ABSTRACT
BACKGROUND
Young adults are less likely than older adults to be aware they have hypertension or to be treated for hypertension.
OBJECTIVE
To describe rates of hypertension awareness and control in a cohort of young adults and understand the impact of health insurance, utilization of preventive care, and self-perception of health on rates of hypertension awareness and control in this age group.
DESIGN AND PARTICIPANTS
Cross-sectional study of 13,512 young adults participating in Wave IV of the National Longitudinal Study of Adolescent Health in 2007–2008.
MAIN MEASURES
We defined hypertension as an average of two measured systolic blood pressures (SBP) ≥ 140 mmHg, diastolic blood pressures (DBP) ≥ 90 mmHg, or self-report of hypertension. We defined hypertension awareness as reporting having been told by a health care provider that one had high blood pressure, and assessed awareness among those with uncontrolled hypertension. We considered those aware of having hypertension controlled if their average measured SBP was < 140 mmHg and DBP was < 90 mmHg.
KEY RESULTS
Of the 3,303 young adults with hypertension, 2,531 (76 %) were uncontrolled, and 1,893 (75 %) of those with uncontrolled hypertension were unaware they had hypertension. After adjustment for age, sex, race/ethnicity, weight status, income, education, alcohol and tobacco use, young adults with uncontrolled hypertension who had (vs. didn’t have) routine preventive care in the past 2 years were 2.4 times more likely (95 % confidence interval [CI] 1.68–3.55) to be aware, but young adults who believed they were in excellent (vs. less than excellent) health were 64 % less likely to be aware they had hypertension (OR 0.36, 95 % CI 0.23–0.57). Neither preventive care utilization nor self-rated health was associated with blood pressure control.
CONCLUSIONS
In this nationally representative group of young adults, rates of hypertension awareness and control were low. Efforts to increase detection of hypertension must address young adults’ access to preventive care and perception of their need for care.
KEY WORDS: hypertension, young adult, health services accessibility, health status
INTRODUCTION
Hypertension is a strong risk factor for the development of cardiovascular and chronic kidney disease.1–3 Hypertension places a large financial strain on the healthcare system, with estimated direct and indirect costs as high as $93.5 billion in health care services and missed work in 2010.4 Unfortunately, studies continue to demonstrate high rates of uncontrolled hypertension in the US, especially among those unaware of their diagnosis. Data from 2003–2010 National Health and Nutrition Examination Surveys (NHANES) show that over half of the 30 % of US adults aged ≥ 18 years who have hypertension have uncontrolled hypertension, and 39 % of those with uncontrolled hypertension are unaware that they have elevated blood pressure.5 Despite the importance of early diagnosis and treatment of hypertension for the prevention of cardiovascular disease (CVD), young adults ages 18–39 years in NHANES are less likely to be aware they are hypertensive (59 % vs. 84 %) and are less likely to be receiving treatment for their hypertension (40 % vs. 77 %) compared to older adults.6
Several factors may contribute to lack of awareness and treatment of hypertension in young adults. Young adults have traditionally been less integrated into the healthcare system, as they are more likely to be uninsured and less likely to have a usual source of care.7–9 Provider specialty and both provider and patient perceptions of risk based on patient age, gender, race/ethnicity, or comorbidities may impact awareness and treatment as well. A recent study of adults with regularly scheduled physician visits who met clinical criteria for hypertension found that those who were ages 18–24 years vs. at least 60 years of age were 28 % less likely to have their hypertension diagnosed by their physician.10 Moreover, young adults are less likely to receive information about lifestyle changes to address hypertension.11 Often described as the “young invincibles,”12 young adults may also not consider themselves at risk for chronic diseases such as hypertension and cardiovascular disease (CVD0.
Identifying and treating hypertension in young adulthood may forestall development of adverse vascular changes that are harder to treat once present at older ages. Despite the importance of detection and treatment of hypertension in young adulthood, limited data exist on their prevalence and determinants. Much of what is known about the national prevalence of hypertension awareness, treatment, and control comes from NHANES, which includes a limited number of young adults. We aimed to describe rates of hypertension awareness and control in a large, racially and ethnically diverse, nationally representative cohort of more than 13,000 young adults aged 24–32 years participating in the National Longitudinal Study of Adolescent Health (Add health). In addition, we aimed to understand the impact of health insurance status, utilization of preventive care, and perception of health status on rates of hypertension awareness and control in this sample. We hypothesized that young adults with hypertension who were without health insurance, who had gone more than 2 years without preventive care, and who perceived themselves to be in excellent health would be less likely to be aware of their diagnosis, or to have their hypertension controlled even if aware.
METHODS
We used data from the fourth Wave of the National Longitudinal Study of Adolescent Health (n = 15,701), a nationally representative school-based study of adolescents enrolled in grades 7–12 at initial recruitment (Wave I) in 1994–1995. Wave IV occurred in 2007–2008, when the participants were ages 24–32 years. Informed consent was obtained at Wave I and the study was approved by the Institutional Review Board at the University of North Carolina Chapel Hill13; additional analyses were approved by the Boston Children’s Hospital Office of Clinician Investigation. We excluded participants with missing data for sample weights (n = 901) and those currently pregnant (n = 487). We also excluded those with height < 58 inches or > 84 inches (n = 219), weight <80 lb or > 440 lb (n = 45), systolic blood pressure < 80 mmHg or > 200 mmHg (n = 2), and diastolic blood pressure < 40 mmHg or > 120 mmHg (n = 22), due to concerns about biologic plausibility or measurement error. In addition, we excluded those who had missing data for either the outcome variable or for any of the key independent variables (n = 513). Because there was a high non-response rate for income (∼7 %), we imputed income by Gaussian normal regression to avoid selection bias. After this imputation and all exclusions, the final sample contained 13,512 young adults (86 % of Wave IV participants).
Outcome Measurements
Outcome Variables
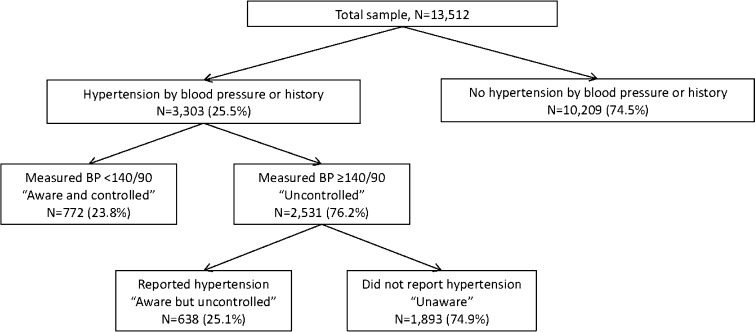
Blood pressure was measured by trained Add Health field interviewers using an appropriately sized arm cuff and an automatic oscillometric monitor approved by the British Hypertension Society (BP 3MC1-PC_IB; MicroLife USA, Inc., Dunedin, FL).14 Three blood pressure measurements were taken at 30-second intervals from the right arm with the patient in the resting, seated position after 5 minutes of rest. The second and third measurements were double-entered and then averaged to give the final blood pressure recorded. We classified participants as hypertensive if they had an average measured systolic blood pressure ≥ 140 mmHg, an average measured diastolic blood pressure ≥ 90 mmHg, or an affirmative response to the question “Has a doctor, nurse, or other health care provider ever told you that you have/had high blood pressure or hypertension (if female, added ‘when you were not pregnant’)?” We defined blood pressure control as an average measured systolic blood pressure < 140 mmHg and an average measured diastolic blood pressure < 90 mmHg (Fig. 1). We assessed awareness of hypertension only among those with uncontrolled hypertension using the question above and control of blood pressure to goal only among those aware of having hypertension.
Figure 1.
Unweighted number and weighted percentage of young adults ages 24–32 years with hypertension† who were aware‡ but not currently measuring hypertensive (controlled)§, aware but still hypertensive (uncontrolled)§, and unaware and uncontrolled. Data from the National Longitudinal Study of Adolescent Health, 2007–2008. BP = blood pressure. †We defined hypertension an average measured systolic blood pressure ≥ 140 mmHg or an average measured diastolic blood pressure ≥ 90 mmHg or self-report of a history of hypertension. ‡Participants were asked, “Has a doctor, nurse, or other health care provider ever told you that you have/had high blood pressure or hypertension (if female, added ‘when you were not pregnant’)?” Those who answered “no” were considered unaware and those who answered “yes” were considered aware. §We defined blood pressure control as an average measured systolic blood pressure ≤ 140 mmHg and an average measured diastolic blood pressure ≤ 90 mmHg among those aware of having hypertension.
Primary Exposure Variables
We categorized health insurance status into uninsured, public insurance (Medicaid or Indian Health Service), or commercial insurance based on participant self-report. We defined recent preventive care as reporting seeing a health care provider for a routine check-up within the past 2 years. We categorized participants as having self-rated excellent health if they answered “excellent” when asked “In general, how is your health?” and collapsed the other response choices of “very good,” “good,” “fair,” or “poor” into a referent category.
Additional Independent Variables
We constructed five racial/ethnic categories based on participant responses to two questions regarding racial identity and whether participants were of Hispanic/Latino origin: Asian/Pacific Islander, black/African American, Hispanic, multi-racial/other, and white. We used participants’ self-reported household income and household size to create income as a percentage of the poverty level in 2008,15 and then categorized based on standards used in NHANES reporting.5 We collapsed the highest level of education achieved as reported by the participant into four categories: less than high school, high school graduate, some college, and college graduate. We dichotomized tobacco use into current smoking (at least one cigarette in the past 30 days) vs. former/never smoking, and alcohol use into at least weekly use vs. less than weekly use based on participant self-report. We calculated body mass index (BMI = weight [kg]/height [m2]) from measured weight and height when available (98 %) and from self-report in the small number of participants missing measured height and weight. We defined underweight as BMI < 18.5 kg/m2; normal weight as BMI ≥ 18.5 and < 25; Overweight as BMI ≥ 25 and <30; and Obese as BMI ≥ 30 using the Centers for Disease Control standard weight status categories. Due to the small number of underweight participants (n = 203), we collapsed underweight and normal weight into one group. We defined use of a blood pressure lowering medication as taking a beta-blocker, calcium channel blocker, diuretic, angiotensin converting enzyme inhibitor, angiotensin II receptor blocker, anti-adrenergic, vasodilator, or antihypertensive combination medication in the past 4 weeks as inventoried in the home by the Add Health field interviewer using Lexicon Plus (Lexi-Comp, Inc., Hudson, OH).14
Statistical Analysis
All analysis was performed using STATA SE 12.1 (Stata Corporation, College Station, TX). Survey sampling weights were applied to account for the unequal likelihood of certain subpopulations being sampled. Bivariate analyses of the covariates of interest with the primary outcomes of hypertension awareness and control were done to test for significant relationships with chi-square tests for categorical variables and simple linear regression for continuous variables. We then created logistic regression models to identify the association of the covariates of interest with the primary outcomes, selecting variables known to be associated with the outcomes in prior literature. We present models including each predictor variable first adjusted for age and gender, and then adjusted for age, gender, time since last routine check-up, health insurance status, self-rated health, race/ethnicity, income as a % of the federal poverty level, highest educational level achieved, tobacco and alcohol use, and body mass index category.
RESULTS
Demographic characteristics of the sample are presented in Table 1. The mean age was 29 years (standard error (SE) 0.1 years). Mean body mass index (BMI) was 28.8 kg/m2 (SE 0.1), mean systolic blood pressure was 125 mmHg (S.E. 0.2), and mean diastolic blood pressure was 79 mmHg (SE 0.2); 1,410 (11 %) reported a history of hypertension and 2,531 (19.4 %) had a measured blood pressure in the hypertensive range, for an overall prevalence of hypertension of 25.5 %. The prevalence of hypertension was higher among participants who were older than 28 years (27.3 %), male (32.9 %), non-Hispanic black (28.7 %), current tobacco smokers (27.2 %), or obese (37.1 %), as well as those who reported an income less than 100 % of the federal poverty level (29.6 %) or a high school education or less (30 %). Participants who reported that their health was less than excellent were more likely to be hypertensive (27.6 %) compared to those with self-reported excellent health (16.6 %). The prevalence of hypertension was higher among those who were uninsured (27.7 %) compared to those with private health insurance (24.8 %).
Table 1.
Demographics Characteristics of Young Adults in Wave IV of the National Longitudinal Study of Adolescent Health 2007–2008, N = 13,512
| Characteristic | N (unweighted) | % (95 % C.I.) (weighted) |
|---|---|---|
| Age | ||
| 24–28 years | 3,964 | 35.3 (28.8–41.7) |
| 29–32 years | 9,548 | 64.7 (58.2–71.2) |
| Sex | ||
| Male | 6,549 | 52.3 (51.1–53.6) |
| Female | 6,963 | 47.7 (46.4–48.9) |
| Race/ethnicity | ||
| White, non-Hispanic | 7, 292 | 66.4 (60.7–72.0) |
| Black, non-Hispanic | 2, 887 | 15.5 (11.5–19.6) |
| Hispanic | 2,158 | 11.9 (8.5–15.3) |
| Asian, non-Hispanic | 867 | 3.6 (2.1–5.1) |
| Other race, non-Hispanic | 308 | 2.6 (2.0–3.3) |
| Income as % of federal poverty level | ||
| < 100 % | 1,478 | 11.9 (10.3–13.5) |
| 100–299 % | 4,989 | 37.2 (35.5–38.9) |
| 300–499 % | 4,060 | 29.7 (28.3–31.1) |
| ≥ 500 % | 2, 985 | 21.2 (19.2–23.1) |
| Highest education level | ||
| Less than high school | 1,020 | 8.9 (7.5–10.3) |
| High school graduate | 2,152 | 17.5 (15.7–19.2) |
| Some post-high school education | 5,977 | 43.2 (41.5–44.9) |
| College graduate | 4,363 | 30.4 (27.2–33.7) |
| Smoking status | ||
| Not current/never smoked tobacco | 8,614 | 60.5 (58.6–62.4) |
| Current tobacco smoker | 4,898 | 39.5 (37.6–41.4) |
| Alcohol consumption | ||
| Less than one drink per week | 9,613 | 69.6 (67.5–71.7) |
| One drink per week or more | 3,899 | 30.4 (28.3–32.5) |
| Self-rated excellent health | ||
| No | 10,936 | 81.1 (80.0–82.2) |
| Yes | 2,576 | 18.9 (17.8–20.0) |
| Routine check-up in past 2 years | ||
| No | 3,305 | 26.9 (25.3–28.4) |
| Yes | 10,207 | 73.1 (71.6–74.7) |
| Health insurance status | ||
| Uninsured | 933 | 7.4 (6.1–8.7) |
| Public insurance | 2,879 | 23.0 (21.5–24.5) |
| Private insurance | 9,700 | 69.6 (67.5–71.8) |
| Weight status | ||
| Underweight (BMI < 18.5 kg/m2) | 203 | 1.5 (1.3–1.8) |
| Normal (BMI ≥ 18.5 and < 25 kg/m2) | 4,350 | 32.4 (31.1–34.2) |
| Overweight (BMI ≥ 25 and < 30 kg/m2) | 4,084 | 30.0 (28.7–31.2) |
| Obese (BMI ≥ 30 kg/m2) | 4,875 | 35.9 (34.2–37.4) |
| Blood pressure classification | ||
| Normal | 4,456 | 31.4 (30.2–32.7) |
| Prehypertension (SBP 120–139 or DBP 80–89) | 6,525 | 49.1 (48.1–50.2) |
| Stage I hypertension (SBP 140–159 or DBP 90–99) | 2,073 | 15.9 (15.0–16.8) |
| Stage II hypertension (SBP ≥ 160 or DBP ≥ 100) | 458 | 3.5 (3.1–3.9) |
| Report history of hypertension | 1410 | 10.9 (10.1–11.8) |
| Hypertension by measured blood pressure or history | 3303 | 25.5 (24.3–26.7) |
| On a medication known to treat hypertension† | 480 | 3.7 (3.3–4.1) |
C.I. confidence interval; BMI Body Mass Index
†Beta-blocker (N = 154), angiotensin converting enzyme inhibitor (N = 137), diuretic (N = 107), calcium channel blocker (N = 58), angiotensin II receptor blocker (N = 37), antihypertensive combination medication (N = 65), or other (vasodilator, anti-adrenergic, N = 17). Of the 480 participants taking a medication known to treat hypertension, 404 (84.2 %) were taking one medication, 59 (12.3 %) were taking two medications, 14 (2.9 %) were taking three medications, and three (0.6 %) were taking four medications
2,531 (76.2 %) of the 3,303 young adults with hypertension had uncontrolled hypertension, and 1,893 (74.9 %) of those with uncontrolled hypertension were unaware that they had elevated blood pressure (Fig. 1). In unadjusted analyses, the prevalence of hypertension awareness among those with uncontrolled hypertension was highest among females, non-Hispanic blacks, those who did not drink alcohol regularly, who were obese, who rated their health as less than excellent, who reported a recent preventive care visit, and those with public health insurance (Table 2). In the multivariate model adjusted for sociodemographic and clinical features, the associations between hypertension awareness and preventive care utilization and self-rated health status were only modestly attenuated compared to models adjusted for age and gender alone (Table 3). Participants who had had routine preventive care in the past 2 years were 2.4 times more likely than those without a preventive care visit to be aware of their uncontrolled hypertension (95 % confidence interval (CI): 1.68–3.55). Young adults who believed they were in excellent health were 64 % less likely (OR 0.36, 95 % CI: 0.23–0.57) to be aware they had hypertension compared to those who reported their health as less than excellent.
Table 2.
Characteristics Associated with Hypertension Awareness Among 2,531 Young Adults with Uncontrolled Hypertension Participating in the National Longitudinal Study of Adolescent Health
| Characteristic | N with uncontrolled hypertension (unweighted) | N aware (unweighted) | % aware (95 % C.I.) (weighted) |
|---|---|---|---|
| Age | |||
| 24–28 years | 618 | 148 | 23.5 (19.4–28.1) |
| 29–32 years | 1,913 | 490 | 25.8 (23.0–28.8) |
| Sex | |||
| Male | 1,716 | 398 | 22.7 (19.6–26.2) |
| Female | 815 | 240 | 30.9 (27.3–34.8) |
| Race/ethnicity | |||
| White, non-Hispanic | 1,320 | 318 | 23.4 (20.8–26.3) |
| Black, non-Hispanic | 593 | 171 | 31.0 (26.4–36.1) |
| Hispanic | 379 | 81 | 23.6 (16.4–32.7) |
| Asian, non-Hispanic | 168 | 48 | 28.0 (19.3–38.7) |
| Other race, non-Hispanic | 71 | 20 | 30.0 (16.0–48.9) |
| Income as % of federal poverty level | |||
| < 100 % | 319 | 101 | 27.1 (21.9–32.9) |
| 100–299 % | 939 | 234 | 25.5 (21.6–29.8) |
| 300–499 % | 742 | 170 | 22.7 (18.9–26.9) |
| ≥ 500 % | 531 | 133 | 26.4 (21.7–31.6) |
| Highest education level | |||
| Less than high school | 242 | 56 | 23.7 (16.7–32.4) |
| High school graduate | 469 | 114 | 22.1 (17.4–27.7) |
| Some post-high school education | 1,142 | 303 | 27.1 (23.2–31.5) |
| College graduate | 678 | 165 | 24.7 (20.8–29.1) |
| Smoking status | |||
| Not current/never smoked tobacco | 1,498 | 388 | 26.1 (23.4–28.9) |
| Current tobacco smoker | 1,033 | 250 | 23.8 (20.5–27.6) |
| Alcohol consumption | |||
| Less than one drink per week | 1,677 | 462 | 27.9 (24.9–31.1) |
| One drink per week or more | 854 | 176 | 19.9 (16.4–23.9) |
| Weight status | |||
| Normal or underweight (BMI < 25 kg/m2) | 431 | 68 | 16.5 (12.4–21.7) |
| Overweight (BMI ≥ 25 and < 30 kg/m2) | 741 | 147 | 19.7 (15.6–24.4) |
| Obese (BMI ≥ 30 kg/m2) | 1,359 | 423 | 31.3 (28.1–34.6) |
| Self-rated excellent health | |||
| No | 2,183 | 602 | 27.3 (24.7–30.0) |
| Yes | 348 | 36 | 11.3 (7.5–16.7) |
| Routine check-up in past 2 years | |||
| No | 710 | 126 | 14.2 (11.0–18.2) |
| Yes | 1,821 | 512 | 29.9 (26.9–33.1) |
| Health insurance status | |||
| Uninsured | 635 | 151 | 21.1 (17.3–25.5) |
| Public insurance | 176 | 54 | 34.8 (25.9–44.9) |
| Private insurance | 1,755 | 433 | 25.8 (23.0–28.8) |
C.I. confidence interval; BMI Body Mass Index
Table 3.
Odds of Hypertension Awareness Among 2,531 Young Adults with Uncontrolled Hypertension Participating in the National Longitudinal Study of Adolescent Health
| Characteristic | Adjusted for age and sex | Additionally adjusted for all covariates in the table |
|---|---|---|
| OR (95 % CI) | ||
| Time since last routine check-up | ||
| More than 2 years | 1.0 (ref) | 1.0 (ref) |
| Within past 2 years | 2.46 (1.74–3.47) | 2.44 (1.68–3.55) |
| Health insurance status | ||
| None | 1.0 (ref) | 1.0 (ref) |
| Public health insurance | 1.72 (1.03–2.90) | 1.45 (0.79–2.67) |
| Private health insurance | 1.28 (0.98–1.68) | 1.06 (0.77–1.45) |
| Self-rated health | ||
| Less than excellent | 1.0 (ref) | 1.0 (ref) |
| Excellent | 0.35 (0.22–0.56) | 0.36 (0.23–0.57) |
| Age 24-28 years | 1.0 (ref) | 1.0 (ref) |
| Age 29-32 years | 1.11 (0.83–1.49) | 1.08 (0.79–1.47) |
| Female | 1.0 (ref) | 1.0 (ref) |
| Male | 0.66 (0.50–0.87) | 0.87 (0.64–1.19) |
| White, non-Hispanic | 1.0 (ref) | 1.0 (ref) |
| Black, non-Hispanic | 1.39 (1.06–1.81) | 1.27 (0.96–1.69) |
| Hispanic | 1.02 (0.65–1.60) | 0.95 (0.58–1.57) |
| Asian, non-Hispanic | 1.28 (0.79–2.07) | 1.14 (0.68–1.92) |
| Other race, non-Hispanic | 1.40 (0.61–3.23) | 1.29 (0.52–3.20) |
| Income < 100 % FPL | 1.0 (ref) | 1.0 (ref) |
| Income 100–299 % FPL | 0.96 (0.67–1.38) | 1.04 (0.64–1.67) |
| Income 300–499 % FPL | 0.84 (0.58–1.22) | 0.91 (0.55–1.52) |
| Income ≥ 500 % FPL | 1.06 (0.72–1.57) | 1.31 (0.76–2.23) |
| Less than high school education | 1.0 (ref) | 1.0 (ref) |
| High school graduate | 0.91 (0.54–1.52) | 0.94 (0.54–1.62) |
| Some post-high school education | 1.16 (0.71–1.91) | 1.16 (0.67–2.04) |
| College graduate | 1.01 (0.60–1.70) | 1.13 (0.60–2.13) |
| Not current smoker/never smoked | 1.0 (ref) | 1.0 (ref) |
| Current smoker | 0.92 (0.74–1.14) | 1.10 (0.86–1.41) |
| Less than one alcoholic drink per week | 1.0 (ref) | 1.0 (ref) |
| One alcoholic drink per week or more | 0.68 (0.51–0.92) | 0.77 (0.56–1.04) |
| Normal/underweight | 1.0 (ref) | 1.0 (ref) |
| Overweight | 1.25 (0.80–1.95) | 1.20 (0.76–1.89) |
| Obese | 2.26 (1.57–3.27) | 1.89 (1.27–2.80) |
OR Odds Ratio; C.I. confidence interval; FPL federal poverty level; ref referent group. OR in bold differ significantly from the referent group (p<0.05 or less)
To examine whether awareness was associated with severity of blood pressure elevation, we conducted a secondary analysis restricting cases to the 458 young adults with Stage II hypertension (SBP ≥ 160 or DBP ≥ 100). Although a higher rate of awareness was found among those with Stage II hypertension (42 %) compared to those with uncontrolled hypertension in general, 267 of the 458 young adults with very elevated blood pressures were unaware they had hypertension. Correlates of awareness of Stage II hypertension were similar to those observed for overall hypertension. In models adjusted for all sociodemographic and clinical variables, individuals with stage II hypertension who had (vs. didn’t have) a recent preventive care visit were more likely to report a history of hypertension (adjusted odds ratio (OR) 2.08, 95 % CI 1.13–3.82), while those with self-rated excellent health were less likely to report a history of hypertension than those reporting less than excellent health (adjusted OR 0.27, 95 % CI 0.08–0.96).
Only 772 (55.4 %) of the 1,410 participants who were aware of having hypertension had their blood pressure controlled to goal levels. In unadjusted analyses, blood pressure control was more common in females (60.2 %) than males (52.2 %). Although hypertension prevalence was higher with higher with weight status, control was more likely among those of normal weight (67.4 %) compared to those who were obese (50.6 %). Neither recent preventive care, health insurance status, nor self-perception of health was associated with blood pressure control in unadjusted or adjusted models. Males (OR 0.71, 95 % CI 0.53–0.95) and those who were obese (OR 0.47, 95 % CI 0.31–0.70) were less likely to have their blood pressure controlled in fully adjusted models. Among the 1,410 participants who were aware of their hypertension, taking a medication known to treat hypertension (N = 362, 25.5 %) was not associated with greater likelihood of control of blood pressure to goal (OR 1.03, 95 % CI 0.78–1.37).
DISCUSSION
The results of this study demonstrate that hypertension and hypertension unawareness are common in the young adult population. One-quarter of participants in this nationally representative sample of over 13,000 young adults had hypertension, but 76 % did not have their blood pressure adequately controlled, and three-quarters of them were unaware they had elevated blood pressure. While the rates of hypertension awareness were higher among young adults with stage II hypertension, perhaps reflecting providers’ increased willingness to diagnose hypertension in young people with significantly elevated blood pressures, the majority of those in this higher risk group were also unaware. Given that markers of preclinical CVD, such as left ventricular hypertrophy, increased arterial stiffness, and increased carotid intima-medial thickness are more likely to be present in pre-hypertensive and hypertensive young adults relative to their normotensive counterparts,16 lack of hypertension awareness and control in young adults may have significant clinical impact in terms of increasing rates of myocardial infarction, stroke, congestive heart failure, and kidney failure as this population ages.
The prevalence of measured hypertension observed in the Add Health cohort is greater than the 4 % prevalence seen in a similar age group in the NHANES population,14 although rates of hypertension unawareness are high in both cohorts.6 Add Health used an oscillometric device whereas blood pressure is auscultated for NHANES participants. The algorithm for the device used in Add Health has been rigorously validated17 and the reliability of the Add Health measurement protocol has been established.14 Furthermore, the prevalence of measured hypertension in Add Health is similar to rates of hypertension in young adults in other countries.18 However, it is unclear whether population estimates from Add Health or NHANES are closer to the true prevalence of hypertension in American young adults. While some regression to the mean is expected in repeated measurements of blood pressure over time, in one study of young men ages 23–41 years, of whom 34 % were hypertensive at enrollment, 24 % of all participants remained hypertensive after 5 years of follow-up.19 Thus, it is likely that a proportion of those participants who measured hypertensive in Add Health will have persistent hypertension, but the exact number is unknown.
Hypertension awareness was about two-fold higher in young adults who had seen a provider for routine health care in the past 2 years. This finding is similar to associations found in studies of all adults aged ≥ years 18 in NHANES.5,20 The Affordable Care Act, which allows individuals under age 26 to be covered as dependents under their parents’ insurance21 and requires preventive services be provided without any co-payment, holds promise for improving rates of screening, diagnosis, and treatment of CVD risk factors in young adults. However, additional efforts to keep youth connected to the health care system as they leave their pediatric medical home and transition to adulthood will likely be required as well.22 Public health campaigns should continue to raise awareness that medical problems such as hypertension can start early in life and not cause symptoms.
Only female sex and non-obese weight status were associated with control of hypertension to goal levels among those young adults reporting a history of hypertension. Being on a medication known to treat blood pressure was not associated with greater odds of blood pressure control, which may reflect sub-optimal compliance with medications in this age group.8,23 While we were unable to assess whether the participants received lifestyle counseling for any health problems, there is evidence from prior studies that young adults with hypertension11 and young adults in general24 are unlikely to receive counseling regarding healthy diet and exercise. Strategies to increase both prescription of and adherence to lifestyle recommendations and medication therapies are likely needed to improve blood pressure control in this age group.
Our study has several strengths. Add Health is a large, nationally representative cohort and contains greater numbers of young adults with greater racial and ethnic diversity than in NHANES, from which most of the previous literature on blood pressure awareness and control in young adults has been derived. Moreover, due to its focus on adolescents and young adults, we were able to examine factors that are especially germane to young adults, such as self-rated health status and attendance at routine preventive care visits. However, our study has several important limitations. Having been told one had hypertension was based on self-report and thus is subject to either under-reporting or over-reporting. Given that we assessed young adults’ own awareness of having hypertension, not clinician reports, we cannot distinguish between patient and provider factors leading to lack of awareness in this study. Because participants were not asked why they were taking medications during the medication inventory, we cannot be sure that medications were prescribed for blood pressure control as opposed to other indications, and we do not have data on medication compliance. Finally, because this is a cross-sectional observational study, one should not assume that the associations between preventive care, self-rated health status, and hypertension awareness or control are causal.
In conclusion, hypertension was relatively common in this large nationally representative sample of young adults. The majority of young adults with hypertension were unaware of their elevated blood pressure and rates of blood pressure control were substantially worse than those seen in older adults. Efforts to increase detection and treatment of hypertension should address young adults’ access to routine preventive health care and perception of their need for such care.
Acknowledgements
We thank Yuanjun Hu for thoughtful comments on the manuscript. Holly Gooding is supported in part by the Boston Children’s Hospital Office of Faculty Development Career Development Fellowship. This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
REFERENCES
- 1.Stamler J, Stamler R, Neaton JD. Blood pressure, systolic and diastolic, and cardiovascular risks. US population data. Arch Intern Med. 1993;153(5):598–615. doi: 10.1001/archinte.1993.00410050036006. [DOI] [PubMed] [Google Scholar]
- 2.Hsu CY, McCulloch CE, Darbinian J, Go AS, Iribarren C. Elevated blood pressure and risk of end-stage renal disease in subjects without baseline kidney disease. Arch Intern Med. 2005;165(8):923–8. doi: 10.1001/archinte.165.8.923. [DOI] [PubMed] [Google Scholar]
- 3.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903–13. doi: 10.1016/S0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 4.Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123(8):933–44. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 5.Vital signs: awareness and treatment of uncontrolled hypertension among adults--United States, 2003-2010. MMWR. 2012;61:703-709. [PubMed]
- 6.Yoon SS, Burt V, Louis T, Carroll MD. Hypertension among adults in the United States, 2009–2010. NCHS Data Brief. 2012;107:1–8. [PubMed] [Google Scholar]
- 7.Schiller JS, Lucas JW, Ward BW, Peregoy JA. Summary health statistics for U.S. adults: National Health Interview Survey, 2010. Vital Health Stat 10. 2010;2012(252):1–207. [PubMed] [Google Scholar]
- 8.Neinstein LS. The New Adolescents: An Analysis of Health Conditions, Behaviors, Risks and Access to Services Among Emerging Young Adults Los Angeles: University of Southern California Keck School of Medicine; 2013.
- 9.Fortuna RJ, Robbins BW, Mani N, Halterman JS. Dependence on emergency care among young adults in the United States. J Gen Intern Med. 2010;25(7):663–9. doi: 10.1007/s11606-010-1313-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johnson HM, Thorpe CT, Bartels CM, et al. Undiagnosed hypertension among young adults with regular primary care use. J Hypertens. 2013;32(1):65–74. doi: 10.1097/HJH.0000000000000008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Valderrama AL, Tong X, Ayala C, Keenan NL. Prevalence of self-reported hypertension, advice received from health care professionals, and actions taken to reduce blood pressure among US adults–HealthStyles, 2008. J Clin Hypertens (Greenwich). 2010;12(10):784–92. doi: 10.1111/j.1751-7176.2010.00323.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bibbins-Domingo K, Burroughs PM. Caring for the "young invincibles". J Gen Intern Med. 2010;25(7):642–3. doi: 10.1007/s11606-010-1388-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harris KM, Halpern CT, Whitsel E, et al. The National Longitudinal Study of Adolescent Health: Research Design. 2009; http://www.cpc.unc.edu/projects/addhealth/design. Accessed January 8, 2014.
- 14.Nguyen QC, Tabor JW, Entzel PP, et al. Discordance in national estimates of hypertension among young adults. Epidemiology. 2011;22(4):532–41. doi: 10.1097/EDE.0b013e31821c79d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Annual Update of the HHS Poverty Guidelines. US Department of Health and Human Services. Washington, DC: Federal Registrar; 2008:3971-3972.
- 16.Drukteinis JS, Roman MJ, Fabsitz RR, et al. Cardiac and systemic hemodynamic characteristics of hypertension and prehypertension in adolescents and young adults: the Strong Heart Study. Circulation. 2007;115(2):221–7. doi: 10.1161/CIRCULATIONAHA.106.668921. [DOI] [PubMed] [Google Scholar]
- 17.Cuckson A, Reinders A, Shabeeh H, Shennan A, Society BH. Validation of the Microlife BP 3BTO-A oscillometric blood pressure monitoring device according to a modified British Hypertension Society protocol. Blood Press Monit. 2002;7(6):319–24. doi: 10.1097/00126097-200212000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–23. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 19.Tongia R, Gupta R, Agarwal M, Gupta VP. Five-year blood pressure trends and regression-to-the-mean in an industrial population. J Assoc Physicians India. 2005;53:693–6. [PubMed] [Google Scholar]
- 20.Angell SY, Garg RK, Gwynn RC, Bash L, Thorpe LE, Frieden TR. Prevalence, awareness, treatment, and predictors of control of hypertension in New York City. Circ Cardiovasc Qual Outcomes. 2008;1(1):46–53. doi: 10.1161/CIRCOUTCOMES.108.791954. [DOI] [PubMed] [Google Scholar]
- 21.Cantor JC, Monheit AC, DeLia D, Lloyd K. Early impact of the Affordable Care Act on health insurance coverage of young adults. Health Serv Res. 2012;47(5):1773–90. doi: 10.1111/j.1475-6773.2012.01458.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lemly DC, Weitzman ER, O’Hare K. Advancing healthcare transitions in the medical home: tools for providers, families and adolescents with special healthcare needs. Curr Opin Pediatr. 2013;25(4):439–46. doi: 10.1097/MOP.0b013e3283623d2f. [DOI] [PubMed] [Google Scholar]
- 23.Ishisaka DY, Jukes T, Romanelli RJ, Wong KS, Schiro TA. Disparities in adherence to and persistence with antihypertensive regimens: an exploratory analysis from a community-based provider network. J Am Soc Hypertens. 2012;6(3):201–9. doi: 10.1016/j.jash.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 24.Fortuna RJ, Robbins BW, Halterman JS. Ambulatory care among young adults in the United States. Ann Intern Med. 2009;151(6):379–85. doi: 10.7326/0003-4819-151-6-200909150-00002. [DOI] [PubMed] [Google Scholar]