Abstract
Spinal posture affects how individuals function from a manual wheelchair. There is a need to directly quantify spinal posture in this population to ultimately improve function. A fiber optic system, comprised of an attached series of sensors, is promising for measuring large regions of the spine in individuals sitting in a wheelchair. The purpose of this study was to determine the agreement between fiber optic and optoelectronic systems for measuring spinal curvature, and describe the range of sagittal plane spinal curvatures in natural sitting. Able-bodied adults (n=26, 13 male) participated. Each participant assumed three sitting postures: natural, slouched (accentuated kyphosis), and extension (accentuated lordosis) sitting. Fiber optic (ShapeTape) and optoelectronic (Optotrak) systems were applied to the skin over spinous processes from S1 to C7 and used to measure sagittal plane spinal curvature. Regions of kyphosis and lordosis were identified. A Cobb angle-like method was used to quantify lordosis and kyphosis. Generalized linear model and Bland-Altman analyses were used to assess agreement. A strong correlation exists between curvature values obtained with Optotrak and ShapeTape (R2=0.98). The mean difference between Optotrak and ShapeTape for kyphosis in natural, extension, and slouched postures was 4.30° (95%LOA: −3.43-12.04°), 3.64° (95%LOA: −1.07-8.36°), and 4.02° (95%LOA: −2.80-10.84°), respectively. The mean difference for lordosis, when present, in natural and extension postures is 2.86° (95%LOA: −1.18-6.90°) and 2.55° (95%LOA: −3.38-8.48°), respectively. In natural sitting, the mean±SD of kyphosis values was 35.07± 6.75°. Lordosis was detected in 8/26 participants: 11.72±7.32°. The fiber optic and optoelectronic systems demonstrate acceptable agreement for measuring sagittal plane thoracolumbar spinal curvature.
Keywords: Spine, posture, spinal curvatures, fiber optic technology, sitting
1. Introduction
Postures while sitting affect how manual wheelchair users function in their environment [1, 2]. Static assessments of spine alignment in sitting demonstrate that posture and upper extremity reach height can be affected by changes to wheelchair configuration [2]. Additionally, in a small group of individuals with tetraplegia, a decreased amount of spinal kyphosis in sitting was associated with changes in ease performing wheelchair-based activities [1]. This information about spine posture has been gleaned from lateral photographs and other approaches. To date, it has been difficult to more directly measure the spinal posture of manual wheelchair users with external sensors due to the presence of a backrest.
The limitations of our current understanding of spine function during wheelchair-based activities are likely due to the lack of a tool that can measure curvature effectively in such a situation. Tools that have been applied to measure large regions of the spine in various individuals, such as retro-reflective markers, radiographs, flexible curves, and a spinal mouse, cannot measure the spine in the presence of a backrest while also tracking a large region of the spine [3-8]. Recently, a fiber optic system, comprised of a connected series of fiber optic sensors along a flexible strip has been used to measure lumbar spine posture and motion [9]. In this application, the fiber optic system showed good agreement with a reflective marker system for quantifying curvature of the lumbar spine during flexion and a lifting task. The system has since been applied to compare lumbar spine movement between individuals with acute and chronic low back pain [10]. This newer method seems to be a promising tool capable of measuring spinal curvature in manual wheelchair users. The fiber optic system covers a large region of the spine, conforms to changes in curvature, can be applied with ease, and allows for quick data captures. Furthermore, the sensors do not need to be visible to detect their location, setting it apart from camera-based systems and making it applicable in the presence of a backrest.
However, additional investigation is warranted to determine the potential for using this fiber optic system to measure larger regions of the spine in sitting. Specifically, it is important to quantify curvature in both the thoracic and lumbar spine while sitting in different postures to determine if fiber optic sensors will be effective for measuring this large region of the spine in manual wheelchair users. Therefore, the purpose of this study was to determine the agreement between fiber optic and optoelectronic systems for measuring spinal curvature, and describe the range of sagittal plane spinal curvatures in natural sitting in this sample. We hypothesized that the spinal curvature values obtained with the fiber optic system will agree with those obtained with the optoelectronic system. To quantify accuracy across a range of spinal postures, including those that could be assumed by manual wheelchair users, healthy individuals were recruited and measured while sitting in three different postures.
2. Methods
2. 1. Participants
Twenty-six healthy adult, able-bodied individuals, between the ages of 18 and 50 years old were recruited and represented a sample of convenience. Individuals were excluded from participation if they had limitations in lumbothoracic or cervical spine active range of motion as evaluated by a licensed physical therapist, history of scoliosis resulting in deformity detectable during range of motion exam, current back or neck pain, a history of back or neck pain requiring medical attention within the past year, history of spinal injury or surgery, radicular symptoms in any extremity, or known allergy to any adhesive. The study was approved by the internal Institutional Review Board. All participants completed written consent prior to engaging in study procedures.
2.2. Equipment and Procedures
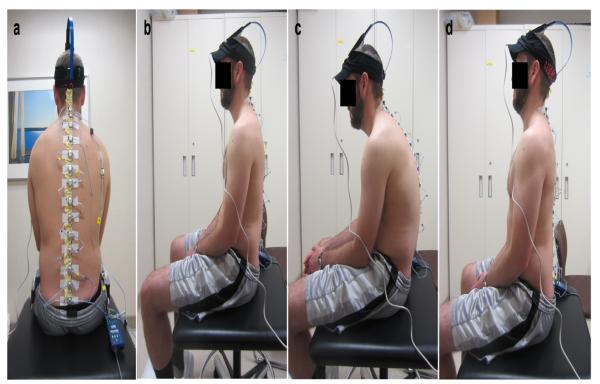
A fiber optic system (ShapeTape; Measurand, Inc.; Fredericton, New Brunswick, Canada) and an optoelectronic system (Optotrak; Northern Digital, Inc.; Waterloo, Ontario, Canada) were applied simultaneously over the spinous processes from the first sacral vertebra (S1) to the seventh cervical vertebra (C7, Figure 1a). Both systems were placed on all participants by the same licensed physical therapist. The ShapeTape was custom-made to include 17 sensor points spaced 46 mm apart along the length of the 20 mm wide system. This created an available 736 mm of sensorized length to be applied to the spine. The Optotrak system consisted of 13-15 infrared strobing smart markers, depending on the participant’s height, with a diameter of approximately 20 mm.
Figure 1.
Sensor Set-up and Postures.
(A) ShapeTape (enclosed within a flexible sleeve) and Optotrak Smart Markers (silver discs) applied to the spine from S1 to C7; (B) participant in natural sitting; (C) participant in slouched sitting; (D) participant in spinal extension sitting.
The ShapeTape was first housed within a flexible sleeve and placed over the participant’s back, allowing it to warm up to the individual’s external body temperature and prevent thermal drift effect in the results. Once the temperature reached a plateau, as visually observed in real time, the ShapeTape was laid flat to define the zero curvature position. The free end of the ShapeTape, which extended beyond the flexible sleeve, was taped directly to the skin overlying S1. The first sensor in series (at the caudal end) placed over S1 was defined as the origin of the Cartesian coordinate system for the ShapeTape output. For the remainder of the measured spine, the sleeve was secured on the skin overlying the spinous processes. The flexible sleeve conformed to the spine during changes in posture while the ShapeTape was able to slide in a cranial-caudal direction and maintain sensors over the entire region of interest throughout the data collection.
The Optotrak, optoelectronic, markers were adhered to the sleeve enclosing the fiber optic sensors in such a way to maintain their contact with the sleeve and conform to spinal movement (Figure 1a). The Optotrak markers were placed at approximately the same distance apart (46 mm) as the ShapeTape sensor locations while the participant was sitting in his or her natural posture. Visibility of all of the Optotrak markers by one Optotrak Certus position sensor (Northern Digital, Inc.; Waterloo, Ontario, Canada), was confirmed prior to data collection. The Optotrak Certus position sensor comprised of three attached cameras was oriented vertically. The Optotrak system was used as the standard against which to compare the ShapeTape due to its high level of positional accuracy. The positional accuracy with a 10 mm translation has been reported as 0.04 mm and 0.02 mm with in plane and out of plane motions, respectively [11].
2.3. Experimental Tasks
Participants sat on a large stool with no backrest throughout the data collection (Figure 1b). A footrest was provided to allow knees and ankles to be positioned at approximately 90 degrees each. Participants sat with their buttocks and thighs supported on the stool with a one to two inch gap between the end of the stool and the back of their knees. Participants were instructed to maintain this leg position, keep their hands relaxed in their lap, and look straight ahead throughout the data collection.
Participants were cued to sit in three different postures: natural, slouched, and extension (Figure 1b-d). Order of postures was not randomized. First, participants were asked to assume a comfortable, natural posture while sitting on the stool. Second, participants were instructed to slouch or slump (accentuating kyphosis) from their natural position to assume the slouched posture. Participants appeared to accomplish this by increasing spinal flexion, posteriorly tilting the pelvis, or both. The extension posture was assumed by instructing the individual to sit with his or her back arched (accentuating lordosis). This was typically accomplished by increasing extension of the spine through the lumbar and lower thoracic region. Study staff demonstrated, as needed, to help the participants find slouched and extension postures that differed from their natural sitting position. Participants were prompted to find slouched and extension postures that were comfortable to hold, not necessarily at the end range of their motion.
Participants were instructed to hold each of these postures once while three static capture trials, lasting 1-2 seconds each, were obtained simultaneously with the ShapeTape and Optotrak. The data was recorded using Shape Recorder (Measurand, Inc.; Fredericton, New Brunswick, Canada) software for the ShapeTape at 78 Hz and MotionMonitor software (Innovative Sports Training, Inc.; Chicago, Illinois) for the Optotrak at 100 Hz. Data were saved for all sensors within each sensor system in Cartesian coordinates.
2.4. Data Analysis
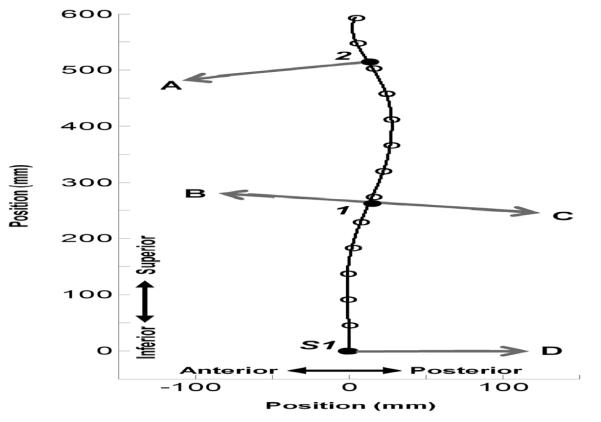
The ShapeTape and Optotrak systems were compared for overall agreement in defining kyphosis and lordosis curves in the thoracolumbar spine. Cartesian data from each system were imported into Matlab (MathWorks; Natick, Massachusetts). A cubic spline was fit to each data set, ShapeTape data and Optotrak data (Figure 2). The sign (+/-) of the second derivative of the spline fit was used to determine inflection points along the length of the total spine curve within the ShapeTape data set. These inflection points along the total spine curve were used to define where the curve changed from lordosis to kyphosis, if lumbar lordosis was present, and where the kyphotic region of the spine terminated cranially (Figure 2). These points were defined as the distance along the ShapeTape curve (arc length), starting from zero at the first sensor point over S1. These distances along the curve were applied to the spline fit of the Optotrak data to identify corresponding points of interest on the Optotrak curve. For both systems, the normal lines to the curve at the points of interest were extended into the concave side of the curve (Figure 2). The curvature of the region of interest was defined as the angle formed between these normal lines, comparable to the definition of Cobb angles calculated on sagittal plane radiographs using the end plates of vertebrae.
Figure 2.
ShapeTape data points, spline fit, and angle identification.
This plot shows the data points from one participant during extension sitting which has both a lordotic and kyphotic curve. The black open circles represent the X and Y Cartesian coordinates (in mm) for each sensor point. The black curve is the spline fit for this data. The black closed circles are S1, the first inflection point (1), and the second inflection point (2). The gray arrows are vectors of the normal lines at each endpoint pointing into the curve of interest. The angle created between vectors A and B is the kyphotic curvature value and the angle created between vectors C and D is the lordotic curvature value.
2.5. Statistical Analysis
Since the participants did not move between the three short trials (1-2 seconds each) captured within a posture, the curvature values were comparable across trials, as expected. The difference was typically within one degree of agreement. To select a representative trial for each participant and posture, data from the second trial collected of each posture was chosen for all data analyses. Regression was used to correlate the overall agreement of kyphosis and lordosis (when present) values determined in all postures for all participants. Due to having multiple measures per participant when compiling all curvature values, a generalized linear model was used to determine correlation while accounting for repeated measures. The parameters for this model were determined using generalized estimating equations (GEE) as determined by the GENMOD function in Statistical Analysis Software (SAS) version 9.3 (SAS Institute Inc.; Cary, NC). The output from GENMOD does not include goodness-of-fit information, thus the R2 value was subsequently calculated based on the equation of linear fit and the actual curvature values.
Additionally, the curvature values obtained in each posture were compared using a Bland-Altman technique [12]. The difference in the curvature values between the Optotrak and ShapeTape data were plotted against the mean value with 95% limits of agreement (LOA) of the curvature defined by the two systems. The agreement was expressed as the mean difference with 95% limits of agreement for five conditions: (1) kyphosis during natural sitting, (2) lordosis during natural sitting, (3) kyphosis during extension sitting, (4) lordosis during extension sitting, and (5) kyphosis during slouch sitting. Only one participant had a detectable lordosis in slouch sitting, therefore no agreement analysis was performed.
3. Results
A total of 26 participants (13 male) took part in the study. The sample characteristics, expressed as mean (standard deviation), are as follows – age: 28.2 years (4.7); height: 172.4 cm (9.1); weight: 74.7 kg (12.6); and body mass index: 25.1 kg/m2 (3.5). A range of values for kyphosis and lordosis were noted in each of the three postures (Table 1). The results from both systems, fiber optic and optoelectronic are reported. Lordosis was not always present. In natural sitting, 8 of the 26 participants had a detectable lordosis (not equal to zero). In slouched sitting only one participant had a detectable lordosis, and in extension sitting all but four participants had a detectable lordosis. One participant’s extension posture data was excluded from analysis due to the lack of visibility of an Optotrak marker in that posture. When describing the natural sitting posture of the participants as quantified by ShapeTape, a lordosis was detected in six of the females with mean (standard deviation): 13.06° (8.14) and two of the males (6.94° an 8.54°). The kyphotic values in natural sitting were 34.10° (6.15) and 36.04° (7.42), mean (standard deviation) for females and males, respectively.
Table 1.
Range of curvature values presented for each posture (natural, slouch, and extension sitting)
| Curvature |
||
|---|---|---|
| Posture | Kyphosis | Lordosis1 |
| Natural | ST: 35.07 ± 6.75° (23.75° - 52.26°) O: 39.37 ± 9.16° (25.98° - 59.96°) n = 26 |
ST: 11.72 ± 7.32° (2.91° - 25.82°) O: 14.59 ± 7.83° (8.16° - 28.71°) n = 8 |
| Slouch | ST: 50.21 ± 7.39° (38.15° - 73.39°) O: 54.23 ± 9.07° (38.99° - 75.71°) n = 26 |
ST: 14.27°2 O: 15.55° n = 1 |
| Extension3 | ST: 28.10 ± 7.42° (15.93° - 40.23°) O: 31.74 ± 8.68° (16.46° - 45.05°) n = 25 |
ST: 14.05 ± 7.73° (1.28° - 30.55°) O: 16.61 ± 8.80° (1.29° - 33.07°) n = 21 |
Each direction (lordosis and kyphosis) and system (ST=ShapeTape and O=Optotrak) indicated by posture. Data presented as: mean ± standard deviation (range).
Not all participants had a detectable lordosis in each posture; therefore, ‘n’ indicates the number who did. Kyphosis was always present.
Only one participant had detectable lordosis in slouched posture, values provided.
One participant’s data was not included in the extension analysis due to the lack of visibility of an Optotrak marker.
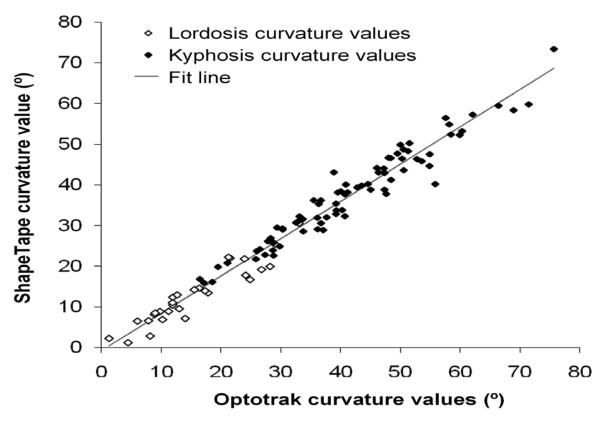
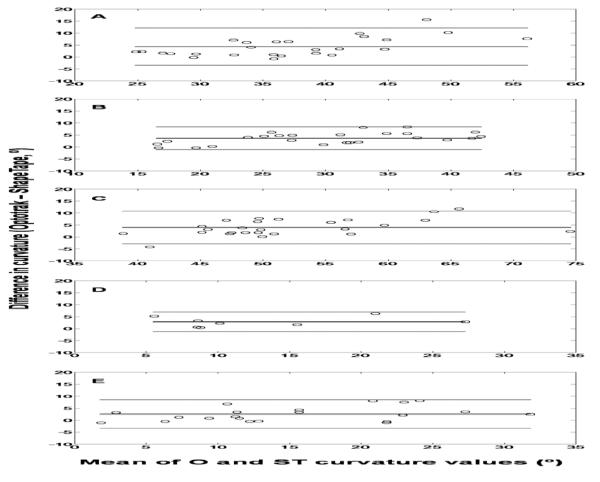
The GEE analysis demonstrated a strong correlation between the ShapeTape and Optotrak results when combining all curvature values across participants and postures (n = 107; R2 = 0.98; linear fit: ShapeTape = 0.92(Optotrak) – 0.74, Figure 3). For the Bland-Altman analyses ShapeTape values were subtracted from Optotrak values. Thus, a positive difference between the two indicates the Optotrak value was larger. The mean difference between Optotrak and ShapeTape for kyphosis in the natural, extension, and slouched postures was 4.30° (95% LOA: −3.43-12.04°), 3.64° (95% LOA: −1.07-8.36°), and 4.02° (95% LOA: −2.80-10.84°), respectively (Figure 4a-c). The mean for lordosis, when lordosis was present, in the natural and extension postures was 2.86° (95% LOA: −1.18-6.90°) and 2.55° (95% LOA: −3.38-8.48°), respectively (Figure 4d,e).
Figure 3.
Correlation of all curvature values.
ShapeTape curvature values plotted against Optotrak for kyphosis and lordosis, when present, from the second trial of all postures (natural, slouch, and extension sitting). The fit line represents results of the generalized estimating equation: ShapeTape = 0.92(Optotrak) – 0.74; R2 = 0.98.
Figure 4.
Bland-Altman plots for kyphotic and lordotic values in all postures.
Data points indicated as black circles, mean difference indicated by solid black line, upper and lower limits of agreement in gray; (A) Kyphosis in natural sitting: mean difference 4.30°, 95% LOA: −3.43-12.04°; (B) Kyphosis in extension sitting: mean difference 3.64°, 95% LOA: −1.07- 8.36°; (C) Kyphosis in slouched sitting: mean difference. 4.02°, 95% LOA: −2.80-10.84°; (D) Lordosis in natural sitting*: mean difference 2.86°, 95% LOA: −1.18-6.90°; and (E) Lordosis* in extension sitting: mean difference 2.55°, 95% LOA: −3.38-8.48°
*Note: sample size for lordosis plots is smaller due to some participants not having a detectable lordotic curve.
4. Discussion
The fiber optic technology, ShapeTape, and optoelectronic markers, Optotrak, demonstrated good agreement in measuring a variety of seated postures and associated sagittal plane spinal curvatures. The two systems were strongly correlated when combining all lordotic and kyphotic curvature values obtained from natural, slouched, extended sitting postures in a group of able-bodied adults. Additionally, mean differences between ShapeTape and Optotrak ranged from 2.55° (lordosis during extension sitting) to 4.30° (kyphosis during natural sitting). The Bland-Altman plots showed 95% limits agreement, including zero, on lordotic and kyphotic regions in the tested postures (natural, slouch, and extension) indicating no significant systematic error.
The mean difference values reported here are similar to those reported by Williams et al [9], who measured lumbar spine alone using the ShapeTape. Additionally, the mean differences are comparable to those that have been reported for intra- and interobserver reliability when measuring Cobb angles on lateral radiographs [3, 6]. On lateral radiographs covering a range of kyphotic postures, the mean intrarater difference (of four orthopedists and a physical therapist) was 3.3° [3]. Comparable results were seen when measuring lateral radiographs of individuals who have Scheuerman’s kyphosis [6]. In this study, four fellowship trained pediatric orthopedic surgeons had an average of 4.3° intrarater difference between readings measured on the same radiographs at least two weeks apart. The error of difference we noted between external measurement methods is comparable to that seen with direct measurement of the spine via radiographs. Thus, the mean differences observed here are reasonable in the context of spinal measurement.
Though we noted good agreement between the two systems, there was a tendency for the kyphosis and lordosis values obtained with Optotrak to be larger than those obtained from the ShapeTape. This could be partly due to the differences in set-up for the two systems. The ShapeTape, as a continuous unit of sensors, creates a smoother overlay on the spine versus the independently placed Optotrak markers which may have affected the contour of the curve and calculated curvature values. The Optotrak system was used as a standard for comparison due to their known position accuracy. However, since the ShapeTape is capable of more directly conforming to the contour of the spine, it may actually be a better approach for measuring spinal curvature.
The curvature values obtained from natural sitting demonstrate a range of values in a sample from an able-bodied population. Of note, the majority of participants (18 of 26) did not have a detectable lordotic curve with our measurement approach. This could be explained by the posterior rotation of the pelvis in sitting relative to standing that subsequently affects the orientation of the lumbar spine. Based on lateral view observation of participants in sitting, the lack of a detected lordosis is consistent with how they appeared to be sitting. Six of the eight participants who did have a detectable lordosis were female. It is possible that sex influences posture in sitting; however our study did not aim to formally assess this detected difference. Additionally, it is possible that due to soft tissue overlying the spinous processes and skin motion artifact, external measures may not directly reflect the bony contour of the spine. Further investigation is warranted to simultaneously measure the spine with ShapeTape, as an external measurement, and medical imagining techniques. This will allow us to determine if an external marker system can accurately represent the underlying bony curvature and at which vertebral level the curvature switches from lordosis to kyphosis in various postures.
In addition to uncertainty of how our curvature values compare to the underlying bony curvature of the spine, there are other limitations that need to be addressed. The ShapeTape is only able to measure curvature changes in the sagittal plane. This might limit a complete assessment of spinal posture when movement or positioning in other planes exists. Despite its limitations, the ShapeTape is able to define spinal curvature, as measured externally, over large regions of the spine. Based on the quality of curvature outcomes reported in this study and the unique attributes of ShapeTape as a measurement system, it is a promising tool for understanding spinal curvature in sitting of those who use manual wheelchairs. Additionally, the fiber optic technology could be used to quantify sagittal plane spinal curvature dynamically, such as during wheelchair-based tasks or other functional movements.
5. Conclusions
When defining spinal curvature as an angle created within a lordotic or kyphotic region of the thoracolumbar spine in sitting, ShapeTape, a fiber optic technology, demonstrated good agreement with the optoelectronic markers. The ShapeTape conforms to the shape of the spine and is not limited by a capture field or need for visualization by a camera system. Fiber optic technology is an effective tool for measuring large regions of spinal curvature in sitting and will be valuable for use with individuals sitting in manual wheelchairs or other conditions with a backrest present.
Highlights.
esearch
▶ 1. We compare measurement of spinal curvature with fiber optic and optoelectronic technologies
▶ 2. Fiber optic measurements yield curvature values comparable to those from optoelectronic markers
▶ 3. Fiber optic technology is effective for measuring spinal curvature over large regions of the spine
Acknowledgements
This publication was supported by CTSA Grant Number TL1 TR000137 from the National Center for Advancing Translational Science (NCATS), NIH Grant Number T32HD07447 from the National Institute of Child Health and Human Development (NICHD), and a Promotion of Doctoral Studies Award from the Foundation for Physical Therapy. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH or the Foundation for Physical Therapy.
The authors would like to acknowledge colleagues in the Orthopedic Biomechanics and Motion Analysis Laboratories at Mayo Clinic for their support in the completion of this work. Additionally, we would like to thank those who participated in the data collection sessions.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bolin I, Bodin P, Kreuter M. Sitting position - posture and performance in c5-c6 tetraplegia. Spinal Cord. 2000;38(7):425–434. doi: 10.1038/sj.sc.3101031. [DOI] [PubMed] [Google Scholar]
- 2.Hastings JD, Fanucchi ER, Burns SP. Wheelchair configuration and postural alignment in persons with spinal cord injury. Arch Phys Med Rehabil. 2003;84(4):528–534. doi: 10.1053/apmr.2003.50036. [DOI] [PubMed] [Google Scholar]
- 3.Carman DL, Browne RH, Birch JG. Measurement of scoliosis and kyphosis radiographs. Intraobserver and interobserver variation. J Bone Joint Surg Am. 1990;72(3):328–333. [PubMed] [Google Scholar]
- 4.Hidalgo B, Gilliaux M, Poncin W, Detrembleur C. Reliability and validity of a kinematic spine model during active trunk movement in healthy subjects and patients with chronic non-specific low back pain. J Rehabil Med. 2012;44(9):756–763. doi: 10.2340/16501977-1015. [DOI] [PubMed] [Google Scholar]
- 5.Preuss RA, Popovic MR. Three-dimensional spine kinematics during multidirectional, target-directed trunk movement in sitting. J Electromyogr Kinesiol. 2010;20(5):823–832. doi: 10.1016/j.jelekin.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 6.Stotts AK, Smith JT, Santora SD, Roach JW, D’Astous JL. Measurement of spinal kyphosis: Implications for the management of scheuermann’s kyphosis. Spine (Phila Pa 1976) 2002;27(19):2143–2146. doi: 10.1097/00007632-200210010-00013. [DOI] [PubMed] [Google Scholar]
- 7.Wang HJ, Giambini H, Zhang WJ, Ye GH, Zhao C, An KN, Li YK, Lan WR, Li JY, Jiang XS, Zou QL, Zhang XY, Chen C. A modified sagittal spine postural classification and its relationship to deformities and spinal mobility in a chinese osteoporotic population. PLoS One. 2012;7(6):e38560. doi: 10.1371/journal.pone.0038560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Youdas JW, Suman VJ, Garrett TR. Reliability of measurements of lumbar spine sagittal mobility obtained with the flexible curve. J Orthop Sports Phys Ther. 1995;21(1):13–20. doi: 10.2519/jospt.1995.21.1.13. [DOI] [PubMed] [Google Scholar]
- 9.Williams JM, Haq I, Lee RY. Dynamic measurement of lumbar curvature using fibre-optic sensors. Med Eng Phys. 2010;32(9):1043–1049. doi: 10.1016/j.medengphy.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 10.Williams JM, Haq I, Lee RY. Dynamic lumbar curvature measurement in acute and chronic low back pain sufferers. Arch Phys Med Rehabil. 2012;93(11):2094–2099. doi: 10.1016/j.apmr.2012.06.012. [DOI] [PubMed] [Google Scholar]
- 11.Maletsky LP, Sun J, Morton NA. Accuracy of an optical active-marker system to track the relative motion of rigid bodies. J Biomech. 2007;40(3):682–685. doi: 10.1016/j.jbiomech.2006.01.017. [DOI] [PubMed] [Google Scholar]
- 12.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–310. [PubMed] [Google Scholar]