at the time of recruitment also was used to complete the Obstetrical Complications Scale (OCS; Littman & Parmelee, 1978), a scale designed to assess the number of perinatal risk factors experienced by the infant. Higher numbers on this scale indicate lower obstetrical risk. Gestational age was calculated by dates and extracted from medical records.
2.4 Identification of Substance Use
Cocaine status was determined by a combination of maternal report, chart review, and maternal hair analysis. Approximately 90% (n = 195) of infants and mothers in the study had urine samples available for assay and hair samples were collected for all participants. Urine toxicologies consisted of standard urine screening for drug level or metabolites of cocaine, opiates, benzodiazepines, and tetrahydrocannabinol. Urine was rated positive if the quantity of drug or metabolite was >300 g/ ml. Hair samples were collected from the mothers at the first laboratory visit and sent to the Psychemedics Corporation for Radioimmunoanalyses (RIAH). Hair samples were screened for cocaine followed by a gas chromatography/mass spectrometry (GC/MS) confirmation for positive cocaine screens. Approximately 55% of the mothers in the CE group had positive urine toxicologies at delivery, and 79% of the mothers in the CE group had hair samples that tested positive for cocaine during pregnancy. There were 23 mothers in the CE group who did not have a positive toxicology result on any biomarker of cocaine, but all of these mothers admitted to having used cocaine in the brief self-report screening instrument administered after delivery and were assigned to the CE group.
The Timeline Follow-Back Interview (TLFB; Sobell et al., 1986) was used to assess maternal substance use during pregnancy and postnatally. Participants were provided a calendar and asked to identify events of personal interest (i.e., holidays, birthdays, vacations, etc.) as anchor points to aid recall. This method has been established as a reliable and valid method of obtaining longitudinal data on substance-use patterns, has good test-retest reliability, and is highly correlated with other intensive self-report measures (Brown et al., 1998). The TLFB yielded data about the average number of days of cocaine use per week, average number of joints smoked per week, average number of cigarettes smoked per week, and average number of standard drinks per week during pregnancy. Of the 116 mothers in the CE group, 93 (80%) provided data on quantity of use as reported in Table 1. Average number of days per week of cocaine use during pregnancy based on the TLFB ranged from 0 to 6.63 days. Postnatal substance use was computed by taking the average of number of days used cocaine, number of cigarettes per week, number of standard drinks per week, and number of joints per week from the 1, 7, 13, 18, 24, 30, 36, 42, 48, 54 month and kindergarten assessments.
Table 1.
Group Differences in Demographic Variables and Birth Outcomes
| Exposure Group: | Non-Cocaine n = 100 |
Cocaine n = 116 |
F value or χ2 |
ηp2 | ||
|---|---|---|---|---|---|---|
|
M or N(%) |
SD |
M or N(%) |
SD | |||
| Demographics: | ||||||
| BM age | 27.79 | 5.60 | 31.03 | 6.05 | 16.50** | .07 |
| BM parity | 3.17 | 1.64 | 4.16 | 2.42 | 12.50** | .05 |
| Years education | 12.02 | 1.88 | 11.64 | 1.91 | 2.12 | .01 |
| Education < HS | 33(33%) | 53 (46%) | 3.60 | |||
| Occupational Status | 3.38 | 1.83 | 2.78 | 1.32 | 7.92** | .04 |
| TANF Recipient | 73(73%) | 89(77%) | .74 | |||
| Birth outcomes: | ||||||
| Gestational age | 39.33 | 1.25 | 38.62 | 1.82 | 10.84** | .05 |
| Preterm Birth | 3 (3%) | 13 (11%) | 7.76** | |||
| Birth weight | 3334.45 | 503.78 | 2922.72 | 530.76 | 33.87** | .14 |
| Birth length | 48.13 | 3.06 | 49.96 | 2.90 | 20.08** | .09 |
| Head circumference | 33.61 | 1.38 | 33.08 | 2.06 | 4.77** | .02 |
| OCS | 100.81 | 17.30 | 85.30 | 16.34 | 45.83** | .18 |
| Cigarettes/week | 12.89 | 25.85 | 37.86 | 43.45 | 25.29** | .11 |
| Drinks/week | .20 | .82 | 3.72 | 11.27 | 9.74** | .04 |
| Joints/week | .47 | 7.36 | 1.29 | 4.14 | .05 | .00 |
| Days cocaine/week | 0 | 0 | .94 | 1.58 | 36.42** | .15 |
Note. BM: biological mother; OCS: Obstetrical complications scale score, high scores are more optimal, gestational age is in weeks, head circumference and birth length is in cm, birth weight is in gms. Occupational status was coded using Hollingshead (1957, 1975) scoring system. All of the substance use variables reflect prenatal substance exposure.
p < .05
p < .01.
2.5 Cumulative Environmental risk
A composite caregiving environmental risk score was computed from the following measures. Maternal psychological distress was assessed using the Brief Symptom Inventory (BSI; Derogatis, 1993) at 1, 7, 13, 24, 36, 48 months and at kindergarten age. This scale is a brief form of Symptom Checklist 90-R, and is a widely used mental health screening measure in a variety of clinical and research settings, including previous studies of maternal cocaine use (e.g., Eiden et al., 2007; Singer et al., 2002). Maternal Exposure to Violence was assessed at 1, 7, 13, 18, 24, 30, 36, 42, 48, 54 months and at kindergarten age using the Timeline Followback Interview (TLFB, Sobell & Sobell, 1996). Although the original interview was a calendar-based method to assess substance use, it has also been used to measure episodes of intimate partner violence in various studies (e.g., Mignone, Klostermann, & Chen, 2009). Women were asked about their witnessing, experiencing, or perpetrating violence using a daily calendar at each assessment point. The total number of days women reported violence were summed within each time point. Given the apparent bimodal distributions at each time point, exposure to violence was dummy-coded (i.e., 0, 1) at each time point and then a count variable was created from each of the dummy-coded time points to reflect exposure to violence across time. Caregiving instability was assessed at 1, 7, 13, 24, 36, 48 months and at kindergarten age using a structured caregiver interview (Platzman, Coles, Lynch, Bard, & Brown, 2001). Following Platzman et al. (2001), individual items from the SCI were summed into a cluster called caregiving instability. The five items included in this scale were as follows: no male adult in the household, baby separated from primary caregiver for more than 48 hours, baby is fed and sleeps significantly less than average, there are custody changes, or baby does not see primary caregiver regularly. Thus, the total score on caregiving instability was based on the presence of absence of the 5 specific risk characteristics described above (see Platzman et al., 2001 for details regarding scale development). The scale is similar to a composite risk index (e.g., Sameroff et al., 1993), based on research suggesting that the total number of risk factors may be more predictive of child outcomes than exposure to any specific risk condition (Seifer, 1995; Zeahah et al., 1997). However, unlike the traditional risk composites or environmental risk scores used in other studies, it is more narrowly focused on factors that are associated with instability in the caregiving environment, particularly among families with drug using mothers. The caregiving instability scores ranged from 0 to 4 in the current study with the majority of the children in the sample having a score of 0 or 1. Thus, caregiver instability was dummy-coded at each time point and a count variable was created from each of the dummy-coded time points reflecting caregiver instability across the time periods. Previous studies have reported significant positive associations between maternal drug use and higher caregiving instability (Eiden, Peterson, & Coleman, 1999; Platzman et al., 2001). The caregiving instability cluster was also associated with an acceleratory heart rate response indicating distress or arousal among cocaine exposed infants (Bard et al., 2000) and was a predictor of child behavior problems among 2 to 5 year old children of cocaine using mothers (Eiden, 1999).
Postnatal substance use variables (average number per week from 1 month to kindergarten age) were dummy coded following the cut-offs used by Yumoto et al (2008). Each substance was dummy coded into the risk category as follows: 28 standard drinks/week or higher (17% of the sample), 7 joints per week or more (21% of the sample), 70 cigarettes per week or higher (13% of the sample), and any postnatal cocaine use (16% of the sample).
The cumulative caregiving environmental risk variable was created by computing a count variable which included BSI, exposure to violence, and caregiving instability for each time point that each variable was assessed and the cumulative postnatal substance use across time. BSI and caregiving stability were assessed at seven time points (i.e., 1, 7, 13, 24, 36, 48 months, and at kindergarten), exposure to violence was assessed at eleven time points (i.e., 1, 7, 13, 18, 24, 30, 36, 42, 48, 54 months and kindergarten), and there were four dummy coded variables reflecting postnatal substance use across time (alcohol, marijuana, cigarettes, and cocaine). Thus, scores for cumulative caregiving environmental risk could theoretically range from 0 to 29. The scores for cumulative caregiving environmental risk ranged from 0 to 24 in this sample.
2.6 Maternal Harshness
Maternal harshness was measured at 7, 13, 24, and 36 months and was based on two different types of observational coding at different ages. Intensity of maternal harshness at 7, 13, and 24 months was assessed using behavioral observations during a free play task. Mothers were asked to interact with their infants as they normally would at home for 10 minutes in a room filled with toys. These interactions were coded using a collection of global 5-point rating scales developed by Clark, Musick, Scott, & Klehr (1980). The scale for maternal harshness consisted of the average of items such as angry, hostile tone of voice, expressed negative affect, displeasure, disapproval, criticism, and angry, hostile mood. Items were reverse coded so that higher scores reflected higher harshness. At 36 months, intensity of maternal harshness was event coded during specific segments of the observational assessments. These included a 10-minute mother-child free play paradigm, a 10 minute clean-up, 8-minute structured play, 10-minute eating a snack, and 5-minute emotion regulation paradigm. Following previous studies (Keenan and Shaw, 1994), this allowed for coding of maternal harshness across varying levels of stress, from none (e.g., during free play), to moderate (clean up), to higher levels of stress (emotion regulation paradigm) (see Eiden et al., 2011 for episode details). Maternal harshness at 36 months was coded on the basis of codes developed in previous studies (Cummings et al., 1989; Keenan & Shaw, 1994). This included physical harshness (hitting, kicking, pushing) directed toward a person; physical harshness directed toward an object (e.g., banging, throwing); verbal harshness that consists of cursing (use of obscene language or gestures); and verbal harshness that consists of threats (words used to attack a person or threats of harm). Event coding of each aggressive episode was triggered by the mother displaying any of these behaviors. An overall rating of intensity of maternal harshness (based on all events) was coded along a 5-point scale ranging from 0 = no harshness to 4 = severe harshness.
Two coders blind to group status rated maternal harshness at all ages. They were trained by the first author until inter-rater reliability criterion was reached (agreement of 90% or above). Subsequently inter-rater reliability was established on 20% of the tapes. Inter-rater reliability on intensity of maternal harshness was high across ages, with intra-class correlation coefficient ranging from .82 to .96. Maternal harshness at the different ages were moderately correlated with each other with Pearson correlation coefficients ranging from r = .30 to r = .38. In order to create a variable that reflected the child’s experience of maternal harshness across the infant/toddler years, a composite measure of maternal harshness was computed by taking the average across the four ages and used in model testing. This final variable ranged from .50 to 4.19 with high scores indicating high maternal harshness.
2.7 Internalizing Behavior Problems
Maternal reports of internalizing behavior problems were obtained at 36 months and at kindergarten using the internalizing behavior subscales of the 1 ½ to 5 year version of the Child Behavior Checklist (CBCL; Achenbach, 1992). The CBCL is a widely used measure of children’s behavioral/emotional problems. It consists of 100-items on a three-point response scale ranging from “not true” to “very true,” with some open-ended items designed to elicit information about a particular problem behavior. Higher scores indicate more internalizing behavior problems. Raw scores were used in all analyses and T scores were used for descriptive purposes. About 18% of children in this sample had T scores in the borderline/clinical range (T score of ≥ 60) at 36 months and at kindergarten according to maternal reports on the CBCL. Confirmatory factor analysis was conducted on the subscales of withdrawn, anxious/depressed, and emotionally reactive at 36 months and at kindergarten. These three subscales at each time point loaded on one factor reflecting internalizing behavior problems with factor loadings of .75, .85, and .89 at 36 months, and .71, .79, and .82 at kindergarten.
2.8 Data Analytic Strategy
Group differences in demographic, perinatal risk characteristics, and maternal substance use variables were examined first using ANOVAs or MANOVAs in order to provide descriptive data and guide selection of potential covariates. MANOVAs were used when multiple theoretically associated constructs were the dependent measures in order to control for high Type I error rate. ANOVAs were used to examine gender differences in internalizing behavior problems. Demographic or perinatal risk variables that were associated with both predictors and outcomes at p < .10 were used as covariates in subsequent analyses. Structural equations modeling (SEM) was used to test the hypothesized model (see Figure 1)with environmental risk and maternal harshness as mediators or intervening variables between maternal substance use and internalizing behavior problems. MacKinnon, Lockwood, and Hoffman (2002) defined intervening variables as those transmitting the effect of an independent variable to a dependent variable. SEM analyses were conducted using Mplus, version 6 software (Muthen & Muthen, 2006) using full-information maximum likelihood estimation procedures (Arbuckle, 1996). Indirect effects (significant association between two variables via a mediating or intervening variable) were tested using the bias-corrected bootstrap method. This method has been found to provide a more accurate balance between Type 1 and Type 2 errors compared with other methods used to test indirect effects (MacKinnon, Lockwood, & Williams, 2004). Five thousand bootstrap samples and the 95% bias-corrected confidence intervals (CIs) were used to test significance of indirect effects. Multiple group analyses were used to examine the hypothesis that environmental risk and maternal harshness would moderate the associations among variables.
Figure 1.
Proposed Hypothetical Model
2.9 Missing data
As expected in any longitudinal study, there were some incomplete data for some of the participants at one or more of the four assessment points included in this study. Of the 216 mother-infant dyads who completed the 4- to 8- week laboratory visit, 177 completed the 24 month assessment, 165 completed the 36 month assessment, and 164 completed the kindergarten assessment. There were no significant differences between families with complete vs. missing on any of the variables included in this study and demographics at any age until the kindergarten assessment. Families with missing data at kindergarten had lower maternal education, F (1, 213) = 4.82, p < .05 (M = 11.89 and 11.26 for those with complete vs. missing data respectively, SD = 1.73 and 2.06). Mothers with missing data at the kindergarten assessment also were more likely to smoke in pregnancy compared to those with complete data, F (1, 213) = 5.24, p < .05 (M = .87 and 3.01 for those with complete and missing data respectively, SD = 4.50 and 8.82, Cohen’s d = .30). Finally, 36.5% of children with missing data at kindergarten were in foster care compared to 22% of those with complete data, Pearson χ2 = 4.02, p < .05, Cohen’s d = .27. Given that these differences were present at only one assessment and reflected small differences, missing data likely had a small impact on findings. As noted earlier, full-information maximum likelihood was used to estimate model parameters for SEM. Variables that were significantly different for families with missing vs. complete data (maternal education, number of cigarettes per day used during pregnancy, and foster care status) were included in model testing as exogenous variables.
3. Results
3.1 Potential Covariates: Demographics and Perinatal Risk
Results from MANOVA with the demographic variables as the dependent measures and CE group status yielded a significant multivariate effect of group status, F(4, 210) = 6.51, p < .01. Results from univariate analyses indicated that control group mothers were younger, had lower parity (number of live births), and reported higher occupation status compared to those in the CE group (see Table 1). None of these demographic variables were associated with internalizing behavior problems.
MANOVA with perinatal outcomes and obstetrical complications as the dependent measures yielded a significant multivariate effect of group status, F (5, 210) = 13.83, p < .001. Univariate analyses indicated that CE infants had lower gestational age, birth weight, birth length, and cocaine using mothers had more obstetrical complications (as indicated by lower optimal scores on the OCS) compared to those in the control group (see Table 1). 11% of CE infants (ranged from 33 to 41 weeks) and 3% of the control group infants (ranged from 36 to 42 weeks) were preterm (<37 weeks gestational age). CE infants were significantly more likely to have been preterm than control infants, Pearson chi-square = 7.76, p < .01. All testing was conducted after age correction for prematurity. Infants ranged from 1531 to 5072 grams at birth (Means = 3142.01, SD = 567.33). When these analyses were repeated after using gestational age as covariate, the differences in birth weight and length remained significant (p < .01). However, there were no significant associations between any of the perinatal risk variables and internalizing behavior problems. ANOVA with child sex as the independent variable and the three subscales (emotionally reactive, anxiety/depression, and withdrawn) as the dependent measures indicated a significant gender difference on anxiety/depression at Kindergarten, F (1, 162) = 4.50, p < .05, with girls exhibiting higher anxiety/depression compared to boys (M = 2.87 and 2.06, SD = 2.66 and 2.25 for girls and boys respectively). Thus, child gender was included as a covariate in model testing.
MANOVA with foster care status as the independent variable and the three CBCL subscales for internalizing behaviors at kindergarten as the dependent variables indicated no significant effects of foster care. Number of care changes and child age when first entered foster care were also examined as potential covariates, but were not associated with any of the hypothesized mediators or with internalizing behavior problems.
Externalizing behavior problems at 3 years was considered as a covariate because of the well documented association between internalizing and externalizing problems. In the current sample, externalizing behavior problems at 3 years was significantly correlated with internalizing behavior problem scales at both 3 years (rs = .55 to .69, ps < .01) and at kindergarten (rs = .41 to .51, ps < .01) at the bivariate level. However, when included in the model, externalizing behavior problems at 3 years did not account for unique variance in the latent construct for internalizing behavior problems at kindergarten. Thus, externalizing behavior problems were not considered further.
3.2 Model Testing
Correlations among variables in the model are depicted in Table 2. We first tested the potential for direct associations between CE and internalizing behavior problems. This model did not include maternal harshness or environmental risk but included maternal education and maternal substance use variables and direct paths from these exogenous variables to the latent variables for internalizing problems at 36 months and at kindergarten. Results indicated a direct association between the average number of cigarettes per week during pregnancy and internalizing problems in kindergarten (β = .24, p < .01). There were no other significant direct associations between prenatal substance exposure variables and internalizing problems.
Table 2.
Correlations among variables.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Cocaine Group Status | |||||||||||||
| 2. # Cigarettes/week P | .33 | ||||||||||||
| 3. # Drinks/week P | .21 | .34 | |||||||||||
| 4. Years education | −.10 | −.22 | −0.21 | ||||||||||
| 5. Environmental Risk | .11 | .18 | .17 | −.12 | |||||||||
| 6. Maternal Harshness | .16 | .09 | .13 | −.19 | .05 | ||||||||
| 7. CBCL Withdrawn 3Y | −.06 | .09 | −.08 | −.08 | −.26 | .14 | |||||||
| 8. CBCL ER 3Y | .00 | .17 | .01 | −.06 | .30 | .11 | .60 | ||||||
| 9. CBCL A/D 3Y | .11 | .22 | .06 | −.18 | .32 | .23 | .56 | .65 | |||||
| 10. CBCL Withdrawn K | −.01 | .19 | .01 | −.13 | .28 | .27 | .42 | .36 | .41 | ||||
| 11. CBCL ER K | .04 | .13 | −.06 | −.09 | .31 | .25 | .35 | .45 | .42 | .68 | |||
| 12. CBCL A/D K | .08 | .13 | −.01 | −.13 | .31 | .28 | .33 | .40 | .55 | .63 | .76 | ||
| 13. CBCL Int 3Y Clinical | −.04 | .13 | −.10 | −.05 | .23 | .02 | .57 | .72 | .64 | .22 | .31 | .36 | |
| 14. CBCL Int K Clinical | .05 | .13 | −.01 | −.06 | .19 | .21 | .20 | .31 | .34 | .67 | .71 | .66 | .19 |
Note: #: Number; P: Pregnancy; 3Y: 3 years; ER: Emotionally Reactive; A/D: Anxiety/Depression; K: Kindergarten, Int: Internalizing problems, Clinical: clinical cut-off yes/no. Numbers in bold reflect correlation coefficients were significant at p <.05. Coding for cocaine group status was 0 = control group and 1= cocaine-exposed group. The sample sizes for correlations ranged from n = 164 to 216.
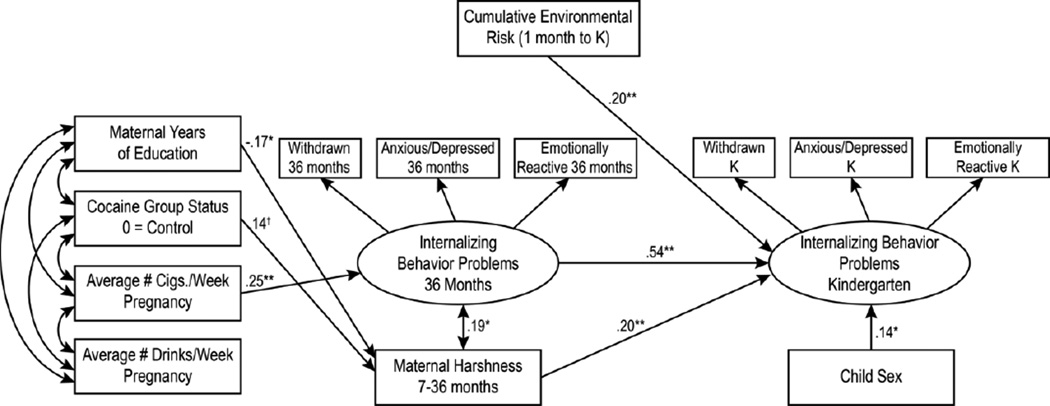
Next, we tested the hypothesized mediational model. This included maternal harshness and cumulative environmental risk as potential mediators or intervening variables between maternal substance use and internalizing behavior problems at kindergarten age. The model also included the covariance between the residuals of harshness and internalizing behavior problems at 3 years, and the stability of internalizing behavior problems from 3 years to kindergarten age. Maternal education was included as an exogenous variable because it was associated with missingness. Foster care was included in the initial model, but was dropped subsequently as it was not associated with any of the mediators or with internalizing behavior problems. Goodness of fit indices indicated that this hypothesized model fit the data well, (χ2(45) = 76.79, p < .05, comparative fit index = .95, root mean square error of approximation = .06. The structural paths indicated that prenatal CE was marginally associated with high maternal harshness from infancy to the toddler years, high maternal harshness was associated with higher internalizing behavior problems at kindergarten age, and high cumulative environmental risk was associated with high internalizing behavior problems at kindergarten age (see Figure 2). Prenatal cigarette exposure was associated with higher internalizing behavior problems at 3 years, and this in turn was associated with higher internalizing problems at kindergarten age.
Figure 2.
Longitudinal associations between prenatal exposure to substances, environmental risk, maternal harshness, and internalizing behavior problems.
Note: The numbers represent standardized path coefficients. Non-significant paths are not depicted in the model for ease of presentation. The indirect or mediated pathway from cocaine group status to internalizing behavior problems in Kindergarten via maternal harshness was non-significant, but maternal harshness moderated the association between cocaine exposure and internalizing behavior problems (see text). *p < .05, **p < .01, +p < .10.
Our model included hypotheses about several indirect effects or mediational pathways. The pattern of path coefficients provided evidence for one potential pathway from prenatal cigarette exposure and higher internalizing behavior problems at kindergarten via higher internalizing behavior problems at 3 years. Testing of indirect effects indicated that this pathway was statistically significant (B = .14, 95% CI: .02, .25).
3.3 Moderation by Child Gender
We examined moderation by child gender using multiple group analyses in SEM. We first examined fit indices for a fully unconstrained model for boys and girls and compared this unconstrained model with a fully constrained model. The chi-square change between these two models was not significant (Δχ2(17) = 22.71, p > .05), suggesting that the model was equivalent for boys and girls.
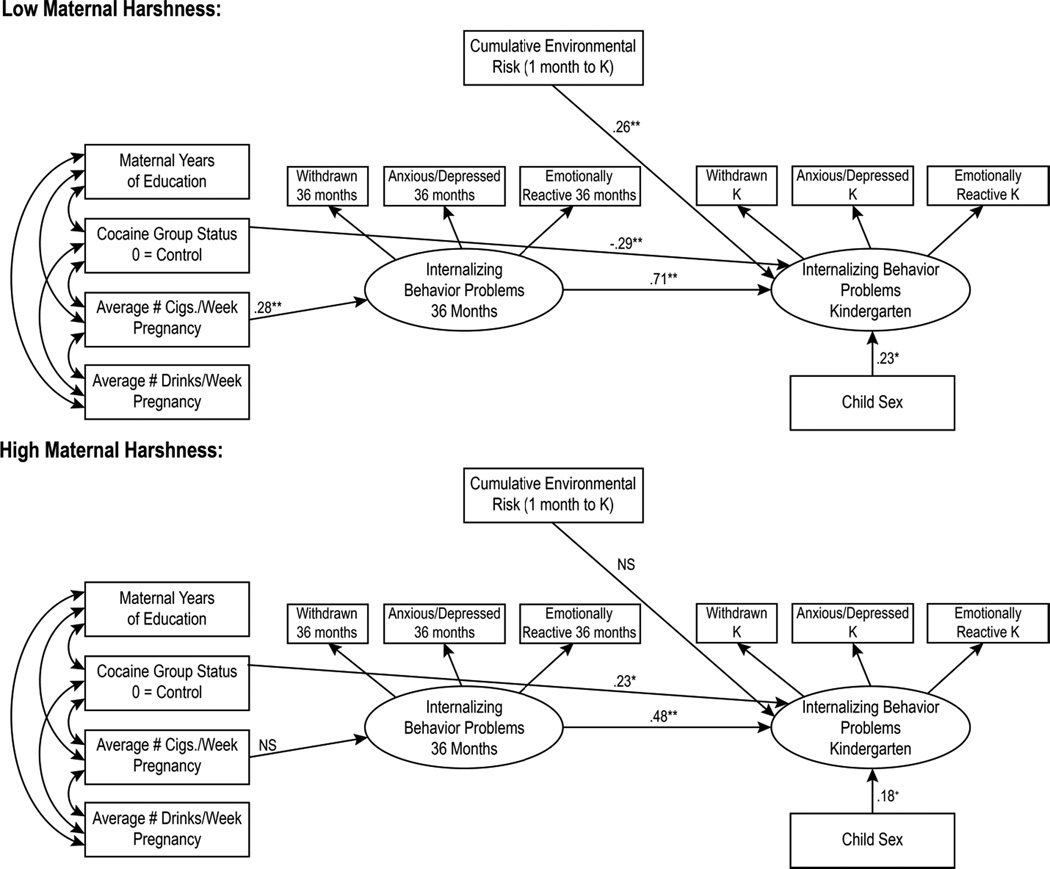
3.4 Moderation by Maternal Harshness
We hypothesized that the association between maternal substance use and internalizing behavior problems would be stronger in the context of high maternal harshness. Two groups reflecting high and low maternal harshness were created using median splits. We compared the unconstrained model with a model constraining paths from maternal substance use variables to internalizing behavior problems at 3 years and at kindergarten and from environmental risk to internalizing behavior problems at kindergarten. The chi-square difference between these two models was significant, Δχ2(7) = 14.10, p < .05. Testing of individual paths indicated that the association between prenatal CE and internalizing behavior problems at kindergarten was significant, but in reverse directions at low vs. high levels of maternal harshness. Specifically, prenatal CE was associated with lower internalizing behavior problems at kindergarten when children experienced low levels of maternal harshness (β = −.27, p < .01), and was associated with higher internalizing behavior problems at high levels of maternal harshness (β = .25, p < .05). None of the other paths from maternal substance use or environmental risk to internalizing problems were significantly different at low vs. high levels of maternal harshness (see Figure 3).
Figure 3.
Moderation by maternal harshness of the association between maternal cocaine use and internalizing problems in kindergarten.
Note. At low levels of maternal harshness, maternal cocaine use was associated with low internalizing behavior problems. At high levels of maternal harshness, maternal cocaine use was associated with high levels of internalizing behavior problems. NS: Non-significant; *p < .05, **p < .01, +p < .10.
3.5 Moderation by Cumulative Environmental Risk
We examined if the association between maternal substance use and internalizing behavior problems varied as a function of cumulative environmental risk using multiple group models, with two groups reflecting high and low levels of environmental risk created using median splits. Comparison of an unconstrained model with a model constraining paths from maternal substance use variables to internalizing behavior problems and from harshness to internalizing problems in kindergarten indicated no significant difference between the two groups (Δχ2(7) = 3.97, p > .05).
4. Discussion
We examined a conceptual model for the development of internalizing behavior problems among cocaine-exposed and demographically similar non-exposed children. This model included an investigation of the role of cumulative environmental risk and maternal harshness. To begin, the hypothesized direct effect of CE on internalizing behavior problems at kindergarten age was not supported. Past research has not consistently found an association between prenatal CE and internalizing behavior problems from early to middle childhood (e.g., Accornero et al., 2002, 2006; Bada et al., 2011). However, past work has hypothesized aspects of the postnatal caregiving environment as being particularly important for the development of internalizing and externalizing problems among CE children (Accornero et al., 2001). However, few have examined indirect pathways or moderation by caregiving variables. Thus, this study adds an important examination of potential indirect pathways and moderators that may better explain the association between prenatal CE and internalizing behavior problems.
More specifically, two indirect pathways linking maternal cocaine use to children’s internalizing problems were examined in this study: first, the path from maternal cocaine use → higher maternal harshness from 7 to 36 months → higher internalizing problems in kindergarten was investigated. This indirect path was not significant; however, the direct path from maternal cocaine use to maternal harshness was marginally significant and the path from maternal harshness to internalizing problems at kindergarten age was significant. This indicated that maternal cocaine use was related to high maternal harshness in infancy to the toddler years and that high maternal harshness was in turn associated with higher internalizing behavior problems in kindergarten age. Although the indirect association between CE and internalizing problems via higher maternal harshness was not significant, maternal harshness was a significant moderator of risk for internalizing problems. The association between prenatal CE and internalizing behavior problems was stronger under conditions of higher maternal harshness, as hypothesized. This is consistent with past research indicating the role of parenting in child internalizing behavior problems (e.g., Reitz, Deković, & Meijer, 2006) as well as the relation between maternal cocaine use and negative parenting practices, such as maternal harshness (e.g, Eiden et al., 2011). The nature of moderation by maternal harshness is supportive of diathesis-stress models indicating that the combination of biological vulnerability and proximal caregiving risk is associated with highest risk for internalizing problems. However, results also suggested that in the context of biological vulnerability posed by prenatal CE, low maternal harshness may be a marker for positive parenting behaviors, thus leading to low levels of internalizing behavior problems.
Second, the path from maternal cocaine use → higher environmental risk from 1 to 54 months → higher internalizing behavior problems in kindergarten was examined. Contrary to hypotheses, this indirect path was also not significant. Further, the association between prenatal CE and internalizing behavior problems was not moderated by level of cumulative environmental risk. However, high environmental cumulative risk was independently associated with high internalizing in behavior problems at kindergarten age. We had hypothesized that the association between CE and internalizing behavior problems would be stronger under conditions of high environmental risk. However, given that the entire sample is at high risk, these risk factors may be salient for the entire group and as such cumulative risk more globally predicted internalizing behavior problems within the sample. A strength of the current study is considering the impact of cumulative environmental risk as children are exposed to nested risk factors and are not facing each risk factor individually. In addition, the present study adds to a growing literature on the role of cumulative risk in the development of internalizing behavior problems (e.g., Appleyard et al., 2005; Ashford et al., 2008) to complement the more significant body of literature on cumulative risk and externalizing behavior problems (e.g., Deater-Deckard, Dodge, Bates, & Pettit, 1998).
We also examined the role of child gender as a potential moderator of the direct association between CE and internalizing behavior problems; however, the models were not significantly different for boys and girls. Given the mixed results in prior literature, we had not hypothesized a direction of effect for gender. It is possible that during this early developmental period, potential gender differences in internalizing problems (for review see Zahn–Waxler, Klimes–Dougan, & Slattery, 2000) have not yet developed. This may be because the differential risk factors or vulnerabilities that may account for gender differences may not have yet emerged developmentally given that they may be more interpersonal or peer-related (Leadbeater, Blatt, & Quinlan, 1995; Leadbeater, Kuperminc, Blatt, & Hertzog, 1999). However, group differences replicated previous findings such that girls exhibited significantly higher anxiety/depression compared to boys.
As cocaine use during pregnancy is often a poly-drug issue (Lester et al., 2003), the consideration of other substance use, such as cigarette smoking, during pregnancy was also investigated. A significant indirect path from prenatal cigarette exposure to internalizing at 36 months to internalizing at kindergarten age was demonstrated. As such, concurrent cocaine and cigarette use during pregnancy may put children at greater risk of internalizing in early childhood. This finding is also consistent with past work demonstrating the association between prenatal tobacco exposure and behavior problems (e.g., Day, Richardson, Goldschmidt, & Cornelius, 2000; Orlebeke, Knol, & Verhulst, 1997), including internalizing behavior problems (Ashford et al., 2008). This finding emphasizes the importance of examining the impact of other substances within the context of prenatal CE in future research, particularly tobacco, given that children prenatally exposed to cocaine are high risk to also be exposed to tobacco (Minnes et al., 2010).
4.1 Limitations and Future Directions
There are several limitations to this study. To begin, accurate assessment of pre- and post-natal substance use can be difficult to obtain, as parents may be reticent to disclose these behaviors; however, the present study employed multiple methods to assess substance use including maternal self-report, chart review, and maternal hair analysis.
Assessment of internalizing behavior problems is in general more difficult and such symptomatology may be less prevalent during this period than externalizing behavior problems (Keenan, Shaw, Delliquadri, Giovannelli, & Walsh, 1998). However, internalizing symptoms exhibit some level of consistency across development and thus warrant continued investigation in the early childhood period (Sterba, Prinstein, & Cox, 2007). Further, this also highlights the importance for continued work to explore different methods for assessing internalizing within early childhood (Keenan et al., 1998). Future research could also investigate the symptom classes of anxiety and depression separately (Sterba et al,. 2007) given that trajectories may be slightly different.
4.2 Implications and Conclusions
This study had many strengths, such as its prospective design, multiple methods of data collection, retention of subjects, diverse sample, observational assessments of parenting behavior, and statistical control for potential covariates and exploration for potential confounds (e.g., the impact of foster care and perinatal risk factors). The assessment and consideration of cumulative environmental risk is a particular strength of the study given that children develop within complicated systems and may be impacted by risks that are additive or interact with each other to put children at greater probability of experiencing negative developmental outcomes, such as behavioral problems (Appleyard et al., 2005).
In conclusion, given that there appears to be a high level of continuity both in general for internalizing problems across development (e.g., Mathijssen, Koot, & Verhulst, 1999) and particularly from kindergarten-age to early adolescence (e.g., Ashford et al., 2008), understanding risk and protective factors during early periods of development is particularly important for intervention and prevention efforts. The results of the study suggest that not all children exposed to cocaine are at risk for internalizing behavior problems by kindergarten. Results indicate that children who are biologically vulnerable due to prenatal CE may be particularly sensitive to maternal harshness during mother-child interactions as a proximal risk factor. Among these children, while high maternal harshness was associated with high internalizing behavior problems, low harshness was associated with the lowest levels of behavior problems. Thus, preventative efforts focused on reducing maternal substance use during pregnancy as well as reducing maternal harshness in early childhood may be productive. Results also highlighted the critical role of cumulative environmental risk for internalizing behavior problems in kindergarten, suggesting that beyond pregnancy, interventions targeted at lowering cumulative risk may be particularly productive.
Highlights.
Cigarette exposed children had more internalizing problems (IP) at kindergarten age.
Cocaine exposed children had more IP when they experienced high maternal harshness.
Cumulative environmental risk in early childhood accounted for unique variance in IP.
Acknowledgements
The authors thank the families who participated in this study and the research staff responsible for data collection and coding of observational assessments. Special thanks to Dr. Claire Coles for collaboration on the larger study, Dr. Amol Lele for collaboration on data collection at the Women and Children’s Hospital of Buffalo, and Dr. Michael Ray for his collaboration on data collection at Sisters of Charity Hospital of Buffalo. Research reported in this paper was supported by the National Institute on Drug Abuse of the National Institutes of Health under award number R01DA013190. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
There is no conflict of interest.
Contributor Information
Rina D. Eiden, State University of New York at Buffalo
Stephanie Godleski, State University of New York at Buffalo.
Craig R. Colder, State University of New York at Buffalo
Pamela Schuetze, Buffalo State College.
References
- Accornero VH, Morrow CE, Bandstra ES, Johnson AL, Anthony JC. Behavioral outcome of preschoolers exposed prenatally to cocaine: Role of maternal behavioral health. Journal of Pediatric Psychology. 2002;27(3):259–269. doi: 10.1093/jpepsy/27.3.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Accornero VH, Anthony JC, Morrow CE, Xue L, Bandstra ES. Prenatal cocaine exposure: An examination of childhood externalizing and internalizing behavior problems at age 7 years. Epidemiologia e Psichiatria Sociale. 2006;15(1):20–29. [PMC free article] [PubMed] [Google Scholar]
- Arbuckle JL. Full information estimation in the presence of incomplete data. In: Marcoulides GA, Schumacker RE, editors. Advanced Structural Equation Modeling: Issues and Techniques. Mahwah, NJ: Lawrence Erlbaum Associates; 1996. pp. 243–277. (Reprinted from: NOT IN FILE). [Google Scholar]
- Ashford Janka, Lier Pol AC Van, Timmermans Maartje, Cuijpers Pim, Koot Hans M. Prenatal smoking and internalizing and externalizing problems in children studied from childhood to late adolescence. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47(7):779–787. doi: 10.1097/CHI.0b013e318172eefb. [DOI] [PubMed] [Google Scholar]
- Bada HS, Bann CM, Bauer CR, Shankaran S, Lester B, LaGasse L, Higgins R. Preadolescent behavior problems after prenatal cocaine exposure: relationship between teacher and caretaker ratings (Maternal Lifestyle Study) Neurotoxicol Teratol. 2011;33(1):78–87. doi: 10.1016/j.ntt.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belsky J, Pluess M. Beyond diathesis stress: differential susceptibility to environmental influences. Psychol Bull. 2009;135(6):885–908. doi: 10.1037/a0017376. [DOI] [PubMed] [Google Scholar]
- Bender Heather L, Allen Joseph P, McElhaney Kathleen Boykin, Antonishak Jill, Moore Cynthia M, Kelly Heather O'Beirne, Davis Steven M. Use of harsh physical discipline and developmental outcomes in adolescence. Development and Psychopathology. 2007;19(1):227–242. doi: 10.1017/S0954579407070125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett D, Bendersky M, Lewis M. Children's intellectual and emotional-behavioral adjustment at 4 years as a function of cocaine exposure, maternal characteristics, and environmental risk. Developmental Psychology. 2002;38(5):648–658. doi: 10.1037//0012-1649.38.5.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell Arin M, Goodman Sherryl H. The association between psychopathology in fathers versus mothers and children's internalizing and externalizing behavior problems: A meta-analysis. Psychological Bulletin. 2002;128(5):746–773. doi: 10.1037/0033-2909.128.5.746. [DOI] [PubMed] [Google Scholar]
- Day Nancy L, Richardson Gale A, Goldschmidt Lidush, Cornelius Marie D. Effects of prenatal tobacco exposure on preschoolers' behavior. Journal of Developmental and Behavioral Pediatrics. 2000 [PubMed] [Google Scholar]
- Easterbrooks M Ann, Bureau Jean-Francois, Lyons-Ruth Karlen. Developmental correlates and predictors of emotional availability in mother–child interaction: A longitudinal study from infancy to middle childhood. Development and Psychopathology. 2012;24(1):65–78. doi: 10.1017/S0954579411000666. [DOI] [PubMed] [Google Scholar]
- Eiden RD, Foote A, Schuetze P. Maternal cocaine use and caregiving status: Group differences in caregiver and infant risk variables. Addictive Behaviors. 2007;32:465–476. doi: 10.1016/j.addbeh.2006.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eiden RD, Peterson M, Coleman T. Maternal cocaine use and the caregiving environment during early childhood. Psychology of Addictive Behaviors. 1999;13(4):293–302. [Google Scholar]
- Eiden RD, Schuetze P, Colder CR, Veira Y. Maternal cocaine use and mothertoddler aggression. Neurotoxicology and Teratology. 2011;33:360–369. doi: 10.1016/j.ntt.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eiden RD, Schuetze P, Coles C. Maternal cocaine use and mother-infant interactions: Direct and moderated associations. Neurotoxicology and Teratology. 2011;33:120–128. doi: 10.1016/j.ntt.2010.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gawin FH, Ellinwood EH. Cocaine and other stimulants: Actions, abuse, and treatment. New England Journal of Medicine. 1988;318:1173–1182. doi: 10.1056/NEJM198805053181806. [DOI] [PubMed] [Google Scholar]
- Huang Chien-Chung, Wang Lih-Rong, Warrener Corinne. Effects of domestic violence on behavior problems of preschool-aged children: Do maternal mental health and parenting mediate the effects? Children and Youth Services Review. 2010;32(10):1317–1323. [Google Scholar]
- Ingram RE, Luxton DD. Vulnerability-Stress Models. In: Hankin BL, Abela JRZ, editors. Development of Psychopathology: A vulnerability stress perspective. Thousand Oaks, CA: Sage Publications Inc.; 2005. pp. 32–46. [Google Scholar]
- Irner Tina Birk. Substance exposure in utero and developmental consequences in adolescence: A systematic review. Child Neuropsychology. 2012;18(6):521–549. doi: 10.1080/09297049.2011.628309. [DOI] [PubMed] [Google Scholar]
- Johns JM, Lubin DA, Walker CH, Meter KE, Mason GA. Chronic gestational cocaine treatment decreases oxytocin levels in the medial preoptic area, ventral tegumental area and hippocampus in Sprague-Dawley rats. Neuropeptides. 1997;31(5):439–443. doi: 10.1016/s0143-4179(97)90037-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keenan Kate, Shaw Daniel, Delliquadri Eric, Giovannelli Joyce, Walsh Brenda. Evidence for the continuity of early problem behaviors: Application of a developmental model. Journal of Abnormal Child Psychology. 1998;26(6):441–452. doi: 10.1023/a:1022647717926. [DOI] [PubMed] [Google Scholar]
- Leadbeater Bonnie J, Blatt Sidney J, Quinlan Donald M. Gender-linked vulnerabilities to depressive symptoms, stress, and problem behaviors in adolescents. Journal of Research on Adolescence. 1995;5(1):1–29. [Google Scholar]
- Leadbeater Bonnie J, Kuperminc Gabriel P, Blatt Sidney J, Hertzog Christopher. A multivariate model of gender differences in adolescents' internalizing and externalizing problems. Developmental psychology. 1999;35(5):1268. doi: 10.1037//0012-1649.35.5.1268. [DOI] [PubMed] [Google Scholar]
- Lester BM, LaGasse L, Seifer R, Tronick EZ, Bauer CR, Shankaran S, Maza PL. The Maternal Lifestyle Study (MLS): Effects of prenatal cocaine and/or opiate exposure on auditory brain response at one month. Journal of Pediatrics. 2003;142(3):279–285. doi: 10.1067/mpd.2003.112. [DOI] [PubMed] [Google Scholar]
- Lester Barry M, Bagner Daniel M, Liu Jing, LaGasse Linda L, Seifer Ronald, Bauer Charles R, Das Abhik. Infant neurobehavioral dysregulation: Behavior problems in children with prenatal substance exposure. Pediatrics. 2009;124(5):1355–1362. doi: 10.1542/peds.2008-2898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Zhihao, Coles Claire D, Lynch Mary Ellen, Hamann Stephan, Peltier Scott, LaConte Stephen, Hu Xiaoping. Prenatal cocaine exposure alters emotional arousal regulation and its effects on working memory. Neurotoxicol Teratol. 2009;31(6):342–348. doi: 10.1016/j.ntt.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Zhihao, Santhanam Priya, Coles Claire D, Lynch Mary Ellen, Hamann Stephan, Peltier Scott, Hu Xiaoping. Increased 'default mode' activity in adolescents prenatally exposed to cocaine. Human Brain Mapping. 2011;32(5):759–770. doi: 10.1002/hbm.21059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Light KC, Grewen KM, Amico JA, Boccia M, Brownley KA, Johns JM. Deficits in plasma oxytocin responses and increased negative affect, stress, and blood pressure in mothers with cocaine exposure during pregnancy. Addictive Behaviors. 2004;29:1541–1564. doi: 10.1016/j.addbeh.2004.02.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch M, Cicchetti D. An ecological-transactional analysis of children and contexts: The longitudinal interplay among child maltreatment, community violence, and children's symptomatology. Development and Psychopathology. 1998;10(2):235–257. doi: 10.1017/s095457949800159x. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39(1):99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathijssen JJJP, Koot Hans M, Verhulst Frank C. Predicting change in problem behavior from child and family characteristics and stress in referred children and adolescents. Development and Psychopathology. 1999;11(2):305–320. doi: 10.1017/s0954579499002072. [DOI] [PubMed] [Google Scholar]
- Mayes LC. A behavioral teratogenic model of the impact of prenatal cocaine exposure on arousal regulatory systems. Neurotoxicology & Teratology. 2002;24:385–395. doi: 10.1016/s0892-0362(02)00200-3. [DOI] [PubMed] [Google Scholar]
- McMurray MS, Cox ET, Jarrett TM, Williams SK, Walker CH, Johns JM. Impact of gestational cocaine treatment or prenatal cocaine exposure on early postpartum oxytocin mRNA levels and receptor binding in the rat. Neuropeptides. 2008;42:641–652. doi: 10.1016/j.npep.2008.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMurray MS, Joyner PW, Middleton CW, Jarrett TM, Elliott DL, Black MA, Johns JM. Intergenerational effects of cocaine treatment and rearing environment on aggressive behavior and oxytocin in rats. Stress. 2008;11:398–410. doi: 10.1080/10253890701850239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minnes Sonia, Singer Lynn T, Kirchner H Lester, Short Elizabeth, Lewis Barbara, Satayathum Sudtida, Queh Dyianweh. The effects of prenatal cocaine exposure on problem behavior in children 4–10years. Neurotoxicology and teratology. 2010;32(4):443–451. doi: 10.1016/j.ntt.2010.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus User's Guide (1998–2006) Los Angeles, CA: Muthen & Muthen; 2006. [Google Scholar]
- Oravecz Linda M, Osteen Philip J, Sharpe Tanya L, Randolph Suzanne M. Assessing low income African-American preschoolers' behaviour problems in relationship to community violence, inter-partner conflict, parenting, informal social support and social skills. Child & Family Social Work. 2011;16(3):310–324. [Google Scholar]
- Orlebeke Jacob F, Knol Dirk L, Verhulst Frank C. Increase in child behavior problems resulting from maternal smoking during pregnancy. Archives of Environmental Health: An International Journal. 1997;52(4):317–321. doi: 10.1080/00039899709602205. [DOI] [PubMed] [Google Scholar]
- Osofsky JD, Wewers S, Hann DM, Fick AC. Chronic community violence: What is happening to our children? Psychiatry. 1993;56:36–45. doi: 10.1080/00332747.1993.11024619. [DOI] [PubMed] [Google Scholar]
- Platzman KA, Coles CD, Lynch ME, Bard KA, Brown JV. Assessment of the caregiving environment and infant functioning in polydrug families: Use of a structured clinical interview. Infant Mental Health Journal. 2001;22(3):351–373. [Google Scholar]
- Reitz E, Deković M, Meijer AM. Relations between parenting and externalizing and internalizing problem behaviour in early adolescence: Child behaviour as moderator and predictor. Journal of Adolescence. 2006;29(3):419–436. doi: 10.1016/j.adolescence.2005.08.003. [DOI] [PubMed] [Google Scholar]
- Richardson GA, Goldschmidt L, Wilford J. Continued effects of prenatal cocaine use: Preschool development. Neurotoxicology and Teratology. 2009;31:325–333. doi: 10.1016/j.ntt.2009.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sameroff AJ, Seifer R, Baldwin A, Baldwin C. Stability of intelligence from preschool to adolescence: The influence of social and family risk factors. Child Development. 1993;64:80–97. doi: 10.1111/j.1467-8624.1993.tb02896.x. [DOI] [PubMed] [Google Scholar]
- Sterba Sonya K, Prinstein Mitchell J, Cox Martha J. Trajectories of internalizing problems across childhood: Heterogeneity, external validity, and gender differences. Development and Psychopathology. 2007;19(02):345–366. doi: 10.1017/S0954579407070174. [DOI] [PubMed] [Google Scholar]
- Yumoto Chie, Jacobson Sandra W, Jacobson Joseph L. Fetal substance exposure and cumulative environmental risk in an African American cohort. Child Development. 2008;79(6):1761–1776. doi: 10.1111/j.1467-8624.2008.01224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahn–Waxler Carolyn, Klimes–Dougan Bonnie, Slattery Marcia J. Internalizing problems of childhood and adolescence: Prospects, pitfalls, and progress in understanding the development of anxiety and depression. Development and Psychopathology. 2000;12(03):443–466. [PubMed] [Google Scholar]
- Zeanah Charles H., Jr . Handbook of infant mental health (3rd ed.) New York, NY US: Guilford Press; 2009. [Google Scholar]